Ortho II Midterm Review
advertisement

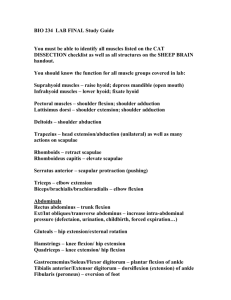
Orthopedics II – Midterm Review MUSCLE GRADING 5- Normal 4- Good 3- Fair 2- Poor 1- Trace 0- Zero Complete range of motion against gravity with full resistance Complete range of motion against gravity with some resistance Complete range of motion against gravity Complete range of motion against gravity eliminated Evidence of slight contractility. No joint motion. No evidence of contractility It is not fair to only test in one area. You need to take it through the full range of motion. Start testing at 3. Have the patient see if they can go through the full range of motion. Then see if some resistance can be given and then apply a little more resistance and see if the patient can complete it. 5 or 4 are acceptable. You might need to move the patient to get them in the right position to perform the test. If you were testing the muscle before it might be a different position for performing the grading of the muscle. When testing the abduction you can test the muscle in the prone position, but when grading the muscle they have to lie on their side. Many times you are testing for strength and symmetry (ROM). Biceps – C5 bicep flexion Triceps – C7 elbow extension Wrist extension – C6 Wrist flexion – C7 Digital Extension – C7 Gripping (8) – C8 Fan/ in between fingers – T1 Deep tendon reflex (DTR) – note if there is reinforcement used, so if testing again you can recreate the results again. Distract the patient while testing since sometimes people can inhibit the reflex Physical reinforcement can also be applied. For a patellar distraction the grip their hands and try to pull them apart. This can also try to allow a DTR. 4+ 3+ Very brisk, hyperactive; often indicative of disease; often associated with clonus (rhythmic oscillations between flexion and extension) Brisker than average; possibly but not necessarily indicative of disease – Spring 05 – Dr. Bozark – 1 Orthopedics II – Midterm Review 2+ 1+ 0 normal; average Somewhat diminished; low normal no response Usually a person who is a well trained athlete will have diminished reflexes. Coffee drinking could increase them. Alcohol and marijuana can cause the reflexes to diminish. Biceps tendon - C5 Brachio Radialis – C6 Triceps tendon – C7 Dermatomes Always check the unaffected side first. Ask the patient if they can feel the sharp or dull pain. If they can not differentiate then you can see there is decreased in sensation. HOMEWORK!! Due Friday the 21st 3 different types of dermatomal maps – compare and contrast the 3 sources You can do 1 – 4 pages of work. Also you can do written, table, or other forms of comparing. Tri 4 proficiency Check Sheet handed out. Dr. O’Brian to do tests. Sign up sheet with Linda. (this is required to complete orthopedics) Neurological Tests C5 – deltoid If wanting to see if the nerve root then test other muscles with C5 Innervation When testing the bicep you use your thumb at crease at elbow. Due not stretch the bicep because this will diminish the reflex. Hit your thumb nail with the hammer. 5 fingers should come up with the test. Epaulette (little shoulder) is the area with the True axillary nerve innervation Brachio radialis is an elbow flexor. C6 will flex the fingers and thumb C7 will flex middle finger dermatome, C8 dermatome is medial forearm T1 dermatome is medial arm, motor is interossie on fingers – Spring 05 – Dr. Bozark – 2 Orthopedics II – Midterm Review Read Chapter on cervical and lumbar. In the Hoppenfeld book. 1-19-05 Talked about inclinometers. Many different kind. (inclinometer is a goniometer and a goniometer is not always an inclinometer. Taking Measurements Take 3 measurements with each range and they should be within 10% of each other. Average them and then round to the nearest 5. Normal Values of ROM. Cervical, Shoulder, elbow, knee, ankle, wrist Regional Exam Inspection antalgic posture, lesions of skin, asymmetry, Palpation tissue tone, swelling ROM o Active what the patient can do o Passive or over passive you can apply a little more ROM without pain Orthopedic Neurologic o Sensory/motor/reflex DTR/superficial (skin (babinksi sign is testing the plantar reflex and is called babinksi’s sign when there is abnormal extensor) or mucosa)/pathologic Differential Diagnosis consider the likely possibilities rule in or rule out with Examination and relevant questions in History Decide which Special tests may be informative “Clinically Indicated” if the test results will affect your treatment plan X-ray is necessary on children sometimes when your treatment would change on the information received from the X-ray. Special tests X-ray Other imaging Lab o Blood o Urine o Other (hemoccult) EMG, Nerve Conduction Velocity, etc. 1-21-04 Coding these are located in the conditions manual 800 codes trauma, 700 subluxation these codes allow you to talk to the payer and other doctors Cervical strain and sprain are the same code (however there are differences) – Spring 05 – Dr. Bozark – 3 Orthopedics II – Midterm Review o Strain muscular injury by definition o Sprain is a ligamentous injury Grading 1 (ONE) o Simple strain/sprain – minimal disruption of adjacent fibers o 1-10% fiber damaged o Decreased motion due to swelling (sometimes) o Minimal pain, splinting, minimal palpatory pain o Trigger points, some loss of ROM (due to swelling or pain) o Fixation & decreased joint play in spine 2 (TWO) o Moderate strain/sprain – partial tearing of the ligaments or muscle, hemorrhage, marked pain & splinting o Mechanical stimulation of nociceptors along with chemicals given off by damage o 11-50% fiber damage – this can add to sloppy motion (hyper mobile) o Stretching ligaments results in pain o Athletic injury, lifting, trauma o Same clinical picture as above but more severe o Discoloration will be present and can be worse when lymphatic drainage is not present. (RICE) Rest, Ice, Compression, Elevation o Elevation can help with discoloration o The more immobilized the are the less the lymphatics will work 3 (THREE) o Severe strain/sprain – may be complete laceration o Refer for surgical evaluation (51-100% Fiber damage) At 100% rupture you must referral out At 51- 65% it may be feasible to treat the patient A complete strain is not manageable either (ACL) o Ecchymosis o Some say that there is no pain due to no tension, but there is due to other problems o Marked dysfunction o Palpate torn muscle Tendons are more vascular that ligaments Differential diagnosis testing (BE ABLE TO REPRODUCE THIS CHART)!!! (NMS) Passive ROM STRAIN mid to no pain except at end range (muscle stretch) SPRAIN Pain – ligaments are stretched Active ROM STRAIN painful (decreased ROM due to pain) SPRAIN Painful (decreased ROM due to pain) Isometric Contraction – Spring 05 – Dr. Bozark – 4 Orthopedics II – Midterm Review STRAIN Pain SPRAIN Mid or No Pain STRAIN muscle SPRAIN ligamentous Inclinometers Lumbar Lateral Bending Subtract the inferior from the superior one (coronal plane) Make sure that both are in the same orientation and plane. Flexion support them as in belts test and watch for the hips to move. Extension make sure that they keep the lower body stationary and focus the motion on the area being tested (Lumbar) Cervical Spine Flexion / Extension Cranium & at T1 Lateral bending Cranium & at T1 Need ROM equipment (read intro plus ch 1&2 from hoppenfeld) 5 cervical documentations for ROM ROM Cervical Orthopedics Lab Valsalva individual is going to hold breath and bear down. This increases intrathecal pressure. (this will show space occupying lesion) (DO NOT PERFORM IF KNOWN CARDIOVASCULAR DISEASE IS PRESENT) Spinal percussion tap down the spinouses to try and reproduce the pain. This helps with localizing the pain and with knowing where the subluxations are present. (spinous can show level, interspinous level reproduction can show CT problem / ligament sprain) O’Donoghue maneuver Resisted motion (compare with passive this can show ligamentous problems) Maximal cervical compression test involves rotation and lateral bending and the patient is instructed only on this test Foraminal compression test straight down in axis and this will compress the IVF. Do one face forward and one on each rotational side Jackson compression test Lateral bending trying to close joints on concave side (BE CAREFUL WITH THIS TEST) Spurlings test doctor drops hand onto his other hand that is placed on patients head. (lateral bending with some rotation / extension) Cervical Distraction should relieve pain when distraction is done Swallowing test Rust’s sign – Spring 05 – Dr. Bozark – 5 Orthopedics II – Midterm Review Cervical Facet syndrome – usually this type of fixation will be localized and is not dermatomal, but can be scleratomal (signs will follow spurlings test and relief will be given in cervical distraction) IVF – radicular symptoms, and present in compression Ligamentous problem – signs on distraction (pain) Tissue healing and repair deals with rabbit ligaments from Woo What is normal tissue healing? Clinical Phases of Recovery Phase 1: acute inflammation o First 72 hours o Hematoma/inflammation o Redness, pain, heat, swelling o White cells, phagocytes, and later o Fibroblasts are active at the site of injury Phase II: repair/ regeneration of cellular matrix o 28-72 hours until 6 weeks o Inflammation subsides and healing begins caution patient since the area may feel better even though it is not totally healed o Organization of blood clot o Granulation tissue and fibroblasts produce extracellular matrix (disorganized) o Increase in collagen concentration/elastin appears Phase III: remodeling / maturation o May require 12 months or more (ins. Will normally try to take away the patients money for care, yet they are not the one responsible) o Vascularity and cellularity decrease o Density of collagen increases, fibrils increase in diameter o Tensile strength may be only 50-70% after the healing is complete (this can set the stage for re-injury Phase IV: Maturation o Woo, et al o Rabbit MCL o Timing details of healing are ligament and individual specific o May be influenced by systemic and local factors Patient had whiplash from accident aka: cervical acceleration/ deceleration injury (CAD) CODE = 847.0, this code can be manipulated to fit a little better Cervical Strain (muscle) Cervical Sprain (ligament) Strain/Sprain implies injury to both, often misused If strain or sprain treat correctly, do not use strain/sprain freely – Spring 05 – Dr. Bozark – 6 Orthopedics II – Midterm Review Picture of accident of rear end crash Acceleration Torso is thrown forward and the head cannot follow so it hyper extends Lap belt keeps the body from ramping (pelvis lifts up and cervical spin is then the fulcrum Lumbar can also hyperextend. The seat is accelerating forward, this can cause the leg and knee to go backward and the force can be thrown into the hip Deceleration body forward, seat belt holds person (it may save the persons life, but it can destroy tissue and produce injury) Now head is going forward due to deceleration, the seat belt holding you in, and the extensors firing with a flexion response. Plus sometimes the seat can help catapult the head forward again Temperomandibular joint can be over stretched. Try extending with your mouth closed. Then try it with your mouth open. The symptoms are the same between the joint and cervical damage. So, make sure you are looking for the damaged joint as this can be affected by the accident. Make sure you evaluate all the cranial nerves too. (this takes 90 sec) Funduscopic exam. You actually look at the nerve and tissue. OBGYN, kidney, spleen, abdominal exam. Terms Active care – directed to ward returning the patient from an injury or illness to pre clinical status relief care rendered to reduce symptoms to a tolerable level and improve function Therapeutic care directed to further reduce symptomatology and improve function through correction of subluxation and its various component. This should enable a patient to perform most normal daily activities without frequent reoccurrences Rehabilitative care restoration of strength and stability Supportive care permanent, on going problem Acute – sharp, poignant, having a short and relatively severe course. Acute in this instance is meant to designate the new condition in less than 12 months mild no major joint involvement, a slight strain in back or neck with no prior history Moderate this condition usually requires rehabilitative care, but may not require supportive care in the mil-to-moderate case. severe severe, may reach maximum medical improvement (MMI), permanent change is structure Chronic – persisting over a long period of time, more than 12 months, reoccurring condition Mild without acute exacerbation, this condition may require little or no intensive relief care, but will require therapeutic, rehabilitative and supportive care Moderate with acute exacerbation, this condition will require all four levels of care – Spring 05 – Dr. Bozark – 7 Orthopedics II – Midterm Review Severe with serious acute exacerbation, this condition requires extended periods of all four levels of treatment Using the orthopedic tests you can see if your treatments are making a difference. With each level, mil to severe, a level of care will be determined for each. How long you do each type of care whether relief, therapeutic, rehab, or supportive care. Each will be different. TOS read the shoulder chapter in Evans (4 syndromes listed below) There are several specific types of TOS Scalene anterior syndrome Looking at the scalene and the compression which is sometimes called the interscalene pressure The floor is the 1st rib. Anterior and middle scalene make the walls of the triangle C2- C5 and T1 will be the effecting vertebrae. There can also be clavicle involvement sometimes, so look for it. Symptoms C7-T1 distribution of problems and it is called a plexopathy. The chief complaint in paresthesia which would be tingling or pain. Subclavian artery is also involved. So this TOS is a neuro/vascular problem. In order for the blood to move through a high velocity high pressure jet is formed. (this can blow out the blood vessel wall and even possibly start an aneurysm. Sometimes there will be a sound with this (a train or blowing across the top of a bottle sound), but normally there should not be any sound unless it is coming from the heart. It can be positional or permanent depending on the movement. Know the fundamentals of this for your practice. That way you can manage the area appropriately. BRUIT French word for sound Costo-clavicular compression Anterior weight bearing of the head and low shoulders. The patient will show this posture The clavicle is very mobile and is a major role in shoulder complaint. Pec major, clavicular, platisma, SCM, all attach to the Clavicle Bone Scoliosis this will also cause torque on the clavicle A broken clavicle can heal with large cartilage bundle. This could also cause compression at some point. TESTS retraction and rotation is one test exaggerated military stance Bringing the clavicle down Double crush syndrome more than one sight of compression and the clavicle is compressing it Pec minor/ coraco syndrome, Hyperabduction syndrome – Spring 05 – Dr. Bozark – 8 Orthopedics II – Midterm Review pec minor attaches to the coracoid process and to the 3rd-5th ribs. The nerves are wrapped around the artery (axillary) Hyper abduction will aggravate the syndrome the most Postural component and chief complaint always makes up the TOS syndrome Cervical Rib an anomaly which is just an enlargement of the cervical TP at C7 2/2/05 Anterior Head Carriage Extensors are working all the time, weakness of the deep flexors. Use kickball and flex your neck to your chest, flexing joint by joint. Also doing abdominal, core work in order to change the posture. Stabilize the sternum Figure 3-62 Soto Hall – Doctor will flex head This can show cord problems With this watch for knee flexion Lhermitte’s sign Figure 3-47 Passively flex head and neck if the patient experiences sharp radiating pain or paresthesia…this could show cord involvement Nattzigers Test Figure 3-52 Looking for back up of venous pressure with radicular pain…this would show pain from space occupying lesion do not apply bi lateral pressure on the neck (principle the same as valsalvas Swallowing Test Figure 3-70 Direct esophageal problems or space occupying lesion. this can also be a test for people with normal mechanical activity Rust’s Sign Figure 3-56 (NB TEST) They are holding the weight of the cervical spine up because the neck is not stable…this could happen with a diver and this could be a sign of a fractured atlas While laying down they hold their head up is also the same sign. Read the book by next wed. 2-9-04 Whip Lash make sure you are not fictitious with findings some victims get a lawyer so you might have to communicate the records to other people Hyperflexion / hyperextension Know what windows might have been cracked and if their head hit it. (door window or windshield) this could cause mild traumatic brain injury Inside the cranium – Spring 05 – Dr. Bozark – 9 Orthopedics II – Midterm Review o The frontal bone will slam into the frontal cortex. Then the brain slams back into the occiput. (this term is called contra coup. The head continues the slam back in forth in the calvarium until the energy is dissipated. Common Symptoms of PCS (post conclusive syndrome) (40 – 60% of the time some of these symptoms will arise. light headedness (top one) Vertigo/Dizziness (top one) Neck pain Headache Photophobia Phonophobia Tinnitus Impaired Memory Easy Distractibility Impaired Comprehension – this is hard on a Forgetfulness Impaired Logical Thought Difficulty with New or Abstract concepts Insomnia Irritability Easy fatigability Apathy Outbursts of Anger Mood Swings Depression Loss of libido Personality change Intolerance to alcohol – this can also be a sign of a person who has had a stroke These are all significant if the symptoms carry on over time Patients who have chronic pain for any reason can sometimes come up with some of these syndromes. PET positron electron transmission this looks at the brain to see what frequencies are going on CMT Chiropractic manipulative treatment 98940 Chiropractic manipulative treatment (CMT) : spinal, one to two regions 98941 spinal, three to four regions 98942 spinal, five regions 98943 extraspinal, one or more regions Fee Facts this is a reference book that can be found in the library – Spring 05 – Dr. Bozark – 10 Orthopedics II – Midterm Review Sensory motor and reflex testing, cervical spine, TOS, ROM (KNOW THIS FOR LAB) FEB 22nd lab test, Feb 23rd written 2-7-05 Types of shoulder problems Strain – muscle Shoulder sprain – rotator cuff sprain (ligamentous) Bursitis zip lock bag with some oil in it w/ no air. This is kind of how the bursa work. Since there is synovial fluid in it when synovitis occurs the fluid swells and can rupture. Abnormal movement usually causes this. Bursitis is usually a secondary trauma. (subdeltoid bursa and subacromial bursa moves with humerous head and would reproduce pain if shoulder is brought back) Tendonitis just means inflammation of the tendon. This can be caused by low grade irritation. (biceps long head tendon has a transverse ligament that covers it. 4 different muscles to consider supraspinous, infraspinous, teres minor, subscapular Flexion, Extension, Abduction , Adduction can be inhibited by breast or abdomen, internal and external rotation bend arm at elbow and then measure Dawbarns sign palpating the bursa, come inferior to acromian with pressure posterior and rotate arm back (this should create pain) Then abduct shoulder with palpation this will give relief to patient Appley’s test (scratch test) sometimes a camera might help with showing the patient the abnormalities. Reach behind back from above and below. (you can mark spinouses to measure differences. There should also be no pain with this test.) – deep knee bend is the equivalent for the lower extremity. Yergason’s test palpating long head of biceps tendon (palpate on anterior side of the humerous) looking at elbow flexion and forearm supination Speed’s test shoulder flexion and supinator resisted (palpate long head of bicep tendon) Transverse Humeral ligament test looks a lot like the shoulder ROM – internally and externally rotate the arm…seeing if the biceps tendon is coming out of the groove Abbott-Saunders palpate the transverse humeral ligament (long head) abduct the shoulder then swing it into external rotation…is the ligament staying in the groove Ludington’s Test procedure used for inspection and palpation of the biceps – patients hands on head and then ask them to flex (used to see if a tendon has ruptured) Codman’s sign or Codman’s drop arm if the patient has a torn rotator cuff (most common tear is supraspinatous) then the arm will not be able to stop at 90° when the doctor lets go. This is to test the integrity of the rotator cuff and bursa involved. – Spring 05 – Dr. Bozark – 11 Orthopedics II – Midterm Review Supraspinatous press test 4-65 tests for deltoid strength and supraspinatous – move arms in anterior and externally rotate from being abducted at 90°. 120% from glenohumeral joint 60% rotation from 30% at AcromioClavicular (AC) joint and 30% at SternoClavicular (SC) joint Impingement syndrome – chronic / repetitive Supra spinatous tendon and long head tendon of the biceps Great tuberosity and acromian process - rolling and sliding of the joint is needed o if it can roll but not glide and the humerous stays high, then it is lacking inferior slide (this is common too) o pure abduction supra spinatous, flexion long head o calcific tendonitis there is calcium there to try and reinforce the area that has been chronically weakened (it is also radiopaque) o Bursa is also nearby – the calcification can rupture the bursa Acute is smaller, Chronic is bigger calcification Adhesive capsulitis Passive and active motion is equal and reduced MUA manipulation under anesthesia Treatment protocol adjustment how often Exercise protocol all exercises should be performed vigorously at least 8 times a day. Joint motion should be carried into painful range. (pendulum and circular swing) Osteoporosis make sure you are careful with this Rotator cuff tear Subscapularis is torn and on the verge of tearing are the subscapularis and infraspinatous tendons. Ludingtons Test Rupture of Biceps brachii this can happen with trauma, or with tendon degeneration It Ends up as a big lump of flesh in arm. Function is lost also De Quervains Disease Stenosing Tenosynovitis Tendons that have a synovial sheath around it. And when narrowing happens the tendon then begins to wear. In the extensor retinaculum there is inflammation Usually cause pain in the snuff box Finkle Steins Test checks for this Involve abductor pollicis longus & Extenser pollicis brevis Trigger finger Stenosing Tenosynovitis – Spring 05 – Dr. Bozark – 12 Orthopedics II – Midterm Review Proximal to the distal metacarpal hand…what happens is that the tendon cannot slide through the retinaculum. It meets resistance Ganglionic cyst of the wrist Synovial hernia, a blow out form some synovial sheath. Begnin. Some people slam this with a book to make it go away or if it gets adjusted it could be corrected Dupuytrens contracture palmar apenuroisis is all over grown, they do not know what causes this. Conditions manual 124-125pg (NB part 2) Finish shoulder up in lab Shoulder dislocation This will not require guessing in the acute situation. Bryant’s sign 4-29 Inspection finding. We are to be looking at the axilla. The inferior portion will be more inferior on the side of dislocation. This could also be present in a scoliotic patient. In a patient who has it there will be a step off from the acromion process. Calloway’s Test 4-30 Tape measure used to check to see if there is asymmetry. An increased measurement could be from swelling. Atrophy can cause decreased measurement. Hamiltons test 4-46 Straight edge and go from lat. Epicondyl and touch the acromion process then the humerus has shifted Dugas Test 4-40 Patient places the hand on opposite shoulder. Then have patient bring elbow down to chest wall. This could not happen if a dislocation was present. Mazion Shoulder Maneuver 4-53 Hand on chest of opposite shoulder. Then lift the shoulder up. From chest up across brow. This is a test would increase pain if present. Apprehension test 4-25 Used for the old dislocation to see how intact the shoulder is and to see what type of reaction the patient will have. This should illicit a pain or fear response. You need to be able to see the facial response of fear. There are really three tests, Anterior, posterior, and another. House maids knee the knee blows out and is swollen. Pre-patellar bursitis Olecranon bursitis students elbow Ischial bursitis deep pain and tenderness over ischial tuberosity Acillobursitis – Spring 05 – Dr. Bozark – 13 Orthopedics II – Midterm Review VBAI RED BOOK pg 37 MEMORIZE THIS 5Ds and 3Ns ataxia also exists 1. Dizziness – know this from vascular and neurology etiology. Different things cause you to be dizzy. 2. Drop Attacks – loss of consciousness (syncope). Could be due to drop in blood pressure. 3. Diplopia – vision problems / 4. Dysarthria – speech problems 5. Dysphasia 6. Ataxia of gait 7. Nausea – possible vomiting 8. Numbness 9. Nystagmus (Transient ischemic attack) TIA short term ischemic attack to the brain Stroke permanent neurological damage (brain cells destroyed). Typically when these happen there is no recognizable cause or event that set the causes for the stroke. A common site is between C1 and C2 area. Rotational stretching is the main ideology. C2 and C3 is another common area too. Vascular accidents with cause childbirth, anesthesia, yoga, hanging up laundry, backing car up, dental work, amusement rides, break dancing, swimming, beauty parlor, football, intercourse, tai chi, star gazing, sleeping position. Intimal tearing of the arteries can cause the damage that could create a stroke condition. Thrombus can cause additional problems if things build up. Then if it breaks loose it becomes an embolism. Dissecting aneurysm is when the blood starts filling up into the vascular tissue Infarct stroke Wallenburg syndrome 1895. the vessel most commonly associated PICA (posterior inferior cerebellar artery) Lockdens syndrome middle portion of basilar artery (persistive vegetative State) In your history look for(smoking, oral contraceptives, Heart disease is not the number one cause of death now in country. It is number one in heart problems though. Warfarin used ion heart problems – Spring 05 – Dr. Bozark – 14