Habib & Scotti - School of Computer Science and Statistics
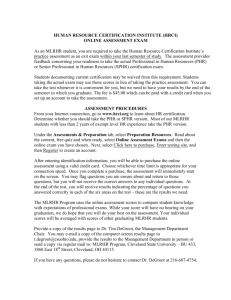
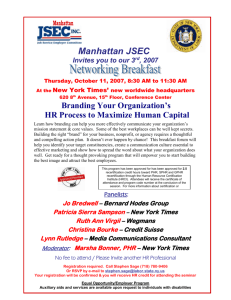
advertisement

IMPLEMENTING INNOVATION IN THE SERVICE RELATIONSHIP: HOW MANAGING CHANGE IN FRENCH HEALTHCARE COMPLEX SYSTEM? THE CASE OF THE PERSONAL HEALTH RECORD (PHR) PROJECT ----------------------------------------------------------------------------------------Habib Johanna CEROG- Public Management Institute Paul Cézanne University, Aix-Marseille III, 21 rue Gaston de Saporta, 13100 Aix-en-Provence France Email : johanna.habib@univ-cezanne.fr ----------------------------------------------------------------------------------------Scotti Nelly CEROG- Public Management Institute Paul Cezanne University, Aix-Marseille III, 21 rue Gaston de Saporta, 13100 Aix-en-Provence France Email: nelly.scotti@univ-cezanne.fr ---------------------------------------------------------------------------------------- Johanna Habib is a doctoral student in Management Science at. Paul Cézanne University, CEROG Public Management Institute, Aix-Marseille III, France. Her researches are focused on Innovation, Knowledge Management, Organizational Learning and complexity. Nelly Scotti is a doctoral student in Management Science at Paul Cezanne University, CEROG Public Management Institute, Aix-Marseille III, France. Her Investigation lines are focused on Public Management, Service Relationship and Healthcare Organizations. Abstract Our paper is focused on the implementation of the Personal Health Record (PHR), an innovation in the French healthcare system. This national experimental project provides the public health insurance users with a secure electronic medical record, under their own control. This paper attempts mainly to identify the specificities of the management of innovation in the service relationship and to provide some evidence about the key elements which favour or block the process of general and deep change in the healthcare system. First, the results show that innovations in the service relationship induce us to turn a particular attention about three essential aspects of change: technical, cultural and relational dimensions. Second, the case analysis reveals that several elements of Project Management seem overriding to generate change in the healthcare systems and to facilitate the generalization process of innovative approach. These Project Management dimensions are gathered in three themes: the diversity of interests, the contours of project and the project piloting. Afterwards, the empirical research confirms the relevance of the Service Relationship concept to apprehend the PHR innovation particularities and of Complex Adaptive System framework to understand innovation and change processes in the public system. Finally, we discuss the implications of these findings for research and practice and also make recommendations to encourage change opportunities in the process of implementing innovation in the service relationship. Key words Innovation, Service, Relationship, French Healthcare System, Complex Adaptive System, Qualitative Approach. 1 Introduction Increasingly, public organisations are becoming aware of the importance of Information Systems to manage their relationships with users. Most innovations in the public sector are currently focused on the “service delivery process” and “service relation”. After the movements of managerial rationalization of work and decentralization of competencies, the public service modernization took a new direction: the way of “service” for the users, characterised by a set of themes as processes reorganization, new technologies diffusion, development of electronic services, work’s polyvalence, reception training... However developing and implementing an innovation in the service relationship within public systems seems complex. In fact, this kind of innovation, focused on users’ needs, implies major transformations in organizational processes and configurations of interaction. Our paper is focused on the implementation of the Personal Health Record (PHR), an innovation in the French healthcare system. This national experimental project provides the public health insurance users with a secure electronic medical record, under their own control. The PHR is available on-line and contains all relevant medical information required for healthcare patients. It intends to improve the healthcare quality through an easier healthcare patient access to the medical information and through healthcare professional coordination and information-sharing. Yet, if the PHR seems expected by users of French healthcare system, its appropriation by healthcare professionals seems more problematic. This innovation necessitates that the healthcare system changes its culture, work modalities and interrelationships… This paper attempts mainly to identify the specificities in the management of innovation in the service relationship and to provide some evidences about the key elements which favour or block the process of general and deep change in the healthcare system. In this aim, the theoretical framework is built on a review of innovation and service relationship management theories and Complex Adaptive System (CAS) literature in order to propose a relevant and effective approach to change management in healthcare system. We use a classical case study methodology (Eisenhardt, 1989, Yin, 1994) based on a qualitative investigation (Miles and Huberman, 1984) and a combination of different collection methods – interviews with healthcare experts (key actors of PHR project), non-participant observations of workgroup sessions, and analysis of strategic documents. The used methodology allows exploring the external and internal change drivers. Our research intends to answer the following questions: - What are the specificities of innovation in the service relationship? - How grasping is the change in the complex healthcare organizations? - What are the key dimensions to implement innovation in the service relationship within the complex Healthcare system? 1. Innovation in the service relationship 1.1 The concept of service relationship 1.1.1 from particular characteristic to complex process Goffman (1961) introduced the concept of service relationship in an essay about psychiatric hospitals. According to Goffman (1961), the service relationship between two persons allows to understand the institutions (for example psychiatric hospital) in which the relationships are formed. The author doesn’t consider service relationship out of a specific professional context. In fact, the notion of service relationship relies on interaction. The customer’s (or user’s) participation constitutes the foundation of this specificity and establishes the service relationship. The active part of the customer consists in the production of data that the agent, the professional will be able to translate into relevant information for the service situation. 2 However more and more the service relationship is becoming automated and doesn’t need human contact even if human interaction is often necessary to complete or to help customers and conceive the concept of service relationship. By way of illustration, in French post offices or in the new projects in French hospitals, machines are set up to buy the television service, to select the channels and to take the remote control. In these cases of relation automatization, organizations used Medias like computers and software with specific interface in accordance with the kind of service. To obtain the best service relationship, the agents who have to use the technical interface (software, machine…), have to know and master it (having been trained). This induces that the service relationship activity is based on the agent’s technical expertise and on the customer’s trust towards the agent (Goffman, 1961). Sometimes when agents don’t receive sufficient training and are not acclimated to the technological change, the media can become a difficulty and act as interference within customers’ interaction. In parallel, Goffman (1961) makes apparent a distinction between different levels of verbal exchange in the service relationship. He discerns: a technical part linked to the technical competence of the agent (informational interaction), a “contractual part” (about frame, shapes of the unfolding of the service delivery process) and a sociability part (greetings). De Bandt and Gadrey (1994) submit a widening of Goffman distinction and strengthen operational interaction, the most important part even though it is reduced for some situations. This extension included information/data collection, advice/guidance or assistance. This proposal of De Bandt and Gadrey (1994) to use this concept to account for service delivery enhanced the first theoretical frame. “The service relation is a specific kind of producer-consumer relationship” (De Bandt and Gadrey, 1994, p.14) The concept of service relationship is defined by “the connexion modality between the suppliers and the customers about the object of the request.” (De Bandt and Gadrey, 1994, p.24). They observe in concrete service relationship existence of cooperation in the conception, realization and control of the service delivery process between actors of the “service offer” and those of the “service request”. The examination of service relationship concrete situations shows this cooperation is always accompanied by a variable uncertainty. If we can know about means committed by the two parts to deliver the service, we can’t foresee the final result (for example: customer’s satisfaction) (De Bandt and Gadrey, 1994). Moreover, we can consider the service relationship as “an experience within the experience”. The notion of service defines as an experience. The “servuction model” (Eiglier and Langeard, 1988) points to the decisive part played by contact agents in the production of service, as one of the three elements that are part of the organization. In our research, the meaning of service relationship comes from Goffman’s contribution crossed with De Bandt and Gadrey’s. We define service relationship as an interaction that needs cooperation between actors and constitutes a service experience not only for agents but also for users. 1.1.2 The key conditions of service relationship First, the service relationship profession requires various and complex competencies. The service relationship induces competencies of which the beneficiary of service is deprived. All service relationships unfold in a specific place that constitutes for the agent as well as for user a “meeting or encounter point”. For the agent, this place represents a workspace he has to control to facilitate activities he has to lead. The service relationship profession requires wide and various competencies. From the workspace control to the perceptive abilities, agents have to build the diagnostic and to formulate the request of the user explicitly, to be careful and listening to the public, to be didactic. The major part of its occupation consists in translation from user language to the agent’s language level and after that, in machine language, to collect and record information in the computer. It concerns to decode the request of the user and to encode it in a specific language of the software. More and more, this contact personal has also to develop management conflict abilities. Finally, the contact agent is a “sense worker” (Habermas, 1997). Then, the public service relationship relies on the users’ listening. Indeed in public services, the reflection around the service relationship is not new and is more often characterised by a strategic belief than by actual implementations. Service relationship then being mostly a slogan, to the point of sometimes loosing all meaning (Weller, 1998). “Service relationship is liable to serve as an example, 3 not in the sense where it would represent a kind of formula to be replicated, but where it would put at stake the connections between the various dimensions of work.” (Ughetto and al., 2002, page). Public organizations are concerned about serving their users better. (Weller, 1998). Numerous means are invested to improve the public service relationship. Public managers have become aware of the importance of contact agents and approach the problems of the service relationship and more particularly the wicket henceforth like a strategic point in their service delivery. “Personalization of processing, hybridization of “back office” with “front office”, the contact with agents, the emergence of administration control devices, the application of quality control and contentment proceedings of users contribute the wickets to be changed into important places of production and arbitration, whereas they just constituted annex of bureaucratic structure.” (Weller, 1998, p.3) Changes and evolutions of public services are focused on the user. In that extent, “service relationship” became a reference for managers. In order to analyse these evolutions, research reports have been developing new concepts and methods, as the model suggested by Erving Goffman (1961) about “tinkering trades”. These references give a better understanding of the whole complex activities of public servants and of the organizational framework in which they daily accomplish their work. But it also underlines moral troubles and abusive political implications of such a reference, when the expert servicing model is introduced into administrative institutions. 1.2 Innovate in the service relationship: What does it mean? 1.2.1 The concept of innovation If the concept of innovation refers traditionally to the development of new products and services, it covers different elements and viewpoints according to the disciplines and the selected analysis level – individual-oriented, structure-oriented, and interactive-oriented or systems of innovation oriented (Johannessen and al, 2001). In this research, the concept of innovation is defined as “the development and implementation of new ideas by people who over time engage in transactions with others within an institutional order. […] A new idea, which may be a recombination of old ideas, a scheme that challenges the present order, a formula, or a unique approach which is perceived as new by individuals involved.” (Van de Ven, 1986, 590-591). This definition offers a holistic view of innovation (new ideas, people, transactions and institutional context) and apprehends implicitly innovation as a learning and change process. The approach advocated here considers: First: innovation as a learning interactive process in which the participants improve their knowledge and their know-how by exchange and experimentation (Harkema, 2004; Baets, 1998). It concerns a sense making process that takes place in a specific social and institutional context (Weick, 1995) and brings about large structural relations between organizations; departments, services, and work groups with several different skills. Second: we assert that the innovation process cannot separate from the organizational change concept. Innovation induces systematically a dynamic of change. It seems in fact difficult and not relevant to mark out a fundamental distinction between innovation and change (Van de Ven, Angle & Poole, 2000). In a systemic and interactionist view, the analysis of the innovation process implies necessarily the study of change process which is connected with the development and implementation of newness and a change in collective representations which constitutes a point of leverage for innovation process. 1.2.2 How situating innovation in the service relationship: A third way between organizational and technological innovations? First of all, we must define the concepts of organizational and technological innovation in order to clarify the concept that we develop in this research: innovation in the service relationship. Technological innovation is generally considered the development and/or introduction of a new product or procedure which touches fundamental knowledge, techniques and methods within a specific business area (Temri, 2000). Often technological innovation relies on the evolution of scientific knowledge which is connected with the needs of market. This kind of innovation produces licenses and develops more frequently in the R&D department of one or several firms. Naturally, the development of technological innovation can cause organizational change and/or innovation. 4 The term 'organizational innovation' refers to the creation or adoption of an idea or behavior new to the organization (Daft 1978; Damanpour and Evan 1984; Damanpour 1996). This kind of innovation allows modifying more or less radically working methods of agents within organizations” (Charreire, 2003). Organizational innovations essentially concern management practices, work organization, decision-making process, etc. According to David (1996), organizational innovations have in common “the fact that the process linked with their introduction within organization concerns at once the relationships and the knowledge”. The relationships embody the whole contacts between entities within the organization and the knowledge regards the whole individual and collective knowledge within the organization. For instance, the introduction of project management into an organization modifies both relationships – especially the hierarchical relations between actors or groups of actors – and the way to create new knowledge. This definition could be appropriated to innovation in the service relationship if the external dimension (customers or users) was included. In fact, if innovation in the service relationship combines the two characteristics of organizational innovation (change in the relations and the modalities of knowledge creation), its main specificity relies on an external dimension: its customers or users. Moreover, this third way to innovate implies generally a technological component (Habib, 2007). We can consider the innovation in the service relationship required by a holistic and complementary perspective with the characteristics of technological and organizational innovations. PHR innovative project studied in this research demands to take into account both its internal dimension – change in the French Health Care operating and working–, its external dimension – change in the relationships between healthcare professional and users– and finally, in its technological dimension – appropriation of new technological tools and change in the social professional practices (De Sanctis and al, 2003). To study an innovation, customers or users, necessitates finally to consider technological and organizational innovation as mutually dependent. 1.2.3 Innovation in the public service relationship: the predominant role of Information System Modernization of public services is mainly centered on users. In order to simplify its steps and facilitate the relationship between public organizations and citizens, the essential lines of French reform is based on the best information for users and an internal reorganization of public services limiting the bureaucratic approaches. There is a need to rehabilitate the role of reception centers of public services, that is to say, to turn a particular attention to the agents’ management in contact with the users. At the present time, the reconfiguration of the agents’ work in contact with users in terms of service relationship is favorable to innovative approaches based on Information System – i.e. administration, e-government, e-democracy, computerization of administrative documents, geolocalization, etc… This is explained in particular by the backwardness of the public sector in relation to the private sector in the IS area. Indeed, when the private sector develops bottom-up innovation by the use of technologies analysis, the public sector tries to adapt its work organization and its services to ITC evolution. In other terms, public managers attempt to grasp the opportunities of ITC through the development of IS implementation. It seems indeed that IS in the public sector is able to ameliorate the representation and accessibility of users and more generally the performance and quality of service providers by a best rapidity, flexibility and transparency. Moreover the development of IS innovative approaches requires a transverse dynamic of change that could allow to limit the bureaucratic and hierarchical tendencies of public organizations. The ITC possibilities of communication and exchange invite to redefine the role of users and citizens in front of public services. The passive representation of users is not any more appropriate to the knowledge economy. These logics, impacting nearly the whole French public services, seem to particularly be present in the healthcare system. In the following PRH case presentation, we try to underline the stakes linked with the computerization issues. 5 2. The Personal Health Record case 2.1 The PHR context and stakes 2.1.1 The issue of Healthcare System Computerization In the French Healthcare system one of the difficulties is to reduce the gap of the computerization between liberal clinicians and public hospitals. The origins of this problem are, first, the different levels of information system investment, and second, “the appetence” of the clinicians for this topic. If the liberal clinicians are computerized to a great degree (between 80 and 85%), only 40 to 60% among them use a digital file and few use an opened patient record, sharing the same software. Regarding public hospitals, only 30% of them have an efficient information system. The information system investment corresponds to 5% of the total hospital investments. The PHR was created to provide all public health insurance beneficiaries with a secure electronic medical record, under their own control. The record will be accessible on-line. It will contain all relevant medical information required for patient care. It is intended to improve the quality of healthcare by facilitating coordination and information-sharing between healthcare professionals. The purpose of the PHR is to make patients able to provide healthcare professionals with the information needed for their care. The PHR will prevent possible errors due to healthcare professionals knowing which other healthcare professionals the patient has seen or what treatment he is under. This record will serve as the interface for healthcare professionals, providing them access to the medical information they need (hospital discharge reports, biological analyses, x-rays, medication provided by a pharmacist) and share the data that a given healthcare professional seems helpful to other healthcare professionals. It is also a mean of preventing redundant procedures. 2.1.2 The PHR stakes for the key actors PHR Stakes for patients: The generalized computerization of information systems is supposed to improve the relationship between physicians and patients. The main stake is to provide healthcare continuity to the patient. This centralization of the medical information is supposed to make progress in the quality of diagnosis by providing online decision tools and by helping the development of communication between the health professionals. PHR stakes for clinicians: The aim of the PHR is to improve practice of medicine by various tools especially assistance decision tools (for example: data basis about medicines, access to frame reference of good experiences), access to medical knowledge confirmed and developing teamwork and network. This project aims to expand the city-hospital network and link the town medicine and hospital sector, which is the main stake of the PHR. PHR stakes for public health: The main stake, from the point of view of public health, is to improve public policies by means of better health defence against epidemic and environmental peril by an improved knowledge of health condition of the population and the progression of transmissible disease. The benefit expected is the strengthening of a health watch plan thanks to circulation of vertical information and an improved epidemiological knowledge of the French population. 6 2.2 The PHR content and Project Owner 2.2.1 The PHR Content Foremost, the Personal Healthcare Record is a legal obligation according to articles 3 to 5 of the law concerning health insurance of August 13th 2004. The original idea was to set up a tool enabling us to centralize the patient’s personal health data, available for some medical personnel, respecting personal ownership of medical information. The first ambition of PHR is quality healthcare enhancement, which normally involves economic support. All health insurance cardholders will be able to open a PHR starting on 1 July 2007– in theory. The PHR will be created by the patient electronically, on an access portal. The PHR access portal can be described as a virtual reception centre. If the patient does not have internet access, approved public service providers will provide free access points on their premises. The PHR belongs to the patients who control the access rights. Healthcare professionals will have access to specific information, depending on their profession. The PHR will not be open to occupational physicians, or when a supplementary health insurance policy is taken out. Similarly, the site hosting services will not have access to PHR. For home use, a secured procedure, with login and password, is being prepared. The PHR will be handled by a State-approved healthcare data hosting service. This means that it meets public security requirements. The hosting service will not have access to the content of the PHR. The PHR will contain the last name and commonly-used first name, birth date, information used to identify personal physician and any information needed for healthcare coordination. At this stage, based on public consensus-seeking efforts on the MPR draft decree, the said information is defined as follows: - General medical data: personal medical and surgical histories, previous use of specialised medical services, recognised allergies, intolerances and vaccine history. Healthcare data: results from biological tests, reports from diagnostic and therapeutic procedures, diseases and treatment underway, etc. Imaging data: both reports and images: x-rays, IRM, etc. Each piece of information listed in the PHR will be dated, signed and its author identified. Doctors and healthcare professionals will supply the PHR only with the patient‘s personal approval. Health information will be entered solely by healthcare professionals. However, there will be room for personal statements so that the patient can talk about his health condition. The patient is allowed to hide medical information in his PHR, except from the healthcare professional who wrote it. 2.2.2. The Project team To design the PHR, a public organisation for the “Personal Health Record” (GIP-DMP) was established in spring 2005. It represents healthcare professions (doctors, pharmacists, hospital workers, midwives, dentists, academics, healthcare establishments, etc.) and patients. The latter will soon be more widely-represented. The GIP was first asked to conduct experiments and design the national deployment procedure. The GIP-DMP will steer the entire project, to the called timetable or by the law. The Grouping’s responsibilities will include the following: - - Maintaining relations with representatives of healthcare professions and patient associations regarding the personal medical record; informing healthcare professionals and the general public about the personal medical record; Determining which personal healthcare data, regarding prevention, diagnosis or healthcare, will be listed in the personal medical record and making it possible to monitor such aspects as healthcare procedures and services, pursuant to Article L. 1111-8 of the Public Health Code; 7 - - Determining the access and the hosting conditions of the personal medical record, whether in terms of viewing or making changes to the personal medical record, and conditions for passing on information from the healthcare data categories in the personal medical record. Steering and monitoring the implementation of experiments with the personal medical record on the 17 pilot sites. Designing and producing, as applicable, the supporting IT systems for the personal medical record. Steering and implementing the extension of the personal medical record to the entire population. If GIP-DMP is the project owner, other members are implicated in the PHR project: national government agencies, public health institutions, public health insurance bodies, hosts selected by GIPDMP to experiment PHR (for example Cegedim-Thalés, D3P, France Télécom – IBM, etc…) The experimentation of PHR took place last year, from June to December 2006. This step has been headed by the GIP DMP with six hosts with different offers and 17 pilot sites spread over 13 regions. 1500 liberal healthcare professionals, 68 private and public health organizations and 37 health network have been taking part. The aim of this step was to create 30.000 PHR for real patients and to connect all the hospitals involved. The members of this experimentation have been set up to a secure process, online data service certificates to guarantee the experimenters’ patients data security and confidentiality. If the date of PHR generalization was set up in July 2007, the project current difficulties delay this new stage. The budget dedicated to implementing the PHR system amounts to 1.2 to 1.5 billion €, to be used from 2006 to 2010. It is part of a broader healthcare information systems budget in the amount of 2.3 billion €. By better informing all of the practitioners treating a single patient and by fostering better familiarity with and monitoring of the said patient, the PHR will make it possible to downscale healthcare costs. For instance, 15% of all medical procedures are redundant and generate 1 to 1.5 billion € in costs per year. Likewise, some 128 000 hospitalisations occur each year, due to drug interactions (iatrogenisis), generating 283 million to 472 million € in healthcare costs. 3. The contribution of complex adaptive system theory to grasp innovation implementation in the French Healthcare System 3.1 French Healthcare System: A complex adaptive system? The terms of the complexity theory cover many fields and disciplines of academic research and so, they are characterized by an important diversity and a large multidisciplinary. The main theories classified under this label of “complexity theory” are, according to Stacey and Al (2002), chaos theory (Lorenz, 1972; Ruelle, 1991), dissipative structures theory (Prigogine and Stengers, 1984) and the theory of complex adaptive systems – CAS – (Gell-mann, 1994). Among the latter, CAS theory is the most commonly used in Organization Sciences, notably owing to the fact that it is easy transposable. 3.1.1 CAS Overview A CAS is made up of multiple interconnected and non-linear elements and numerous interdependent agents– individuals, groups and/or organizations – in interaction (Holland, 1995). The agents interact with each other, their behaviour are adaptive. They act locally according to their own functioning process. There is no global and fixed plan. The relations between agents are self-organised locally. “Entities’ adaptation is guided by the search of local interests and not by a mutual purpose to the whole agents” (Thiétart, 2000). The action processes evolve continuously by learning, adaptation to external influences, mutual and spontaneous interactions, etc. If the agents have autonomous and independent behaviours and act with their individual schemas, they are mutually dependent on the system. It seems important, in fact, to underline the highly connected nature of agents’ relationships in an adaptive system. The complexity of the system is produced by these multiple interactions between agents that can lead stable states as well as instable states. The system, understood as a whole that differ from the sum of the parts in interaction, is dynamic and non linear. The environment variations and changes and the agents’ capacities of adaptation, memorization and learning are so many 8 elements that make the behaviour of the system unpredictable. CAS generates emergent behaviours and self-organization. Thus, a CAS is dynamic and adaptive because their agents have the capacity to experiment and explore with new actions, to reconstruct and modify their mental schemas, to adapt and learn from their experiences and from experiences of other agents as well as the variations and changes in their environment. “Their ability to learn and adapt is underpinned by self-organizing behaviours, including exploration and experimentation” (Carlisle and MacMillan, 2006). After, this general CAS overview, it appears interesting to synthesize its main characteristics. 3.1.2 CAS Characteristics First, a CAS has a dynamic behaviour because of the presence of numerous heterogeneous agents, their interdependence, and their capacities to learn and adapt their behaviours according to the changes of their environment. Therefore, A CAS is constantly changing. Second, a CAS is a highly interrelated system. The variables and agents in the CAS operating are large in number, interdependent and connected in complex and non-linear ways. Besides, numerous factors influence the system operating and the interrelations between variables and agents. Third, a CAS operates simultaneously at many different independent scales (individual, group and organization). If each individual agent acts in an independent way, the agents’ interaction and adaptation (to each other) locally allow the emergence of group or organizational behaviours. These levels are both interdependent and connected with each others. Thus, they show regularities or similarities as well as irregularities and differences. Fourth, a CAS can evolve at the edge of chaos. Feedback loops – positive and negative – produce both periods of stability and periods of instability and chaos in the operating system. To survive and optimize the system, the agents, which evolve in an open environment, adapt and change their behaviours. In a CAS, equilibrium and stability can generate the death of the system. A CAS takes turns with order and disorder stages. The edge of chaos, a stage of moderated instability or “creative destruction”, fosters the appearance of emergent processes like change, creativity or innovation. In this perspective, Stacey (1995) compares creative and innovative act to a process that goes away to equilibrium, accepts disorder and uncertainty, self-organizes and adapts itself through learning. Fifth, a CAS is a self-organized and emergent system. The multiple interaction of agents and elements in the system produce new global patterns. Especially, when the system is situated at the edge of chaos, a bifurcation process allows the system self-organization and the emergence of new operating models and new behavioural rules. This change comes from an internal dynamic, as well as the influences of the external environment. New global patterns can be generated by small changes. Many works, especially in Management Science, have shown that organizations can be considered and therefore modelled as a complex adaptive system (Stacey 1993, 1995, 1996; Thiétart et Forgues, 1995; Cheng et Van de Ven, 1996; Brown et Eisenhardt, 1997; McKelvey, 1997; Boisot et Child, 1999) and more precisely as a CAS (Gell-mann, 1994, Stacey, 1996, Anderson, 1999). “A wide range of organizational theorists and practitioners have argued that organizations are complex, non-linear systems whose members (agents) can shape their present and future behaviour through spontaneous self-organizing which is underpinned by a set of simple order-generating rules” (Burnes, 2005, 81) Nevertheless, if complexity theory considers organizations as CAS (Gell-mann, 1994) it seems essential to note, following Stacey (1996) and Chiva (2004), that human CAS have many distinctive characteristics in comparison with biological CAS. In human systems, the agents – individuals – are affected by emotions and feelings that influence interaction processes. The individuals are, besides, able to think in a systematic way, to prioritize their goals, or also for instance, to implement power strategies (Chiva, 2004). Thus, human CAS seems more complex than biological CAS. It is advisable to be prudent in the application of this theory to the organizations. So, the first step consists in checking the relevance of analogy between a CAS and the French Healthcare System. 9 3.1.3 CAS Transposition to French Healthcare System Cilliers (1998) defines many attributes characterizing the CAS. In introducing and detailing these main attributes, we will show why innovation processes can be perceived as a CAS and so, can be modelled with this theory. Table 1: Application of CAS theory to the French Healthcare System Large number of elements The French Healthcare System is made up of numerous agents (individual, groups and organizations) and is under the influence of numerous parameters These elements interact dynamically These agents (individual, groups and organizations) interact in order to develop their activities and to defend their own interests. Many interdependent actions combine in the French Healthcare System Interactions are non-linear Theses interactions are complex (actors’ games) and unpredictable by nature (the actions convergence is not predetermined) There are feedback loops in these interactions Interactions generate many feedback loops which allow agents to adapt their actions according to the actions of others. There is no global plan but a general interdependence of local plans. The system is open Agents seek information and knowledge in the French Healthcare System environment. They learn and adapt their behaviours according to variations of external environment. The system operates far from equilibrium The implementation and diffusion of innovation in the French Healthcare systems cause exploratory and chaotic behaviours, conflicting events and provoke a stage of disorder, situated far from equilibrium (Stacey, 1995). The system has history The French Healthcare system is embedded in a specific history and organizational culture. Agents implement the concept of innovation according to their particular context, i.e. social and institutional built. Source: Adapted of Cilliers, 1998. These different elements exhibits that the French Healthcare system model according to the CAS theory is perfectly conceivable. The system’s characteristics allow us to better understand the dynamic of innovation implementation and the emergent organizational change. In other words, to consider the healthcare organizations as professional complex adaptive systems (Anderson and McDaniel, 2000) is similar to an heuristic approach to explore the relationships between agents and their emerging patterns, in order to frame how to manage change and innovation. It seems, in fact, essential to focus on the relational network between the organizational agents and their mutual adjustments and interactions within the environment dynamics. 3.2 Implications to explore organizational change in French Healthcare System Ideas from the complexity theory emphasise on the emergent nature of change. Change comes from continuous interactions between the agents in the system (Brown and Eisenhardt, 1997). “Emergent change consists of ongoing accommodations, adaptations and alterations that produce fundamental change without a priori intentions to do so. Emergent change occurs when people re-accomplish routines and when they deal with contingencies, breakdowns, and opportunities in everyday work. Much of this change goes unnoticed, because small alternations are lumped together as noise in otherwise uneventful inertia…” (Weick, 2000, 237) In other words, change occurs spontaneously when connectivity and interdependence between agents (people and groups) are large enough. In this perspective, the management of change consists first on creating interdependences between actors and groups in order to foster a convergence of actions, a local coordination allowing self-organization of system. Accepting the principles of emergence and self-organization in the complex system leads to rejecting the logic of intentional change, global plan and top-down. Emergent change induces to develop skills of managing disorder and uncertainty as well as to encourage experimentation, diversity of views, creative actions, improvisation and deviant behaviours. The focus of organisational change interventions in a complex view moves away from ‘planning 10 change’ into ‘facilitating emergence and self-organization”. So, how fostering to self-organization is the complex system? According to Gell-mann (1994) self-organization occurs when the system stands at the edge of chaos. This stage of moderated instability or “creative destruction” encourages the appearance of emergent processes like change, creativity or innovation. This stage of ‘edge of chaos’ is facilitated by five factors (Eigen and Schuster, 1979 ; Juarrero, 1999 ; Kauffman, 1993 ; Ingber, 2000 ; Andriani, 2001) : 1) Multiple interactions between agents 2) Multiple interactions between agents and their external environment 3) Numerous information and knowledge flows 4) Large cultural diversity among agents 5) Equilibrium between formal and informal structures (of exchange) within organizational system After this explanation of theoretical foundations and of the PHR project, it seems that empirical study must search for answers to the following question: Do factors facilitating a state at the edge of the chaos, in the CAS theory, influence the organizational change required for implementing the PHR innovation in the French Healthcare System? In this objective, a qualitative methodology based on the single case of PHR has been designed. 4. Research methodology 4.1 Case study methodology This research intends to explore the process of innovation in the service relationship in the specific case of French Healthcare System. A single case study has been chosen in order to propose a depth investigation. According to Yin (1994), a single case may be relevant 1) to confirm or test a theory, 2) to represent a unique or extreme case or 3) to observe a phenomenon that was previously inaccessible to the academic community. In our research, this is the second situation that justifies the single case relevance. Yin (1993) identified three main types of case studies: Exploratory, Explanatory and Descriptive. The PHR case study is an exploratory one. This type of case studies can be considered as a prelude to some social research and data collection aims to precise the research questions. Moreover, an exploratory case study requires selecting the case according to the conceptual framework in order to maximize the research process and the relevance of first results. In parallel, our case study has been designed on a multi-level analysis: actors, groups of actors and the interaction between them (the system). Feagin, Orum, & Sjoberg, (1991) state that: a case study is an ideal methodology when a holistic or systemic view is required for understanding a social process. This implies to use multiple sources of data. In other terms, the case provides an exhaustive collection of data. The PHR case study allows us to examine the resistances and issues to change (linked to the innovation implementation in the French Healthcare System), and to identify the external and internal change drivers. 4.2 Data collection and analysis Case study research requires a delicate data collection to control the data authenticity. The PHR case study has been designed in using a combination of different collection methods (Stake,1995). We have made a qualitative investigation (Miles and Huberman, 1984). 11 First, the collection of primary data includes: - Centred interviews (20 interviews of one hour each) with the PHR keys actors. The healthcare experts interviewed were mainly: Information System Managers in public hospitals, Executive Managers of main structures in charge of the PHR implementation, Ministry of Health PHR project manager, heads of pilot department in the PHR experimentation, etc. - Non-participant observations, especially during the workgroup sessions of the PHR key actors. These meetings allowed monitoring the PHR experimentation and identifying the main issues of project. However, in most cases, these work sessions were not for the unique subject of the PHR, but more generally the computerization of public healthcare system. Second, we organized a collection of secondary data (Weick, 1993) through: - A set of strategic documents explaining the project stakes, the stages of implementation, the actors, the first lessons of experimentation, etc. These documents come from diverse sources: internal documents to PHR project, documents written by main pilot structures, strategic document of the Ministry of Health or the Parliament, etc. - A set of newspaper articles in periodicals, medical magazines, specialised press, etc. This collection method provides a data triangulation and a robust chain of evidence (Miles et Huberman, 1984). The data analysis had been a qualitative one through a thematic content analysis (Bardin, 2001) and had been achieved with the assistance of Nvivo (qualitative data analysis software) in order to organize the verbatim in categories of themes and under-themes. Our data analysis may be characterized as a method of categorical aggregation (Stake, 1995). 5. Research findings : the main points of blocking 5.1 Technical aspects 5.1.1 A lack of communication and a compartmentalization approach The PHR project represents for the hospital’s personnel (medical, paramedical and administrative) a new further project to carry out which adds to their workload. Moreover, the PHR is a legal obligation for hospitals and is like a constraint “for us it is impossible to free up time and staff to work on this new project”, said a manager hospital, “We already have important inner restructuring projects that mobilize some agents. Our challenge is to make coherent inner projects with national obligation projects”. This quotation raises two main problems of the PHR project. First, we can observe a lack of communication around the PHR. One of the actors interviewed who have taken part at the experimentation said “One of the main difficulties is the mobilization of personal and experimentation is very difficult to launch if you do not have a minimum of good will. The PHR project and more particularly the experimentation has been done in a confidential way without a real national communication campaign even though this step of the project could impact 3000 hospitals. ” In spite of the major stakes of the PHR project and the obligatory nature of the project, the numerous partners didn’t invest in communication campaign to mobilize hospital personal, to explain the project’s goal and perspectives to prepare and organize the implementation and the experimentation step. This confidential aspect poses a real problem in the project appropriation by everyone who has to act in it. Second, as the PHR project was not introduced for the personal, they do not realize the stakes and the extent of this innovation. This lack of communication makes tough the mobilization and creates a compartmentalization approach of the project. Each part tries to understand what is expected and how to integrate these new activities to the other or the PHR project is a transverse project with global finalities. “There is a hiatus between the global vision wished by the authorities and the work oriented vision of each actor.” 12 5.1.2 The illusion of the interoperability: “On the track of a standard…” At this time the PHR is not a sustainable and perennial tool. It is complicated to supply and a lot of technical aspects are still not solved. The main stake of the PHR project is the interoperability to provide a national healthcare record available in hospitals like in general practices and supplied by all the clinicians, to improve the health condition’s knowledge, diagnosis and to develop a data exchange. Today one of the problems is the national identification norm and compatibility of the formats between the hosts. Main actors of the PHR project neglected the reflection about the patient identification norm. A major part of the hospitals try to run over this problem, for example in a pilot site “We do not know everything about the PHR project. We know we have to be the best on the patient identification and on the professionals’ identification.” This quotation illustrates the problem of compartmentalization on the national territory and the lack of preliminary reflection, anticipation of the main technical problem. Another important obstacle is data security and confidentiality. According to an information system manager “One of the main problems is the identification and the confidentiality and security of the data contained in the PHR.” Some hospitals, not necessarily experimental ones, have foreseen the identification problem and have been forming alertness identification units. According to the security expert in the PHR project, it deplores the following; “We have had to standardize the identification methods before the launch of the project”. For another actor “The technical part [of the PHR project] isn’t complex because it is a high tech rather than because there is no standard to implement”. This absence of standard is emphasized by the multiplicity of hosts involved in the project. Indeed, six different hosts have been selected to develop software for this project. Actually, the project began too early, whereas experts didn’t deal with the main preliminary problems like the identification of patients and standard conceptions for national territory. This lack of preliminary work has been creating great confusion and a dilution of the PHR project goals. The question remains on how to share information between different hospitals through national territories with different hosts and different formats? How to promote interoperability where there is diversity and multiplicity of software and versions of the project? 5.1.3 A innovation project: the necessity of training for the change In spite of the numerous structures involved in this project, none of them have considered training for the change. No organized training to prepare personnel has been decided by the decision-making structures. In an experimental site, a manager has to organize training without taking time to prepare it: “We organized a part of the training for the physicians and it is a heavy step that we haven’t anticipated.” This time dedicated to the training organisation would have come to PHR project team because they hold competencies and knowledge to manage change. The PHR project would have required a national training plan to introduce a new culture around a specific population. Indeed, the project impacts medical personnel, clinicians and administrative agents and each group has its practices, habits and has to incorporate this new tool to their work. The information system manager of a French hospital noticed: “We are worried about how to inform administrative personnel of the necessity of accurate patient data collection. According to me it was of utmost importance before beginning the experimentation. Furthermore it is important to locate and to mark identification-high-risk units like emergency services where the identification patient is fussy.” Training for change represents a strategic step in the implementation of this kind of innovation in the service relationship. PHR project’s owner would have had to create training sessions for different populations involved and diffuse the computerization culture not only to the experts like information system manager but also to the other levels of hospitals. French hospitals are bicephalous, composed of medical personnel (paramedical, physicians…) and administrative agents who often have bureaucratic practice. It is necessary to coach the change to restrict resistances to the change. 13 5.1.4 The PHR project: a new workspace The implementation of new software modifies work conditions and requires a specific acquisition of new reflexes and new behaviour. In contact management, agents are stressed and submitted to an important uncertainty (De Bandt and Gadrey, 1994). The setting up of a new technological tool represents a supplementary stress for them. To deliver a service relationship in good conditions the agents need to control their workspace. The set up of new software means for agents a new stress to manage and they need time to be self-confident when they work with this new technological tool to give information to people or to answer their questions. The software is considered like a support, a mean to be more efficient when agents inform users. If it becomes unfriendly, it modifies the way service relationship is delivered and users begin to complain. The PHR project represents a modification of the technological workspace of agents, not only for paramedical and medical staff but also for the administrative part like the hostess at the front desk and administrative entrance where patients have to present paperwork for the healthcare insurance and mutual company. “This category of agents is a small and very delicate group. When something is changed in their workspace it is essential to explain the reasons and the benefits for their everyday labour. Otherwise, they have the ability to go on strike since they are unionized.” 1 This extract shows the specificity of contact agents who work in an unsure environment and how the smallest change in their environment creates a stress and may disrupt all of the hospital management by producing sick leaves or a strike. We can suggest working in task groups with concerned agents to present the PHR project and the impacts of this project on the work conditions. We consider this is not a training phase or an information step but a specific communication dedicated to the contact agents who have to represent the hospital in front of users and patients. This suggestion concerns the ergonomic aspects in the PHR project. When we modify the workspace we change marks and for some agents it corresponds to an additional stress in their workspace. 5.2 Cultural aspects 5.2.1 For the clinicians The PHR project modifies the medical and the clinician’s culture. People are accustomed to thinking of clinicians as wise men who are able to cure all illnesses. They are considered like a God who holds the supreme knowledge and is able to control life and death. In their diagnosis clinicians are aware of this authority and are the owners of their diagnosis and of their data. First because they use jargon and make decisions for which they are responsible and second because as usual the clinician keeps his memorandum and the patient examinations in his practice. The PHR project transfers the authority of the patient data from the clinicians to the patient himself. With this centralization of the health data in a virtual space, the patient becomes the owner of his health condition. Symbolically the clinician loses the control of his knowledge, his expertness and especially of his data. Moreover, the PHR changes the patient into a client who can compare the diagnosis between different clinicians. Clinicians have to not only write the diagnosis and their memorandum in the PHR but also make it public so that another clinician can read and reconsider it. This sharing of the diagnosis is a revolution in the field of medicine. Another aspect in the PHR project is the possibility for the patient to hide information. This functionality allows the patient to hide some data from clinicians, which can be very dangerous for their diagnosis as they need all the information in order to make vital decisions. This revolution in the positioning of the clinicians is not considered by the managers of the project groups. This cultural change needs to be presented to the clinicians because they may be resistant to this project. For example, the results of the first experimentation show that only 23% of the clinicians declared to sustain the PHR. One of the perspectives to consider for the PHR managers is to give value to the medical stakes of the PHR program for the clinicians to obtain a conjunctive involvement from hospital clinicians and city clinicians. 1 IS manager of a Public Hospital 14 5.2.2 For the medical staff The PHR represents “another form”, even though it is digital, to fill out by the medical staff. It corresponds to a bureaucratisation of their job. French nurses complain of numerous documents they have to fill out when they take care of the patients and according to them this bureaucratic aspect of their job is at the expense of the human aspect of it. Moreover, the nurses have evolved in an oral culture. In the hospital units they have some staff meetings to inform the night team and the day team about the patients’ conditions. With the set up of the PHR, nurses will have to write with precision and to develop their written culture. “One of the bigger problems of the PHR implementation is not the technical aspect but the supplying. This part of the job concerns the medical and paramedical staff for the medical aspect as well as the administrative agents for the administrative part. 2” The transition from an oral culture to a written culture represents an important change in the work routine of the nurses as with the PHR they now are supposed to be conversant not only with people but also with the software. Unfortunately we can observe that “clinicians and administrative managers are involved in the PHR experimentation but nurses and administrative agents are reluctant and very cautious. They grasp the PHR like an overburden in their daily work and not like a tool.” 3 This quotation underlines the lack of communication about the PHR and the cultural change that the PHR represents. Another IS manager of a public hospital adds “We are conscious of the circulation issues because we are working on them but the medical and paramedical staff do not take part in these brain-trusts.” Finally we can notice that the PHR project managers did not consider the diversity of the cultures that coexist in the hospital and adopted a point of view that corresponds to their approach. In spite some efforts to involve clinicians and medical personnel, the PHR project conception remains an IS project that complicates the cultural integration for the “non-specialists”. We can observe that the large majority of the persons involved in the PHR project come from an information system culture and are used to set up this kind of project but they are not able to translate the technical aspects into medical or administrative stakes. The PHR implementation difficulties indicate the cultural gap or the “cultural shock” between nurses who want to stay with the patients to take care of them, clinicians who want to be owner of their diagnosis and their expertness and the administrative agent who want easy software to type in patient information. This centralization of the health information disturbs the habits and culture of each part and gives patients ownership over their body and information about their health condition, without the knowledge. 5. 3 Project Management issues Some aspects of Project Management equally increase the resistance to change of healthcare actors. We present, in this second part of the results, the three main dimensions linked to PHR project management and we show how these block the PHR process deployment and could cause the future failure of this innovation. 5.3.1 The lack of Interests Diversity Management The French Healthcare System is made up of a multitude of actors, groups and institutions with different interests and strategies. Implementing a radical innovation needs to manage this diversity of interests reflecting various cultures, professions, expertise, etc… especially when it concerns an Information System Project with a transverse perspective. In PHR´s case, GIP-DMP did not take into account this diversity in the project management. The different categories of health actors have practically never been associated in the project conception although this stage is essential to obtain 2 3 Executive Manager of the MAINH (the National Support Mission of Health Investment.) IS manager of a Public Hospital. This hospital took part of the experimentation step. 15 actors’ support and mobilization. According to MAINH 4 representative: “There are different professional views about this project as PHR integrates objectives and speeches that, in the short term, appear antinomic. Today, we take orientations that leave numerous questions in suspense.” The main interest in the diversity approach for the PHR concerns the duality: cost/quality. For Government, Social Security and health insurances, PHR represents an opportunity to structurally change the health system in order to make it more effective and efficient. In other terms, PHR replies to a “productive requirement” of cost savings. For patients and health professionals PHR should improve the coordination of medical care as well as the general quality of care. PHR, in this logic, is similar to an information exchange support allowing the development of communication networks between health professionals and the continuity of cares between several health establishments. The aim is to create collaborative informal networks operating on horizontal communication. We could qualify this second approach of “sharing logic”. These two points of view seem in complete opposition and block the PHR deployment. “Today clinicians suspect the general strategy of cost reduction behind PHR and block its diffusion. Some criticize the project in public meeting, in press and in their institution or in front of the patient.” 5. The economic perspective of PHR aiming to control the costs of health services is perceived by clinicians as a monitoring of health activities and a control method of daily practice. It reflects a top-down perspective of implementation: PHR is “a centralized proceeding of medical work which must increase our productivity”6. Moreover, this predominance of cost savings logic causes another problem: the one of PHR inadequacy with medical practice which reinforces the resistance to change of liberal and hospital clinicians. If naturally the financial interest of PHR seems particularly interesting in view of the health system’s current spending, this one can not justify the project validity for health professionals and for patients. PHR implementation requires health professionals’ adhesion about its prior objectives. For the time being, we are far from that and the dialogue does not seem to be in search of it. To illustrate this difficulty, the “Midi-Pyrénées” regional union of liberal clinicians removed itself from PHR experimentation because it considers that its advices were not taken into consideration by the heads of the project. To overcome these difficulties, it seems essential that GIP-DMP associates more with the different health actors involved in PHR implementation in order to obtain a dialogue about PHR objectives and consequently the mobilization of the health system. Through the setting up of PHR team project, it appears necessary to gather, as much as possible, the different professional cultures (clinicians, auxiliary nursing staff, administrative staff, IS staff, executive staff, etc.). The aim is to create value through the diversity of culture, profession, practice, expertise, etc. The contradictory logics and the tensions linked to interest diversity could be beneficial to innovative and performance approaches around PHR if different views of information and collaboration are organized and are anticipated in the project management (Andriani, 2001, Habib, 2006). For the time being, in the complex health system, the diversity of interests seems to block change because it is not managed at the different levels of project action. 5.3.2 The “blurred contour” of PHR Project The second dimension that causes problems to PHR innovation is the lack of delimited contours to the project. We observe through the analysis of experts’ interviews that PHR project mingles with other projects associated to strategic axis of healthcare organizations’ computerization. By the way of illustration, the Information System Managers of Public Hospitals merge in practice PHR project with the issues of Emergency Computerization, Interoperability IS, Vital card new generation 7, Health Professional Card, Patient or Professional Identification, etc. In other terms, the content of PHR project being not clearly defined, the key actors involved do not know how tackle PHR project. “In my hospital, we have decided to approach PHR with the Professional Identification issue. We are aware of limits of this scope but the priority lines of PHR are not explicit”8. “In terms of regional objectives, this is not clear. We are some difficulties to grasp the coherence of planed actions. We wish to know the prior 4 The MAINH is the National Support Mission of Health Investment. This organization is a support structure that supports central administration and the cabinet of ministry, ARH and hospitals. The latter is accountable of animation, consolidation of data and communication. 5 Executive Manager of GMSIH (the Organization for the Modernization of French Hospital Information Systems) 6 Extract of interview with a hospital clinician. 7 Vitale card is an electronic claims submission consisting to simplify and accelerate exchange between health care professionals, patients and health insurance. 8 IS manager of a Public Hospital 16 aims. During the meetings of ARH9, this one evokes several aims, several questions, several solutions … but we do not know what the immediate target is: The PHR or more simple things like the health network?”10 This lack of Project delimitation is also underlined by a Senate Report in 2007 which reveals that the main piloting authority, The PHR project owner (GIP – DMP), can not yet answer to essential questions about PHR: What is the PHR content? What must be the operating principles (local, regional or national)? What is the global cost? What is the PHR cost for the main actors and structures of healthcare system, etc…? This “deliberate vagueness” gives the feeling to the expert interviewed that “the PHR for the time being is only in the speech”. This feeling is reinforced by the unrealistic planning of PHR actions which set the PHR generalization in July 2007. This produces multiple local actions without coordination and leads, in some cases, to the demobilization of key actors’. Besides, it seems important to consider that PHR for health organizations is similar to an external project that is a governmental requirement. With very few exceptions (i.e. the cancerology institutions), PHR is not necessarily in observance with the general strategy of health organization and especially with the program of computerization. This implies that there is not an automatic convergence with internal or local projects. Thus we observe a duality between these two perspectives: external vs. internal projects and top-down vs. bottom-up approaches. Often in the cases studied, we note that local actors give preference to local projects of computerization (notably because theses projects are financed on their own budget) and neglect the national PHR project. If the PHR project was better delimited and the prior objectives more clear, it seems that local actors could integrate PHR easier in their local initiatives. “We wish to transform the top-down approach of PHR into an assistance to our local projects but at the present time we do not know how realize it. The content of the PHR project is too vague.”11 In terms of managerial implications, it appears that the PHR project must clarify its prior objectives to facilitate the local initiatives in order to focus on the same objective (convergence of local initiatives) and to avoid the demobilization of health actors. Moreover, it seems interesting that piloting instances take into account these dualities - external vs. internal – top-down vs. bottom up – because the PHR project can not be implemented as a law. This important IS project requires transversal approaches and participative management at each level of action. 5.3.3 The failings of Piloting Several problems of piloting now obstruct the deployment of PHR. We intend, in this part, to explain why the current piloting of the project is not adapted to the IS project implementation and to enhance some possible solutions. First, we remark that too many structures are implicated at the central level in the PHR project and its piloting. For example, at the governmental level, four ministerial directions – “hospitalization and cares direction”, “Social security direction”, “health direction” and “research direction” – intervene in the PHR project management. Each direction has created a “PHR cell” and leads its own actions without coordination with the other directions. That is explained largely by the traditional competition between these ministerial directions. It is the same logic for the structures involved directly in the PHR deployment – Mainly the GIP-DMP (PHR project owner), the MAINH (National Support Mission of Health Investment) and the GMSIH (Organization for the Modernization of French Hospital Information Systems). If these structures have officially definite missions, nevertheless in reality they act in similar directions and develop a large confusion about the piloting organization. “It is difficult to understand the role of each institution. For example, last week I was present at two meetings with the same actors. First a meeting about the emergency computerization project (which is managed at central level by the MAINH and the GMSIH and at regional level by the ARH) and second a meeting about PHR experimentation with the same partners. More or less the two meeting revolved around the same subjects.”12 The analysis of expert interviews reveals the stacking of structures without clear functions and missions, the lack of continuity between these central structures of piloting (ministerial directions and PHR structures), and the responsibilities are weakening. Generally speaking, we observe the absence 9 Regional Agency of hospitalization IS manager of a Public Hospital 11 IS manager of a Public Hospital 12 IS manager of a Public Hospital 10 17 of structure having a sufficient visibility to pilot the project in a general view and to assure the coordination of local actions about PHR or its key axis. At the regional level – intermediary programming –, we note the absence of regional instance to federate the local initiatives. For the time being, the PHR management does not plan the regional piloting. In some regions, the ARH (Regional Agency of Hospitalization) that plays the role of coordinator but the implication of this structure differs from a region to another. In other cases, the local health networks assume the coordination role. At last, in other regions, no other structure invests in this mission. The absence of a regional reference poses mainly a problem in terms of knowledge mutualization and synergy effects between the local structures embedded in the PHR experimentation. Without coordination, the local structures can not exchange information and expertise about the project. And that is all the more prejudicial with the absence of PHR project prior objectives and the investment realized by local structures in different axis of PHR. Several actors interviewed speak about “a wasting of resources, means and energy”. Finally, at the local level, the GIP-DMP has chosen to base essentially the PHR experimentation and generalization on the university hospitals in neglecting the mobilization of the small public health organizations and the liberal health professionals. If this option can be justified in relation to the PHR technical difficulties and the implication need of structures with a high level computerization and IS expertise, it is not necessarily the best choice to create a participative local dynamic around PHR. Indeed, the interviewed experts underline the difficulty for hospital clinicians to invest time in the communication and/or creation of a PHR. Thus, the non-association of small public structures and liberal clinicians blocks the process of PHR. Notably because these actors could play an important role in terms of communication with patient and the opening of records and more largely in the change process of health complex. The entirety of these piloting problems reflect a lack of interactions between actors implicated in the PHR project at each level of action (central, regional and local) and between these different levels. The lack of interactions – in internal as well as in external – do not allow the information and knowledge exchange required to develop the PHR project. At last, the main structures of piloting approach the project with an inefficient top-down management that does not authorize a balance between formal and informal structures. These located elements, according to the CAS theory (Eigen and Schuster, 1979; Juarrero, 1999; Kauffman, 1993; Ingber, 2000; Chiva, 2004), block the “edge of chaos” phase and the deep change process needed by PHR deployment. To favour the change linked to PHR, we suggest the following axis: - - - At the central level, it seems relevant to reinforce the visibility of the project owner (GIP-DMP) so that a unique central structure pilots the PHR. In this end, we recommend the creation of PHR team project common to GIP-DMP, GMSIH and MAINH and which integrates the key actors of central directions. This team project, attached to GIP-DMP, could be a legitimate instance of PHR piloting. At the regional level, it appears interesting that a structure federates the local initiatives. However, the analysis shows that there is no preferential regional structure (ARH, University Hospitals, Health network) to assume this responsibility. Besides, if some experts pointed out the ARH for this mission, it seems difficult to constrain the implication of AHR in PHR project management. To remedy the regional piloting problems, we advise that in each region the GIP-DMP team project appoint a regional representative in charge of the creation of a regional committee project. This committee, in associating the representatives of the main heath actors13 implicated in PHR deployment, could facilitate a participative project management, reinforce coordination and expertise exchange between local actors as well as between them and central actors, and increase synergy effects. At the local level, it seems judicious to initiate a dynamic of actors’ interdependencies through a better role sharing and the association of a large majority of health actors. In a similar perspective we suggest the creation of local project committees (in coordination with the regional committee) in order to incite the local health actors’ mobilization and to organize the main PHR actions in the territory. The aim is to favour the emergence of local actors’ network and of the dynamic of implication. 13 Representatives of ARH, University Hospitals, Public and Private hospitals, health structures, liberal clinicians, auxiliary nursing staffs, administrative staffs, chemists, Patients’ associations, etc. 18 These elements should be accompanied by a general communication about PHR. Indeed, for the present time, no communication campaign around PHR has been realized towards health professionals and patients. Now without communication about PHR (its stakes, its benefits, its content, the patients’ right, the role of health professionals, etc.), the dynamics of mobilization needed to PHR deployment seems difficult to emerge. Figure 1 : The Piloting of PHR Local committee Local committee Local committee Local committee Local committee Local committee Local committee Local committee Local committee Local committee Regional committee of PHR project Regional committee of PHR project Representatives of regional health actors Representatives of regional health actors PHR team Project Common to GIP-DMP, GMSIH, MAINH and ministerial directions Regional committee of PHR project Regional committee of PHR project Representatives of regional health actors Representatives of regional health actors Local committee Local committee Local committee Local committee Local committee Local committee Local committee Local committee Local committee Local committee These suggestions could move PHR deployment from a top-down to a bottom-up approach, increase the interactions at all actions level and between each of them and integrate the key conditions of change in the complex health system. In fact, the findings are consistent with the suggestions coming from the CAS approach which looks at the healthcare system as a complex adaptive system. Thus, the change required by PHR deployment should be managed in a participative and dynamic way with a particular focus on: the diversity of actors involved, the multiplication of interactions and information 19 flows and a balance between formal and informal structures of exchange. About this last point, the PHR piloting through the creation of team or committee projects at each action level seems particularly well adapted to respect this balance and foster the success of innovation diffusion. Conclusion The PHR project is a national project which concerns every public hospital. This project aims to make easier the generalization of the computerization in the health sector. The main objective is to centralize the health information in a single file which gathers all the medical information and medical examinations. This new way to collect information represents a real revolution in the clinician’s culture and more particularly in the way to consider the patient and the clinicians. We may name this a cultural revolution because the PHR project corresponds not only to a change in the way to manage the service relationship in the health sector but also in the way to approach the physical relationship to the medical practitioner. Furthermore, we should point out here the passage from a bureaucratic approach of data processing to a ‘pure’ information system approach. However, the experiment and the conviction that the logic of the project management is most effective in such a context haven’t specifically guided the experimentation step of the project. A specific project management is more adapted to this kind of information system project. This project approach is better adapted to the context and the technical constraints specific to the management of the information systems, however, the PHR project concerns all the French population and not a specific population. Project management and training are the main axis to implement a major scale project as the PHR. The transition and the change from an all powerful clinician to a diagnosis shared between clinicians needs a specific organization to change management and mobilize key actors. The diversity of the professional culture is one of the neglected aspects which raise the complexity to find an agreement between the different actors and their own logic and interests about the kind of information that they have to supply the PHR. Even if all the actors of this project pursue the same goal: to provide the best possible service to the users. To achieve this goal each part looks to protect its interests (work conditions, power, workload…). This compartmentalization is the result of a lack of communication and a lack of consistency in the project management. Implementation of a new tool is always viewed as a revolution, when it concerns health in a public context founded in bureaucratic culture, the change management and the research of sense for each part of the project is essential to the achievement of it. 20 References Anderson, P. (1999 ), “Complexity theory and organization science”, Organization Science, Vol. 10, pp.216-232. Anderson R.A. and McDaniel R.R. (2000), “Managing health care organizations : Where professionalism meets complexity science”, Health Care Management Review, Vol 25, n°1, pp.83-92 Andriani, P. (2001), “Diversity, Knowledge and Complexity Theory: Some Introductory Issues”, International Journal of Innovation Management, Vol.5, n°2, pp.257-274. Baets, W. (1998), Organizational learning and knowledge technologies in a dynamic environment, Kluwer Academic Publishers, Dordrecht. Bardin, L. (2001), L’analyse de contenu, Paris, PUF. Boisot M.H. and Child J. (1999), “Organization as Adaptive Systems in Complex Environments: The Case of China”, Organization Science, Vol.10, n°3, pp. 236-252. Brown, S.L. and Eisenhardt, K.M. (1997), "The art of continuous change: linking complexity theory and timepaced evolution in relentlessly shifting organizations", Administrative Science Quarterly, Vol. 42, n°1, pp.1-34. Burnes, B. (2005) "Complexity Theories and Organizational Change" . International Journal of Management Reviews, Vol. 7, No. 2, pp. 73-90, June 2005 Carlisle, Y.M., McMillan, E. (2006), “Innovation in organizations from a complex adaptive systems perspective”, Emergence, Complexity and Organizations, Vol. 8, n° 1, pp. 2-9. Charreire S. (2003), “Les innovations en tant qu’objets d’apprentissage organisationnel : une mise en perspective“, XIIème Conférence Internationale de Management Stratégique, AIMS. Cheng, C. and Van de Ven, A.H. (1996), “Learning the Innovation Journey: Order out of Chaos”, Organization Science, Vol.7, n°6, pp.593-614. Chiva, R. (2004), “Repercussions of complex adaptive systems on product design management”, Technovation, Vol. 24, pp. 707-711. Cilliers, P. (1998), Complexity and Postmodernism: Understanding Complex Systems. London: Routledge. Daft, R.L. 1978, "A dual-core model of organizational innovation", Academy Of Management Journal, Vol 20, pp.193-211. Damanpour, F. and Evan, W. M., (1984), "Organizational innovation and performance: the problem of organizational lag", Administrative Science Quarterly, Vol 29, pp.392-409. Damanpour F. (1996), “Organizational complexity and innovation : developing and testing multiple contingency models”, Management Science, vol. 42, n°5, may. David, A. (1996), “Structure et dynamique des innovations managériales”, Cahier de Recherche du CGS, n°12, Juillet. De Bandt, J., Gadrey, J.,(1994), Relations de service, marchés de services, CNRS. De Sanctis, G., Fayard, A-L., Roach, M., Jiang, L. (2003), “Learning in online forums”, European Management Journal, Vol. 21, n° 6, pp 565-577. Eigen, M. and Schuster, P. (1979), The hypercycle: a principle of natural self-organization. Springer-Verlag, Heidelberg. Eiglier, P., Langeard E., (1988), Servuction : le marketing des services. Editions Mac Graw Hill, Collection Stratégie et Management. Eisenhardt, K.M. (1989), “Building theories from case study research”, Academy of Management Review, vol. 14, pp.532-550. Feagin, J., Orum, A. and Sjoberg, G. (1991). A case for case study. Chapel Hill, NC: University of North Carolina Press. Gell-Mann, M. 1994), The Quark and the Jaguar - adventures in the simple and the complex, Brown and Co.,London. Goffman, E. (1961), Asylums: Essays on the Social Situation of Mental Patients and Other Inmates. New York, Doubleday. Habermas, J., (1981), Theorie des kommunikativen Handels ; traduction française : Théorie de l’agir communicationnel, Habermas, J., (1997), L’espace public, Payot, Paris. Habib J., (2006), “Diversité(s) & Innovation : explorer le lien entre la diversité et l'innovation, l'apport du paradigme de la complexité“, Deuxième rencontres internationales sur la diversité, IAE de Corte, France, Octobre 2006. Habib J., (2007), “La dynamique des trajectoires de connaissance dans un projet d’innovation : Analyse comparative de deux études de cas de projets d’innovation dans le secteur public“, Conférence annuelle de l’Association Information et Management (AIM), Lausanne, Juin 2007. Harkema, S.J.M. (2004), Complexity and emergent learning in innovation projects, Veenendaal: Universal Press Holland J. H. (1995), Hidden Order: How Adaptation Builds Complexity, MA: Addison-Wesley. Ingber D.E. (2000), “The origin of cellular life”, Bioessays, Vol 22, pp.1160-1170. Jeannot, G., Joseph, I., (dir), (1995), Métiers du public : les compétences de l’agent, l’espace de l’usager. Johannessen, J-R, Olsen, B. and Lumpkin, G.T. (2001), “Innovation as newness: what is new, how new, and new to whom?”, European Journal of Innovation Management ,Vol, 4, n°1, pp 20-31 Juarrero, A. (1999), Dynamics in action: Intentional behaviour as a complex system. Cambridge, MA: MIT Press Kauffman, S. (1993), The Origins of Order: Self Organization and Selection in Evolution, Oxford University Press, Oxford, U.K. Lorenz, E. N. (1963), “Deterministic non-periodic flow”, J. Atmos. Sci., Vol 20, pp130-141. 21 McKelvey, B. (2004), “Complexity science as order-creation science: New theory, new method”, Emergence , Vol. 6, n°4, pp. 2-27 Miles, M., & Huberman, M. (1984). Qualitative data analysis: A source book for new methods. Beverly Hills, CA: Sage Publications. Prigogine I. and Stengers I. (1984), Order Out of Chaos: Man’s Dialogue with Nature, NY: Bantam books. Ruelle, D. (1991), Hasard et Chaos. Editions Odile Jacob. Stacey R.D. (1993), “Strategy as order emerging from chaos”, Long Range Planning, Vol. 26 , n°1, pp.10–17. Stacey R.D. (1995), “The Science of Complexity: An Alternative Perspective for Strategic Change Processes “ Strategic Management Journal, Vol.16, n°6, pp. 477-495. Stacey R. D. (1996), Complexity and Creativity in Organizations. Berret-Koehler Publishers, San Francisco. Stake, R. (1995). The art of case research. Thousand Oaks, CA: Sage Publications. Temri, L., (2000), “Les processus d’innovation : une approche par la complexité“, IXème conférence Internationale de Management Stratégique, AIMS. Thiétart, R.A. and Forgues, B. (1995), “Chaos theory and Organization”, Organization Science, Vol.6, n°1, pp.1931. Thiétart, R.A., (2000), “Management et complexité : Concepts et théories“, Cahier de recherche DMSP, n°282, Avril. Ughetto, P.& al, (2002), « La relation de service : une tension vers un nouveau modèle de travail ? », IRES review, vol.39 n°2. Van de Ven, A. (1986), "Central Problems in the Management of Innovation", Management Science, vol. 32, n° 5, may. Van de Ven, A., Angle H.L., Poole, M.S., and Alii (2000), Research on the Management of Innovation, The Minnesota Studies, Oxford University Press. Yin, R. (1993). Applications of case study research. Newbury Park, CA: Sage Publishing. Yin, R. (1994). Case study research: Design and methods (2nd ed.). Thousand Oaks, CA: Sage Publishing. Weick, K. E. (1993), “The Collapse of Sensemaking in Organizations: The Mann Gulch Disaster”, Administrative Science Quarterly, Vol 38, n°4, pp.628-652. Weick K.E. (1995), Sensemaking in Organizations, Thousand Oaks, Sage. Weick, K.E. (2000), “Emergent change as a universal in organizations”. In M. Beer and N. Nohria (Eds.), Breaking the code of change (pp.223-241). Boston, MA: Harvard Business School Press. Weller, J-M., (1998), « La modernisation des services publics par l’usager : une revue de la littérature (19861996) », Sociologie du travail, n°3, pp.365-392. Weller, J-M., (1998), « Abuse-t-on de la notion de relation de service ? », Education Permanente, n°137) Editions Fayard. 22