pathology of esophagus
advertisement

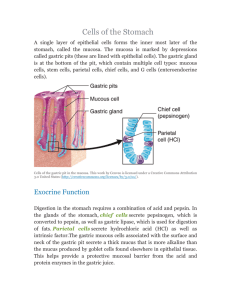
PATHOLOGY OF THE GASTROINTESTINAL TRACT 1 PATHOLOGY OF ESOPHAGUS Clinical signs of esophageal lesions: -dysphagia- means difficulties in swallowing. Most diseases of esophagus cause dysphagia -retrosternal pain = heartburn-commonly occurs when acidic gastric juice refluxes into the esophagus -hematemesis= vomiting of blood 1) CONGENITAL ESOPHAGEAL DISORDERS: -tracheoesophageal fistula- is the commonest congenital anomaly of esophagus abnormal communication between the trachea and esophagus -clinical findings- cyanosis, respiratory distress- surgery needed -esophageal atresia- very rare, narrowing or obstruction of a part of esophagus 2) INFLAMMATORY LESIONS OF THE ESOPHAGUS: -reflux esophagitis ( peptic esophagitis) caused by reflux of acid gastric juice into the lower part of esophagus -symptomatic esophagitis occurs when normal mechanisms of clearing the esophagus are impaired (even in normal individuals without clinical signs of esophagitis- some reflux occurs, but in normal persons- any fluid regurgitated into the esophagus is rapidly returned to stomach by peristalsis) causes of reflux esophagitis -impairment of peristalsis- may cause symptoms of reflux esophagitis -composition of regurgitated gastric juice- higher levels of acids and enzymes, as well as the presence of bile and pancreatic enzymes -relation to hiatal hernia- is not clear hernia is defined as protrusion of part of stomach through the diaphragmatic hiatus pathology: superficial erosions of the mucosa of lower esophagus- peptic ulcus and fibrous narrowing of esophagus histology: hyperplasia of the basal cells of the squamous epithelium and presence of neutrophils in the epithelium clinically: low retrosternal sensation of burning pain called "heartburn" -in chronic cases- the pain may be constant and is accompanied by dysphagia -Barrett's esophagus -intestinal metaplasia of the epithelium of lower part of esophagus, presence of gastric mucosa of cardial type is normal within lowest 3 cm of esophagus 1 -primary adenocarcinoma of esophagus may arise in Barrett's esophagus or peptic ulcer may appear -infectious esophagitis infections of esophagus are rare, except of in immunocompromised patients (AIDS, patients receiving anti-cancer therapy), esophagitis is most commonly of fungal origin-candida albicans -esophageal candidosis caused by Candida albicans, it is most common opportunistic infection morphology: the yeasts infect superficial layers of the epithelium- the surface is covered by white plaques - grossly visible, composed of cellular debris, inflammatory cells and fungi -viral esophagitis common in AIDS- intranuclear inclusions and occurrence of herpetic giant cellscaused by herpes virus, other type is cause by cytomegalovirus- infects submucosal endothelial cells- necrosis, hemorrhage, inflammation 3) FUNCTIONAL DISORDERS OF ESOPHAGUS -Plummer-Vinson syndrome consists of severe iron-deficiency anemia, koilonychia, atrophic glossitis and dysphagia-results from the atrophy of pharyngeal mucosa, increased risk of development of squamous cell carcinoma of tongue, esophagus and pharynx -more common in women, -dysphagia is corrected if the iron-deficiency is treated -achalasia of the cardia -congenital, the cause is unknown -”achalasia” means failure to relax- the cause of the disorders lies in the lack of ganglia in the myenteric plexus- this results in failure of peristalsis- the cardiac sphincter does not relax- the esophagus dilates massively and becomes elongated -the patients present with dysphagia, retrosternal pain, vomiting, predisposition to cancer possible complications: reflux of the contents into the trachea- aspiration pneumonia- lung abscess formation treatment: myotomy and repeated dilatation of cardia -esophageal diverticula diverticulum- outpouching of the lumen outside the wall -pulsion diverticulum- occurs when internal pressure forces an epithelial sac out through weakened muscle layer -traction diverticulum- are due to external infiltrative processes- accompanied by fibrosis of periesophaeal tissue -esophageal varices occur in lower esophagus and in gastric fundus in patients with portal hypertension- most common cause is liver cirrhosis 2 morphology: dilated veins in submucosa may rupture- severe hemorrhage (hematemesis, melena) -Mallory-Weiss syndrome -patients with prolonged vomiting (pregnancy, alcoholism)- longitudinal tears in mucosa of the lower part of esophagus- hematemesis occurs TUMORS OF ESOPHAGUS 1- Carcinoma -accounts for over 95% of all malignant tumors of esophagus -it is highly lethal-more common in old persons etiologic factors: cigarette smoking and chronic alcoholism increase the risk of carcinoma premalignat conditions: include- Barrett's esophagus and Plummer-Vinson syndrome gross appearance of carcinoma: plaque-like thickening of the mucosa with ulceration- stricture or narrowing of the lumen microscopically: over 90% are squamous cell carcinoma - adenocarcinoma is less common- it arises in mucosal glands or in Barrett esophagus spread of carcinoma through the esophageal wall- invasion of bronchial walltracheoesophageal fistula -invasion of the aorta may cause massive fatal bleeding lymphatic spread-is very rapid, through the lymphatic capillaries in the submucosa- lymph node metastases bloodstream spread- metastases to the liver and the lungs clinically: most patients present with dysphagia abd pain, severe weight loss, anemia-due to chronic bleeding prognosis is poor 2- other tumors of esophagus- are rare, include leiomyoma-benign, derived from smooth muscle malignant- lymphoma, melanoma have been reported PATHOLOGY OF THE STOMACH Clinical manifestations of gastric diseases: -pain and dyspepsia-pain is a feature of acute gastritis and peptic ulcer disease -pain is often accompanied by nauses and vomiting dyspepsia- includes pain, distension and eructation -loss of apetiteloss of desire for food is called anorhexia -it occurs in gastritis and gastric cancer 3 -bleedingbleeding into gastric lumen is a common manifestation of gastric diseases with mucosal erosions and ulcers -when bleeding is rapid- the patient vomits bright red blood = hematemesis -when bleeding is less rapid-blood is altered, it passes through the intestine, produces black colour of the stools = melena chronic slow GIT bleeding results in iron-deficiency anemia -palpable mass in the epigastrium NON - NEOPLASTIC DISORDERS OF THE STOMACH 1) Congenital pyloric stenosis one of the most common congenital disorders of GIT, this disorder affects males four to five times more often than females -marked hypertrophy of pyloric sphincter results in obstruction of gastric emptying symptoms- 1-2 weeks after birth- projectile vomiting after feeding treatment: surgical muscle splitting is curative 2) inflammatory lesions of stomach- gastritis Gastritis is simply defined as inflammation of the gastric mucosa, inflammation may be predominantly acute (neutrophilic leukocytes), or chronic (lymphocytes and plasmacytes) 1- Acute gastritis -is an acute mucosal inflammatory process of transient nature, may be accompanied by hemorrhages- severe form of acute erosive gastritis may cause acute GI bleeding grossly: affected mucosa shows red colour, erosions, and hemorrhages microscopically: hyperemia, edema, leukocytic infiltration of the lamina propria etiologic factors: the pathogenesis is poorly understood, acute gastritis is frequently associated with: Heavy use of nonsteroid anti-inflammatory drugs, such as aspirin, excessive alcohol consumtion, heavy smoking, treatment with anti-cancer drugs, uremia, systemic infections, such as salmonelosis, viral infections,severe stress, ischemia and shock, gastric irradiation, etc. It must be emphasized that some patients have idiopathic acute gastritis without any associated disorder -decrease of resistence of gastric mucosa may be caused by the following reasons: -1- inhibition of prostaglandin secretion- (smoking, aspirin, anti-inflammatory drugs) -2-interference with mucosal regeneration - (antimitotic drugs) -3- ischemia- decreased mucosal blood supply plays a role in development 4 of gastritis associated with shock clinically: clinical course depends on the severity of anatomic changes-epigastric pain, nausea, vomiting, anorrhexia occur in moderate degree of gastritis -endoscopic and microscopic changes are minute -in more severe types- massive hemorrhages, hematemesis, and potentially fatal blood loss- in alcoholics 2- Chronic gastritis chronic gastritis is defined as the presence of chronic mucosal inflammatory changes leading possibly to mucosal atrophy and epithelial metaplasia, chronic gastritis is notable for distinct causal subgroups with different location, histology and clinical features. Pathogenesis: the major etiologic associations of chronic gastritis are as follows Immunologic, associated with pernicious anemia, chronic infection, caused by Helicobacter pylori, toxic, as with heavy smoking and alcohol consumption postsurgical, especially following antrectomy and gastrectomy with reflux of bilious duodenal secretions granulomatous conditions, such as in Crohn disease miscellaneous- GVHD, uremia, etc. Basically, three major types of chronic gastritis can be distinguished: Type A gastritis -associated with pernicious anemia -involves mainly fundus and body -is of autoimmune origin- antibodies to parietal cells- is characterized by hypochlorhydria or achlorhydria (decreased acid secretion) resulting from parietal cell destruction, up to 60% patients have decreased production of intrinsic factor- leading to failure of vitamin B12 absorption and development of pernicious anemia on endoscopy: gastric mucosa is atrophic, appears markedly thinned histologically gastric mucosa shows-chronic atrophy with decreased number or absence of parietal cells, lamina propria of mucosa reveals an intense lymphocytic infiltration, most are CD4+ T lymphocytes, with admicture plasma cells and B lymphocytes -as the infiltration persists, the oxynthic glands disappear and are replaced by mucin producing glands -erly stage disease is associated with proliferation of endocrine cells, some patients may develop low grade gastric carcinoids -complete intestinal metaplasia with Paneth and goblet cells is common, less commonly glandular cell dysplasia occur-represents a precancerous lesion Type B gastritis -much more common than type A -involves mainly antral region of the stomach -is of non-immune origin, is caused by infection of the mucosa of the stomach by 5 H.pylori. This microorganism is a nonsporing, S-shaped gram negative rod clinically: epigastric discomfort, pain, nausea -patients with chronic g-itis caused by H. pylori usually improve when treated with antimicrobial agents, and relapses are associated with reappearance of H.pylori in the stomach -very important is the relationship between chronic gastritis and peptic ulcer, the patients are possibly in higher risk of development of gastric cancer Eosinophilic gastritis -rare disease-believed to develop due to allergic hypersensitivity, pathogenesis- unclear microscopically: gastric mucosa is infiltrated by chronic inflammatory cells including eosinophils-intestinal mucosa my be also affected, sometimes- small vessel vasculitis and epithelioid granulomas 3) Peptic ulcer disease -chronic, most often solitary ulcers in any portion of the alimentary tract arising from exposure to acid-peptic juices- most cases occur in the duodenum and stomach epidemiology: most often in middle age, more common in men, duodenal ulcer is more frequent in patients with alcoholic cirrhosis, chronic renal failure and hyperparathyroidism morphology: grossly- sharply punched out defect with overhanging mucosal borders, smooth and clean ulcer base microscopy: four layers can be identified -a thin superficial layer-necrotic debris, zone of inflammation, which is underlaid by a layer of granulation tissue, beneath which there is fibrous scar -surrounding mucosa exhibits a chronic gastritis Pathogenesis: peptic ulcers are produced by an imbalance between the gastroduodenal mucosal defence mechanisms and damaging force of gastric juice mucosal defense mechanisms- include surface mucus secretion, bicarbonate content in secretion, mucosal blood flow, apical epithelial cell transport systems, epithelial regeneration, mucus defence is impaired by shock, ischemia, delayed gastric emptying, and duodenal reflux damaging forces- include gastric acid and pepsin, H. pylori infection, aspirin, cigarettes, alcohol, impaired regulation of acid secretion, stress-uncertain Clinical features: typical symptoms are epigastric burning, aching pain that is worse at night, or 1 to 3 hours after meals, nausea, vomiting, belching, etc. complications include anaemia (because of occult bleeding), hemorrhage, perforation, obstruction (oedema and/or scar in a pyloric channel), malignant transformation vascular gastropathy 6 is characterized by abnormalities in gastric blood vessels without inflammation -it may be dues to portal hypertension-called portal hypertensive gastropathy -important cause of gastric bleeding, changes confined to gastric body and fundus-edema, red mucosal spots, marked vascular ectasias -second lesion is gastric antral vascular ectasia (VAGE)- endoscopic appearance of “watermelon stomach”-raised, red mucosal stripes of dilated and tortuous blood vessels in antrum, often seen in elderly women with other autoimmune diseases, histologically multiple intravascular thrombi, myofibroblastic proliferation in lamina propria TUMORS OF THE STOMACH GASTRIC POLYPS AND BENIGN TUMORS gastric polyps- are rare-there are two major types of epithelial polyps the term polyp refers to any nodule or mass that projects above the level of the surrounding mucosa, majority of gastric polyps are hyperplastic/inflammatory (90%) -hyperplastic polyps -smooth-surfaced, sessile or pedunculated -they represent non-neoplastic lesions- regenerative, inflammatory -may be multiple histologically: consist of epithelial tubules and cysts interspersed within an inflammatory stroma -adenomatous polyps -benign neoplastic lesions -usually single- lobulated surface histologically: consist of closely packed tubular epithelial structures with varying degree of cellular atypia and polymorphism- called dysplasia -higher risk of malignant transformation Multiple polyps are seen in polyposis syndromes, such as -familial adenomatous polyposis (FAP) is an autosomal dominant polyposis exhibiting numerous adenomatous polyps in the colon, stomach and elsewhere, with high risk of progression to adenocarcinoma -treatment- prophylactic colectomy, adenomas elsewhere create continued problems -Peutz-Jeghers syndrome is an autosomal dominant inherited disorder composed of melanotic pigmentation of mucosal and skin surfaces, hamartomatous polyps of the small intestine and colon, and increased risk of carcinoma of breast, pancreas, lung, ovary and uterus -hamartomatous polyp- is large pedunculated, with arborizing smooth muscle surrounding normal abundant glands -Gardners syndrome is an FAP variant exhibiting multiple osteomas (mandible, skull, long bones), 7 epidermal cysts, fibromatosis (desmoid tumor), and numerous adenomatous polyps in GI MESENCHYMAL TUMORS -uncommon, well-circumscribed benign tumors within the wall of the stomach, covered by preserved mucosa, smooth surface -neurofibroma -lipoma -leiomyoma -epithelioid leiomyoma =leiomyoblastoma- is a variant of leiomyoma peculiar to the stomach -biologically benign, well circumscribed, may be large intramural mass histologically: composed of large spindle or round pleomorphic cells with features of smooth muscle cells -inflammatory fibroid polyp=pseudotumor- rare, probably non-neoplastic lesion -first description by prof. Vaněk as eosinophilic granuloma of the stomach -histologically: it consists of highly vascularized myofibroblastic and fibroblastic proliferation with polymorphic inflammatory infiltration dominated by eosinophilic leukocytes MALIGNANT TUMORS 1. Gastric carcinoma -accounts for over 90% of malignant tumors of the stomach -geographic differences in the incidence- 10 times higher in Japan than in the U.S.for example- environmental factors play role -precancerous lesions for gastric carcinoma include: -chronic atrophic gastritis with dysplasia- its association with PA -adenomatous polyps with dysplasia -chronic peptic ulcers grossly:-early cancer- =gastric carcinoma restricted to the mucosa and submucosa -recognized in Japan- diagnosis by endoscopic examination and biopsy -advanced gastric cancer- =gastric carcinoma that invades the gastric wall-presents as- endoscopic gross morphology: -fungating mass that protrudes into the lumen- polypoid -as a malingant ulceration with raised edges -as an ulcer resembling the peptic ulcer - as a diffusely ifiltrating lesion that causes diffuse thickening of the gastric wall microscopically: all gastric carcinomas are adenocarcinomas of varying degree of differentiation -the most common -poorly differentiated so called diffuse carcinoma of signet-ring cell type 8 -well differentiated carcinoma resembling the tubular adenocarcinoma of the intestine is less common= intestinal type of gastric cancer spread: gastric carcinoma is locally aggressive- rapidly spreads through the whole wall of the stomach -lymphatic spread- rapid, lymph node metastases -spread along the surfaces of the peritoneum -bloodstream spread- to the liver and lungs -Kruckenberg tumor = unilateral, and more often bilateral metastasis to ovaries clinically: early cancer- asymptomatic advanced cancer-anorhexia, anemia, weight loss, hematemesis and melena diagnosis: endoscopy and biopsy prognosis: depends almost entirely on the depth of invasion of the tumor early gastric cancer- 5-year survival rate of 85% advanced cancer- " of only 30% staging is very important, grading of little prognostic value 2. Malignant lymphoma accounts for about 3 % of malignant tumors of the stomach grossly: polypoid masses, ulcers or mucosal thickenings diagnosis: only by endoscopic biopsy (histological examination of the specimen) primary gastrointestinal ML= MALT lymphoma -arises in mucosa-associated lymphoid tissue -majority of lymphomas are of B-cell type, derived from follicular-center cells gastric lymphoma- responds well to chemotherapy- better prognosis than that of carcinoma MALT-lymphomas have better prognosis than nodal lymphomas of the same typelower tendency to disseminate 3. Gastric leiomyosarcoma -accounts for about 2% of gastric malignancies grossly: large masses that originates in the wall of the stomach -lower tendency to metastasize than in carcinoma microscopically: composed of malignant smooth muscle cells with high mitotic activity, necroses and foci of hemorhages clinically: bleeding, blood loss, anemia, palpable mass tumor is often located deep in the wall- diagnosis by endoscopy usually impossiblevariant of this tumor- epithelioid leiomyosarcoma (mitotic activity, necroses, aggressive growth ) 4. Carcinoid -arises from neuroendocrine cells present within the mucosa of the stomach- histological appearance and biological behaviour - similar to identical tumours of the intestine 5. GIST (gastrointestinal tumor) -is mesenchymal tumor of GIT (most common in intestine, but occurs from 9 esophagus to rectum throughout the whole GIT) composed of spindle shaped cells arranged in short fascicles with variable proliferative activity mitotic count, necroses, locally aggressive growth pattern and about half of the cases recur and cause metastases (liver) -the most important factors for prognosis include size of the tumor, and mitotic rate grossly: large bulky intramural tumors or subserosal projections on cross section: the tumor has a soft, fish-flesh appearance with or without haemorrhages genetics: the tumor arises from interstitial cells of Cajal, majority of the tumors have mutations in genes encoding for the c-kit protein (immunohistochemically positive staining for CD117/c-kit) -c-kit protooncogene is located on chromosome 4q, and oncodes a transmembrane tyrosine kinase receptor- this allows a treatment by selective inhibitor of tyrosine kinase with activity against KIT (imatinib, gleevec) therapy: surgical resection remains primary treatment 10