Cations – transmit nerve impulses to muscles and contract skeletal
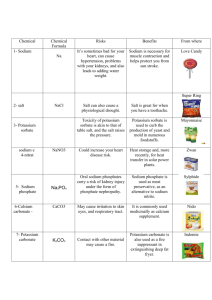
advertisement

Cations – transmit nerve impulses to muscles and contract skeletal and smooth muscles (K, Na, Ca, Mg), positive charge (t is like the plus sign) Anions – attached to cations (CL, HCO3, PO4, SO4), negative charge (n reminds you of negative) Osmolality – concentration of body fluid, normal is 275 – 295, if less is hypo-osmolar (result of excess water intake or fluid overload caused by an inability to excrete excess water, if more is hyperosmolar (caused by severe diarrhea, increased salt and solutes (protein) intake, inadequate water intake, diabetes, ketoacidosis or sweating) Sodium – main extracellular electrolyte, major fxn is to regulate body fluids Isotonic solutions – D5W, NS, LR, Ringer’s solution, very similar to extracellular and intracellular fluids, used with fluid volume loss; D5W when given rapidly or continuously will become hypotonic because dextrose is rapidly metabolized into water and carbon dioxide Crystalloids – dextrose, saline, LR, used for replacement and maintenance fluid therapy Colloids – volume expanders, dextran solutions, amino acids, hetastarch, plasmanate, dextran is not a substitute for whole blood because it doesn’t have any products that can carry oxygen, hetastarch is isotonic and can decrease platelet and hematocrit counts and is contraindicated in bleeding disorders, CHF, renal dysfunction, plasmanate can be used instead of plasma or albumin to replace body protein Blood and blood products – whole blood, packed RBCs, plasma, albumin Lipids – fat emulsion solutions, indicated when IV therapy lasts longer than 5 days Daily water need – 2000 ml/day average, 15 ml/pound, increase by 15% if pt has fever Potassium – 20 times more prevalent in cells than in vessels, 3.5 – 5.3, narrow normal range, too little or too much can lead to cardiac arrest, poorly stored in the body so give it daily, bananas and dried fruits are higher than oranges and fruit juices, necessary for transmission and conduction of nerve impulses and for contraction of skeletal, cardiac and smooth muscles; given with an anion (ie. Chloride or bicarb), extremely irritating to the GI and intestinal tract so give with glass of fluid, IV K must be diluted in IV fluids, cannot be given as a bolus or push, always must be diluted Hypokalemia – when cells are damaged from trauma, injury, surgery or shock, potassium leaks from the cells into the intravascular fluid and is excreted by the kidneys, with cellular loss of potassium it shifts from the blood plasma into the cell to restore the cellular potassium balance leading to hypokalemia, vomiting and diarrhea also decreases K levels; s/s – nausea, vomiting, dysrhythmias, abdominal distention, soft flabby muscles; for low levels encourage foods high in potassium (ie. fruit juice, citrus fruits, dried fruits, bananas, nuts, veggies); certain drugs promote K loss – hydrochlorothiazide, Lasix (potassium-wasting diuretics), cortisone preparations; if they take these drugs they need to eat more foods with potassium; use potassium cautiously in pts with renal insufficiency, be cautious is urine output is less than 600 ml/day Drugs – there are potassium-wasting diuretics (excrete K, Na, Cl in the urine) and potassiumsparing diuretics (retain K but excrete Na, Cl in the urine); laxatives, corticosteroids, antibiotics, potassium-wasting diuretics are the major drug groups that cause hypokalemia; oral and IV potassium salts, CNS agents, potassium-sparing diuretics can cause hyperkalemia Hyperkalemia – if the kidneys shut down or are diseased, K accumulates in the intravascular fluid, caused by renal insufficiency or administration of large doses of K over time, for mild elevation restrict foods high in K, to immediately decrease K levels use sodium bicarbonate, calcium gluconate or insulin and glucose or Kayexalate with sorbitol (this drug therapy exchanges a NA ion for a K ion in the body and is a more permanent means of correcting hyperkalemia), s/s – nausea, abdominal cramps, oliguria, tachycardia or late bradycardia, weakness, numbness or tingling in the extremities Sodium – major cation in the ECF, normals 135-145, regulates body fluids, promotes the transmission and conduction of nerve impulses, part of the sodium/potassium pump that causes cellular activity; Na shifts into cells as K shifts out of cells repeatedly to maintain water balance and neuromuscular activity, Na combines readily with Cl or HCO3 to promote acid-base balance Hyponatremia – can result from vomiting, diarrhea, surgery, potent diuretics; s/s – muscle weakness, headaches, abdominal cramps, nausea, vomiting; can give NS to increase sodium content in the vascular fluid Hypernatremia – requires sodium restriction; s/s – flushed skin, elevated body temp, elevated BP, rough dry tongue; can result from consuming certain drugs (cortisone, cough meds, some antibiotics) Water – essential nutrient, more important to life than any other nutrient, body needs more water each day than any other nutrient, can survive only a few days without water, minerals help the body maintain an appropriate balance and distribution of water, 60% of an adult’s body weight, more in a child Carries nutrients and waste products Maintains the structure of large molecules Participates in metabolic reactions Serves as a solvent for minerals, vitamins, amino acids, glucose Acts as a lubricant and cushion around joints, eyes, spinal cord Aids in regulation of normal body temp Maintains blood volume Water intake – when the blood becomes concentrated (having lost water but not the dissolved substances in it) the mouth gets dry and the hypothalamus initiates drinking behavior, thirst lags behind the body’s need, first sign of dehydration is thirst, if you can’t get fluid or don’t perceive the thirst message you get dehydrated rapidly; water intoxication leads to hyponatremia Water sources – water itself and other beverages, fruits and veggies have up to 90% water, meats and cheeses contain 50%, water is also generated during metabolism, caffeine can be counted towards total intake, alcohol acts as a diuretic and dehydrates you Fluids maintain blood volume which, in turn, influences blood pressure, central to the regulation of blood volume and BP are the kidneys, instructions on whether to retain or release substances or water comes from ADH, rennin, angiotensin and aldosterone (see Figure 12-3, pg 401 Nutrition) ADH – retains water; (also called vasopressin) whenever BP or blood volume falls too low or extracellular fluid becomes too concentrated they hypothalamus signals the pituitary gland to release ADH, this is a water conserving hormone that stimulates the kidneys to reabsorb water, so the more water you need the less your kidneys excrete, this also triggers thirst Renin – retains sodium; cells in the kidney release renin in response to low blood pressure causing the kidneys to reabsorb sodium, sodium reabsorption is always accompanied by water retention which restores blood volume and BP Angiotensin – constricts blood vessels; renin also activates angiotensin which is a powerful vasoconstrictor which raises BP Aldosterone – retains sodium; angiotensin causes the release of aldosterone from the adrenal glands, it signals the kidneys to retain more sodium and water, the effect is that when more water is needed less is excreted Cells – must maintain a balance of 2/3 body fluids inside the cells and 1/3 body fluids outside cells, if too much water enters then the cell can rupture, if too much water leaves cells can collapse; to control the movement of water, the cells direct the movement of the major minerals If an anion enters the fluid, a cation must accompany it or another anion must leave so that electrical neutrality is maintained, it’s a good bet that whenever Na and K ions are moving, they are going in opposite directions Electrolytes attract water, some electrolytes reside outside cells (sodium, chloride) and some inside cells (K, Mg, PO4, SO4), cell membranes are selectively permeable (they allow passage of some molecules but not others), whenever electrolytes move across the membrane water follows, proteins attract water and help to regulate fluid movement, regulation occurs mainly in the GI tract and the kidneys Na and Cl are the most easily lost because they are the primary extracellular electrolytes, sweating, bleeding or excretion Start at pg 404, Acid-Base balance