File - Pocket Prof Apps
advertisement

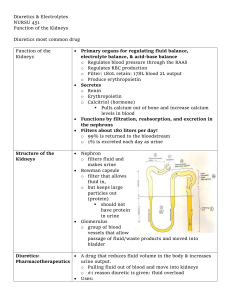
Fluid & Electrolyte Disorders Disclaimer - Pocket Prof Apps has used reasonable efforts to ensure that the information provided is both accurate and current. However, your education is ultimately your responsibility, and Pocket Prof Apps makes no guarantee to the accuracy or applicability of any information provided, and assumes no liability for your reliance on any information we provide. Further, the information provided in resources published by Pocket Prof Apps represents the understanding and opinions of the presenters and authors, and may or may not be consistent with the opinions or preferences of your own professors. We therefore recommend that you use information provided by Pocket Prof Apps to supplement your other education resources, and not replace your own study, group discussions, and class lectures. ©2013 www.pocketprofnursing.com by Pocket Prof Apps Fluid Volume Deficit (No Water, No Salt, Or Both) • No Water (hypertonic) – Profuse sweating, hyperventilation, DKA, fevers, diarrhea, renal failure, DI • No Salt (hypotonic) – Water intoxication, chronic illness, malnutrition, renal failure • Both (isotonic) – NPO, poor intake, hemorrhage Fluid Volume Deficit • • • • • • Low BP, high HR Dry mouth, thirst Rapid weight loss Low urine output Confusion, lethargy SG>1.030, high Hct, high BUN, low Na, high osmo What can you do? What are the symptoms? • Fluids (oral if alert) • NS or LR (no potassium until urine output is increased) • Daily weight, strict I/Os • May need antidiarrheals, antiemetics, abx, antipyretics Fluid Volume Excess • Happens when there is increased sodium and water • Causes: – Hypervolemia (isotonic) • Too much IV fluid, kidney failure, corticosteroids – Water intoxication (hypotonic) • CHF, SIADH, IV fluids, psych problems, wound irrigation – Too much sodium intake (hypertonic) • Too much salt, 3% saline IV, too much NaHCO3 Fluid Volume Excess • • • • • • • Rapid weight gain Edema High BP, bounding pulses May have urine output JVD, crackles, dyspnea Decreased LOC Low Hct, low BUN, high Na, low osmo What can you do? What are the symptoms? • • • • Diuretics Fluid restriction (no IV fluids) Sodium restriction Daily weights, strict I/Os Lab Normals Electrolyte Range Magic 4 Potassium 3.5 – 5.5 4 Chloride 98 – 106 104 Sodium 135 - 145 140 pH 7.35 – 7.45 7.4 pCO2 35 – 45 40 HCO3 22 – 26 24 FYI – Hematocrit normal is 3 times the hemoglobin (10-14 is normal) Sodium (135 – 145 mEq/L) • Major cation of ECF • Sodium level reflects the ratio of sodium to water • Regulated by kidneys, ADH, aldosterone • GI tract absorbs sodium from food • Imbalances are typically associated with fluid volume problems • Foods high in sodium – processed meats, condiments, dairy Hypernatremia ( Na) • Water loss or excess sodium • Na excretion – renal failure, corticosteroids • Na intake – eating too much salt, too much sodium in IV fluids • water loss – fever, infection, hyperventilation, sweating, diarrhea, dehydration F R I E D “You Are Fried” Fever (low grade, flushed skin) Restless (irritable) Increased fluid retention and BP Edema (peripheral and pitting) Decreased urine output, dry mouth Hypernatremia ( Na) What can you do? Reduce sodium slowly! • Treat the underlying cause • Diuretics • Sodium restriction • Seizure precautions Hyponatremia ( Na) • • Water excess or loss of sodium Dilution – polydipsia, freshwater drowning, SIADH, CHF excretion – sweating, diuretics, GI wound drainage, renal disease intake – NPO, low salt diet, severe vomiting/diarrhea Symptoms: Confusion, headaches Seizures (can progress to coma) Abd cramps, n/v Hyponatremia ( Na) Replace sodium slowly! What can you do? • • • 3% normal saline If caused by fluid excess, will need fluid restriction Usu. can’t be fixed by adding sodium to the diet Potassium (3.5 - 5.0 mEq/L) • Major cation of ICF • Sodium-potassium pump is a major controller • Moves into cells during formation of new tissues and leaves the cell during tissue breakdown • Source of potassium – diet • Primary route of loss - kidneys • Foods – avacado, fish, banana, OJ, raisins, dried fruits, meat, milk, fruits, veggies, salt substitutes Hyperkalemia ( K) Causes – kidney failure (most common), use of salt or potassium supplements, receiving old blood, cell destruction, acidosis, hypoxia, exercise, catabolic state, use of potassium-sparing diuretics Can get false high results if specimen not handled properly “MURDER” M U R D E R Muscle weakness Urine, oliguria, anuria Respiratory distress Decreased cardiac contractility ECG changes Reflexes, hyperreflexia, or areflexxia Hyperkalemia ( K) What can you do? • Cardiac monitor • Kayexalate, calcium gluconate, or glucose & insulin IV • Lasix if kidneys are functioning • Stop potassium in IV fluids • Have pt avoid foods high in potassium • Dialysis if severe Hypokalemia ( K) • Causes – Vomiting, NG suction, diarrhea, medications (diuretics, laxatives, insulin), metabolic alkalosis, rapid cell building (ie. B12 or erythropoietin to increase RBCs) • Signs/symptoms – Dysrhythmias, weakness, n/v, paralytic ileus, constipation, low BP, weak pulse, increased digoxin toxicity, muscle weakness and paralysis, diuresis Hypokalemia ( K) can you do? Watch for Digoxin toxicity! What Potassium Administration •Must have urine output •Never give IV push •Must be on cardiac monitor •Assess IV site often (prefer CVC) •Always dilute and give no more than 20 mEq, no faster than 1 hr •Max concentration in IV fluids is 40 mEq/L • • • • Cardiac monitor Foods high in potassium Watch for dig toxiciity Potassium IV (only if good urine output) • Spirinolactone • Treat constipation • Keep pt safe from falls Calcium (9.0 – 10.5 mg/dL) • Primary source is bones • Regulated by parathyroid hormone, calcitonin, and vitamin D • Affects transmission of nerve impulses, heart and muscle contractions, blood clotting, and forming of teeth and bone Hypercalcemia ( Ca) What are the symptoms? What causes it? What can you do? Hypocalcemia ( Ca) C A T S “CATS Convulsions Arrhythmias Tetany Spasms and stridor Phosphate Imbalances • Hyperphosphatemia – Cause - renal failure, tumor lysis syndrome – S/S – calcium deposits in joints, skin, kidneys, eyes; hypocalcemia, tetany, neuromuscular irritability – Tx – fix hypocalcemia • Hypophosphatemia – Cause – malnutrition, malabsorption syndrome, alcohol abuse, too many antacids – S/S – CNS depression, confusion, muscle weakness, dysrhythmias, fractures – Tx – oral supplements (Neutra-Phos), decrease calcium intake, IV phosphate (but this can cause sudden hypocalcemia), stop anatacids and calcium supplements Magnesium Imbalances • Hypermagnesemia – Cause – increased intake (ie. MOM, Maalox) with chronic kidney disease – S/S – lethargy, n/v, loss of DTRs, can have respiratory and cardiac arrest – Tx – avoid magnesium-containing drugs, increased fluid intake, may need dialysis • Hypomagnesemia – Cause – prolonged fasting or starvation, chronic alcoholism, diuretics – S/S – confusion, hyperactive DTRs, tremors, seizures, cardiac dysrhythmias – Tx – oral supplements, increase green veggies, nuts, bananas, oranges, peanut butter, chocolate; IV or IM magnesium (if given too rapidly can cause cardiac or respiratory arrest) Medications • Loop diuretics • Thiazide diuretics • Potassium sparing diuretics • Electrolytes • Kayexalate Don’t forget rules for giving potassium! General Rules • Don’t give at night • Commonly given with an anti-hypertensive • All but potassiumsparing will decrease potassium levels • Watch for more videos coming soon. • Check out our website (www.pocketprofnursing.com) for my notes, videos, and games to test your knowledge. • Watch for more Med Surg videos and app coming soon. © 2013 www.pocketprofapps.com Bringing practical nursing education to your mobile devices - teachers helping students. • We welcome and ask for your feedback so we can make improvements. Click below the video to comment, suggest other video topics, and/or ask questions. • Please rate our videos by clicking “like” or “dislike”. • Please “share” this video if it was helpful to you. • Subscribe to our you tube channel so you will be the first to see new videos. • Thanks for watching!!!! Image Attribution • Slide 1 – Flickr by Randy Le'Moine Photography; www.pixabay.com, no attribution required • Slide 6 – Flickr by IvanWalsh.com • Slide 19 - www.pixabay.com, no attribution required • Much information on these slides (not images) was utilized from Mosby’s Fluid & Electrolyte Memory Notecards