Biochemistry –Second year, Coll
advertisement

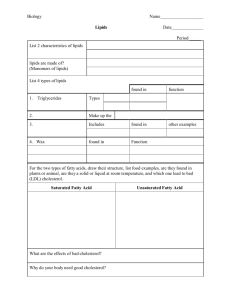
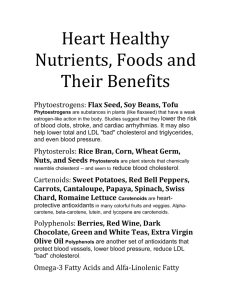
Biochemistry –Second year, Coll. of Medicine-Baghdad Univ. 2011-2012. Dr.Basil Oied Mohammed Saleh. Subject:Lipid Lecture 1 29-3-2011 Lecture 2 6-10-2011 Lecture 3 13-10-2011 Lecture 4 20-10-2011 Introduction to lipid Objective: Illstrates the meaning of lipid, types and their functions. Lipid are compounds that are soluble in organic solvents, such as ether and relatively insoluble in water or aqeous media e.g.human body fluid such as blood, seminal and interstitial fluid(water account for about 93 % of blood).The principal unit of different forms of lipid is fatty acid with general formula: RCOOH; R: is aliphatic carbon chain structure: CH3(CH2)nCH2; n is the number of carbon. In nature fatty acid may be: 1.Saturated; CH3CH2……., the common one in human body is Palmitic acid(C16) 2.Monounsaturated CH3CH2CH=CH……(one double bond), and 3.Polyunsaturated CH3CH2CH=CHCH2CH2CH=CH…….(2 or more of double bonds ).The most important of polyunsaturated fatty acids are the Essential Fatty Acids(EFAs).The EFAs are those fatty acids that are required in human body but cannot be synthesized in it, so must be supplied in the diet to support the growth and include: Linoleic acid C18, 2 double bonds Linolenic acid C18, 3 double bonds Arachidonic acid C20, 4 double bonds. The absolute EFAs are the linoleic acid, the precursor of arachidonic acid that is a substrate for Prostaglandins synthesis and the Linolenic acid, the precursor for other ω-3 fatty acids formula important for growth and development.These EFAs are important components of phospholipids of cell membrane and mitochondrial membrane and their deficiencies result in defect in growth and development.Even the incidence of EFAs deficiencies is rare, it can lead to scaly dermatitis, visual and neurologic defects. Fatty acids also may be: Short : C2-C4 Medium: C6-C10 Long: C12 and more. The saturated fatty acids are naturally found in Zigzag form, while the unsaturated fatty acids in kinked form. The degree of unsaturation(number of double bonds) and the carbon chain length are important in determining of melting point of fatty acids and so of biological membrane fluidity composed of them(permeability to lipid soluble substances). The important structures of lipid materials are: 1. Triglycerides; Simple lipid 2. Phospholipids; Complex lipid 3. Sphingolipids and Glycolipids; Complex lipid 4. Cholesterol, Cyclolipid 5. Lipoproteins, Male and Female Sex Hormones, Adrenal Cortical Hormones(cortisol and aldosterone), Vitamin D, and other derived lipid: Derived lipid. Defintions: Triglyceride; TG (Triacylglycerol): Are fatty acid ester of glycerol alcohol; 3 fatty acids+ Glycerol (CH2OH-CHOHCH2OH). Diglyceride; 2 fatty acids+ Glycerol Monoglycride: 1 fatty acid+ Glycerol. In nature fatty acids contained in acylglycerol are different in carbon chain length and degree of saturity. TG represents(its function) the principal storage form of energy in adipose tissues that needed physiologically in prolonged fasting and starvation and pathologically, for example in uncontrolled diabetes mellitus. It is also the preferred form of nutrient that is used by muscle in producing of chemical energy ATP under normal conditions. TG forms about 95 % of dietary fat. The general structure of TG is: CH2OCOR1 CHOCOR2 CH2OCOR3 : R1,R2,R3 are different fatty acids.TG is considered as nonpolar structure and so not implied in CM formation. Phospholipids;PL( Phosphoglycerolipids): These lipids also composed of Fatty acids(R) and Glycerol as TG, but also phosphoric acid(PO4) and nitrogen base. These two latter structures(PO4 and nitrogen base) confer the PL compounds the relative polarity and so their function in CM and mitochondrial membrane structures. The general formula of PL is: CH2OCOR1 CH2OCOR1 CHOCOR2 CHOCOR2 CH2OPO3-Nitrogen base is PL, while CH2OH is Phosphatidic acid Type of PL is defined according to the type of contained nitrogen base: Base PL Choline Lecithin Ethanol amine Cephalin Serine Phosphatidyl serine Inositol Phosphatidyl inositol triphosphate And Cardiolipin phospholipid; Diphosphatidyl glycerol. PLs are also reffered to as amphipathic compounds because of their formation from polar(PO4 and nitrogen base) and nonpolar(fatty acids) structures. Lecithin PL is: 1.the predominant type of PL in CM 2.the source of choline component of the neurotransmitter, the Acetylcholine 3.the principal lipid component of Lung surfactant(90 % lipid and 10 % protein), its deficiency in preterm infants is associated with inadequate production or secretion of surfactant causes Respiratory Distress Syndrome(RDS), the significant cause of death. Lecithin is made and secreted by pneumocytes to act as surfactant, decrease the surface tension of fluid lining the alveoli so reducing the pressure needed to reinflate alveoli, thereby preventing alveolar collapse(atelectasis) 4. involved in emulsification of fat diet in small Intestine along with Bile salt. Cardiolipin PL is the principal type of PL that involved in inner mitochondrial membrane structure(important for maintenance of certain respiratory complexes). The laboratory test, Anti-cardiolipin ACL is used in investigation of abortion or dead infant delivery, because this PL cardiolipin is recognized by antibodies that raised against Treponema Pallidum the bacterium that causes Syphilis. Phosphatidyl inositol triphosphate in CM act as a second messenger(internal messanger) for protein hormones action. Platelet activating factor PAF and Plasmalogensare compounds that belong to PL structure but differ in containing ether linkage ROR instead of ester linkage ROCOR at C1 of PL. PAF is synthesized and released by a variety of cell types, binds to surface receptors with triggering potent thrombotic and acute inflammatory processes. It causes platelets to aggregate and degranulate, and neutrophiles and macrophages to produce superoxide radicals, the killing substance of infected bacterium. Sphingolipids(Phosphoshingolipids: Sphingomyelin): These are also PL but differ from phosphoglycerolipids(previous types) in their structure: They are composed of Sphingosine alcohol instead of Glycerol. Sphingosine is C18 monoalcoholamine: CH3(CH2)12CH=CHCHOHCHNH2CH2OH Sphingosine+fatty acid=Ceramide Ceramide+Nitrogen base= sphingolipid. Of the most significant type of these PL in humans is sphingomyelin in which the base is choline. It is an important component of myelin sheath of nerve fibers, insulates and protects neuronal fibers of the central nervous system(preventing the short circulation of nerve electrical pulse transmission). Glycolipids: These are anthor type of lipid. Their structure are relatively similar to sphingolipid; Ceramide+ carbohydrate moity(or moities)=Glycolipids. Of which : the simple forms are glucosylsphingolipid and galactosylsphingolipid(only one unit of CHO).The complex forms are Globoside and Gangalioside(2-9 units of CHO).They are found in outer leaflet of plasma membrane and contribute to cell surface antigen(anti-genicity), cellular interaction(cell-cell adhesion) and blood group(A B O system). Cholesterol : Is anthor form of lipid called sterols. Cholesterol is the major sterol in humans. It is cycloaliphatic carbon chain C27. It is present in blood in two forms: Free chol.(1/3) and Esterified chol.(2/3). Total chol. Represents the two forms: The free form is relatively polar because of free OH group at C3, while the esterified form is nonpolar because the free OH is occupied by acyl group(fatty acid RCOO) . Cholesterol is the precursor for synthesis of many vital substances: Male and Female sex hormones (Androgen such as testosterone and Estrogen, E2 ), vitamin D, Cortisol and aldosterone hormones.Cholesterol is also an important constituent of CM structure. 2. Lipoproteins: Objective: Illustrate the definition and metabolism of different types of lipoproteins Lipoproteins LPs are spherical structures composed from lipids and proteins and function in supporting the transport of lipids in circulation. In these structures the water insoluble lipids (TG and esterified cholesterol) are oriented to the core of the spherical LP, while the water soluble lipids(PL, Free chol. and added proteins) are directed to the surface of LP. However, these structures in their later form still relatively insoluble in systemic circulation and need for addition of specific proteins, called apolipoproteins(apoLPs) to confer them sufficient water solubilitiy and so transporting in blood.There are major five LPs in blood of human body,along with additional sixth one apo a that is related to LPs structurally but not functionally.The five Lps are classified in order of ascending densities by ultracentrifugation as: 1.Chylomicron 2.Very Low Density Lipoprotein (VLDL) 3.Intermediate Density Lipoprotein(IDL) 4.Low Density Lipoprotein(LDL) 5.High Density Lipoprotein(HDL) Chylomicron(Exogeneous LP): It is synthesized in small intestine from dietary lipid after being digested and absorbed. The reabsorbed lipid(fatty acids, PLs, free cholesterol) are resynthesized in enterocyte again into TG, PL, and cholesterol ester. These lipid are oriented as mentioned above into spherical structure and converted into LPs after addition of apolipoproteins, principally apo B48 and to a lesser extent apo A I. Chylomicron composed mainly of TG 90 %, and the remainder are PLs, cholesterol and apoLPs.Because of its low density(large size), it is secreted firstly into lymphatic system and gives this system its milky appearance, then passes into systemic circulation, where this LP accepts apo C II into the circulation from anthor LP(HDL). In blood, chylomicron is transported to adipose tissue and skeletal muscle where there are an important enzyme Lipoprotein Lipase (LPL) which anchored by heparan sulfate to the capillary walls of the most tissues, but predominantly those of adipose tissue and cardiac and skeletal muscle. This LPL catalyze the hydrolysis of TG contained in this LP into Free fatty acids(FFAs) and glycerol in the presence of apo CII as coenzyme. FFAs are taken up by adipose tissues(stored as TG) or muscle for production of energy ATP. Glycerol is transported to the liver to be used in lipid synthesis TG, glycolysis or gluconeogenesis, however it caanot be used by adipose tissue ?. As more than 90 % of TG is removed from chylomicron by LPL and as the apoCII is returned to HDL, the remainder particle is reffered to chylomicron remnant which is taken up by hepatic receptors via recognition the apo E on the surface of this remnant by endocytosis(engulf process). Components of the engulfed remnant; FFAs, cholesterol, PL and amino acids that are produced and released by lysosomal enzymes are used by hepatocytes. Pathological condition: Familial Hyperchylomicronemia(Hyperlipoproteinemia type I). Is deficiency of LPL or apo CII with resultant hyperchylomicronemia and hypertriglyceridemia(TG 2000-10,000 mg/dl Normal value= 150 mg/dl) even in fasting state. Normally, chylomicron is absent from circulation in fasting state and only present in nonfasting(postprandial condition). This disorder is expressed in childhood period, less than 10 year of age and characterized by the symptoms; severe abdominal pain, acute pancreatitis, eruptive xanthoma and lipemia retinalis. VLDL (Endogeneous pathway): VLDL is also composed mainly of TG but with less amount compared with chylomicron (VLDL contains 55-60 % TG). It contains also apo B100, much amount of PL , cholesterol and apoproteins, so with higher density and smaller size than chylomicron.VLDL synthesized endogeneously in the liver from chylomicron remnant(dietary lipid)?? and from those synthesized in the liver from excess ingested CHO??. The pathway of VLDL metabolism is started from its secretion into the systemic circulation in the presence of apo B100. It is transported in the blood to different tissues, mainly the adipose and muscle where there are LPL which acts in the presence of apoCII on the TG contained into the VLDL particles as in chylomicron pathway. After removal of much amount of TG as FFAs and glycerol, VLDL is converted into VLDL remnant which undergoes again subsequent hydrolysis of TG by LPL to produce what is known: Intermediate density lipoprotein IDL. This IDL which is present normally in blood transiently, is composed from equal molar amount of cholesterol and TG, and mainly apo B100 and apo E. The IDL is either taken up by hepatic receptors which recognize the apo E on the surface of IDL or is converted into LDL after removal of the remaining amount of TG contained into IDL. The IDL lipid migrate into β position in electrophoresis technique. Pathological conditions: HyperVLDLemia due to deficiency of LPL and / or apo CII with increase in blood level of VLDL and TG. Normally, the increase in TG blood level in fasting and postprandial states reflects the abnormalities in chylomicron and VLDL, respectively ?. Familial dysbetalipoproteinemia,Broad beta disease(Hyperlipoproteinemia Type III) is abnormal state in lipid metabolism which characterized by appearance of IDL in blood which is normally undetectable or transient due to presence of abnormal or variant of apo E2 on the surface of IDL and prevent its uptake by hepatic receptor.This disorder is characterized by palmar xanthoma, hypercholesterolemia and premature atherosclerosis. Abetalipoproteinemia is a rare disorder of lipid metabolism characterized by hypo- chylomicronemia and hypo-VLDL due to defect in enzyme TG Transfer Protein which involved in incorporation of apoB 48 and apo B100 in lipid of these LPs with consequences of accumulation of TG in small intestine and liver(Fatty liver disorder). Note: The function of chylomicron and VLDL is mainly to transport of TG(and to very lesser extent the cholesterol) present in diet or synthesized endogeneously to peripherial tissues, principally the cardiac and skeletal muscle and adipose tissue. LDL Low Density Lipoprotein: This type of lipid or LP is differentiated from other LPs in its principally forming from cholesterol(free and esterified) and only apo B 100. It formed as mentioned before from ILD in the circulation and functions in transporting of cholesterol(not TG) from the liver to the peripheral tissues; cardiac and skeletal muscle, adrenal and gonadal glands?, skin ?and the others. LDL, which scientifically written as LDLcholesterol(LDL-C) is important for growth and development because of need of the body for cholesterol in CM structure and synthesis of many vital substances?, but it is(LDL-C) also the Bad Lipid because of direct correlation between the blood levels of this lipid and the incidence of atherosclerosis; coronary artery diseases(CADs), cerebrovascular disease(CVD), and the peripheral atherosclerosis. The metabolism of LDL is mainly by the liver(2/3 of LDL-C) and the remainder(1/3 of LDL-C) by scavenger uptake.The uptake of LDL by the liver is dependent on hepatocellular Receptor uptake of LDL. These Receptors (R) are negatively charged glycoproteins and are distributed in the pits on the CM surface of liver.The hepatic Rs recognize,bind and internalize by endocytosis the LDL particles depending on the presence of apo B 100 and also the apo E on the surface of LDL-C. After endocytosis of R-LDL-C complex(known as endosome), the LDL-C dissociates from complex because of endosomé s low PH and (the LDL particle) is hydrolyzed by lysosomal enzymes to release the amino acids of apo- B100 and the free cholesterol.The cholesterol that carried by LDL particle may derived from dietary lipid(chylomicron remnant) or mainly hepatic endogeneous synthesis. This pathway of LDL-C clearance is very important in removal and regulation of blood cholesterol, but it is saturable pathway. The latter(saturable ) means that when hepatic Rs uptake of LDL-C increased for any reason such as increased dietary cholesterol, the Rs are saturated and the uptake of LDL is stopped with accumulation of cholesterol contained in LDL in circulation; Hypercholesterolemia. Normally, after hepatocellular uptake of LDL-C and release of free cholesterol intracellulary, 1.Free cholesterol is converted into esterified cholesterol(E.cholesterol) by enzyme Acylcholesterolacyltransferase(ACAT) which is less toxic than free one 2. Free cholesterol is transpoted to different tissues for vital substances synthesis 3. the endocytosized Free cholesterol inhibits the intracellular de novo synthesis of cholesterol by negative feed back inhibition of regulatory enzyme of cholesterol synthesis pathway, the Hydroxy Methyl-Glutaryl-CoA reductase HMG-CoA reductase enzyme to prevent the toxic accumulation of free cholesterol but with increased blood level of it 4. the endocytosized cholesterol also inhibits the transcription(gene expression) of LDL-C R and so decreases the availability of these Rs on the surface of liver cells with resultant hypercholesterolemia. The above pathways of endocytosized cholesterol are important to regulate the intracellular cholesterol. Note: Statin drug of different nomenculture;levostatin,avostatin… is mainly act as anti-hyperlipidaemic or anti- hypercholesterolemic by its inhibition of HMG-CoA reductase enzyme. The second pathway of cholesterol clearance is Scavanger receptor class A(SRA).These SR can bind the chemically modified LDL-C such as the oxidized LDLC(oxidation of its fatty acids or the apo B100), but irrespective of their intracellular levels. This means that the SR-A pathwary is not down-regulated by the intracellular endocytosized cholesterol levels. These SRs are predominantly found in Macrophages (the Monocyte leukocytes) which after engulfing and accumulation of large amounts of cholesterol are, the macrophages transformed into foam cells, which participate(the early step) in development and progreesion of atherosclerotic plaque. Pathological condition: Familial Hypercholesterolemia FH(Hyperlipoproteinemia type II). It is primary genetic defect in the hepatic LDL-R gene, The R that is responsible for recognition, binding and removal of LDL molecule from the circulation. Deficiency or defective(mutant) of LDL-R causes significant elevation of blood LDL-C and consequently the cholesterol in blood and premature atherosclerosis.Complete deficiency of LDL-R(homozygotes) leads to FH in childhood and death from myocardial infarction MI before the end of the third decade.In partial deficiency of LDL-R(heterozygotes) the clinical manifestation of MI appear during the fourth decade of life. FH is characterized clinically by increased plasma LDLcholesterol levels with their deposition in skin, tendons and the arteries. The level of plasm LDL-C is 2-3 in heterozygotes, and 4-6 in homozygotes times that of normal individuals. Tendon xanthoma(Achillus xanthoma), xanthelesma and premature MI are characteristics of FH disorder. 3. HDL High Density Lipoprotein: Objective: Part of it is complemntary to prevous lecture and the remainder part illustrate the Hyperlipidaemia types and some types of Hypolipidaemia and illustration of Lipid Profile. Is the good lipid or LP. It is synthesized in the liver and small intestine as diskshapped containing only PL and apo A II(the predominant apoLP),C and E. This nascent disk-shapped HDL is transported by blood to peripheral tissues for uptake of intracellular or CM excess amounts of cholesterol(so act as protective LP, prevents the arterial subendothelial accumulation of cholesterol) and converted into spherical shape. HDLpartical is the excellent acceptor of free cholesterol(unesterified cholesterol)and so the carrier of excess amounts of peripheral cholesterol. The received cholesterol by HDL is esterified promptly by Lecithin Cholesterol Acyl Transferase(LCAT) enzyme to prevent the escape of cholesterol again to peripheral tissues?. LCAT is synthesized in the liver and carried after release on the surface of HDL particle for esterification of cholesterol, the enzyme need for apoA II for its function. The mechanism of HDL in transporting of excess(unrequired) cholesterol from peripheral tissues to the liver as the latter is the only organ deal with removing of excess cholesterol, either by conversion it into bile acids or by excretion as unmetabolized cholesterol through the bile duct(Reverse cholesterol transport) are: 1. direct uptake of whole molecule of HDL-C 2. Selective uptake of cholesterol from the HDL-C 3. Exchange of lipid between HDL-C and chylomicron and VLDL remnant, the E.cholesterol is transffered from HDL-C to the remnant and the TG is transffered from the remnant to the HDL-C. Then, the transffered E.cholesterol into the remnant is uptake by the liver through the apo E found on the surface of these remnants. There two types of HDL: HDL-3 is the newly release particle which is E.cholesterol poor particle and the HDL-2 which is the E.cholesterol rich particle that carried the cholesterol to the liver.The inverse relation between the plasma HDL-C and the incidence of CAD (and in general atherosclerosis) made it the Good lipid or LP. Hyperlipidaemia(Hyperlipoproteinemia): Hyperlipidaemia was defined by several ways; genetic as mentioned above(FH,Familial hyperchylomiconemia….), ultracentrifugation and the laboratory analysis. The best one in understanding and interpretation of hyperlipidemia is that dependent on Laboratory Analysis which classified this disorder into: 1. Primary 2. Secondary Each type is subdivided into: Hypercholesterolemia, Hypertriglyceridemia and Combined Hyperlipidemia CHL.The primary Hypercholesterolemia and hypertriglyceridemia are those characterized by significant elevation of only plasma cholesterol or TG, respectively due to genetic defect in metabolism pathways(Enzymes or Receptors) of LPs, such as FH.The secondary type is due to diseases other than the genetic causes, for example; Diabetes mellitus and Heavy alcohol abuse leads to hyperTG, While Hypothyroidism and Nepherotic syndrome result in hypercholesterolemia. So, in secondary type the defect is not in Enzymes or receptors involved in lipid pathway metabolisms. The combined Hyperlipidaemia implied the increased of plasma levels of both cholesterol and TG in the same individual, also due to genetic abnormalities(primary type) in lipid metabolism pathways or non-lipid causes(secondary type). The diagnosis of hyperlipidaemia is firstly made by excluding of secondary type; DM, Hypothyroidism…, which then make the primary type is the cause. The correction of hyperlipidaemia is depend on the type; the secondary is by correction of the underlying diseases, while the primary is by genetic treatment. Familial Hypercholesterolemia FH is usually diagnosized from the markedly elevated plasma cholesterol and the presence of tendon xanthomain the patient or first-degree relation. Possible FH is defined as a plasma cholesterol level of more than 7.5 mmol/L(NR 3.5-5.0 mmol/L) in adult(more than 6.7 mmol/L in children under 16 years). In homozygous FH, the plasma cholesterol concentration can be as high as 20 mmol/L. The severe hypercholesterolemia is accompanied by relatively normal plasma TG level. HDL-C may be low. Primary hypertriglyceridemia is often observed with low HDL-C concentration.The precipitating causes of hyperTGemia include obesity, high alcohol intake, DM and the use of estrogen. There may be an increased risk of CAD because of concomitant increased of TG and decreased of HDL-C. Actually, the increased risk of CAD that accompanied the hyperTG emia is due to elevation in plasma level of dense and small size remnant lipid. Secondary causes of Hypercholesterolemia: Primary hypothyroidism Nephroteic syndrome Cholestasis Anorexia nervosa Drug; ciclosporin Secondary causes Hypertriglycerdaemia: Alcohol excess DM chronic renal failure Drugs: estrogens, thiazide diuretics cortisol… Tangier disease: This pathogenesis of this disorder is due to absolute absence of HDL-C caused by defect in apo-A II synthesis, the integrated apoLP component of HDL. This disease is characterized by: Increased risk of CAD, CVD and peripheral atherosclerosis. Abetalipoproteinemia: Absolute deficiency of LDL-C which may lead to mental and physical retardation and failure to thrive, mainly in infants. Lipid Profile: Investigation of patient for hyperlipidaemia need to be in fasting state, the patient fasts overnight for aroun 12 hours and is only allowed to drink water. The fasting state must for plasma TG level assessment, but not for plasma cholesterol concentration. History of therapy usage is also necessary. Lipid profile means the measurement of plasma or serum levels of Test Desirable level Total cholesterol less than 200 mg/dl TG less than 150 mg/dl HDL-C 35-60 mg/dl LDL-C less than 100 mg/dl and VLDL-C. The lipaemic appearance of blood sample on standing reflects the increased level of TG due to abnormal elevation of VLDL level?. The creamy layer that appears on surface of blood sample indicates the presence of high level of chylomicron?. The abnormal increases of HDL-C and LDL-C level is not accompanied by either the lipaemic or milky layer of the blood sample?? Statin drug for hypercholesterolemia is indicated when plasma level of LDL-C is more than 100 mg/dl, however this dependent on the presence of the risk factors of CAD, DM, age of more than 40 year for male and46- 50 year for female ??, BMI and cigarette smoking. Fibrate drug for hyperTG aemia is indicated when plasma TG is more than 450-500 mg/dl, the level of 200-450 mg/dl may be trated by dietary regieme. Lecture 4 Objective: Cases about hyperlipidaemia and Illstration of pathways of Fatty acids synthesis. Case 1 A 23-year-old female had the following plasma lipid levels: Plasma Total cholesterol 550 mg/dl Plasma TG 90 mg/dl Plasma HDL-C 45 mg/dl On examination, she had tendon xanthoma on her Achilles tendons. What is the suspected diagnosis?. Case 2 A 15-year-old female presented to the surgical unit with acute pancreatitis. Some of her laboratory results were as follows: Plasma Total cholesterol 500 mg/dl Plasma TG HDL-C 2400 mg/dl 40 mg/dl On examination, she had reuptive xanthoma on her arms and lipaemia retinalis. What is the suspected diagnosis? Fatty acids synthesis Fatty acid is very important component of lipid because it participates in structures of all forms of lipid compounds. There are three pathways in humans that used in fatty acids synthesis, of the most important one is the de novo synthesis pathway. This de novo pathway means the formation of fatty acid, principally the palmitic acid C16 from the simple unit the acetyl CoA. This pathway occurred mainly in the liver, lactating glands and to a lesser extent , in the adipose tissue. The synthesis of fatty acids in humans is derived mainly from excess ingested amounts of particularly the CHO, and to a lesser extent proteins. The de novo pathway of fatty acids synthesis occurred in the cytoplasmic portion of the cells of the above defined organs and included: 1. Production of Acetyl-CoA in the cytoplasm. This molecule is produced mainly from excess amount of glucose, beyond the need for production of ATP energy. Also, acetyl-CoA is produced from fatty acids oxidation, ketone bodies, and from catabolism of some amino acids(ketogenic amino acids). However, acetyl-CoA is exclusively formed from these molecules in the mitochondria and it cannot pass the membrane of mitochondria to be available into the cytoplasm, the cite of de novo pathway synthesis. The alternative way to cytoplasmic availability of this unit is by formation of citrate molecule from condensation of mitochondrial Acetyl-CoA and oxaloacetate(steps of citric acid cycle, CAC). The formed citrate is directed through the mitochondrial membrane into the cytoplasm, this movement is enhanced when amount of produced NADH, and consequently ATP is adequately increased to inhibits the isocitrate DH enzyme(CAC). The cytoplasmic citrate is then dissociates again into Acetyl-CoA and oxaloacetate by enzyme ATP-citrate lyase. The result Acetyl-CoA in the cytoplasm is available for steps of de novo fatty acids synthesis. ∙Acetyl-CoA + oxaloacetate…citrate synthase……».. citrate(Mitochondria) ∙Citrate(mitochondria)……….».citrate(cytoplasm)…ATP-citrate.lyase…»AcetylCoA(cytoplasm)+oxaloacetate 2. The rate limiting step, the regulatory step in this pathway synthesis is the formation of Malonyl-CoA molecule from carboxylation reaction of Acetyl-CoA by CO2 in the presence of ATP. This reaction is catalyzed by Acetyl-CoA carboxylase enzyme, the regulatory enzyme of de novo pathway synthesis of fatty acids. Acetyl-CoA carboxylase Acetyl-CoA ………CO2…………………………… Malonyl-CoA C2 unit ATP……ADP+Pi When the regulatory enzyme C3 unit Acetyl-CoA carboxylase is stimulated the overall pathway of fatty acid synthesis is enhanced, and vice versa. Regulation of this enzyme included: Short -term regulation of Acetyl-CoA carboxylase: The enzyme is found in active form, polymer and in inactive form, the dimer. The formation of polymer active one is stimulated allosterically by citrate and inhibited by long chain fatty acids or their acyl-CoA(the formation of dimer inactive form). Also, this regulatory enzyme is activated by Insulin(normally postprandial) and inhibited by antagonsits hormones, glucagon and adrenaline through dephosphorylation and phosphorylation reactions, respectively. Insulin (+) Acetyl-CoA carboxylase-P ……………………………»Acetyl-CoA carboxylase Inactive form Glucagon(-) Long- term regulation of Acetyl-CoA carboxylase active form The long term regulation is dependent on the stimulation or inhibition of gene expression of the enzyme with resultant increase or decrease amount of the enzyme rather than the activity only. This stimulation is by Insulin in case of prolonged excess amount of ingested CHO meal or caloric diet, while the inhibition is by low CHO or caloric diet. 3. Addtion of two carbon unit C2 to the formed malonyl CoA(step 2) under the action of Fatty acid synthase enzyme. This enzyme is dimer, each monomer is multicomplex enzyme composed of 7 enzymes and acyl carrier protein ACP needed for the enzyme activity. The enzyme is active only in its dimer form, its splitting into 2 monomer losses the activity of it. The carrier of the added C2 is another molecule of malonyle-CoA with loss of CO2. So,with each turn of pathway the native Malonyl-CoA gained two carbon unit, the number of turns depended on the chain length of synthesized fatty acid, in lactating glands the short and medium chains are required, while in nervous system the long and very long chains are required C24 and more. All steps of addition of C2 units are carried by components of Fatty acid synthase enzyme, transporting the substrate from one component to the next one. The end step is catalyzed by Thioesterase enzyme which split the formed fatty acid from the Fatty acid synthase enzyme. CH3CoA+OOCCH3CoA…-CO2...» CH3COCH2COO-. .....+.NADPH….» Acetyl-CoA +Malonyl-CoA Attached to –SH groups of enzyme CH3CHOHCH2COO- …………-H2O……» CH3CH=CHCOO-…+NADPH…». CH3CH2CH2COO- with gain two carbon unit, the growing chain which still attached to enzyme is processed in next turn to accept another C2 from added new malonyl-CoA and so. Sources of NADPH required in pathway synthesis The required NADPH molecules for reduction steps in synthetic pathway are derived from: 1.Hexomonophosphate shunt pathway(Pentose phosphate pathway) 2. conversion of cytoplasmic oxaloacetate into malate and then pyruvate with formation of NADPH in the cytoplasm and so can be used by fatty acid synthetic pathway. NAD….»NADH H NADP……»NADPH H Oxaloacetate….……………………» Malate……-CO2………………» Pyruvate Another pathways of fatty acid synthesis are: Reverse of β-oxidation pathway Elongase system; This pathways elongates the saturated synthesized fatty acid in de novo pathway, mainly Palmitic acid. The pathway occurred in the endoplasmic reticulum ER(microsomal fraction of cell) and mitochondrial of nervous system to produces very long chain fatty acids required in the synthesis of brain lipids. Unsaturated Fatty Acids: These important fatty acids are synthesized in ER also from the satursted ones, particulary the Palmitic acid by insertion or adding double bond,one or more by enzymes known as Oxidases or Desaturase which need for NADH and O2. Lecture 5 Oxidation of Fatty Acid