ICM - Ynet
advertisement

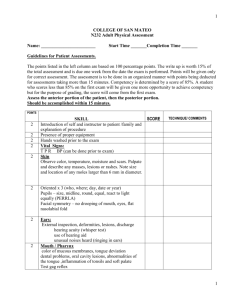
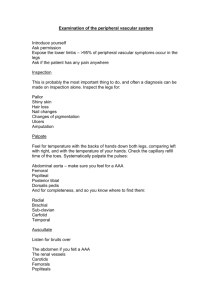
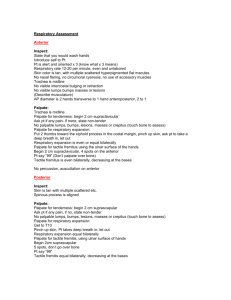
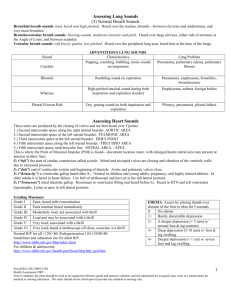
ICM Physical Examination Skills Student Checklist Upon Entering the Room: Introduce yourself by name and inform the patient that you are about to perform a complete physical examination. Remember to shake the patient's hand upon this introduction. Ask the patient how s/he would like to be addressed. Don't assume that a patient wants to be called by his/her first name. Inform the patient that throughout the exam you will explain what it is you are doing and if s/he has any questions, the patient should feel free to ask. Inform the patient that if you cause him/her pain at any time during the exam, the patient should let you know immediately. Inform the patient that you will always verbally warn him/her prior to touching any part of the body so that the patient is not taken by surprise. Ask the patient if there is anything you need to know about him/her today that may in any way hinder or affect the physical exam (e.g. is she experiencing any aches, pains or tenderness so that you know to be careful with that part of the body during the exam.) NOTE: This checklist is organized by systems (which is not necessarily an ideal order). Use your best judgment when deciding the most comfortable and logical flow of the head to toe examination of your patient. Wash hands before starting the examination. VITAL SIGNS Measure blood pressure in each arm. Hold the arm up at heart level. Place cuff snuggly in correct anatomical location. Palpate radial pulse (thumb side of wrist) for at least 15 seconds. Pulse should be taken for a full 15 seconds. Measure the respiratory rate for at least 15 seconds. HEAD AND SINUSES Examine the Skull, Hair and Scalp Step # 1: Inspect the skull for its general size, shape and contours. Step # 2: Note the hair texture and quantity. Step # 3: Examine the scalp for skin lesions. Have patient bend her head slightly forward. Inspect the skin by parting the hair in several places with your fingers. Note scaliness, lumps, or other skin lesions. Step # 4: Palpate the scalp. Use the palmar aspects of the fingertips. Feel front to back with short sweeping motions. Note lumps or tender areas. Palpate or percuss (tap) for frontal sinus tenderness above each eye. 1 Palpate or percuss (tap) for maxillary sinus tenderness below each eye. NODES AND THYROID Palpate the preauricular (in front of ears) lymph nodes. Palpate posterior auricular (behind ears) lymph nodes. Palpate occipital (base of skull) lymph nodes. Palpate the anterior cervical nodes (in front of and on top of the sternocleidomastoid muscle). Palpate the supra clavicular nodes (above the collarbone). Palpate the tonsillar lymph nodes (at angle of jaw). Palpate the submandibular lymph nodes (between tonsillar and submental nodes). Palpate the submental lymph nodes (directly under the chin). Prior to palpating the thyroid, observe the thyroid gland by asking patient to swallow. This will give the examiner a visual cue as to where the patient's thyroid is located. Palpate the thyroid gland first without and then with swallowing. Recommended technique: Examiner stands behind patient. However, this may be done while standing in from of the patient, as well. Note: Be prepared to offer the patient a cup of water in case the patient is having difficulty swallowing. EYES Test visual acuity in each eye separately with a pocket visual screening chart by holding the chart 35cm from the patient's face. It is acceptable for the patient to hold the card him/herself. Note: If the patient wears glasses, patient should be allowed to keep them on during this exam. Test visual fields (four quadrants for each eye by confrontation, each eye separately). Note to students: Make sure your fingers are outside of the patient's field of vision before you begin this test. Check with the patient as you test each quadrant to be sure that your fingers cannot be seen at the onset. Step # 1: Stand approximately 30cm from patient, outside of the patient's field of vision. Step # 2: Ask patient to close her right eye. Student than closes her left eye. Student then extends her right arm and wiggles her fingers while bringing arm in slowly at the diagonals. Student asks patient to inform her when the fingers are visible. Step # 3: With patient's right eye still closed and student's left eye still closed, student then should extend her left arm and wiggle her fingers while bringing arm in slowly at the diagonals. Student asks patient to inform her when the fingers are visible. Step # 4: Ask patient to close her left eye. Student then closes her right eye. Student then extends her left arm and wiggles his/her right arm and wiggle his/her fingers while bringing arm in slowly at the diagonals. Again, ask patient to inform you as to when the fingers are visible. 2 Both eyes (4 diagonals or quadrants) must be tested. Check for convergence by holding your finger in front of patient's face, and moving your finger in towards the patient's nose. You should start at arm's length and go about 15cm from nose. Test cranial nerves III, IV, and VI by asking patient to hold his head completely still and follow only your finger, looking rightward and leftward, up and out, up and in down and out, and sown and in. You must test the 6 cardinal positions. Test cranial nerve VII motor function by asking patient to force her eyelid closed against resistance (upper division). Note: Another method that is accepted is asking the patient to close her eyes as student tries to force the eyelids open. Observe papillary responses: Both eyes must be examined for credit. Note: The Direct Response is tested as you shine pen light into the patient's eye. You will first look into that eye for a direct response to the light. The Indirect Response to light (consensual) is tested by looking into the other eye (with the light still on the original eye). Inspect each eye separately for the condition of the lid, cornea and conjunctiva. Step # 1: Ask patient to pull down her lower eyelids and look up while you examine the eyes. Step # 2: Ask patient to pull up on her upper eyelids and look down while you examine the eyes. (By having the patient pull up and down on him/her own eyelids, you can prevent infection.) Position patient for ophthalmoscopy at a height comfortable for the examiner. Hold ophthalmoscope at proper distance to visualize the posterior structures of the eye. Hold ophthalmoscope with right hand to look through scope with your right eye when inspecting patient's right eye. Hold ophthalmoscope with left hand to look through scope with your left eye when inspecting patient's left eye. EARS Test auditory acuity by whispering into each ear at a distance of two feet (an alternative method is to create a sound by rubbing your thumb and fingers together at a distance of about 10cm from each ear, separately). Inspect the external ear thoroughly, looking in front, and then pull ear forward to look behind the ear. Examine each internal ear with otoscope by pulling up on patient's ear and inserting the speculum and carefully examining the internal ear. Perform the Rinne Test – Using the 512 Hz tuning fork Step # 1: To create a sound, hold the tuning fork by its base. Strike it gently on the heel of your hand or with the reflex hammer. Step # 2: Place the tuning fork on the mastoid process (the bony ridge behind the ear) and ask patient to tell you if she can hear (not feel) the 3 sound of the tuning fork. If she can, hold it there until she signals that the sound has faded away. Step # 3: At that point, move the fork as near to the external ear canal as possible, sweeping away overlying hair, if necessary. Hold one tine of the fork close to his/her ear. As if s/he can again hear the tuning fork. If she can, have him/her indicate when s/he cannot. Step # 4: When s/he signals s/he can no longer hear it, you should listen to the fork yourself. It should be barely audible. If so, this is normal conduction (where air conduction exceeds bone conduction and matches your own threshold of hearing). Perform the Weber Test – Using the 512 Hz tuning fork. Step # 1: Activate the fork. Step # 2: Press the base of the fork firmly on the apex of the skull in the midline. If s/he cannot hear the fork, press the base on the middle of the forehead. Step # 3: Ask where she hears it. Normally, it is heard in the midline. Abnormally, it lateralizes to one side, either toward the side of air conduction loss or away from the side conduction (sensorineural) loss. NOSE Test the openness of each nasal passage. Instruct the patient to close one nostril while sniffing through the other. Then test the other nostril in the same manner. MOUTH AND THROAT Inspect the lips, gums, tongue and teeth with the help of a tongue blade and light. You must pull patient's cheeks out with the tongue blade and inspect the teeth and gums on both sides of the mouth. You may ask the patient to pull lips up and down to inspect front teeth and gums. Inspect the posterior pharynx. Using a pen light and a tongue depressor, instruct patient to breathe through an open mouth only and not through the nose. This facilitates the inspection of the posterior pharynx. Observe the elevation of the palate by instructing patient to say "ah". Test cranial nerve XII by asking patient to protrude the tongue and move it from side to side as you observe. Test cranial nerve V motor function. First, place your hands on both sides of patient's face by the masseter muscles. Then, ask patient to bite down while palpating the contraction of the masseter muscles. Test cranial nerve VII motor function by asking patient to show the teeth (lower division). Test cranial nerve XI: Check the strength of the Sternomastoids. One at a time, have patient keep her head in the midline as you try to push the chin to one side and then the other. When she resists you, the direction you are pushing points to the muscle you are testing. Watch for bulging. Test cranial nerve XI: Check strength of Upper Trapezius. Step # 1: Place your hands on the patient's shoulders. 4 Step # 2: Have patient attempt to shrug his/her shoulders upward against your resistance. (Because of the large size of the trapezius muscles, most individuals can do this easily.) LUNGS AND THORAX – Note: All percussion and auscultation must be done on skin. Percuss the posterior lung fields bilaterally and symmetrically, over the upper and lower lung fields, comparing the left side and the right side at each of three levels. Instruct patient to breathe through an open mouth. Auscultate the posterior lung fields bilaterally and symmetrically, comparing right and left. Percuss the anterior lung fields (only on one level) on the upper chest, bilaterally and symmetrically. Instruct patient to breathe through an open mouth. Auscultate the anterior lung fields (only on one level), bilaterally and symmetrically. BREAST EXAM – Part 1 With the patient in the sitting position, ask patient to lower the gown so that both breasts are visible. Instruct patient to hold both arms above the head and examine each breast for dimpling, contour changes, and skin discoloration. Instruct patient to hold hands against hip and press forward. Inspect again for dimpling. Palpate the axillary nodes in the following four areas: 1) anterior axillary fold; 2) posterior axillary fold; 3) along the proximal humerus; and 4) deep in the axillary vault. Note: This examination can be performed over or under the gown. Ask patient to take the supine position on the examination table. BREAST EXAM – Part 2 Instruct patient to lie down supine. Instruct patient to raise the ipsilateral arm above the head. Use the middle three fingers of your dominant hand to palpate the breast starting at the top of the breast on the die of the sternum. Repeat on the opposite breast. Note: You must use 3 types of pressure while palpating, starting with a light pressure, then a medium pressure, then a firm pressure on each area covered. Fingers must never lose contact with the skin of the breast. Recommended technique: The "strip" technique – with your fingers never losing contact with the breast, descend from top to bottom and bottom to top in vertical lines until all regions have been palpated. However, most students have been taught to examine the breast in a circular motion. This is also acceptable, as long as your fingers never lose contact with the breast. 5 HEART Elevate the trunk, head and neck so that the jugular venous pulse is visible. If no jugular venous pulse is visible, return patient to the supine position and check again for a visible right jugular vein. Note: Only one pulse in one side of the neck needs to be examined. Note: The following heart exam may be done with patient sitting upright or supine. Regarding the term "palpation" when used during the cardiac examination: this palpation is designed to feel for pulses, thrills, etc. You are not feeling for masses. Therefore, your fingers should not move in a circular motion but rather should remain motionless in the appropriate anatomical location. Palpate the aortic area (2nd intercostals space on the right). Using only the pads of the fingers, not the finger tips, palpate patient's chest on the right side, towards the center. Palpate the pulmonic area (2nd and 3rd intercostals spaces on the left). Using only the pads of the fingers, not the finger tips, palpate patient's chest on the left side towards the center. Palpate the tricuspid area (4th and 5th intercostals spaces at the left sternal edge). Using only the pads of the fingers, not the finger tips, palpate patient's chest at the 4th and 5th space in the ribs. Palpate the mitral (cardiac apex) area (5th intercostals space, midclavicular line). Using only the pads of the fingers, not the finger tips, palpate patient's chest at about 5cm below the nipple line on the left side. Cardiac Auscultation Use the diaphragm of the stethoscope to auscultate the aortic area. Use the diaphragm of the stethoscope to auscultate the pulmonic area. Use the diaphragm of the stethoscope to auscultate the tricuspid area. Use the diaphragm of the stethoscope to auscultate the mitral (cardiac apex) area. Use the bell of the stethoscope to auscultate the aortic area. Use the bell of the stethoscope to auscultate the pulmonic area. Use the bell of the stethoscope to auscultate the tricuspid area. Use the bell of the stethoscope to auscultate the mitral (apical) area. For patient with suspected acortic valve disease: have patient sit up, lean forward and, using diaphragm of stethoscope, auscultate LSB 2-3rd ICS. For patient with suspected mitral valve disease: Step # 1: Ask patient to roll to left lateral position. Step # 2: Relocate apex. Step # 3: Auscultate apex with bell. Step # 4: Auscultate apex with diaphragm. In patient with suspected heart disease: check effect of Valsalva, hard grip, squatting etc., on murmurs with stethoscope placed along LSB. 6 Pulses Instruct patient to hold breath and auscultate each carotid artery. Palpate the carotid pulses (in the neck, just medial to and below the angle of the jaw) one at a time, bilaterally. Alternative method for popliteal pulses: have patient supine or seated and use both hands to palpate the pulse. Palpate the posterior tibial pulses bilaterally (at the ankle behind the medial malleolus). Note: The posterior tibial pulse is located on the inside of the ankle behind the ankle bone. Palpate the dorsalis pedis pulses bilaterally (located on the middle of the top of the foot, midway between the toes and the ankle, along the tendon line). ABDOMEN – Note: All auscultation, percussion and palpation must be done on skin. Position patient supine on the examining table and adjust table to be flat. Stand next to patient's right side. Auscultate prior to manipulation or palpation. Auscultate each of the four quadrants of the abdomen. Palpate the left upper quadrant using two pressures (gently then firmly). Palpate the right upper quadrant using two pressures (gently then firmly). Palpate the right lower quadrant using two pressures (gently then firmly). Palpate the left lower quadrant using two pressures (gently then firmly). Percuss the Traube space for splenic enlargement. Palpate the spleen. Place your hand in the proper location and ask patient to take a deep breath as you push up and in, at the bottom of the left rib cage. Then ask patient to exhale as you continue to push up and in, without causing pain to patient. This can be done either supine or in the right lateral decubitus position. * Percussion of the liver span was done prior to palpating the liver edge, in order to facilitate finding the liver edge. Percuss the liver span from just below right nipple line to just below right rib cage listening for sound to change. Palpate the liver edge. Place your hand in the proper location. Ask patient to inhale as you attempt to push up and under right rib cage. Then, ask patient to exhale and continue to push up and under liver edge, without causing pain to patient. Ask patient to sit up on examination table. MUSCULOSKELETAL Inspect both hands (palms and dorsums). Assess finger extension by asking patient to spread the fingers. Examine both hands. Assess finger flexion by asking patient to make a fist with each hand. 7 Inspect both fists. May be done actively or passively. Step # 1: Have patient extend his/her arms, palms down. Step # 2: Inspect wrists for redness and swelling. Screen range of motion for both wrists. May be done actively or passively. Step # 1: Have patient extend his/her arms, hands down. Step # 2: Have patient extend each wrist while you observe. Step # 3: Have patient flex each wrist while you observe. Screen range of motion for fingers. Step # 1: Have patient extend his/her arms. Step # 2: Observe the flexion of his/her fingers by asking her to make a fist. Step # 3: Observe the extension of his/her fingers. Screen range of motion of elbows. May be done actively or passively. Have patient extend arms in pronation and then supination. Inspect elbows. Step # 1: Have patient flex elbows and raise them to the horizontal position. This makes the elbow tips easier to see. Step # 2: Inspect the olecranon areas for bursal or joint swelling, and over the ulnar ridge for nodules. Shoulder flexion: Stand behind patient and have patient's gown completely untied and open in the back. Observe shoulder flexion by asking patient to bring the arms forward and then raise them overhead. May be done actively or passively. Shoulder internal rotation: Stand behind patient and have patient's gown completely untied and open in the back. Instruct the patient to place both hands behind the back as high up on the back as possible while you observe from behind. May be done actively or passively. Shoulder external rotation: Stand behind patient and have patient's gown completely untied and open in the back. Instruct patient to clasp both hands behind the neck and to pull the elbows back while you observe from behind. May be done actively or passively. Ask patient to take the supine position on the examination table. Note: All the following items must be performed with patient in a supine position. Inspection of both knees. Step # 1: Note any muscle atrophy, especially of the quadriceps. Step # 2: Examine the fossae above (medial and lateral) and below the knee. They should all be visible. Step # 3: Note the shape and size of the patella. Step # 4: Note any skin lesions, such as psoriasis. Screen the range of motion of the knee: Flex each knee, then extend and raise each knee. As it rises, view the joint, front and back for swelling. Palpate joint line (easiest to do with joint flexed). Check patellar motion. Check for stability of collateral ligaments (medial, lateral) – (slight flexion, stabilize at thigh, push lower leg in opposite direction). 8 Check for stability of cruciate ligaments (anterior, posterior) – (flex knee, sit on foot, hands in popliteal fossa, thumbs on joint line, move anterior and posterior). Perform bulge sign checking for fluid (milk fluid from inside of knee up, then tap the lateral margin of the patella). Assess hip flexion. Recommended technique: Grasping the heel and moving the thigh up toward the thorax, as far as it will go. External and internal hip rotation. Recommended technique: Return the thigh to a position perpendicular to the exam table while holding the shin parallel to the exam table. Now, move the ankle medially to assess hip external rotation. Move the ankle laterally to assess hip internal rotation. Return the leg to the table. Repeat these examinations on the other leg. Inspection of both ankles. When inspecting the ankles, check for swelling or redness in the gastrocsoleus complex and in all surfaces of the ankle joint. Pay close attention to any swelling around the malleoli. Screen range of motion of both ankles. Observe plantar and dorsal flexion in both ankles. Inspect the mid foot and toes of both feet. Inspect the plantar surface of both feet. Assess neck flexion by instructing patient to place the chin on the chest. Assess neck extension by asking patient to look up at the ceiling. Assess right and left rotation of the neck by asking patient to place the chin on each shoulder. Assess lateral bending of the neck by asking patient to incline each ear toward each shoulder. Ask patient to stand. Note: Inform the patient that you are going to place your hands on their hips, over the gown, to guard the patient from losing their balance and falling and also as a way to keep the gown from falling of the patient as they perform the maneuvers. Observe the alignment of the knees, heels and feet: Stand behind patient and have patient's gown completely untied and open in the back while you carefully observe the alignment of the patient's knees, heels and feet. Assess thoracolumbar lateral flexion by asking patient to bend torso to the right and to the left. Stand behind patient and have patient's gown completely untied and open in the back. Assess lumbar flexion by asking patient to bend forward at the waist and to attempt to touch the toes. Stand behind patient and have patient's gown completely untied and open in the back. Assess lumbar extension by asking patient to bend backwards. Stand behind patient and have patient's gown completely untied and open in the back. 9 Kidney punch tenderness: Perform fist percussion of the costovertebral angles by gently punching on the right and left side of patient's back, just below the rib cage. Ask patient if he feels pain. NEUROLOGICAL Romberg Test: Step # 1: Instruct patient to stand with her arms down at his/her sides and with feet together, eyes open. Watch for obvious unsteadiness. If s/he remains steady, continue with the test. Step # 2: Move closer to the patient. Place your hands on his/her shoulders. Ask him/her to close eyes and say, "I won't let you fall." Step # 3: Remove your hands to a few inches away, ready to catch him/her if necessary. Observe the patient for signs of swaying for at least 15 seconds. Ask patient to walk away from you while you observe the gait. Ask patient to walk towards you on tip toe and observe. Ask patient to walk away from you on heels and observe. Ask patient to walk towards you heel-to-toe (tandem gait) and observe. Ask patient to sit on the examination table. Drift Test: Step # 1: Ask patient to close eyes and hold arms out in front, palms up. Step # 2: Observe for at least 15 seconds for signs of one of the arms dropping below the other. Test patient's grip strength bilaterally by asking patient to squeeze your index finger as you try to pull it our of patient's grip. Test the deltoid muscle strength bilaterally by pushing downward on the patient's abducted arms. Test the biceps muscle strength bilaterally by positioning patient's elbow to a 90 degree bend, palm up. Then brace one palm on the biceps, grasp the wrist and pull. Test the triceps muscle strength bilaterally by positioning patient's elbow to a 90 degree bend, palm up. Then brace one hand on triceps, grasp wrist and push. Test the hip flexor muscle strength bilaterally but separately by having patient either seated on table with legs dangling, or supine. Resist flexion by having patient raise each knee or leg as you push down on thigh. Test the lower leg muscle strength bilaterally by asking the patient to push away your hand (placed on the ankle); then ask patient to pull towards herself. Note: Student should position the knee to a 90 degree bend. Resist flexion by pulling up on lower leg. Resist extension by pushing down on lower leg. Test the biceps reflex bilaterally. Step # 1: With the elbow slightly flexed and forearm resting in the patient's lap, palm down, palpate the biceps tendon with your thumb and press in to produce moderate tension. 10 Step # 2: Stretch the tendon by striking your thumbnail. Note speed and intensity of each response. Test the brachioradialis reflex bilaterally. Step # 1: Let patient's arm rest in her lap, elbow bent, forearm halfway between supination and pronation. Step # 2: Palpate the radial styloid (at wrist by base of thumb) and move 5cm proximally. Step # 3: Palpate the tendon over the radius. Step # 4: Stretch the tendon by striking your finger (or thumb). Watch for flexion and supination of the forearm. Test the triceps reflex bilaterally. Step # 1: Position yourself posterior to the patient, his/her arms are still in lap. Step # 2: Palpate the triceps tendon just above the olecranon. If you have trouble finding the tendon, press on the tendon as s/he extends arm against your resistance. The tendon will tighten and bulge. Step # 3: Strike the tendon directly, without an interposed finger. (Stay clear of the ulnar groove, just medial to the tendon.) Watch for extension of the forearm or contraction of the muscle. Test the patellar reflex bilaterally. Step # 1: Position the patient with his/her legs dangling freely. Then move to one side so that you do not get kicked. Step # 2: Locate the tendon just inferior to the patella. Step # 3: Tap briskly and observe extension of the knee or contraction of the quadriceps muscle. Test the Achilles (ankle) reflex bilaterally. Step # 1: With the legs still dangling, grasp the foot by the ball, and slightly dorsiflex it. Step # 2: Strike the tendon briskly. Watch for the intensity of the plantar flexion and how quickly it relaxes afterward. Test the Babinski reflex bilaterally. Step # 1: Use the wooden end of a tongue depressor, or the handle of the reflex hammer. Do not use any sharp object during this exam. Step # 2: Hold patient's ankle and gently stroke the plantar surface. Begin by the heel on the lateral side. Continue upward to the ball, then curve medically over the ball to the large toe. Note: This test should not be painful for the patient. Inform the patient that it may tickle a little or feel slightly uncomfortable. Test the finger-to-nose coordination bilaterally by positioning your finger 2 feet from patient's face at shoulder level. Then, ask patient to hold his/her head still. Have patient touch index finger to your finger, then to his/her nose, alternating back and forth several times. Student should move her finger several times, in different directions, so patient must accurately alter directions. Demonstrate to patient, while patient is watching, the difference between "sharp" (using the broken end of a Q-tip) and "light touch" (using a cotton ball). Instruct patient to close his/her eyes. Test light touch and sharp on upper extremities. With patient's eyes still closed, test light touch and sharp on lower extremities. 11 With patient's eyes still closed, test light touch and sharp on the trunk. Position Sense Demonstration. Step # 1: Grasp the large toe by the sides. Step # 2: To avoid confusion, demonstrate to the patient, while patient is watching, what is meant by up and down motion of the large toe. The joint must be completely relaxed. Position Sense Test: Must be done bilaterally. Step # 1: Ask patient to close the eyes, grasp large toe by the sides and then move the large toe in an up or down direction. Step # 2: Ask patient to tell you "up" or "down" after each motion. Vibratory Sense Demonstration: Step # 1: Use a low pitched 128 Hz tuning fork. Step # 2: Demonstrate to patient, while patient is watching you. Step # 3: Hold tuning fork near its base and activate it by tapping it on heel of your hand or by striking it with reflex hammer. Always press it to a bony prominence. Step # 4: Ask patient if s/he can feel the 'vibration'. Vibratory Sense Test: Step # 1: Ask patient to close eyes or to look away. Step # 2: Test the vibration sense in each ankle or each big toe using the 128 Hz tuning fork. Step # 3: Ask patient if she feels a "vibration" and then ask the patient to inform you of when the "vibration" stops. If you still feel the vibration when s/he cannot, s/he may have sensory loss. Note: Asking the patient to tell you when the vibration stops was not demonstrated on the video but is still required as part of the technique for this item. Testing for Peripheral Edema: Check each shin for pitting edema by pressing on the lower anterior tibia or medical malleolus, or dorsum of foot for 3-5 seconds. Note: Must examine both legs. Must be done on skin. Must be done for at least 3 seconds for credit. 12