Alternative antimicrobial drug(s) for treating penicillin
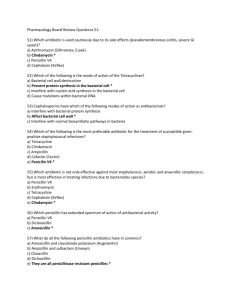
advertisement

Alternative antimicrobial drug(s) for treating penicillin-resistant S. aureus: A. vancomycin (Vancocin) B. nafcillin (Nafcil, Unipen) C. methicillin (Staphcillin) D. All of the above E. None of the above ANSWER: B Aminoglycosides antibacterial A. hetacillin B. aztreonam C. gentamicin (Garamycin) D. vancomycin (Vancocin) E. Clarithromicin ANSWER: C Antibacterials regarded as generally safe to prescribe in pregnancy. A. erythromycin B. cephalosporins C. tetracyclines D. All of the above E. None of the above ANSWER: A Antibiotic: Newborn toxicity due to impaired glucuronidation in infants A. chloramphenicol (Chloromycetin) B. tetracycline (Achromycin) C. ampicillin D. all E. neither ANSWER: A Bacterial cell wall synthesis inhibitor--like penicillins: A. bacitracin B. lincomycin (Lincocin) C. cephalosporin D. streptomycin E. none of the above ANSWER: C First generation cephalosporin: A. cefamandole (Mandol) B. cefaclor (Ceclor) and C. cefoxitin (Mefoxin) D. cephalexin (Keflex) E. none of the above ANSWER: D Fluoroquinone;effective in treating urinary tract infections (UTI) caused by multidrug resistant strains. A. isoniazid (INH) B. sulfasalazine (Azulfidine) C. ciprofloxacin (Cipro) D. streptomycin E. none of the above ANSWER: C Topical use only: A. penicillin B. bacitracin C. clindamycin (Cleocin) D. ampicillin E. none of the above ANSWER: B Which of the following is a short acting leukotriene synthesis (5-lipoxygenase) inhibitor? A. Zileuton B. Zafirlukast C. Montelukast D. Omalizumab E. Theophyline ANSWER: A Anti-inflammatory drugs are: A. prednisone (Deltasone) B. aspirin C. naproxen D. prednisone & aspirin E. prednisone, aspirin & naproxen ANSWER: E Analgesic effects of aspirin: A. peripheral action (inflammation) B. subcortical site of action C. decreasing PGE2 synthesis D. all the above E. neither ANSWER: D Aspirin may be fatal in taken in sufficient quantity. The syndrome of fatal salicyate overdose in children is characterized by A. marked hypotermia secondary to an antipyretic effect B. fever, tinnitus C. peripheral oedema D. disturbance in acid - base and electrolyte balance E. all of the above ANSWER: E Common adverse reactions of corticosteroidal therapy are: A. bradycardia, mental dullness B. anorexia, polyuria C. tachycardia, insomnia D. “moon face”, obese trunk E. all of the above ANSWER: D For a 6-year-old child with fever, what NSAIDs would be preferred? A. aspirin B. acetaminophen C. indomethacin D. ibuprofen E. all of the above ANSWER: B Glucocorticoid effects: A. inhibition of leukotriene production B. inhibition of prostaglandins C. increased chemotaxis D. inhibition of leukotriene production & inhibition of prostaglandins E. all of the above ANSWER: D NSAID primarily promoted as an analgesic, not as an anti-inflammatory agent: A. piroxicam B. ibuprofen C. naproxen D. ketorolac E. sulindac ANSWER: D The following is not true about corticosteroids: A. have anti-inflammatory activity B. highly lipophillic C. decrease the quantity and viscosity of mucus secretions D. decrease the synthesis of adrenergic mediators E. decrease the transcription of genes coding for pro-inflammatory cytokines ANSWER: D The following is not true about corticosteroids: A. have anti-inflammatory activity B. C. D. E. highly lipophillic decrease the quantity and viscosity of mucus secretions decrease the synthesis of adrenergic mediators decrease the transcription of genes coding for pro-inflammatory cytokines ANSWER: D What adverse effects are associated with chronic use of systemic corticosteroids? A. Candidosis B. Gastrointestinal complications C. Hypotension D. Hypoglycemia E. all of the above ANSWER: B A pharmacologic agent which has the potential to cause increased biliary tree pressure is: A. morphine B. warfarin C. phenytoin D. acetazolamide E. carbon tetrachloride ANSWER: A All of the following statements regarding acetaminophen toxicity are true EXCEPT: A. acetaminophen is the principal metabolic product of phenacetin B. an overdose of 10 grams or more may produce hepatic necrosis in adults C. acetaminophen overdose may produce transient azotemia or renal failure D. forced diuresis may be a useful form of therapy for acetaminophen overdose E. liver pathology is centrilobular and midzonal necrosis ANSWER: D Anesthetic associated with the highest incidence of hepatitis. Anesthetic Partition Minimum Alveolar Coefficient Concentration (MAC) A. halothane B. enflurane C. nitrous oxide D. isoflurane E. methoxyflurane ANSWER: A Anesthetic that must be administered in a lipid diluent due to poor aqueous solubility. A. thiopental B. propofol C. ketamine D. etomidate E. fentanyl ANSWER: B Aspirin is a nonopioid analgesic which is thought to work by inhibiting: prostaglandin reductase, prostaglandin synthetase, thromboxane synthetase, cyclooxygenase A. prostaglandin reductase, prostaglandin synthetase, thromboxane synthetase B. prostaglandin reductase, thromboxane synthetase C. prostaglandin synthetase, cyclooxygenase D. cyclooxygenase only E. All of the above ANSWER: C Characteristically observed in individuals following acute overdose of opioids. A. pinpoint pupils B. depressed respiration C. coma D. convulsions E. All of the above ANSWER: A FALSE statement regarding ketamine as an anesthetic: A. contraindicated in a patient with asthma because it may cause bronchoconstriction B. recovery from anesthesia associated with emergence phenomenon of hallucinations and vivid dreams C. produces dissociative anesthetic state, whereby patient appears awake but is unconscious D. produces analgesia E. None of the above ANSWER: B Histamine-1 receptor antagonists include: A. ranitidine B. nizatidine C. famotidine D. diphenhydramine E. All of the above ANSWER: D Morphine's affects the eye by: A. producing miosis through an action on the oculomotor nerve B. producing mydriasis through an action on the sympathetic system C. decreasing pupillary responses to light D. directly acting on the smooth muscles of the iris E. directly acting on extrinsic muscles of the eye ANSWER: A Neuropathic pain is often characterized by episodes of: A. Achy pain B. Colicky pain C. Gnawing pain D. Shock-like pain E. Squeezing pain ANSWER: D Pain that is described as “dull, achy” and is well localized, is best described as: A. Autonomic pain B. Neuropathic pain C. Somatic pain D. Vascular pain E. Visceral pain ANSWER: C Drugs which may increase gastric wall permeability include: A. erythromycin B. indomethacin C. nitrofurantoin D. aspirin E. indomethacin & aspirin ANSWER: E The maximum recommended daily dose of acetaminophen is: A. 2 grams B. 4 grams C. 6 grams D. 8 grams E. 10 grams ANSWER: B The most important supplemental therapy to consider when starting patients on opioids for pain is: A. Amphetamines to increase alertness B. Antidepressants to supplement pain relief C. Antiepileptic medications to treat neuropathic pain D. Laxatives to prevent constipation E. Non-steroidals (NSAID’s) to treat inflammation ANSWER: D The pharmacologic effects of morphine include all EXCEPT: A. behavioral changes B. miosis C. respiratory depression D. diarrhea E. postural hypotension ANSWER: D Which of the following antitubercular agents is associated with the development of ototoxicity? A. rifampin B. ethambutol C. isoniazid D. streptomycin E. para-aminosalicylic acid ANSWER: D Which of the following antibiotics is most closely associated with the development of hepatitis? A. kanamycin B. penicillin G C. tetracycline D. isoniazid E. ethambutol ANSWER: D Aminoglycosides A. must be dosed on the basis of renal function; are primarily active against gram-negative aerobes; are not active against anaerobes B. must be dosed on the basis of renal function; are not active against anaerobes C. primarily active against gram-negative aerobes, penicillin may be synergistic against enterococcus D. penicillin may be synergistic against enterococcus only E. All of the above ANSWER: E Antibacterials regarded as generally safe to prescribe in pregnancy. A. erythromycins B. cephalosporins C. tetracyclines D. erythromycins & cephalosporins E. none of the above ANSWER: D Azole most likely to get into the cerebral spinal fluid (CSF): A. ketoconazole B. itraconazole C. fluconazole D. all of the above E. none of the above ANSWER: C Bactericidal drugs that act by inhibiting DNA gyrase A. Aminoglycoside B. Fluoroquinolones C. Macrolides D. Rifamycins E. Sulfonamides ANSWER: B Combination of metronidazole (Flagyl) and penicillin in treating an abscess caused by beta-lactamase producing Bacteriodes and anaerobic streptococci is an example of: A. synergistic drug treatment B. antagonistic drug effects C. additive drug effects D. all of the above E. none of the above ANSWER: C Combination of these two drugs would produce an antagonistic (undesirable) antimicrobial effect when treating an infection A. Amoxicillin+ gentamicin B. Cephalexin+ gentamicin C. Sulfamethoxazole+ trimethoprim D. Tetracycline+ amoxicillin E. Vancomycin+ gentamicin ANSWER: D Females with odorless, white or yellow cheesy discharge with itching. Possible diagnosis A. Chalymida B. Syphilis C. Chalmdyia D. Candidias E. none of the above ANSWER: D Given by i.v. administration, the drug of choice for nearly all life-threatening mycotic infections--usually used as the initial induction regimen A. ketoconazole B. itraconazole C. flucytosine D. amphotericin B E. nystatin ANSWER: D Impaired vision is an adverse effect of: A. carbenicillin B. ethambutol C. rifampin D. colistin E. cycloserine ANSWER: B Inhibits the formation of folic acid by competing with PABA for dihydropteroate synthase A. Metronidazole B. Rifampin C. Sulfamethoxazole D. Trimethoprin E. Linezolid ANSWER: C More likely to cause polyneuritis in patients who are"slow acelators"; this antibiotic is inactivated by the liver. A. clindamycin (Cleocin) B. isoniazid (INH) C. nafcillin (Nafcil, Unipen) D. vancomycin (Vancocin) E. none of the above ANSWER: B Most potent of the presently available anti-fungal azoles: A. fluconazole B. itraconazole C. ketoconazole D. all of the above E. none of the above ANSWER: B Ototoxicity and nephrotoxicity associated with this antibiotic: A. cefotaxime (Claforan) B. amikacin (Amikin) C. aztreonam (Azactan) D. ceftriaxone (Rocephin) E. All of the above ANSWER: B Properties of tetracycline (Achromycin): A. inhibitor of bacterial cell wall synthesis B. dug of choice in treating typhus C. cleared primarily by the liver D. inhibitor of bacterial cell wall synthesis & dug of choice in treating typhus E. none of the above ANSWER: B Rifampicine is used mainly in the treatment of : A. Cholera B. Typhoid fever C. Tuberculosis D. Rickettsial diseases E. Pseudomonas infections ANSWER: C Special concerns in using antimicrobials in newborns and young children: A. sulfonamides can be safely given to newborns B. tetracyclines should not be administered to children betlow the age of eight C. newborns should not be given chloramphenical because they are unable to metabolize the drug adequately. D. tetracyclines should not be administered to children betlow the age of eight & newborns should not be given chloramphenical because they are unable to metabolize the drug adequately. E. none of the above ANSWER: D Synergistic antimicrobial combination: A. amoxicillin-clavulanate B. ampicillin -streptomycin C. sulbactam-ampicillin D. all of the above E. none of the above ANSWER: D The structure is administered along with a penicillin in a preparation known as Tazocin or Zosyn. Which penicillin is used? A. Amoxicillin B. Piperacillin C. Ampicillin D. Methicillin E. None of the above ANSWER: B The combination of sulfamethoxazole and trimethoprim is a useful drug for treating UTIs. Bacterial resistance to trimethoprim occurs primarily by A. Acetylation of trimethoprim B. Acetylation of the drug receptor C. Decreased bacterial uptake D. Upregulation of dihydrofolate reductase E. Upregulation of beta-lactamase ANSWER: D The drug of choice for Streptococcus pneumonia (pneumococcus) in a patient with no drug allergies is: A. erythromycin B. penicillin C. vancomycin D. ceftriaxone E. gentamicin ANSWER: B What crucial feature of a penicillin is involved in its mechanism of action? A. Carboxylic acid B. beta-lactam ring C. Acyl side chain D. Thiazolidine ring E. All of the above ANSWER: B What drugs are present in the preparation Augmentin? A. Ticarcillin and clavulanic acid B. Ampicillin and sulbactam C. Ampicillin and clavulanic acid D. Amoxicillin and clavulanic acid E. None of the above ANSWER: D Which form of resistance to the effect of antimicrobial drugs is specific to beta-lactam type antibiotics A. Decreased drug uptake B. Methylation of the antibiotic’s receptor C. Decreased metabolic activation D. Altered amount of drug receptor E. Increased enzymatic destruction of the antibiotic ANSWER: E Which of the following antibiotics is most closely associated with the development of renal and ototoxicity? A. kanamycin B. C. D. E. penicillin G tetracycline isoniazid ethambutol ANSWER: A Which of the following antimicrobial drugs is bactericidal A. Azithromycin B. Doxycycline C. Erythromycin D. Gentamicin E. Tetracycyline ANSWER: D The state of “general anesthesia” usually includes: A. Analgesia B. Loss of consciousness, C. Inhibition of sensory and autonomic reflexes D. Amnesia E. All of the above ANSWER: E An ideal anesthetic drug would: A. Induces anesthesia smoothly and rapidly B. Secure rapid recovery C. Posses a wide margin of safety D. Be devoid of adverse effects E. All of the above ANSWER: E Which of the following general anesthetics belongs to inhalants? A. Thiopental B. Desfluran C. Ketamine D. Propofol E. Diprofol ANSWER: B Indicate the anesthetic, which is used intravenously: A. Propofol B. Halothane C. Desflurane D. Nitrous oxide E. All of the above ANSWER: A Indicate the intravenous anesthetic, which is an ultra-short-acting barbiturate: A. Fentanyl B. Thiopental C. Midazolam D. Ketamine E. Propofol ANSWER: B Indicate the intravenous anesthetic, which is a benzodiazepine derivative: A. Midazolam B. Thiopental C. Ketamin D. Propofol E. Fentanyl ANSWER: A Which of the following intravenous anesthetics has antiemetic actions? A. Thiopental B. Propofol C. Ketamine D. Fentanyl E. All of the above ANSWER: B A 44-year-old patient has ischemic heart disease, angina on exertion, II functional class. What is the drug of choice in treatment of acute attack? A. Platelet inhibiting agents B. Nitroglycerin sublingually or in spray form C. Spasmolitics IV D. Digitalis IV E. Sedative agents orally ANSWER: B A 45-year-old men with diagnosis: Paroxysmal arrhythmia. Arterial hypertension II. Drug of choice for stopping attack: A. Metoprolol B. Nitroglycerin C. Potassium chloride D. Digoxin E. Lidocain ANSWER: A A 45-year-old women with diagnosis: Paroxysmal arrhythmia. Arterial hypertension II. Drug of choice for stopping attack: A. Anaprilin B. Nitroglycerin C. Potassium chloride D. Digoxin E. Lidocain ANSWER: A A 60-year-old women has stenocardia on exertion II functional class. Taking of nitroglycerin potentiate a sever headache. Which of the following drugs is the most useful in this case? A. Amiodaron B. Molsidomin C. Nifedipine D. Propranolol E. Verapamil ANSWER: B A 61-year-old patient complains of intensive and prolonged retrosternal pains, decreased exercise tolerance for 4 days. Which of the following groops is the most useful? A. ACE inhibitors B. dyslipidemic drugs C. beta-blockers D. nitrates E. digitalis ANSWER: D A drug, or class of drugs, that has been documented to reduce mortality following a myocardial infarction: A. Class Ia antiarrhythmics B. Class Ic antiarrhythmics C. Class II antiarrhythmics D. Class III antiarrhythmics E. digoxin ANSWER: C A man 36 years old has arterial hypertension. Which group of drugs may be used for her treatment? A. Betaadrenomimetics B. Bet-blockers C. Glucocorticoids D. Preparations of calcium E. M-cholinolitics ANSWER: B A patient has arterial hypertension with bradyarrhythmia. Which of the following drugs is necessary to administer? A. Nifedipine B. Klonidine C. Propranolol D. Diltiazem E. Methyldopa ANSWER: A A patient has bronchial asthma for a long time. Angina pectoris attacks have appeared recently Which of the following drugs is contraindicated? A. Propranolol B. Molsidomin C. Nifedipine D. Carvedilol E. Aspirin ANSWER: A A side effect of furosemide that can increase the automaticity of ectopic cardiac pacemakers: A. hypercalcemia B. hyperkalemia C. hypokalemia D. hyponatremia E. hypothyroidism ANSWER: C Acebutolol is A. Beta-adrenoreceptor antagonist B. Calcium channel blocker C. Beta-adrenoreceptor agonist D. Angiotensin II receptor antagonists E. ACE inhibitor ANSWER: A Adverse effects of organic nitrates are: A. nausea and constipation B. bradycardia, bronchospasm, heart failure C. peripheral edema, headache, heart failure D. throbbing headache, dizziness, tachycardia E. lightheadedness, weakness, peripheral edema ANSWER: D Adverse effects of beta-adrenergic blocking agents are: A. bradycardia, bronchospasm, heart failure B. hypotension, dizziness, lightheadedness C. headache, heart failure, pulmonary edema D. nausea and constipation E. hypotension, dizziness, tachycardia ANSWER: A Agents which may lower circulating plasma lipids include: A. Clofibrate B. Nicotinic acid C. Cholestyramine D. Dextrothyroxine E. All are correct ANSWER: E All of the following statements concerning nitroglycerin are correct EXCEPT: A. It causes an elevation of intracellular cGMP B. It undergoes significant first-pass metabolism in the liver. C. It may cause significant reflex tachycardia D. It can not cause throbbing headache E. It can cause postural hypotension ANSWER: D Antihypertensive drugs belonging to the same class: A. doxazosin (Cardura), prazosin (Minipress), metoprolol (Lopressor) B. nifedipine (Procardia, Adalat), verapamil (Isoptin, Calan), diltiazem (Cardiazem) C. clonidine (Catapres), guanabenz (Wytensin),terazosin (Hytrin) D. lisinopril (Prinvivil, Zestril), fosinopril (Monopril), guanadrel (Hylorel) E. None of the above ANSWER: B Calcium channel blockers with prolong action: A. Nifedipine B. Verapamil C. Diltiazem D. Amlodipine E. Nebivolol ANSWER: D Diltiazem: A. decreases calcium entry through L type channels B. increases total peripheral resistance C. increases cardiac output D. increases heart rate E. increases gastrointestinal motility ANSWER: A During a treatment, patient develops a drug-induced dry cough. The drug(s) possibly responsible for this cough is (are): A. propanolol B. indomethacine C. captopril D. furosemide E. acetaminophen ANSWER: C GI problems—nausea, vomiting, flatulence, constipation or diarrhea, abdominal discomfort are the most common adverse effects of: A. dyslipidemic drugs B. calcium channel blockers C. beta-adrenergic blocking agents D. nitrates E. diuretic drugs ANSWER: A In the treatment of exertional angina: A. nitroglycerin reduces O2 demand by decreasing preload B. nitroglycerin increases O2 supply by dilating atherosclerotic vessels C. attacks frequently occur during sleep D. nitroglycerin increases cardiac myocyte cAMP levels E. beta blocking agents have no beneficial action ANSWER: A Indicate the antiarrytmic drug from of adrenoblockers group A. Nitroglycerin B. Amiodaron C. Metoprolol D. Verapamil E. Asparcam ANSWER: C Indicate the side effect of nitroglycerine A. Itching of skin B. Bradicardia C. Headache D. Rise of arterial pressure E. Intestine atony ANSWER: C Inhibits 3-hydroxy-3-methylglutaryl CoA reductase, the rate-limiting step in cholesterol synthesis: A. Atorvastatin B. Niacin C. Cholestyramine D. Clofibrate E. Probucol ANSWER: A is a specific alpha-adrenergic antagonist: A. Prazosin B. Timolol C. Labetalol D. Atenolol E. Sotalol ANSWER: A Isosorbide dinitrate: A. Antiarrhythmic action is via beta-adrenergic blockade B. Ventricular premature depolarizations C. Angina pectoris prophylaxis D. Conversion of atrial fibrillation to sinus rhythm E. Treatment of ventricular fibrillation ANSWER: C Mechanism of action:diltiazem (Cardiazem) A. phosphodiesterase inhibitor B. blockade of calcium channels C. alpha-1 receptor antagonists D. beta-1 receptor antagonist E. all of the above ANSWER: B What diuretic has potassium-sparing action? A. Furosemide B. Mannitol C. Dihlothiazid D. Triamterene E. Urea ANSWER: D What diuretic is belonging to osmotic diuretics? A. Spironolactone B. Mannitol C. Furosemide D. Dihlothiazid E. Triamterene ANSWER: B What diuretic is used for forced diuresis? A. Dihlothiazid B. Triamterene C. Spironolactone D. Furosemide E. Diacarb ANSWER: D The major causes of hypocalcemia in the adult are: A. Hypoparathyroidism B. Vitamin D deficiency C. Renal failure and malabsorption D. All of the above E. None of the above ANSWER: D Interactions of calcium drugs with ________ is: A. Ethanol: decreases absorption B. Loop diuretics: increase renal excretion C. Glucocorticoids: stimulate renal excretion D. All of the above E. None of the above ANSWER: D