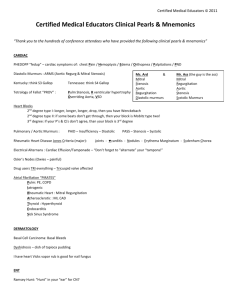
Chest 1. Which one is not true for sternal angle? A. It is also termed
advertisement

Chest 1. Which one is not true for sternal angle? A. It is also termed Louis angle. B. It is formed by the protrusion of the conjunction composed of sternum and manabrium sterni. C. It acts as an important landmark for counting rib(parallel to third rib) and interspace. D. It indicates the bifurcation of the trachea, the upper level of the atria of heart, the demarcation of upper and lower part of mediastinum, and the fifth thoracic vertebra as well. KEY: (C) 2. The depressed region above the clavicle, which corresponds to the upper part of each lung apex, is called( ). A. Suprasternal fossa B. Supraclavicular fossa C. Infraclavicular fossa D. Suprascapular region KEY: (B) 3. Barrel chest is often seen in ( ). A.tuberculosis B.emphysema C.chronic hectic disease D. pneumonia. KEY: (B) 4. Subcutaneous emphysema at chest is commonly due to the following EXCEPT( ). A. injuries of lung B. injuries of trachea C. injures of pleura D. local infection of bacillus aerogenes KEY: (D) 5. How to describe the mass of breast in terms of palpation ? ①Location: The exact location of the mass must be designated. General method is to take the nipple as the central point, describe the mass according to the clock numbers and axis. Furthermore, the distance of the mass from the nipple must be recorded for the sake of accurate location of the mass. ② Size: The mass must be described in length, width and thickness, for the comparison in the future to determine if it progresses or regresses. ③Contour: pay attention to whether the mass is regular or irregular, the margin is dull or acute, and whether it adheres to surronding tissue or not. Most benign tumors have a smooth, regular contour, whereas most malignant masses are convavoconvex, with firmed margin. However, it must be mentioned that inflammatory lesions may also have an irregular contour. ④ Consistency: The hardness must be described clearly. It may be described generally as soft, cystic, moderately firm or extremely hard. A benign tumor is usually felt soft, cystic; while a firm consistency mass with irregular contour usually denotes 1 a malignant lesion. However, a hard region may also be caused by inflammation. ⑤ Tenderness: It should be ascertained whether or not the lesion is tender, and, if so, to what degree. An inflammatory process is usually moderately or markedly tender, whereas most malignant lesions are not obviously tender. ⑥Mobility: The examiner should determine whether the lesion is freely movable. If it is movable in certain directions, or fixed, he must determine wether the mass is fixed to the skin, to the deep structures, or to the surrounding breast tissue. Most benign lesions have a large mobility, inflammatory lesion is considerably fixed, and a malignant lesion in early stage is movable, however, as the process developes, it becomes fixed because other structures are invaded. Lung 6. Deep slow breathing (Kussmaul’s respiration) is typical of ( ). A.alkalosis B.acidosis C.hypernatremia D.hyponatremia KEY: (B) 7. Tachypnea indicates the increased respiratory rate, over ( A.20 B.22 C.24 D.26 KEY: (C) ) per minute. 8. Which of the following is wrong for the lower boundary of lung? A. the anterior part which begins from the sixth rib B. at the level of the sixth interspace along the midclavicuar line C. at the level of the eighth interspace along the midaxillary line D. the posterior part of the lower boundary that approaches horizontal line at the ninth rib level by the inferior angle line KEY: (D) 9. Which of the following is incorrect? A.Tidal breathing is also called cheyne-stokes respiration. B. Cheyne-stokes respiration waxes and wanes cyclically so that periods of deep breathing alternate with periods of apnea (no breathing). C. Ataxic breathing is characterized by unpredictable irregularity. Breaths may be shallow or deep, and stop for short periods. D. Ataxic breathing is less severe than the tidal breathing. KEY: (D) 10. Fremitus is decreased or absent in the following conditions EXCEPT( A. obstructed bronchus or chronic obstructive pulmonary disease. B.pleural effusion C. pneumonia D. fibrosis KEY: (C) ). 11. Hyperresonance can be heard during the percussion of ( ) A. pneumonia B. emphysema 2 C. .tuberculosis KEY: (B) D. pleural effusion 12. Which one is not true for bronchial breathing? A. Bronchial breath sounds are in general higher in pitch than vesicular or bronchovesicular sounds. B. Expiration usually surpasses inspiration in length. C. Bronchial breathing is normally heard over the lungs. D. It occurs only with pulmonary consolidation. KEY: (C) 13. The increase of vesicular breath sounds may indicate ( ). A. pleural fluid B.fever C. foreign body in trachea D. pneumatothorax KEY: (B) 14. One of the most common causes of decreased or absent breath sounds is (). A. pneumothorax B. fluid in the pleural space C. empyema D. complete bronchial obstruction KEY: (B) 15 Which of the following characteristic is incorrect for moist rale? A. It is formed because of there present stricture or partial obstruction of the trachea, bronchi or bronchioles, B.It is formed due to the passage of air through thin secretions in the respiratory tract. C.It can be caused by exudate, sputum, blood, mucus, or pus. D.The sound may diminish after cough. KEY: (A) 16. Please describe the etiology and characteristics of moist rales and rhonchi. Moist rale: produced due to passage of air through thin secretions in the respiratory tract, such as exudate, sputum, blood, mucus, or pus etc. The sound could also be regasded as crackles produced by reopening of the bronchials at inspiration when bronchiolar wall adheres and closes because of tenacious secretion at expiration. Characteristics of moist rales: adventious sounds besides breath sound, discrete and short in time, often series of jeveral sounds appear, siginificant in inspiration or in the terminal phase of inspiration, present sometimes in the early phase of expiration, the location is rather fixed, quality not variable, medium and fine rale could be present simultaneously, it may diminish or disappear after cough. Rhonchi: produced because there present stricture or partial obstruction of the trachea, bronchi or bronchioles, air through these passways becomes turbulent, the pathologic basis for which is inflammatory membranous congestion and edema oversecretion, bronchial muscular spasm, obstruction due to tumor and foreign bodies in the bronchial lumen, and stricture due to oppressian of extraluminal enlarged lymph nodes or mediastinal tumors. Characteristics of rhonchi: they are continuous, relatively long, and musical adventious breath sound. Rhochi are rather high-pitched with the basic frequency of about 300-500 Hz. Audible both during inspiration and expiration, in general more prominent during expiration. Rhonchi are easily variable in intensity, quality and 3 location, sometimes they change obviously instantly. 17. Try to make differential diagnoses among consolidation of lung disease, emphysema, atelectasis, pleural diffusion and pneumothorax inspection Chest appearance Cons olidat ion Symmetrica l Emph ysem a Atele ctasis Barrel-shap ed Pleur al dffusi on Fullness of the affected side Thick ened pleura Denting of the affected side pneu moth orax Fullness of the affected side Denting of the affected side Respirato ry movemen t Diminish ed on the affected side Diminish ed on both sides Diminish ed on the affected side Diminish ed or disappear anced on the affected side Diminish ed on the affected side Diminish ed or disappear anced on the affected side palpation Trachea location Vocal fremitus Central Increased on the affected side Diminish ed on both sides Diminish ed or disappear ed Central Deviate toward the affected side Deviate toward the normal side Deviate toward the affected side Deviate toward the normal side Percussio n Note Dullness or flatness Hyperres onance Dullness Auscultation Breath sound rale Vocal resonance Bronch ial breath sound Dimini shed Moist rale Strengthened Always without Diminished Disapp Withou Disappeared or eared t diminished or diminis hed Dimini Withou Diminished or shed or t disappeared disappe ared Diminish ed or disappear ed Flatness Diminish ed Dullness Dimini shed Withou t Diminished Diminish or disappear ed Tympany Dimini shed or dissape ared Withou t Diminished or disappeared 4 Heart 18. The best way to make distinction between pleural friction sound and pericardial friction sound is( ) A.sound timing B. sound quality C.sound relation with respiration D.sound location KEY: (C) 19. Which one is not true for gallop rhythm? A. It is the pathologic counterpart of the S3 and occurs at the time of rapid diastolic ventricular filling. B. It is a brief low-pitched sound. C. It occurs at middle diastole at the end of rapid filling phase of diastole. D. It reflexes that the RV function is decreased. KEY: (D) 20. Continuous murmur can be heard in ( ). A. Mitral Stenosis B. Mitral Insufficiency C. Aortic Stenosis D. Patent Ductus Arteriosus KEY: (D) 21. How to differentiate between S1 and S2? 1) S1 apex pitch , lasting time S2 basic, pitch lasting time 2) Duration: S1__S2 S2__S1 3) Apical pulse 22. Describe the characteristics of atrial fibrillation in terms of Auscultation. (1) The ventricular rhythm has absolutely no regularity; (2) The intensity of S1 is inconsistence; (3) The rate of heart and pulse are unconcerned. 23. Explain the term auscultatory valve area. l. Mitral valve area: it is at the apex, in the fifth left intercostal space, medial to the midclavicular line. 2. Aortic valve area: there are two auscultatory area of AV, one is located in the second right intercostal space, just lateral to the sternum. The other is at the third or fouth intercostal space, left to the sternum border. We call it the second auscultatory area of AV. 3. Pulmonary valve area: in the second intercostal space just lateral to the sternum. 4. Tricuspid valve area: at the lower part of the sternal near the xiphoid. .The physician should adopt a systematic way of listening: start at the apex, then move to the PV area , AV area, second AV area, TV area. 24. Do you know the mechanisms of heart murmurs? l). Increased velocity of blood flow though normal valves; 2). Forward flow though narrowed or deformed valves; 5 3). Backward or regurgitant flow through incompetent valve; 4). Abnormal connection; 5). Vibration of loose structure within the heart; 6). Increase with diameter of a major vessels. 25. Try to make distinction between functional murmur and organic murmur. Age Location Quality Timing Intensity Thrill functional child,younger apex or pulmonary valve area: blowing,tender short <3/6 negative Radiation not long organic any age people any location harsh long,in all systolic period ≥3/6 positive long,transmitted with the direction of the bloodstream 26. Paradoxical pulse can been found in ( ). A. constrictive pericarditis B.cardiac infarction KEY: (A) C.shock D. anemia 27. Could you tell us the definitions and classifications of blood pressure levels? Category systolic(mmHg) diastolic(mmHg) Optimal <120 <80 Normal <130 <85 High-normal 130-139 85-89 Hypertension ≥140 ≥90 Isolated systolic ≥140 <90 hypertension 28.The most important sign indicating aortic incompetence is (): A. Decrease in intensity of S1 B. Boot-like heart C. Diastolic murmurs in aortic area D. Austin-flint's murmurs in apical area E. Water hammer pulse KEY: (C) 29.Graham-stell's murmur means (). A. diastolic murmur in the apical area caused by structural mitral stenosis B. diastolic murmur in aortic area caused by aortic incompetence C. diastolic murmur in pulmonic area caused by relatively pulmonic incompetence D. diastolic murmur in apical area caused by relatively mitral stenosis E. diastolic murmur caused by relatively tricuspid stenosis KEY: (C) 30.Which sign refers to structural heart disease? A. lifted apex beat 6 B. displacement of the apical impulse to the left C. percussion of dullness extended bilaterally D. systolic murmurs in apical area E. wide splitting of S2 in pulmonary area KEY: (C) 31.Which of the following characteristic is wrong as to S3? A. a lower pitched sound than S2 B. shorter duration C. easily heard at supine or left lateral decubitus D. more clear in the area inner and superior to the cardiac apex E. more clear at the end of inspiration KEY: (E) 32.Which of the following characteristic is not consistent with the increase in the intensity of S1? A. aortic incompetence B. ventricular premature beats C. mitral stenosis D. LGL syndrome E. atria and ventricle apartness KEY: (A) 33.Which factor that may influence the intensity of heart murmurs is not correct? A. Weaker murmur means less stenosis. B. Faster the blood flows, louder the murmur. C. The greater difference of pressure between two borders of the stenosis makes the murmur louder. D. Stronger contraction makes murmur louder. E. The most severe stenosis doesn't mean the loudest murmur. KEY: (A) 34.Which of the following characteristic is not consistent with the typical diastolic murmur in mitral stenosis? A. increase in early and mid diastolic phase B. increase in late diastolic phase C. localized D. louder in the apex area E. not accompanied by S4 KEY: (A) 35.Which of the following can occur in left ventricular failure? A. water hammer pulse B. pulsus tardus C. dicrotic pulse D. pulsus alternans E. pulsus paradoxus KEY: (D) 7 36.Which is the most typical test for diagnosing mitral stenosis? A. ECG B. chest X-ray C. increase in S1 D. subcutaneous nodus E. not all above KEY: (E) 37.Lifted apical impulse is most commonly seen in: A. pulmonic heart disease B. cardiomyosis C. right ventricular hyperplasia D. hypertension heart disease E. not all mentioned above KEY: (E) 38.In blood pressure testing, straitly curve will: A. increase B. decrease C. not change D. cause pulse pressure to decrease E. cause diastolic pressure to decrease and pulse pressure to increase KEY: (A) 39.Which of the following characteristic is not consistent with splitting of the S2? A. loss of synchronization in closure of aortic and pulmonary valves B. most clearly heard at the end of inspiration C. paradoxical split of S2 may be caused by right bundle branch block. D. fixed split of S2 is mainly due to atrial septal defect. E. it can be heard in physical and pathological situations. KEY: (C) 40. To describe the symptoms and signs of mitral stenosis. The Symptoms are dyspnoea, hemoptysis, cough, wheezing, and hoarseness. Other symptoms such as chest pain, thromboembolism, and infective endocarditis could be manifested. Signs include mitral facies, in particular pinkish-purple patches on the cheeks, normal or small arterial pulse, a prominent jugular venous pulse wave, an inconspicuous left ventricle, opening snap occurring later at the apex, and low-pitched, rumbling diastolic murmur. 41. To illustrate the definition and clinical significance of ventricular gallop. It is also called S3 gallop or protodiastolic gallop, with low intensity and pitch, occurring after S2, most clearly heard in the apex at the end of the expiration and weakened during inspiration. Clinical value is implicated in low left ventricular function, hard burden in the diastolic period and severe myocardiopathy, which means lower EF or CI but higher PCWP, left atrial pressure and left ventricular congestion. 8 9