TERMS:
advertisement

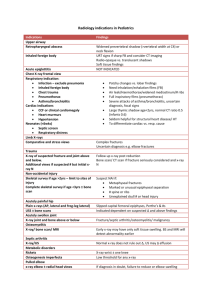
X-ray Diagnosis Tri 6 1 TERMS: Osteopenia – reduced bone mass; decreased bone density. Radiolucent – clear to X-ray photography (appears black). Radiopaque – X-ray dense or absorbed (appears white from X-ray absorption). Cortical bone, trabecular bone, muscle, water, air, fat Contrast (image) – differentiation, generally in black and white. High contrast = reduced grayscale. Differential absorption – different absorption properties of different materials based on atomic properties. Contrast (i.e. oral, bronchogram, angiography [arteriograms and venograms], arthrogram, air-sinogram) – foreign substance introduced to the body that yields high contrast radiography. Metastasis – beyond stasis; malignant cancer or infection. DESCRIBE TYPES OF BONE DEVELOPMENT: Intramembranous and enchondral. Intramembranous – primarily flat bones (facial, calvaria, ilia). Periosteal tissue maintains bone via periosteum and endosteum. Bone repair following fracture ensues via this method. Enchondral – classic manner of long bone formation; formed in chondral tissue. Hematopoietic sites in a: Child: bones (all). Necessary for growth and development. Adult: ends of the longs bones (metastasis) and flat bone (pelvis, sternum, ribs, and spine). Geriatric: Reduced to smaller areas of the metastases and spine, ribs, ilium) Draw a femur and label the parts: Greater trochanter Lesser trochanter Shaft Neck Head Fovia capitis Medial condyle Lateral condyle Medial epicondyle Lateral epicondyle Linea aspira Nutrient foramen Growth plates Intertrochanteric line Epiphysis Metaphysis Periosteum Cortex Why do we use X-ray? Proper use of X-ray is for attempting to document the differential or confirm a diagnosis: Trauma Mammography or other familial disease Review of systems When do we use radiology? General procedure for a patient: Paperwork X-ray Diagnosis Tri 6 2 Interview and consultation History (LOPPQqRSTTxB) Inspection and PE Palpation Percussion Instrumentation ROM Orthopedic Neurologic Document clinical findings and derive a differential diagnosis Appropriate time for report of findings, or release the patient, or accept the person as a patient with contractual obligations. E X-ray Lab There are exceptions to following the above protocol. Documentation: Liability: GP read all films – held as specialist in X-ray in court. GP reads some films and sends others - held as specialist in X-ray in court. GP sends all – GP liability only. Basically, this translates to only two levels of liability. Chiropractic radiologists 71.00 Skeletal radiologists and fellows Chiropractic radiology residents General medical radiologists Medical radiology residents Medical clinicians Chiropractic clinicians Chiropractic students Medical students 70.18 61.54 51.64 44.64 31.26 28.38 20.45 05. Rule in, rule out, or monitor a know condition all with proper documentation is purpose for taking X-ray. It is easy to sue for low initial court filing costs. Some recommend that you not let a patient’s bill get over $200. Much of what we learn has design to protect against legal suits. Often it is more profitable to outsource as much as possible to reduce liability. HOW DO WE COMMUNICATE THE RESULTS: The X-ray report has design to verbally communicate the X-ray status. Useful to communicate between doctors and offices. X-ray Diagnosis Tri 6 To allow investigation by other specialists. X-ray report is satisfactory replacement of X-ray film. Attorneys need reports to make a case. Workers Comp and Insurance have reviews for reimbursement. The patient pays for the information derived from the X-ray but not the X-ray itself. Additionally, the doctor has legal obligation to maintain the X-ray records. INFORMATION ON AN X-ray REPORT: I. Imaging center (who is interpreting the report). II. Patient information (who, age, DOB). III. Radiographic information (date of exam, series, technique [mA x time x kVp] optional normally in a logbook). IV. Body of report: generic, descriptive, in the fewest words possible (with use of “buzzwords”). V. Impressions: interpretation noted (differential diagnosis from most important to least important). VI. Recommendation/comment (optional) – Dr. Kuhn says to rarely use this part. IMAGING TOOLS AVAILABLE Know about the study, cost, and what it will do or not do. Have the ability to communicate the method to a patient. Imaging tools Plain film Myelography Computerized tomography Helical Computerized tomography MRI Bone scan SPECT Plain film – Wilhelm Conrad Roentgen (11/8/1895) Strengths: availability, relatively low cost, well known usage. Weaknesses: ionizing radiation, relatively poor resolution, poor spatial localization, soft tissues generally not seen. Proper use: introductory study, can evaluate IVF well, use to rule out contraindications for advanced imaging, not good for central canal stenosis. Conventional tomography – largely replaced by CT. 1. Linear. 2. Circular. 3. Elliptical. 4. Hypocycloidal. 5. Trispiral. Myelography Production: utilizes ionizing radiation, depends on displacement of contrast column, differential absorption. - air was the first contrast agent used. Other materials include poppy seed oil, pantopaque. In the 1940’s water soluble products (very toxic). 1970 metrizamide non-ionic, water soluble, in use today. 3 X-ray Diagnosis Tri 6 4 Complications: arachnoiditis, infections, arterial bleeding, headache is the most common complication. Proper use: Disc herniation – sharp angular indentation on the thecal sac, decreased IVD, enlargement of a nerve root sleeve secondary to edema, displacement of non-filling of a root sleeve. If CT or MR are not available Patient who cannot undergo MRI because of time, size, claustrophobia, other contra-indications May be used in conjunction with CT. Weakness: more expensive than MRI, ionizing radiation, relatively poor resolution, soft tissues not well seen, high rate of false negatives, potential complications from contrast agent. Strengths: relatively good availability, good cost benefit ratio, well known utilization. Computerized Tomography: Technical aspects: ionizing radiation, absorption differentials, computer generated pictures, Hounsfield unit, pixels, voxels, volume averaging, slice thickness scout films. Best thing it does is axial imaging. Strengths: widely available, improved visualization of soft tissues, can provide three dimensional imaging, accurately measure a variety of structures, image manipulation possible. Only 1-3 percent change in bone density will show up on CT. Allows for a change in parameters to view different level(s) and window(s). Weaknesses: higher cost than plain film and lower than cost MRI, ionizing radiation, intracranial artifacts, artifacts secondary to metallic implants, dose is a consideration. Proper use: very good axial images, excellent bone detail, some application in the neurology work-up. Vacuum phenomena – air trapped in what was nucleus pulposis. Vacuum cleft – air trapped in what was the annulus fibrosis. Helical computerized tomography: CT donut spins and patient continually moves through the scanner. Throughput time and image quality improved. Produces a higher density of data. MRI: Technical aspects: - MRI technologies developed from nuclear resonance used to evaluate chemical composition of laboratory samples. - Raymond Damadin first produced a full body MRI in 1976. Equipment: - gantry contains one of three types of magnets. 1. super conducting magnet – primary magnetic coils super cooled 2. permanent magnets – open magnetic resonance utilizes this type of magnetic reducing claustrophobic affects. Cannot achieve the high field strength of super conducting magnet. High noise to signal ratio. Improved software improved these images. 3. Resistive electromagnets – classic electromagnet, low initial cost, lower in weight, very high power consumption – may consume savings in the long run. Functional MRI requires a BIG magnet, super-cooled. Claustrophobia is the number one reason for failure. There are reports that the contrast material irritates this situation. Magnetic resonance gradient magnetic coils: located within the gantry allow “slicing” of the patient’s anatomy along sagittal, coronal, or axial planes rapid on/off switching produces the loud clicks and taps heard by the patient. Radiofrequency (RF) coils: placed on or near the area of interest used to excite target tissue also receives information regarding hydrogen nuclei relaxation X-ray Diagnosis Tri 6 5 Image production hydrogen is a charged particle representing 80% of all the atoms in the body hydrogen behaves like a small bar magnet they are randomly oriented and their charges cancel out the MR scanner can spatially locate hydrogen within the body in the strong magnetic field of the MR unit, the hydrogen molecules tend to align with (or less often against) the field. The hydrogen molecules are not held static, but are induced to demonstrate precession (wobble) They are aligned, but they precess or spin out of phase A strict linear relationship exists between the frequency of precession and the MR magnetic field. Energy must be added to the system. RF identical to the Larmor frequency is pulsed into the patient. This is the concept of resonance. This causes the aligned hydrogen atoms to precess in phase. The RF pulse is turned off in the “excited” hydrogen atoms undergo “relaxation”. Spin Echo Sequence The appearance of the image reflects the intensity of the emitted signal. High signal intensity appears bright and dark areas represent areas of low signal intensity. Intensity of the signal is determined by the quantity of mobile hydrogens and two magnetic relaxation times. T1 AND T2. Manipulating the repetition of administered RF pulses (repetition time, TR) and collection of the emitted RF signal (echo time, TE) influences the image characteristics. Images may be described as proton density in which the image is based on the population of hydrogen T1-weighted or T2-weighted MR PULSING SEQUENCES WEIGHTING TR PROTON LONG T1 SHORT T LONG TE SHORT SHORT LONG T1 protocols utilized TR’s of 200-500 milliseconds approximately TE’s lasting approximately 15 milliseconds T2 images are very tiny consuming protocols and have long TR’s and long TE’s Hybrid images have been developed to take advantage of T2 type images with greater economy of time Imaging protocol in MRI the parameters selected usually represent a compromise between radiologist preference, diagnostic capability and examination time. Differential considerations greatly affects image sequence selection Extradural disease represents the most common diagnostic request. T1-spin echo essential to exam the spine; exams anatomy, marrow space, sagittal gradient echo. Intramedullary disease MRI – CONTRAST non-iodinated: adverse reactions very rare magnetic contrast agents gadolinium is the most common agent - works as a T1 shortening agent which causes tissue containing gadolinium to appear bright on T1 - very useful in cases of: CNS tumor MS disc herniation versus scar tissue X-ray Diagnosis Tri 6 6 MRI STRENGTHS superior resolution superior tissue contrast images soft tissue very well non-contrast enhancement in the spinal canal axial images OK coronal, sagittal, etc. images are superior MRA can produce non-contrast visualization of major and minor vessels Measurements may be accomplished MR reports on the physiology as well as anatomy Not reliant on attenuation of ionizing radiation No known harmful effects MRI WEAKNESSES time and money cannot manipulate the image if the MR scanner is no sequenced correctly, information may be lost or hidden high resolution MR bone detail is adequate and on standard MR images, bone detail is poor MRI CONTRAINDICATIONS pace makers, ear implants, miscellaneous implanted electronic devices, cerebrovascular clips, machine shop workers, claustrophobia, orthopedic implants (distorts gaussian field) FMR – functional MR; most recent work to map brain activity or functionality. BONE SCAN 1. Injection of a radioactive isotope (technetium) 2. Uses a gamma camera or scintilla scope to view osteoblastic activity as demonstrated by technetium uptake. SPECT/PET SCAN (Single Photon Emission CT/Positron Emitted Tomography) SPECT is to bone scan as CT is to plain film. PET utilizes uptake of glucose to generate pictures. COLOR-DUPLEX SONOGRAPHY OF THE ARTERIES Can measure the amount of occlusion. Basic anatomy and physiology review. Apophysis – a bump on a bone that has/had a growth plate but no articular cartilage (greater/lesser trochanter). Calcium and phosphorous. Calcium is in use for clotting, contraction, conduction; parathormone regulates blood calcium level and is in a 2:1 ratio with phosphorous (Ca:P). Acid phosphatase (break-down) and alkaline phosphatase (build-up). Calcium: phosphorous allows Ca to complex into the bone matrix. Parathormone releases with low serum Ca; this allows improved complexing of Ca in serum through the vitamin D loop. There are normal levels of parathormone required. Calcitonin: (unknown where, specifically, it produces) inhibits serum level increases of Ca. Estrogen and androgens control growth as does products of anterior pituitary (growth hormone). Short lecture on acromegaly, dwarfism, etc. Glucocorticoids released in response to certain stresses and can lead to bone loss. X-ray Diagnosis Tri 6 7 MENSURATION Sella turcica size Basilar angle (Martin’s, Welcker’s, spenobasilar ) Chamberlain’s line – know this enough to not use this McGregor’s line Horizontal : widest diameter Vertical: fossa floor to clinoids Nasion – center sella turcica Basion – center sella turcica Average 11mm 8mm 137 Min 5mm 4mm 123 Max 16mm 12mm 152 Pituitary and extrapituitary masses enlarge the fossa Basilar impression and platybasia widen the angle. Yokum uses 1 (congenital; fusion) and 2 (acquired; Paget’s, osteomalacia, fibrous dysplasia) Basilar impression when odontoid more than maximum distance above. (Paget’s, osteomalacia, etc.) Hard palate – opisthion (difficult to see without high kVp/mAs technique) Below line to 3mm above 7mm Hard palate – occiput. Note relative odontoid apex. Below line Basilar impression when odontoid more than maximum distance above. (Paget’s, osteomalacia, etc.) Right and left digastric grooves: (a) line-odontoid distance (b) line-C1/OCC joint distance 11mm Males 8mm Females 10mm 21mm ADI C1 anterior tubercle – odontoid Adult Child 3mm 5mm George’s line Alignment of posterior body margins Aligned Posterior cervical line – more often spinolaminar line Sagittal canal dimension – know that it doesn’t work Atlantoaxial alignment (rotation) Spinolaminar junction lines Aligned Transverse ligament rupture or instability. Trauma, Down’s, occipitalization of atlas, etc. and inflammatory arthritis may increase ADI. ADI should not gap at all in flexion/extension. A to P vertebral malpositions when line not smooth; traumatic, >2mm suspect instability (ligament laxity). A to P vertebral malpositions when line is not smooth, especially at C1 and C2; used in conjunction with George’s line for spinal canal stenosis (when less than 12mm). Spinal stenosis when less than 12mm. Intraspinal tumor when enlarged C1 lateral mass – C2 articular pillar margin alignment Aligned Jefferson’s or odontoid fractures or alar ligament instability when margins overlap. If C1 articular mass slides more than 2mm over C2, suspect fracture [with 5 suspect dens fracture, 7 confirmed dens fracture]. Cervical gravity line Vertical line from odontoid apex Lordosis or angle of C-spine Line from inferior endplates of C7; line through anterior and posterior tubercles of C1; take perpendicular lines from each above to obtain angle Posterior margin of pharynx and anterior margin of spine Passes through C7 body 40 AP displacement is a gross indicator of gravitational stress at the cervicothoracic junction. Role unclear. Decreased following trauma, muscle spasm, spondylosis, and patient tucking the chin at time of exposure Digastric line Retropharyngeal space 1mm (odontoid not above the line) Posterior body – spinolaminar junction lines 1mm 1mm 12mm 35 45 Basilar impression when odontoid is above the line. 7mm - 20mm considered normal C5, Pharynx above is 7 Trachea below is 20 Enlargement often from pus, blood, cells X-ray Diagnosis Tri 6 Cobb’s angle Risser-Ferguson Thoracic kyphosis (straight back syndrome) Thoracic cage dimension Sacral base angle Lumbosacral disc angle Hadley’s S curve Ferguson’s gravity line, Ferguson’s weight line, lumbar gravity line McNab’s line Ullmann’s line Interpediculate distance Eisenstein’s method (line) Unreliable. Intertrochanteric line Klein’s line Teardrop distance most inferior endplate of lowest vertebra for first horizontal line, and superior endplate of highest vertebra for second horizontal line; perpendicular lines form each form an angle Centers of end and apical segments joined and the angle measured T1 superior endplate – T12 inferior endplate, then intersecting perpendiculars and the angle measured Posterior sternum – anterior T8 body 8 Scoliosis named for the side (levo or dextro) and degree at any level. 10 or more is a scoliotic curve, less is a convexity. Scoliosis evaluation – this method demands that a vertebra is a apex or base. Kyphosis evaluation – often presents with abnormal cardiac sounds. Male 14cm Female 12cm 11cm 9cm 18cm 15cm Endplate of S1 to horizontal line angle Angle between opposing endplates of L5 and S1 Line along the inferior surface of TP along lamina along articular process across joint A perpendicular line is drawn from the center point of L3 body 41 26 57 -- 10 15 A line along the inferior endplate Should be above superior articular process L5 behind the line Endplate line through S1, perpendicular from sacral promontory Shortest distance between inner surfaces of opposing pedicles Tips of superior and inferior articular processes joined. Distance between posterior midbody and this line (except at L5) Inclined line through neck of femur – tangential line to outer femoral neck, head just overlaps laterally Femoral head – teardrop distance Smooth across joint AP and Oblique views may be used. Altered in various mechanical pathologies within 1 cm of sacral promontory Variable 12 is normal Straight back syndrome when the distance is less than 13 cm in males and 11 cm in females. Normal > 13cm form male and >11cm for female. Follow-up measure for less than normal requires cardiac exam. Normal is 41 +/- 7; altered in various mechanical pathologies. Altered in various mechanical pathologies Injury / facet subluxation Famous but not very useful; extension malposition, normal variant. Originally used on recumbent positioning, weight bearing has an effect. Detection of subtle spondylolisthesis when L5 body crosses perpendicular line. Decreased lordosis may give false (+). Widened in intraspinal tumors, fracture / trauma; narrowed in spinal stenosis. Always wide on kids. Spinal stenosis suspected when less than 15mm Not reliable, indicates need for CT or MRI. CT or MRI for (+). 15mm Slipped femoral capital epiphysis when head does not intersect line; often presents with knee pain (not hip). 9mm 6mm 11mm Early Perthes or other inflammatory joint disease may widen the space more than 11mm or create a 2mm difference from the normal side X-ray Diagnosis Tri 6 Hip joint space width Protrusio acetabuli Presacral space Shenton’s line Boehler’s angle Femoral neck angle Gleno-humeral joint space Fermoral head – acetabulum distance. a. superior b. axial c. medial (Kohler’s to head) Pelvic inlet-outer obturator. Acetabulum should be lateral to the line Soft tissue density between the rectum and anterior sacral surface. Smooth curvilinear line along medial femoral neck and superior obturator border Three superior points joined on the calcaneus. Posterior angle is measured. Lines through the axis of the femoral shaft and neck Average humeral head-glenoid distance (superior, middle, inferior). Acromialclavicular Lateral tip clavical to medial aspect acromion Acromiohumeral joint space Solid white line of the articular acromion to the head of humerus Gailula lines (three arcs of the wrists) Draw proximal line of proximal portion of proximal row; then the distal portion of the proximal row; and the proximal portion of the distal row. Endplate lines at opposing segments. Measure from the posterior body to point of intersection. Van Akkerveeken’s measurement 9 4mm 4mm 8mm 3mm 3mm 4mm 6mm 7mm 13mm Child: 3mm Adult: 7mm 1mm 2mm 5mm 20mm 30-35 28 40 120 130 2.5mm 2.1mm 4.1mm 3.7mm 7mm 11mm 4-5mm Male: 3.3mm Female: 2.9mm 9mm Equal measures 1.5mm differ Various joint diseases decrease these distances: Degenerative joint disease Rheumatoid arthritis Degenerative (OA) and rheumatoid arthritis Protrusio acetabule (Paget’s disease, etc.) when acetabulum is medial to the line. Soft tissue mass (tumor, infection, hematoma), if exceeds maximum distance. Femur dislocation or fracture if line is interrupted, femoral neck fracture, slipped femoral capital epiphysis. Calcaneal fractures may reduce the angle to less than 28. Coxa Vera: less than 120 Coxa valga: more than 130 Adding, dividing by three and comparing, degenerative and crystal arthritis diminish the space. Posterior dislocation may widen it. Distance divided by 2; traumatic shoulder separation; degenerative arthritis decreases distance. Separation and resorption widens distance. 11mm or less rotator tear. Arthritic changes, dislocation/subluxation; rotator cuff tear decreases distance. Subluxation and dislocation increases distance. Nuclear, annular and posterior ligament damage if more than 1.5mm difference. In slide testing for Dr. Kettner, if it’s in a box, it’s an infection. Spondylolisthesis: Meyerding’s grading divides the sacral base into quarters with the relative position of the posterior body of L5 determining grades I - IV (25%, 50%, 75%, or 100%). A more accurate method is measuring the distance of slip [of the slipped vertebra] and dividing by the length of the endplate of the stable (unslipped) vertebra. Canal body ratio or Stenosis of vertebral canal: Take the ratio of the vertebral body to the canal; divide the canal by the body. Less than 82% is stenosis. More accurate than sagittal canal dimension method above but plain film is not good enough no matter what. CT or MRI is the best form of examination. In blocked vertebrae: if congenitally fused, there is a C type cavity where the disc was, as opposed to a fused block vertebra. Vastine-kinney angle (sella turcica) X-ray Diagnosis Tri 6 10 VanAkkerveeken and flexion and extension have been largely replaced by the more sensitive compression/distraction study. Lateral projection; draw two lines through and parallel to opposing segmental endplates until they intersect posteriorly. The distance from the posterior body margins to the point of intersection is then measured. Alternatively, the displacement can be assessed by measuring the offset in the oppoosing body corners Should be Lateral bending study may suggest ligament laxity and/or muscle spasm poor correlation between this and clinical picture PRINCIPLES OF X-RAY INTERPRETATION. Seven categories of bone disease: Congenital, trauma, arthritis, tumor, infection, hematologic, nutritional/metabolic/endocrine (VICTANE?). Analysis of the lesion - Skeletal location - Position within bone - Site of origin - Shape - Size - Margination - Cortical integrity Behavior of the lesion Matrix Periosteal response Soft tissue changes Joint changes Preliminary analysis - Clinical data: age, sex, race, history - Number of lesions - Symmetry of lesions - Systems involved Supplementary analysis - Other radiologic procedures - Lab exam - Biopsy Age (decades) Size: 0-6 cm 6+ cm Monostotic polyostotic Cortical destruction Periosteal resction Solid Laminated Spiculated Codman’s Destruction Geographic Motheaten Perireactive Margins: Sharp Inperceptiple Matrix Soft tissue mass Joint space Begign 123 Primary 1234567 Secondary 4567 +++ + +++ + - + +++ +++ + +++ + +++ ++ +++ +++ +++ ++ ++ + ++ +++ ++ + + +++ - + +++ +++ +++ +++ +++ +++ - + +++ ++ +++ - + +++ + - X-ray Diagnosis Tri 6 11 OSTEOLYTIC BEHAVIOR Geographic lesion Solitary Greater than 1 cm Sharp margin Motheaten lesion Multiple 2-5mm ragged margins and coalescence imperceptible transition permeative lesion multiple less than 1mm imperceptible transition OSTEOPLASTIC BEHAVIOR Diffuse lesion Homogenously sclerotic (“ivory”) Obliterated corticomedullary junction Localized lesion Single or multiple Irregular, hazy border Asymmetrical MIXED BEHAVIOR Both osteolytic and osteoblastic features Table 7.1 - Normal Laboratory Values: Acid phosphatase, alkaline phosphatase, calcium, CBC (hematocrit, hemoglobin, RBC, WBC), C-reactive protein (CRP), ESR, phosphorus, protein (total or fractions [albumin, globulin]), special antigens (HLA B27, RA factor), uric acid. DYSPLASIA Achondroplasia – most common form of dwarfism. “champagne glass” pelvis or “wine glass” pelvis; normal is brandy snifter. A more rectangular shaped pelvis, the scapula also appears blunted; can demonstrate coxa vara or valga; interpedunculate space narrowed and central canal stenosis with a scalloped appearance on lateral Xray via dural actasia (due to a lack of room for the cord allowing for the pulsation of the CSF to impress on the vertebra) gives a bullet shaped vertebra. most common complication is central canal stenosis and DJD in the adult (multiple laminectomy often necessary); frequent cause of neonatal death stenosis of foramen magnum. This is a bilateral process with grossly short bones; proximal more than distal affected and longer bones more than shorter bones yields the rhizomelia classification. Higher, flatter forehead; depressed nasal ridge; protruding buttocks and abdomen; incomplete extension of arm (shallow olecranon fossa); champagne glass pelvis, short extremities (rhizomelia), diminished interpeduncular spaces AP view; affects endochondral bone development (achondroplasia) but normal intramembranous development; spine typically acquires normal length; and trident hand is a classic X-ray finding (when patient completely opens hand, the thumb is off by itself, first two fingers and second two fingers group). Overall etiology unknown; 80% considered spontaneous. There are lethal forms, serious complications in adult; normal intelligence. Cleidocranio dysostosis (dysplasia) – common appearance of MID-LINE defects. Appearance of lots of wormian bones in occipital region with a lack of lambdoidal suture. They do not qualify as a dwarf though short and with a little larger head and smaller face than usual (altered craniofacial) and depressed shoulder. Cleft palette, cleft lip, missing pubic symphasis, prevalent wormian bone, small face in relation to skull, drooping shoulders and slender neck, high mobility of shoulders allowing for a large amount of self love arm wrapping. This is not rare, though not common. Smaller ribs at the top giving a funnel shaped chest cavity. 10% have congenital absence of the clavicle. X-ray Diagnosis Tri 6 12 Marfan’s syndrome – arachnodactyly; long, slender foot and hand bones. Occular abnormality (lens dislocation) and very tall (over 6 foot). There is a tendency for dissecting aortic aneurysms. Look for the thumb sign: fold your thumb into your hand and close your fingers around it and push the thumb under; typically you can see the entire distal phalanx sticking out the other side. Ligamentous laxity. Equal prevalence is equal between men and women. Body habitus is on the thin side with low body fat and joint laxity. About 45% have scoliosis. Poor dentition with lots of dental caries. Consider, upon seeing a scoliotic child, how tall are they, are they wearing glasses, how are your teeth, can you bend your thumb, do you have a murmur. Often these people have valvular and chamber deformities in the heart. Enchondral bone growth exagerated, though intramembranous is pretty normal. Pectus excavatum results in heart disposition. Common and clinically recognizable. First site of aortic aneurysm is the arch (first highest pressure zone in the aorta) second is in the bifurcation of the common iliacs (the second highest pressure zone in the aorta). Osteogenesis imperfecta (OI) – hands demonstrate arachnodactyly, short stature due to multiple fractures causing premature closure of growth plate. Bone has a thin cortex and lack of density in trabecula. Fractures can lead to subperiosteal bleeding leading to a large, exuberant callous formation. Bilaterally curved femurs, the degree of bowing can indicate the severity of affliction. Trivial trauma can produce fracture. Osteoporosis with great fragility, 90% have a blue sclera due, and abnormal dentition. There are two forms: Congenitive: worse, recognized at birth, higher mortality rate, if they live past infancy they are profoundly affected as adults. Tartiform: comes out incidentally later. A form of brittle bone disease along with osteopetrosis. SCLEROTIC DYSPLASIAS Maloryostosis – part of the bigger group of sclerosing ostoses. Adds cortical bone endogenously and exogenously. This has more cortical bone than is normal and increased density inside the bone without changing the contour of the bone. Most findings are incidental (found during investigation of a different complaint). Symptomology produces through compression of soft tissue, nervous tissue, tendinous tissue, etc. offering a molten waxed appearance. Most common in the extremities. Osteopetrosis – “bone-within-a-bone” polyostotic, increased densities a.k.a. chalk bone; very unusual. Bone has no exaggerated osteoblastic activity. Trivial trauma can produce fracture. A form of brittle bone disease along with OI. Osteopoikelosis – polka-dot appearance of bone on plain film, normal bone scan, no pain syndromes, does not appear to change the bone strength. KNOW A BUNCH OF THE FOLLOWING STUFF: Asphyxiating dysplasia Aperts with brachycephaly (short skull) not bradycephaly, Schaphocephalic (boat head) normal coronal suture growth and early closure of sagittal suture. Turycehpaly Underdeveloped distal palanges, bulbos nose and thick, coarse hair = trichorhinopalangeal Shortened metacarpals. Stippled epiphysis – multiple growth centers Spondyloepiphyseal dysplasia – heaped up appearance of the body of the vertebra. Angleman’s disease (progressive diaphysiseal dysplasia)– demonstrates less density than maloryostosis (no candlewax appearance) and is internal only. Picnodysostosis – very small, pinched faces (elfin), more head than face and increased density within the bone. Osteolysis (resorption of bone). Acroosteolysis – know the film. With skin induration and retraction of soft tissue and difficulty in swallowing is not picnodysostosis but is scleroderma. Most typically, an acquired blocked vertebra will produce greater degrees of DJD. X-ray Diagnosis Tri 6 13 Developmental cleft – a normal “step” in a vertebral body Limbus vertebra – when the nucleus pulposis goes through the ring apophysis (growth ring) of the vertebra instead of into the endplate or through the longitudinal ligament. It is not mobile because the sides are still in fusion with the remainder of the ring and body. Block vertebra is an indication for flexion/extension series to examine ADI instability. The classic block will demonstrate a “wasp” waist at the rudimentary disc area. CONGENITAL Hyperostosis internus (the whole inner table is bigger/thicker); frontalis is limited to the frontal bone. Parietal foramen – congenital failure of the fontanels to ossify. Hypoplasia of the frontal sinus; clinical significance – none. There are two spikes to sinus formation: just before puberty and just before skeletal maturity. Concern for a benign frontal osteoma. Occipitalization (craniovertebro synostosis)– occiput and C1 fusion; see what appears as a foramen like radiolucency in that area. Express concern for transverse ligament damage; pay attention to the ADI (accumulated microtrauma will increase the ADI resulting in weakening transverse ligament possibly resulting in guillotine). This condition calls for flexion/extension cervical series. Spodylo-schisis – modified submental - failure (agenesis) of both anterior and posterior tubercle C1. Paradental sulcus Frontal suture closure result in taller head; mid sagittal closure results in craniocephaly. Ponticulus posticus (arcuate foramen) – a physiologic pattern of soft tissue calcification: Serum Ca++ Tissue Physiologic normal normal Metastatic metastatic normal Dystrophic normal abnormal About 10% of patients will have recognizable complaints associated with this. This is particularly important with concern to VBAI. 1. 2. 3. Os odontoidium – failure in ossification of dens to body C2. Cervical digit – an articulation on/of a rib. Cervical ribs Sacral agenesis Posterior scalloping – from achondroplasia with dural ectasia; or from NF Geriatric: Things you expect to see: OP, compression, DJD, change in contour Surprises that are common to see: congenital anomalies, benign tumors (fibrous), Paget’s disease License stealers: Metastasis, AAA, infection (lung or bone) Old men: less OP Young adult: Things you expect to see: trauma, posture abnormalities. Surprises that are common to see: Fibrous lesions, congenital anomalies License stealers: infection X-ray Diagnosis Tri 6 14 Pediatrics: Things you expect to see: no abnormalities. Surprises that are common to see: Fibrous lesions, congenital anomalies License stealers: Metastasis, infection Ununited apophysis. Cervical digit. Sprengel’s – unilateral elevation of scapula; actually, failure of scapula to descend. Omovertebral bone – often seen with sprengel’s. Often associates Klippel-Feil syndrome, blocked vertebra, webbed neck Rhomboid fossa – a muscular impression on X-ray. No clinical consequence. Hemivertebra – only neatly triangular when drawn. Scrambled spine, also a structural scoliosis. Butterfly vertebra – missing primary ossification centers in the body, apparently migrating to the levels above and below. Intrathoracic rib – unlikely to produce any complications. Synostosis of rib (bifid rib, or costal synostosis). Failure to separate. Elongation of L5 TP, considered a physiologic variant most likely calcification of iliolumbar ligament. Spina bifida in the lumbar vertebra seems to associate with increased disc pathology. Reversed thoracic kyphosis or thoracic lordosis: recommendable to perform thoracic cage mensuration. If linked with a heart murmur, then straight back syndrome. If there is a heart murmur it is likely a result of floppy valve syndrome. High percentage have pathology requiring valve replacement. Costochondral ossification – physiologic calcification – everything (serum and tissue calcium) is normal. Thoracolumbar transitional ribs. Notochordal persistency resulting in cupid’s bow. Winking owl sign – metastasis (most common) or congenital. Sclerosis of the contralateral indicates congenital because it takes a long time to sclerose. There is an apparent correlation between spina bifida and DJD. Springboard divers, interior lineman, gymnasts are at high risk for acquired splondylolysis. If flexion/extension demonstrate 3% or more translation you confirm unstable listhesis; less than 3% does not rule in or out anything. Oppenheimer’s ossicles – nonunion of growth centers. Lordodic sacrum Injection granulomas [from arthritic injections in the gluteus] called dystrophic calcification (regularly seen in patients). Pseudotumor of the pelvis – results from observation of the growth plate between the ischial and pubic rami. Fabella – sesamoid-like bone in lateral gastroc often confused with synovial chondroplasia. Rockerbottom foot – missing tarsal bones Bipartate sesamoid bones. Tarsal coalition – bony bars in the tarsals. Pseudotumor of the humerous – lucency that results from the attachment of rotators – it disappears on baby-arm Xray Supracondylar process – found on the humerous and points toward the elbow joint (normal variant). Often confused with osteochondroma – points away from the joint, found anywhere on the body, and has a condral cap. Maudline’s deformity – ulnar deviation of wrist Ulna minus – short ulna. Ununited growth center of ulnar styloid process. Radius minus. Synostosis – failure of the bones to separate.