PRE-CLINICAL EVALUATION OF NA APICO AORTIC
advertisement

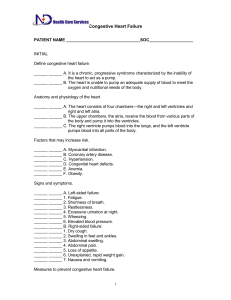
PRE-CLINICAL EVALUATION OF NA APICO AORTIC IMPLANTABLE CENTRIFUGAL PUMP AS A LEFT VENTRICLE ASSIST DEVICE Bruno Silva1, 2, Adib Jatene1, Juliana Leme1, Jeison Fonseca1, Beatriz Uebelhart1, 2, Cibele Silva1, 2, Aron Andrade1, Carlos Suzuki2 1 Centro de Engenharia em Assistência Circulatória, Instituto Dante Pazzanese de Cardiologia/Fundação Adib Jatene, São Paulo (SP), Brasil 2 Departamento de Materiais e Processos de Fabricação, Universidade Estadual de Campinas, Campinas (SP), Brasil E-mail: brunoutiyama@gmail.com Abstract. This work shows a pre-clinical evaluation of the Apico Aortic Blood Pump (AABP), which included an anatomical positioning test, an efficiency study and a experiment to determine blood trauma caused by AABP. Anatomical Positioning test consists implant the device in an animal model (pig, landrace, female, 70kg) to evaluate AABP dimensioning and possible damage to nearby tissues and organs. In the efficiency study we obtained AABP’s hydrodynamic performance curves (pressure x flow) and compared the results with meal performance values for cardiac assist for rotary blood pumps. Blood trauma analysis was conducted by means of a normalized experiment and the indicator for the Normalized Index of Hemolisys (NIH) was the Plasm Free Hemoglobin (PFH), mean NIH was compared with literature values. Anatomic positioning test showed no possible damage do nearby tissues and organs specially the lungs and the implant method was also considered feasible by the clinical staff. AABP s hydrodynamic performance curves appointed a performance which allows AABP application as a left ventricle assist device (LVAD) for cardiac support. NIH obtained in the hemolisys test was an interval considered to cause a minimal blood trauma. Results indicated AABP efficiency as a LVAD and demonstrate that the device can be used for cardiac support. Keywords: Left Ventricle Assist Device, Pre-clinical Evaluation, Blood Pump, Mechanical Cardiac Assistance 1. BACKGROUND Ventricular Assist Devices (VAD) has been proving to be an efficient option for severe heart failure treatment (BOCK, 2011). A significant decrease in death rate in patients in waiting list for a heart transplant was noticed, since the beginning of VAD therapy (JOHNSON, 2010). Apico Aortic Blood Pump (AABP) (Fig. 1) is a centrifugal, continuous flow, to be used as a Left Ventricle Assist Device (LVAD). Figure 1 – Apico Aortic Blood Pump drawings. A – A view showing inlet and outlet cannulas. B – A section view showing some device’s parts. In AABP’s implant method, pump’s inlet cannula is introduced and remains fixed on the left ventricle while implanted and outlet cannula is connected to a vascular graft attached to aorta artery by an anastomosis. AABP’s development was conducted in a multicenter project, which involved multidisciplinary research groups from Institute “Dante Pazzanese” of Cardiology, University of Campinas, University of São Paulo and Brazilian Navy. Development includes a device study as a blood pump, which is called preclinical evaluation. Results from each experiment in the pre-clinical evaluation were used as project guideline. This work reports the results from pre-clinical evaluation of AABP. 2. MATERIALS AND METHODS AAPB’s pre-clinical evaluation was composed by several practical experiments with prototypes. Initially, an anatomical positioning test was made. With this method, is possible to analyze the implant method and the AAPB’s dimensioning (BOCK, 2011, 2012). AABP was implanted in an animal model (pig, 70kg) following the device implant method. Surgical procedure, post implanted device and nearby tissues and organs were analyzed. Hydrodynamic performance curves from prototypes were obtained to obtain data from AABP’s efficiency as a blood pump. A mock circulation loop system constructed with an environment similar to human cardiovascular system was used. In this system, parameters as left ventricle preload and afterload, blood viscosity, cardiac output and arterial compliance were controlled. The objective of this test is to observe AABP performance as a LVAD and compare the hydrodynamic performance curves from prototypes with one different geometrical characteristic among each other. Blood trauma effect caused by AABP, was quantified experimentally in a hemolisys test, according to ASTM F1841 and ASTM F1830 standards. In the test total head pressure was maintained in 100mmHg, with a flow of 5l/min Blood damage indicator was the Plasm Free Hemoglobin (PHF), given by Eq. 1, which uses readings from the samples in three spectrophotometer filters to determine PHF (LEME, 2011). PFH = [2(A205) – (A340) + (A505)] x 83, 6 (1) Where: PFH = Plasm Free Hemoglobin (mg/dl); A 205 = Reading from the A205 filter; A 340 = Reading from the A340 filter; A 505 = Reading from the A505 filter; 83, 6 = Reference value. PFH is used in Eq. 2 to determine the Normalized Index of Hemolisys (NIH). (2) Where: NIH = Normalized Index of Hemolisys (g/100l); ΔPFH = Plasm Free Hemoglobin variation (mg/dl); V = Total Volume (l); Ht = Hematocrit (%); Q = Flow (l/min.); Δt = Time between samples (min.). 3. RESULTS AND DISCUSSION 3.1 Anatomic positioning test First step in AABP implant is to suture a guide ring to the left ventricle apex (Fig. 2). This ring will be used to fix AABP’s inlet cannula. Figure 2 – AABP’s guide ring, previously sutured to the left ventricle apex. After the guide ring suturing, AABP inlet cannula is introduced and fixed by an incision in the left ventricle apex. Fig. 3A shows AABP been fixed and Fig. 3B shows AABP completely implanted. Figure 3 – A. Inlet cannula been fixed in the guide ring. B. Picture from AABP already implanted in the left ventricle apex. The clinical staff involved with this test appointed no signs of lung damage by compression. AABP’s anatomical positioning allows its implant in patients with different body size and pump’s dimensioning were considered feasible for the purposed implant method. 3.2 Hydrodynamic performance tests AABP performance curves are showed in Fig. 4. As described by Nosé, a rotary blood pump should be able to maintain a head pressure of 100 mmHg with a flow of 5 l/min, which is the mean performance required for VAD therapy (NOSÉ, 1998; SILVA, 2012). Figure 4 – AABP’s hydrodynamic performance curves. AABP’s hydrodynamic performance curves appointed that the mean rotation speed for cardiac assist, based on the values from literature would be about 2300 rpm. 3.3 Hemolisys Test Plasm Free Hemoglobin (PFH) values obtained from Eq. 1, in AABP’s hemolisys test are shown in Fig. 5. Figure 5 – Plasm Free Hemoglobin from AABP’s hemolisys test. PFH curve in Fig. 5 indicates constant hemoglobin liberation by the erythrocytes, in each collected sample. A summary of the results from the hemolisys test, including the mean NIH are shown in Table 1. Table 1 – Summary of the results from hemolisys test. A study from Nosé appointed that the ideal mean NIH for a LVAD is 0,01 g/100l (NOSÉ, 1998). 4. CONCLUSIONS Experiments from AABP’s pre clinical evaluation showed so far that AABP is feasible for use as a LVAD. Device dimensioning was considered to allow implant method and anatomic positioning without causing damage to nearby tissues and organs. AABP’s hydrodynamic curves demonstrate the device performance in cardiac assistance. Also, by comparing AABP’s NIH with values from the literature, we concluded that blood trauma cased by AABP, are inside values for long term implant. ACKOWNLEDGMENTS The authors would like to thanks FAPESP, Adib Jatene Foundation, Syrian Sanatorium Association HCor, Brazilian Ministry of Health and CNPq for financial support. REFERENCES ASTM F 1830. (1997) “American Society for Testing Materials; Standard Practice for Selection of Blood for In Vitro Evaluation of Blood Pumps”. ASTM F 1841. (1997) “American Society for Testing Materials; Standard Practice for Assessment of Hemolysis in Continuous Flow Blood Pumps”. Bock, E; Antunes, P; Leão, T; Uebelhart, B; Fonseca, J; Leme, J; Utiyama, B; Silva, C; Cavalheiro, A; Filho, D. S; Dinkhuysen, J; Biscegli, J; Andrade, A; Arruda, C (2011). “Implantable Centrifugal Blood Pump with Dual Impeller and Double Pivot Bearing System: Eletromechanical Actuator, Prototyping and Anatomical Studies”. Artifical Organs. 35(5):437-442. Bock, Eduardo; Galantini, Danilo; Contreras, Carlos; Leão, Tarcísio; Uebelhart, Beatriz; Cavalheiro, Andre; Filho, Diolino; Fonseca, Jeison; Leme, Juliana; Silva, Cibele; Utiyama, Bruno; Dinkhuysen, Jarbas; Andrade, Aron. (2012) “A new surgical technique for aorta cannulation of implantable centrifugal blood pump” ASAIO Journal 58(17). Johnson, M. R; Meyer, K. H; Haft, J; Kinder, D; Webber, S. A; Dyke, D. B. (2010) “Heart Transplantation in United States, 1999-2008”. American Journal of Transplantation. V.10(2), pp. 1035-1046. Leme, Juliana; Fonseca, Jeison; Bock, Eduardo; Silva, Cibele; Utiyama, Bruno; Santos, Alex E; Dinkhuysen, Jarbas; Andrade, Aron; Biscegli, José F. (2011) “A new model of centrifugal blood pump for cardiopulmonary bypass: performance and hemolysis tests”. Artificial Organs 35(5): 443-447. Nosé, Y. (1998) “Design and development strategy for the rotary blood pump”. Artificial Organs. 22(6):438-446. Silva, Bruno U; Jatene, Adib D; Andrade, Aron J. P; Fonseca, Jeison W. G; Leme, Juliana.; Uebelhart, Beatriz; Silva, Cibele; Bock. Eduardo; Antunes, Pedro; Biscegli, José F; Silva, Jorge A; Junqueira, Fernando C; Horikawa, Oswaldo;Ono, Eduardo; Suzuki, Carlos K. (2012) “A new Brazilian Left Ventricle Assist Device (LVAD): Concept, Anatomical and In Vitro Studies” ASAIO Journal 58(17).