Summit 2014, Care of the patient with an LVAD
advertisement

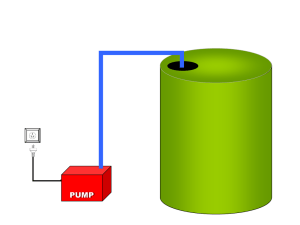
Post Operative Care of the Left Ventricular Assist Device Patient in the Acute Care Setting Presented by Jude Melendez, MS, RN, CCRN- CSC and Loretta Nerney, BS, RN, CCRN Key Concepts The newly implanted LVAD patient is a post op cardiac surgery patient first, LVAD patient second. Nurses need a good understanding of LVAD pump physiology for hemodynamic monitoring. Goal of LVAD therapy: Increase CO Improve end-organ function Improve Quality of Life Improve morbidity and mortality Reprinted with the permission of Thoratec Corporation Pump Physiology Continuous-flow LVADs deliver flow throughout the entire cardiac cycle Flow is determined by Pump speed: Flow increases with speed increases Preload dependent Afterload sensitive The aortic valve may not always open and patients may not have a palpable pulse Pulsatility Index (PI) As the left ventricle contracts and relaxes, the flow through the pump increases and decreases, adding a degree of pulsatility PI is the magnitude of this flow pulse The pulsatility index (PI) will normally decrease as pump speed is increased PI will change with patient conditions that normally affect stroke volume (physiologic demand, volume status, RV function) Suction Events If pump speed is set too high or conditions exist to affect preload, the pump may decompress the LV to the point of collapsing the walls together. Evaluate the cause – they are the same complications that can arise for any cardiac surgery patient Hypovolemia/vasodilation (affecting preload) Post-operative bleeding Tamponade Arrhythmia RV failure Reprinted with the permission of Thoratec Corporation Nursing Assessments Systems Survey Device Parameters and Hemodynamics Monitoring for complications Patient and Caregiver needs Hemodynamic Assessments Arterial line Swan-Ganz catheter Physical S/S of good perfusion TEE when in doubt Device Parameters Monitor for variations from patient baseline Arterial waveform for LVAD patients http://pics3.this-pic.com/key/dampened%20arterial%20line%20waveform Systems Survey: Cardiac Therapy Goals & Interventions MAP 70-85 mmHg Normothermia Pressors (dopamine, vasopressin, levophed) Fluid resuscitation Cardiac Index > 2.2, LVAD flow > 3.5 liters/minute Adequate preload Balance RV failure vs. adequate LVAD filling Increase RV contractility (epi, primacor) Decrease RV afterload: iNO Treat arrhythmias promptly – protect heart function Monitor labs: abg, mvg, lactic acid Systems Survey Neuro status Pain management and sedation Evaluate for CVA Pulmonary status If on iNO, ventilator dependent until weaned off SaO2 may not be obtainable; correlate to abg Underlying pulmonary dysfunction Hematologic status Assess for bleeding: chest tubes, incisions, drive line site Monitor H/H, TEG, Coags Hemolysis? Monitor LDH Systems Survey Renal function: assess for adequate perfusion & functioning Monitor/replace electrolytes Monitor urine output Monitor BUN/creatinine Hepatic function: assess for dysfunction from pre-op history of heart failure Assess for coagulopathies Blood glucose control Systems Survey Infection control Antibiotic prophylaxis Address all risk factors: nutrition, mobility & skin integrity, glucose control, sterile dressing changes, drive line protection GI function & Nutrition Promote gastrointestinal motility post op Assess pre-albumin levels RED HEART ALARM Rule out power failure or equipment malfunction. Otherwise, there is a low pump flow state. Assess the patient for post-op complications. Reprinted with the permission of Thoratec Corporation Complications: LOW FLOW Low Flow and Low CVP Replace volume Give vasoconstrictors if right heart is weak Check H/H; rule out bleeding Rule out mechanical versus coagulopathy Monitor H/H, platelet, PT, PTT, Fibrinogen, TEG : replace products, administer protamine Monitor chest tube drainage Complications: LOW FLOW High CVP & suction events RV Failure Possible Causes : Any increase in RV afterload; pulmonary HTN, volume overload, acidosis, hypoxia, ischemia, pulmonary embolus Cardiac Tamponade S/S: Hypotension, elevated filling pressures, reduced SvO2, reduced urine output, slowed chest tube output CXR/CT scan Complications: LOW FLOW Other Low Flow Considerations Pump thrombus may see power spikes, grating or rough pump noise, falsely high pump flows, clinical signs of heart failure, increased native pulsatility, hemolysis Treatment: anticoagulant or thrombolytic therapy, possible pump exchange Arrhythmia NO CHEST COMPRESSIONS/ OK TO DEFIBRILLATE Inflow cannula obstruction (septal occlusion) may see reduced pump speed and hear device chatter High afterload Rx with vasodilators Safety Pearls No chest compressions ACLS drugs and cardiac defibrillation OK to give No MRI Avoid getting system components wet Maintain patient equipment and keep a spare system controller and a spare power source with the patient at all times Transitioning care • • • • Psychosocial needs Educational needs Elements for discharge to home VAD support group References O’Shea, G. (2012). Ventricular Assist Devices: What Intensive Care Unit Nurses Need to Know About Postoperative Management. AACN Advanced Critical Care. 23(1) 69-83. Slaughter, M., Pagani, F., Rogers, J., Miller, L., Sun, B., Russell, S. …Farrar, D.(2010). Clinical Management of Continuous-flow Left Ventricular Assist Devices in Advanced Heart Failure. The Journal of Heart and Lung Transplantation. 29 (4S) S1-S39. Thoratec Corporation. (2012). HeartMate II LeftVentricular Assist System LVAS: Instructions for Use. Pleasanton, CA: Thoratec Corporation.