File - Logan Class of December 2011
advertisement

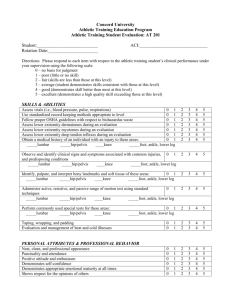
1-15-09 *** Butler and Moseley – Explain Pain…The textbook talks about perception of pain *** *** Midterm 50, Final 50, Lab Exams 40, Quizzes 10 pts (1 per 8 weeks), Paper 5 pts …Total 155 pts *** *** Journal Article on rehabilitation with attached summary between 150-250 words. Can contribute up to 5 points on final grade. Graded on presentation, course, application and clinical importance *** *** E-mail: james.george@logan.edu *** *** Midterm Reading Assignments: Liebenson 1-3 and McGill 5, 6 *** CHIROPRACTIC REHAB What is Rehab? Identifying the tension related to the pain generator (exam), reducing the tension (treatment) and teaching the patient how to keep the tension from returning (patient education and rehab). Evidence Based Practice A combination of what has been proven in the literature, what we have seen clinically and the patients’ goals. You always have to keep in mind your patient’s goals. What is the Biopsychosocial Model? Most pain syndromes, especially sub-acute or chronic cases, involve biologic (structural and functional), psychological and social factors. What are the goals of your exam? ID the pain generator ID the overloading mechanism ID the kinetic linkage (ex…Vary rarely does a patient come in with knee pain without hip and knee involved) How do you know when your patient is better? Decreased Pain Decreased activity limitations Decreased Mechanical Sensitivities (movement that causes an active pain) Improved performance Achievement of Goals The Back Pain Revolution: The Beginning 80% will experience LBP 10% which become chronic and make up 75% of the costs Prescribing disability with rest and medication: Rest and medication lead to disability. You need to get the patient up and moving, as soon as possible and continue to keep them moving. DO NOT PRESCRIBE REST FOR THE LOW BACK! (Waddell, G. Spine 1987) Flynn – Spine 2002; 27: 2835-2843 4 of 5 variables improved likelihood of success with manipulation from 45-95% Symptoms less than 16 days FABQ work subscale score less than 19 (don’t like their jobs) One hip with greater than 35 degrees of IR Hypomobility of lumbar spine (don’t adjust hypermobile segments) No symptoms distal to knee (distal to the knee can indicate radiculopathy and instability) Non-specific low back pain group is a non-homogenous group. Certain patients within the chronic LBP group respond differently to different treatments. These researchers attempted to categorize the patients into subgroups. Active Care (Liebenson) Non Specific LBP may consist of subtypes of LBP Does the pathology model work for back pain? Scott Haldeman (1990) Spine 15: 718-724…He is an MD, PhD, DC….The pathology model is a medical model that says as the symptoms get worse the pathology increase. The model does not work for low back pain. Patients with 8/10 on a VAS scale may be better off than a 4-5/10. The pathology model also says that applying an intervention as the symptoms increase should decrease the symptoms. That is also not true. The patient should feel better within 2 week regardless of what you do. Hadleman’s conclusion is that there is no correlation and that the pathology model doesn’t work for low back pain (don’t get fooled by level of pain). Hip Extension Screen People with LBP don’t distinguish their hips from their low back well. Psoas PIR Relaxation technique for psoas tightness that are easy to do and effective. 1/22/09 MECHANICAL LOW BACK PAIN Pain worse as the day passes: Tight, stiff in the spine over the course of the day that gets worse with time. Dull, Achy Pain Difficult sit to stand: Hallmark of these cases (THINK PSOAS)…Psoas shortens with sitting. They try to hip flex to generate momentum and torque to get up from a seated position. This is not normal. These patients dominate with forward flexion movements. The Thomas test is used to identify. No pain below the knee: Past the knee, indicates a more complicated case. There will be more visits needed. No central provocation: Pushing into the lumbar spine to check for pain or radiation. SLR, WLR negative These are the non-disc, non-nerve low back pain syndromes. These cases are often diagnosed as lumbago, mechanical LBP, lumbalgia. Usually discs are worse in the morning as they hydrate and pressure changes. Mechanical LBP Indications: Symptoms not distal to the knee and no nerve signs Fail the hip extension test Anterior pelvic tilt in standing posture or with gait Pain with sit to stand movements Goals are to address: Weakness: Glut max, abdominals, diaphragm, pelvic floor…Glut max has a tendency to be weak. The patients will use hamstrings to compensate. They’ll extend via the hamstrings instead of via the gluteus max. The diaphragm provides support to the lumbar spine. Glutes are also tied into hip flexors (strong and tight hip flexors and weak, inhibited gluteus). The most common reason is sitting all day. Hypertonicity: Hip flexors, T/L erectors, hamstrings (secondary)…Hamstrings try to help the gluteus out. The hamstrings continue to tighten up. Until they fix the weakness up top, the hamstrings will remain tight. Most people stretch the hamstrings in a position to load the lumbar spine. You will stretch the hamstrings and put the lumbar spine into flexion, loading the spine further. You don’t want to load the lumbar spine, further into flexion. T/L erectors may be taught and hypertrophy, due to lack of hip extension and hinging at the T/L junction. They compensate via T/L extension to extend their hip. Decreased Gluteal Firing Glutes are not used and the patient does not have stability. Lack of glutes is bad for runners and other athletes. Pain Presentation Low back pain can run cephalad (to the head), centralize in the low back or peripheralize into the butt, upper hamstring or lower leg. Posture of Low Back Pain Often anterior pelvic tilt Hip Extension Screen Screen used for most back cases. We want to know how well the hip extends the leg. The back extends the hip in LBP cases, instead of the hip moving the spine. You’ll see loading in the lumbar spine that shouldn’t occur if you move your hips. Hip Extension Screen Examples 1. Flexion of the knee with hip extension = Hamstrings take over 2. 10 degrees of extension (loss of hip extension) = Psoas tightness (prevents hip extension) or neurological weakness Weakness or tightness? You can put them in Thomas test and check the hip flexor. If there is loss of extension with a + Thomas, think psoas involvement. We don’t do these screens in real acute patients. People move differently in acute pain and you can make them worse with a screen. Clinical Information from the Screen Weak Gluteus Max Overactive Psoas, T/L Erectors, Hamstrings Loading into the T/L Junction Activation into the Shoulder Complex The patient should not torque at the back to perform the motion. Tension in the back is an indicator that the screen is not performed correctly. Janda’s Lower Crossed Syndrome Tight and Weak: Erector Spinae, Hip Flexors Long and Weak: Glut Max & Abdominals Training Track for an Inhibited or Weak Gluteus Maximus Brace Bridges (floor and ball) Quadruped Single Leg Raise Rocker Board Wobble Board and balance shoes Kneeling on 2 legs Squats Lunges Reverse Hyper Exercise Release Overactive Muscles PIR Psoas: Patients stuck in forward flexion or seated position over the course of the day. The iliopsoas puts compressive load onto the spine. Releasing the psoas can alleviate the symptoms of the lumbar spine. Self PIR A self technique done to help the treatment “hold.” The technique is used to lengthen and relax the area. Other Soft Tissue Techniques ART PNF Level One Exercise Cat/Camel: Used for Mobility, No Pain, Slow and Controlled, Postural Awareness The exercise can let the erectors go if done correctly. Tightening at the ends of the motion is not indicated and can further the tightness of the erectors. Do not go into the painful zone. Perform this exercise in a pain free range. The exercise is designed for general mobility, not a strengthening exercise. G MAX Bridge Activation of Glut Max Bracing of Abdominals Monitor Hamstrings and Erector Spinae The exercise attempts to consciously activate the glut to where it happens on its own. Runners are notorious for not activating the glutes. Squeezing the butt cheeks indicates activation (you don’t want hamstrings and low back). You want the glutes to dominate. Ball Squats Quad and Glutes are active. The quad may reciprocally inhibit the hamstring dominance. The ball squat keeps the spine neutral. Lunges Can keep the lumbar spine neutral and is a good functional exercise. Deadlift Keeping the lumbar spine neutral is key. It is a good posterior chain exercise if performed correctly. Most patients do not get to this point. Side Bridge Endurance Test Looking at how long you can hold a sidelying position for stability. Most people cannot stabilize at the lateral trunk. Failing this screen may indicate lateral trunk weakness. McGill Table 12.1 Side Bridge is usually held 1 minute to 1.5 minutes. Have them hold for 15-30 seconds in practice. Patients, who fail this, fail this screen quickly. Side Bridge Progression Side Bridge on Knees Side Bridge on Ankles The patient usually feels this exercise in the lateral musculature. They can start this exercise very early in the rehab process. Start active care early and the compliance goes way up. Continuum of Care Key Advice: In/Out of chair, limit prolonged sitting and standing Key Manipulation T/L junction Key Facilitation Exercise: Cat/Camel, G Max, Bridges, Squats, Lunges Key Relaxation or Stretching: Iliopsoas, Rectus Femoris, Hamstring Lab Today Hip extension screen, Psoas PIR, cat-camel Side Bridge Endurance Test Side Bridge Exercise Glut Bridges T/L manipulation LAB 1/22/09 Hip Extension Screen Not done in acute situations (patients move differently with pain)…This is done in sub-acute or chronic situation Don’t give the patient instruction See the lumbar spine (in gown or pull the shirt up). Observe quality of motion…Where is the activity (hip or lumbar spine) Does the movement feel the same side to side? The key is the first 10-20 degrees of motion Example #1: 10 degrees of motion = Weakness of the gluts or restricted from extension via the psoas…Further check, place them into the Thomas test to check for tightness….If no tightness, weakness of the glutes would be present. The motion should be clean with a hinge point in the hips, and not the lumbar spine. If you see torsion in the spine, it can indicate disc involvement. . Example #2: Flexion of the knee = Hamstrings help out and flex the knee while trying to extend the hip. You can palpate the glutes and hamstrings to check for signs of firing during the screen. The key is to find the very dysfunctional person. Find the normal and the abnormal. If you are not sure after the fist couple trials, then it is probably not terribly dysfunctional. In this case, use other screens to find the problem. Example #3: Shoulder Motion = Major dysfunction as the patient recruits extensors up the spine to the shoulder to get extension. Loading of the Spine Tissue tolerance is reached and they have pain. Often times, the patient uses ice & NSAID’s to relieve the inflammatory period. The pain goes away, but returns later. This occurs in cyclical fashion over and over again. Over time the tissue approaches failure sooner and sooner. Psoas PIR 30% Contraction into your hand for 5-10 seconds (hip flexion from Thomas Position) The patient relaxes and you take up the slack Repeat the procedure several times 3-5x Recheck the Thomas Test and Recheck the hip extension screen. This is a relaxation procedure. The contraction is light and taking up the slack is light. A good suggestion is let the weight of the leg take you down to the next barrier and repeat the contraction from that point. Relax and lengthen the muscle. Generating an aggressive stretch actually causes contraction. There will only be a short term benefit from a passive stretch, but greater benefit from the relaxation. In acute conditions, make sure their butt is on the edge of the table. Stabilize the patient as you lower them down into the Thomas position. Make sure the lumbar spine is stabilized and the motion occurs at the hip flexor. A key piece of advice is light contraction to alleviate activation of their lumbar spine. Perform the PIR for several visits and then if needed go for aggressive psoas work like ART and other myofascial releases. Side Bridge Endurance Test They should be able to hold for 1-1.5 minutes We will know if they fail in 15-20 seconds The patient will be sidelying with top leg over bottom leg and on their elbow Perform the test on both sides In some cases patients report feeling it in the shoulder. Make sure the elbow is right under the shoulder to give the best base of support. The patient can also place their opposite hand on their shoulder for further support. Keep the head in neutral posture/position. In most cases, failure is usually greater on one side over the other. The exercises are slightly different from the screen. The exercises are modified to make it less stressful or less painful for the patient. Side Bridge Exercise Knees Bent: Take out some body weight by having the knees bent. Head Straight: Flexion creates a lot of tension in the posterior cervical muscles and should be avoided. Shoulder, hip and knee in a straight line Palpate the lateral trunk to make sure of activation Palpate the neck and upper trapezius to check for tension. 3-5 second holds for 10-20 reps. Increase the time of holds to 10 seconds. Once they hold for 10 seconds for repetitions successfully, then straighten out the legs. Modify the exercise to bridging/slumping up and down from the sidelying, knees-bent position. Glut Max Bridges Lack of glut activation is the indicator. Patient is supine to avoid compressive loads Squeeze the butt cheeks to activate the glutes…Activating the glutes with light contraction is key. You want the glutes tighter than the hamstrings Palpate the hamstrings…You don’t want excessive hamstring firing (less tone than the glutes) Palpate the lumbar spine Perform the bridges once you’ve confirmed that the glutes are active Hip even with the knee (if possible). If the hamstrings are tighter than the glutes, don’t have them bridge. Have them start with glut squeezes instead. Squeeze the glutes 3-5 seconds hold and release. Our goal is conscious activation of the gluteus muscles to get the motor pattern to fire. Some patients may have “Gluteal Amnesia” or lack of firing pattern by the gluteus. Some ideas to trigger firing are: 1).Have them palpate glutes and hamstrings to get more activation 2). Externally rotate the feet to preferentially fire the glutes over the hamstring. Often the glutes are inhibited by chronic LBP. Bridging and squeezes is an activity for lack of Gluteal firing than can be done from athlete to novice. Stay with 8-12 reps and hold 3-5 seconds. It is dependent on age and length of the problem to get the benefit of the exercise. The greater the chronicity of the problem, the longer it will take to groove a motor pattern. The more active you are, the less chance you have of getting chronic LBP. The exercise is not recommended for standing, since the erectors fire up. 1/29/09 Weight Lifting Tolerance Bending over getting a pencil can injure your back. The key is repetitive loading over time that decreased the tolerance of the tissues in your back leading to failure. This is not a one time event, this is an event that occurred over time leading to failure. Hides, Richardson, Sullivan, Hodges – Australian Physiotherapists The multifidi are key to back injury and rehabilitation. Diagnostic ultrasound shows loss of multifidi after back injury. The patient is weaker than before the injury in key areas. The side bridge activates the multifidi. There is low penalty on the spine and it activates deep and superficial muscles. Transversus abdominis firing doesn’t occur well in back patients. Normal people show quick firing vs. back patients had delayed finding of the TA. Stuart McGill said that the TA is not as important as training all the muscles together. Hollowing Sucking in is hollowing, which only activates the TA. The pouching out is the abdominal brace which activates all the muscles at one time. We try to brace rather than hollow. The TA is very small when compared to the remaining abdominal muscles. On EMG we see hollowing not activating the EMG as much as bracing does. Bracing is ideal for daily activities and lifting. Lumbar Flexion Lumbar flexion (repetitive) turns people into LBP patients. Flexion is terrible for the spine. Lumbar flexion with loading makes it even worse. ON diagnostic ultrasound, the motion segments shear anteriorly with flexion. We don’t want this to happen. When the spine is neutral, the fibers of support (longissimus and iliocostalis) are at 45 degrees and support the flexed position better than when going into further flexion. Further flexion, we lose the 45 degrees of support and the fibers orient closer to horizontal. With loading, the fibers are especially susceptible. We are a flexion based society. We need to train extension. Kids mostly have neutral posture, so we adapt a flexion based posture based on society demands (sitting, bending over, etc.). Spinal Loads Profiles 7000 N begins to cause damage in very weak spines (1568 lbs) Competitive lifters manage loads in excess of 20,000 N (4480 lb – McGill, Choewicki, McGill, Normal, 1991) NIOSH limit for repetitive tasks 3300 N The spinal column devoid of its musculature has been found to buckle at a load of only 90 Newton’s (abut 20 lbs) at L5 Motor control system functions well under load. Muscles stabilize joints by stiffening in a manner similar to the rigging on a ship. Ex. Fishing Pole Analogy…The rod buckles with axial force. If the buttresses and supports are added to the rod, it doesn’t buckle. Our spine is the same, as we need to buttress. Safe Exercises Bird Dog Intermediate Quadruped alternating arm and leg movement with an abdominal brace. The exercise focuses on stabilization and is very safe, sparing the spine load. Unsafe Exercises Bent Knee Situps = 3300 N Sit Ups Straight Knee = 3500 N Roman Chair Exercise = 4000 N (890 lb) Superman = 6000 N (1300 lb) The goal is to give safe exercises that benefit the patients and spare loading the spine unnecessarily. Clinical Presentation – Disc Problems Pain worse in the morning (due to disc hydration) Pain is better later in the day Pain past the knee Worse with prolonged sitting (full bodyweight is borne by the spine and this is a flexed position) Pain worse with turning Central Provocation (makes the patient worse with pressure into the spine) Flynn – Spine 2002; 27:2835-2843 4 of 5 variables improved likelihood of success with manipulation from 45-95% Symptoms less than 16 days FABQ work subscale score less than 19 One hip with greater than 35 degrees IR Imaging for Disc Herniations What would you order? Nothing (if your exam is good enough) MRI = Would show a disc, but you would treat them the same regardless MRI study showed 2 groups…1st group when through rehab and the second group had rehab program without being told they had a disc lesion. The second group did better than the first group because they weren’t told what the MRI said. The second group did better, because of fear-avoidance theory and the internalization/hysteria that a disc injury causes. If your patient did not improve, about 2 weeks then pull the trigger on imaging. Posture – By Layers Hamstrings = Tight Gluts = Weak Erectors = tight Scapula = Weak Neck muscles = Tight This is a byproduct of what we do as a culture. Examination SLR/WLR Slump Test = Neural Tension Test Reflex/Motor Flossing – Nerve Mobilization Compression Test Looks at load tolerance and compression fracture. Have the patient stand, come up on their heels, and have their body weight fall on their heels. The patient will point to the area of pain. Seated Compression Test The patient goes from neutral spine posture and pull themselves into the chair. Check for a response. Then, have the patient go into flexion and pull into the chair. Most cases they won’t do this or can’t be in the position for a long period of time. You can use this test as a teaching tool and diagnostic tool. The teaching aspect comes from having the patient avoid the flexed posture and seated position coupled with flexed posture. Hip Extension Screen This should not be done in the acute stage. Do this in the sub-acute stage. Acute Patient Clinical Reasoning Decision to Treat Further Examination Referral Sub-Acute or Chronic Functional Examination: Hip Extension Mechanical Assessment McGill Recommends that for sub-acute exercise training, a safe limit is approximately 3000 N. The key for the sidebridge exercise and other exercises is sparing the spine loading (compressive loading) while activating the core muscles (including the multifidi). The last thing you want is bed rest. Curl UP 2000 N as compared to the side bridge 2600N Cat – Camel Psoas PIR Education – Hip Hinge Hinging at the hips spares the spine You can have the patient assume the “baseball stance”… Continuum of Care Key Advice: Limit Prolonged sitting, flexed postures, excessive stretching, hip hinge, sit to stand Key Joints to Manipulate: T/L Junction, L Spine Key Facilitation Exercise: Brace, Side Bridge, Curl-Up, Bird Dog Key Relaxation or Flexibility: Iliopsoas, Neural Tension Other Factors: Repetitive Lifting or Bending at Work. LAB 1/29/09 Hip Extension Screen Keep a neutral position in the spine. We look for quality of motion in the exam. We are looking for the motion in the hip and not the lumbar spine or through the shoulder. They should not be recruiting other muscles. If the patient fails the hip extension screen, use the Thomas test, Side Bridge Endurance Test, and other screens to rule out stability loss from other areas. Side Bridge Can be used as a test and an exercise. The exercise can be modified from patient with knees as a base of support to feet as a base of support. Make sure to stabilize at the shoulder and have the head in a neutral posture/position during the exercise. The holds are usually3-5 seconds. The test is 20-30 seconds. Glut Bridge Glut Squeezes is the initial step in the exercise, to activate the glutes. Palpate the glutes, erectors and hamstrings. You don’t want too much tension in the hamstrings and erectors. You want a majority of the tension in the glutes. Palpate the back, hips, and hamstrings to check for tension and location of tension. The supine position gives greater advantage for glut activation. Slump Test – Neural Tension Nerves should move, they are not rigid structures. Nerves lose their ability to slide with disc injuries and in some radiculopathies. The nerve is a long rope from the cord to the extremities. If something entangles or impedes on the rope, you get nerve symptoms down the leg. Nerve symptoms can be irritated in the spine or downstream. Start with a supine SLR and the rope is stretched. Often a + SLR with tingling and numbness presents. To distinguish between local spine lesion and neural tension, have the patient flex and extend the neck while performing a SLR. If the lesion is local, then neck motion won’t change the result. If the neck is extended, and motion improves and pain decreases, then neural tension is present because neck motion puts slack in the system. Alternating slack and tension are used in nerve mobilization to release the system of nerve tension. If a local lesion is present, motion of the hip and neck will not alleviate the symptoms. The first part is to check for nerve tension and is done supine. The exercise is done only when neural tension is present, and not a local lesion. The exercise can be done in the seated position. The hip is flexed and the knee extended while the neck is extended to put slack in the system. Then the knee is flexed while the neck is flexed to tension the system. This is done with both alternating. Perform 12-15 times several times daily. The seated position can be done during the work day. David Butler is a source of information for this. There are mobilizations for the femoral nerve, median, ulnar, radial nerves, etc. Central Provocation Push into the lumbar spine when the patient is prone. There will be pain with disc lesions and often radiculopathy. Distinguish the pain from tenderness. Bracing and Birddog “Punching someone in the stomach”…Triggers them to tighten and stiffen, expanding their abdominal cavity. You’ll see pouching out all around the trunk. This is not 100% contraction but 30-50% contraction. Quadruped position unloads the spine. The bracing activation is done 3-5 seconds. Perform 8-12 repetitions. Bracing is the start to the birddog exercise. Do each limb while bracing as a stability test. Have them start by bracing and extending the left hip, then relax. Repeat on the right side with right hip. Repeat with left arm first while bracing, then the right while bracing. When the successfully brace and move each limb successfully, then perform the alternating hip and shoulder motions. Do not twist with the exercise. Emphasize driving the arm and leg straight back and straight up. In some cases, have them brace and do hip extension only if they cannot stabilize properly. There is no hold at the end with the bird dog. Curl-Ups Situps are not a good exercise for the spine. There is a lot of pressure and load of the spine. To properly train the rectus (if needed) abdominis use the curl-up. One leg is bent and the other is straight. Both hands are in the small of the back. Take the shoulders and head, straight to the ceiling 2-3 inches off the table and bring yourself back do. Keep the neck in neutral position. Position them with a little bit of chin tuck. Retract their chin (manually if needed) and have them keep the chin tuck while curling up. A trick is to tuck the tongue to the roof of the mouth for better cervical activation. To make this harder, have the patient pre-brace. Have them tighten as they slowly come up (bracing makes the exercise more difficult). Another trick is to have them lift their elbow and shoulders off the table to lessen the support. Lessening of the support makes the task more difficult. This is a flexion movement that works the rectus and obliques (slightly). The goal with the exercise is to train the rectus safely. Hip Hinge Most patients forward flex to get out of a chair. They do not keep a neutral spine to do so. One of the ways to teach getting up correctly is hands sliding down the thighs and slide hands down legs to sit and get up. Position hands on thighs and come down with the hips. Forward flexion is the enemy. Hip hinging prevents forward flexion while getting up from a seated position. T/L Mobilization Used in pregnancy…This is a long axis distraction maneuver. Come back to the edge of the table. Hands over the head and eyes. Do not have them look down…Have them look forward. Pull up at the T/L junction and lift up. The patient should not come off the table. Sometimes you’ll get a cavitation at the T/L junction. Compress the patient against you. Push them slightly forward to get a relaxation and keep compression. Then lift upward and distract while keeping compression. 2/5/09 MOMS Research Study 599 subjects 67% had Musculoskeletal pain 80% of those with musculoskeletal pain had sleep problems, only 8% of those without musculoskeletal pain had sleep problems Nearly 40% were taking pain meds for pain 85% of those had pain with previous labor Can patient reactions to first chiropractic treatment predict early favorable treatment outcome in persistent LBP? Patients who do better on the first treatment will have a greater chance of making progress over the course of care Clinical Outcomes Most favorable prognostic group 84% reported definitely improved at 4 th visit Intermediate group 63% Least favorable prognostic group 30% Check the movement that hurts. It gives patient feedback as to their problem Mechanical Sensitivities The majority of patients (88%) could be correctly classified as between session improvers or non-improvers based on their within session response to treatment. (Hahne..Australian Journal of Physiotherapy) Evidence Based Guidelines Standard of Care for LBP; Advice Manipulation Exercise (RCGP Low Back Pain Guidelines 2006) UNILATERAL LOWER EXTERMITY Clinical Presentation of Unilateral LE Achilles Tendonitis Patello-femoral syndrome Chronic Hip Pain Groin Pain Plantar Fasciitis Rarely are these cases bilateral. These cases are mostly unilateral. Posture Hyperpronation Lateral pelvic shift Asymmetric Knee Load Asymmetric Heel Load Asymmetric muscular tension Bowstring Effect Overpronation forces compensation at the subtalar joint leading to bowing of the Achilles Tendon. This places stress on the Achilles. The Achilles is predisposed to injury, unless mechanical faults are corrected. Mechanical Sensitivities Lunge Stairs Up from the Floor Toe Raise Lying on the Side SIJ Posterior Pelvic Pain Provocation Test = Knee to 90 degrees and exert posterior force…Localization of pain in SIJ provocation likely involves the joint (simple approach to pain…push on the joint and check for pain and shear) Hip Abduction Screen Watch hip abduction in sidelying position Functional Faults: Lack of Coordination: Could be glut medius Hip Flexion: Psoas Involvement Foot External Rotation: Piriformis Involvement Hip Hiking: QL involvement Decreased Range: Tight adductors may be involved Muscles Involved Shortened Adductors --- Antagonist Overactive piriformis --- Synergist Inhibited Gluteus Medius --- Agonist Kinetic Chain Consequences Poor ankle, knee, hip, SI and L/P stability Frontal plane dysfunction Chronic knee pain, check the hip and the foot/ankle because the knee succumbs to the forces of the hip and ankle (above and below). One Leg Stance Test Arms at Side, Raise one leg off floor Performed with eyes opened and closed 2 chances to maintain for 30 seconds Failure if: Foot is put down Arms reach to grasp something Foot hops ONE leg Stance: Why does it matter? Hip Coordination Foot mechanics and activation Predictor of LBP Patients with LBP shoed a greater variation of reaction time and amount of co-contraction when compared to healthy controls (Spine 2000…Radebold) The research came from Factory Workers. The SLS test predicted future LBP Non-symptomatic subjects, low performance in tests of mobility and standing balance was associate with future back disorders. Knee-Hip and Ankle-Knee Relationship The knee position is “slaved” to the hip and ankle…As the hip and ankle goes, so goes the knee. Clam Exercise Activates the Gluteus Medius…We control patients ability to compensate from the sidelying position. One Leg Stance Matrix Done for failure of SLS. Give them the exercise that reproduced the failure Case Scenario 45 year old male 8 years of left hip pain Bean after horse riding accident Several rounds of PT and chiropractic treatment All imaging negative The patient only loaded the right leg and didn’t load the left leg. He even worked out the right leg to make it stronger to compensate. Visually the girth was increased on the right significantly over the left. Continuum of Care Key advice: Gait/Stance re-education and/or behavior modification Key Joints: Hip Joint, SI Joint, MTP Joints Key Facilitation Exercises: Clam, 1 Leg Stance LAB 2/5/09 Review of Curl-Up: One knee is bent and the other is straight. Have the patient retract their chin, have them lift off several inches off the table or floor. To add difficulty, have them pre-brace. It doesn’t matter which leg you use in the curl-up as the straight leg. Bird Dog Brace first to begin. Straighten one arm while bracing, then the opposite arm, then brace and extend the legs, one leg at a time. Arm and legs are counter-weights, need to be able to balance by bracing. If patient has difficulty, can brace hips for them so they know how it is supposed to feel. The final piece is bracing with movement of alternate arm and leg. Quality of movement is the goal. Unilateral Lower Extremity- SIJ and down Hip Abduction Glut medius is the main agonist and is responsible for hip stabilization. Pt. lies on side. Keep top leg straight with bottom leg bent, having them in neutral sidelying position (without rotation of the torso or pelvis. Slowly raise leg toward ceiling. A). PSOAS = If leg comes into flexion, right away with rocking of pelvis B). TFL = Knee bends a little with abduction C). PIRIFORMIS = Immediate external rotation of leg D). GLUT MED WEAKNESS = Shaky movement E). TIGHT ADDUCTORS = Short ROM Really look at 1st 20-40 degrees to see what is going on. Always double check both sides. Clam Exercise Have knees angle at about 120 degrees, want body straight, knees and feet together. You do not want pelvis to rock backwards. Tell them to slowly raise their top leg as high as they can without compensating with hip. Should be pain free. Once they start getting sore they will not be able to do it properly. Perform 8-12reps a few times a day. Want to eliminate synergist muscles in these exercises and focus on primary muscles. PIR Exercises QL Want patient all they way to the back of the table. Cup under superior leg knee and let leg fall behind table. Once you feel resistance, have pt hike hip, relax, let leg fall, repeat. May need to instruct patient as to what hip hiking is. Hold for 5-7 sec. repeat 3-5 times Piriformis PIR Pt supine, flex hip and knee, push knee toward opposite shoulder. Have patient resist and relax. Repeat several times Adductors PIR 1 or 2 joint Adductor 2 joint Leg stays straight Support opposite hip Adduct leg Ask patient when they start to feel it Back off a little Have patient resist Relax 1 joint Have patient flex knee with leg off side of table Repeat same as above. 2/12/09 Stuart McGill Video Lumbar Shear Test over a Table McGill exerts 2 lbs of shear force into the S1 tubercle to L1 spinous and checks for pain…He then has the patient activate the lumbar extensors and tries to remove pain. Decreased pain indicates that they are a candidate for stabilization. Nerve Flossing Extend the head and extend the knee, alternating with flexing the head and flexing the knee. The maneuver is done on both sides and is done in a slow controlled manner. Make sure the flexion comes from the head, neck and upper thoracic spine, same thing for the extension. There is a pull from one end and relaxation from the other end. Sit Ups vs. Curl Ups Sit ups put the discs at risk. For the curl up, bend one knee, put the hands in the small of the back. The rotation should be mid-thoracic (mid sternum or bra line). If the rotation occurs in the neck, cradle it to decrease motion. Hold the curl up for a couple of seconds. This is a stabilizing, spine conserving exercise. To make the exercise more difficult, lift the elbow from the ground and perform the curl up. Raking the oblique fascia, stimulates greater contraction. Have them fight you as you rake the abdominal muscles and have them perform the curl up. Have them breathe deeply to make it tougher. Raking the fascia will stimulate the core muscles (obliques, TA, multifidi, erectors, RA, etc.). Side Bridge To get into the side bridge position, have them hip hinge into the sidelying position Upper and Lower Abs There is no upper and lower rectus, they fire together. There are neuromuscular compartments in the obliques (posterior, anterior, etc.) Bird Dog with Squares Bird dog with squares are a progression of the bird dog that is very difficult. LAB *** Practical is next week. The practical is in pairs. Each partner will have 1 screen and either 1 exercise or 1 PIR to perform. On the same date, their will be a midterm written exam. *** Review of Hip Hip Abduction test Assess G-med If patient really struggles to perform = G-med weakness…Strengthening Exercise is Clam Shell Foot externally rotates with hip abduction = Piriformis Hip hikes with hip abduction = QL Knee bends and posterior pelvic rotation = TFL Short Range of Motion = Adductors Posterior pelvic rocking without knee bend = Psoas Clam Shell Hand on hip Fingers on ASIS, Thumb in glut med pocket to help stabilize pelvis…You don’t want pelvis rotating posteriorly Perform 8-10 reps a couple times a day. Look to see what synergist muscles are involved: psoas, ql, piriformis, tfl, adductors Hip Adduction PIR Abduct leg until you feel tension, then back off a little Pt pushes with abduction Have patient Relax and feel for muscle to relax Take up the slack Repeat Several Times Can perform one joint or two joint. Don’t perform with an acute groin tear Piriformis Flex the hip and knee, angling the hip to the opposite shoulder Contact patient’s thigh and leg, feel for resistance Patient pushes knee and hip outward against resistance Patient Relaxes Take up the slack Repeat Several Times Acute- start w/PIR, then eventually do soft tissue work (ART, Graston, etc.) Chronic- can start w/soft tissue work (ex. ART TFL PIR Take opposite leg and cross it over affected leg Dr. uses body to adduct affected leg Stabilize top knee and affected leg ASIS Once you feel ASIS start to move, that is when you have patient resist with abduction Keep leg parallel to floor Patient Relaxes Take up the slack Repeat several Times One Leg Stance Screen Have patient stand, find a spot on wall and raise one leg Bring foot to knee (raised leg foot is brought to the knee) Passes, Failures and Indications of SLS Screen Unleveling of Hip or Loss of Balance = G Med Weakness (Hip drop on opposite side)…Failure of Screen Foot should grip ground to aid with balance = Normal Foot Motion (mild-moderate pronation and supination) to Compensate = Normal Excess Foot Motion to Compensate (with or without loss of balance) = Failure Foot Does Nothing and Excess Movement from Elsewhere to Stabilize = Knee and Ankle will wear out sooner due to loss of shock absorption One leg stance is an exercise and screen. Both eyes open and eyes closed can be used. Eyes closed makes the body work differently forcing mechanoreceptors to fire. We spend a good time of walking cycle on one leg, so SLS is important. SLS screen and exercise is particularly good for runners, and LE problems (knee, hip, foot, ankle). Typically, the hip and ankle/foot load the knee, so this exercise is important particularly in knee injuries. Perform on both sides. Short Foot Exercise If foot from one leg stance stays still, do this exercise The exercise helps to activate quadratus plantae Patient is seated Try to perform without using toes…It is difficult to do without the toes as compensation. Small, subtle movement of raising the foot and arch Keep the heel, big toe, and little toe in contact with the floor If the patient cannot perform the exercise, use your hands to “mold” the foot for them If they start cramping, have them stop exercise for now. Lunge with Rotation for Overpronation Have pt. lunge forward and rotate body bringing opposite arm across leg. The exercise can also be performed in single leg stance if patient is unable to lunge.