Orthopaedics 6 – Orthopaedic Paediatrics
advertisement

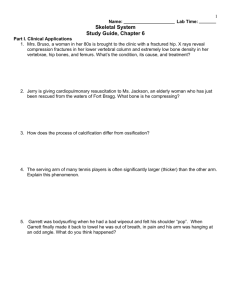
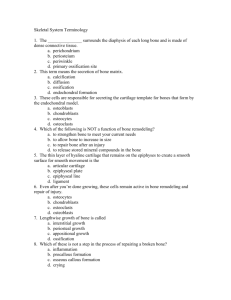
Orthopaedics 6 - Orthopaedic Paediatrics Anil Chopra 1. Describe the anatomy and physiology of the paediatric skeleton 2. Differentiate between paediatric and adult bone and joint pathology 3. Outline the implications of these differences using common paediatric orthopaedic conditions as examples. Normal human growth can be divided up into 7 main stages: Gamete Gametogenesis, meiotic division halves the number of chromosomes Early embryo – weeks 1-2 2 week period from fertilisation to implantation Week 1 zygote repeatedly divides and the blastocyst implants on uterine wall Week 2 amniotic cavity forms and the trilaminar embryonic disc is formed Early embryo usually aborted if serious genetic defect is present Embryo – weeks 3-8 Organ systems begin to develop, usually consists of 3-8 weeks of embryology. The trilaminar disc begins to develop: Different organ buds begin to become recognisable by week 4: dermatome becomes skin myotome becomes muscle sclerotome becomes cartilage and bone Hand plates begin to form by week 5 Individual digits appear by week 6 Upper and lower limbs apparent by week 7 By week 8 the fingers are completely separated and the embryo takes human shape. Foetus – weeks 9-birth Rapid growth occurs Upper limbs become more proportionate in weeks 9-12 Ossification occurs by Intramembranous ossification (the clavicle mainly) Lower limbs become more proportionate in weeks 13-20 and most bones ossify From week 20-birth, the body becomes proportionate Formation of the Bony Skeleton The bony skeleton formation occurs in a number of stages: - condensation of the mesenchymal cells which will eventually become the future skeleton - mesenchymal cells differentiate into chondrocytes - Central portion of cartilaginous anlage (the primordium, the initial clustering of embryonic cells) undergoes chondrocyte hypertrophy and matrix calcification - Cartilage converted to bone by 2 distinct processes o INTRAMEMBRANOUS OSSIFICATION o ENDOCHONDRAL OSSIFICATION Intramembranous Ossification Bone forms directly in collagenous matrix (does not require cartilage) Osteoblasts form a calcified osteoid within a collagenous framework Begins around week 7 in periphery of anlage forming a periosteal sleeve of bone Parts of scapula, clavicle and skull Endochondral Ossification During foetal period primary ossification centres form in diaphyses of long bones Cartilaginous cells hypertrophy and degenerate Vascular ingrowth occurs Brings mesenchymal cells that form osteoblasts and osteoclasts Core of cartilage model is ossified to form primary ossification centre. Ossification continues at the bone-cartilage interface, ossification of long bones occurs before birth, and in infancy for the smaller bones. Secondary ossification centres form in early childhood and occur at the ends of long bones. They result in the formation of a growth plate. The primary and secondary ossification centres fuse in adolescence. Growth Plate Cartilage - has a unique blood supply - is zonal in structure - has a complex biochemistry - matrix mineralisation The role of the growth plate is to produce longitudinal growth by appositional growth of cells within growth plate, including chondrocytes and osteocytes. They result in the production and mineralisation of matrix. The zonal structure of the growth plates represents morphological, metabolic and functional differences: - Reserve zone: relatively inactive - Proliferative zone: centre of cartilage cell replication and growth, has a good blood supply. - Hypertrophic zone: size of cartilage cells increases, and their matrix is prepared for calcification, (3 subzones) o Maturation o Degenerative o Provisional calcification - Metaphysis: vascularisation, bone formation and remodelling occurs here. The bone is converted to lamellar bone. The growth plate is often a site of infection, neoplasms, fractures and endocrine and bone disorders. Disorders of Growth Plates Reserve zone Diastrophic dwarfism pseudoachondroplasia Proliferative zone Achondroplasia Gigantism Type 11 collagen defect Proteoglycan processing defect Defect in cell proliferation Excessive cell proliferation Maturation mucopolysaccharidosis Lysosomal enzyme deficiencies Degenerative mucopolysaccharidosis Lysosomal enzyme deficiencies Provisional calcification rickets Calcium or vitamin D deficiency Primary spongiosa Osteomyelitis Deposition of bacteria Hypertrophic cells extend into metaphysis Metaphyseal dysplasia Secondary spongiosa Osteogenesis imperfecta Osteopetrosis Increase Deformity Hitch Decrease Deformity Plastic deformation – bone bent Incomplete fractures: Greestick: Reduction compleded Torus: Growth plate (physis) - Salter Harris type I and II good prognosos germinal layer not affected (except for femoral head – damage to blood supply) Salter- Harris Classification of growth plate injuries Epiphysis I Germinal Layer II Physis III IV V Metaphysis Salter-Harris type III, IV, and V injuries Damage to germinal area Growth plate arrest Progressive deformity Treatment of Salter-Harris type III and IV injury – anatomical reduction. Secondary ossific centres Apophysis – traction injury (traction apophysis), adolescent growth spurt Fracture healing and remodelling Highest potential in younger children, and metaphyseal fractures Up to 40˚ angulation, and 10-20˚ rotatory deformity corrected 1– asymmetrical physial growth 2 – Bone drift Implications of these differences NAI – non accidental injury/child abuse Fractures at various stages Rib fractures Skull fractures Foot fractures Osteogenesis imperfecta Developmental dysplasia of the hip (DDH) Normal Subluxation Examination – lower limb deformities, spinal deformities, syndromic child associated lower limb deformities: forefoot adducts, club foot, congenital vertical talus, thigh crease asymmetry, torticollis, spina bifida, Clinical findings – limited abduction in flexion (all ages), positive Barlow/Ortolani (less than 3 months), limb shortening and limping (at walking ages) Ortolani Elevate the Femur First, Next Abduct the Hip Dislocation Barlow Adduct the Hip First, Next Push the Femur Posteriorly Treatment – bracing in flexion and abduction (<6 months), preoperative traction, EUA + arthrogram, closed reduction and open tendon release + frog plaster (6-24 months), open reduction +/- Corrective Osteotomy & Hip Spica (>2 yrs) Painful hip in paediatrics – benign in most cases, occasionally sinister Painful knee hip pathology Common conditions: Transient synovitis/irritable hip – o commonest cause of hip pain o pathology: synovial effusion, raised intra-articular pressure o presentation: limp, pain, unable to weight bear, generally well o Examination: hip kept in flexion and external rotation, irritable in internal rotaion, decreased range of movement, sepsis absent o Investigations – X-ray, US o Treatment – reassurance, rest, better within 24-48hrs Osteoarticular infections o Septic arthritis, acute osteomyelitis, neonatal infections, TB o Septic arthritis and osteomyelitis often coexist o Staph aureus < 2yrs o Streptococcus >2 yrs o Septic arthritis: pain, unwell, unable to weight bear, teat with IV antibiotics and arthrotomy and washout o Acute osteomyelitis – unwell, severe pain, unable to weight bear, treat with IV antibiotics, and surgery for suppuration and late cases. Perthes’ disease o Avascular necrosis of femoral head o Unknown aetiology o Necrosis fragmentation healing remodelling o 75% of untreated Perthes’ disease good outcome, 25% poor outcome, area fragments, head deforms, tissue not very strong saddle shaped head o Treatment – surgery (>50% head involvement, >7yrs, significant stiffness) Slipped under femoral epiphysis (SUFE) o Commonest cause of hip pain in adolescents o 40% present with hip pain o predisposing factors: obesity, racial, hormonal (hypogonadism, hypothyroidism, hypopituitarism) o symptoms: pain, limp, unable to weight bear, shortening, external rotation o trethowan’s sign (see picture) o radiology: 2 views mandatory for detection o treatment: surgical stabilization (single screw, urgent surgery – unstable injuries, prophylactic stabilisation – symptoms, hormonal abnormality) Rotational and angular deformities Symptoms Symmetry Stiffness Syndromes Systemic disorders Equinus valgus calcaneous varus normal Normal variants: o Intoe gait – persistent femoral anteversion, internal tibial rotation, forefoot adducts o Bowed legs / knocked knees – Rickets, Blount’s disease, Marfan’s syndrome o Flat feet – reduced longitudinal arch rigid (rare) and flexible (common) flat foot Talipus equilovarus / club foot o Hindfoot: varus (below) equines (right) o forefoot: adductus and cavus o associated abnormalities: reduced muscle bulk, reduced muscle exertion, shorter leg, smaller foot o Conservative treatment: stretching, strapping, serial casting o Surgical treatment – failure of conservative treatment, soft tissue release, bony correction. Neuromuscular disorders o Myopathy o Duchenne muscular dystrophy o Neuropathy o Central – spina bifida o Peripheral – hereditary sensory motor neuropathy o Progressive o Duchenne muscular dystrophy o Hereditary neuropathies o Static o Cerebral palsy – non progressive disorder of immature brain, resulting in abnormal motor function and posture, caused by: birth asphyxia, prematurity, low birth weight. Orthopaedic management: avoid joint contractures (physiotherapy, orthosis, serial casting, Botulinim A toxin, surgical release), correct hip dislocation/sublaxation and scoliosis o Polio Leg length discrepancy o Abnormal leg may be long or short o Less than 2cm difference is common and asymptomatic o Long term consequences: limping, inefficient gait, back pain, scoliosis o Congenital (e.g. DDH, congenital short femur, tibia/fibula dysplasia…) or acquired (e.g. fracture malunion, growth plate injury, neurological damage to limb) o Treatment o Shortening of long leg: 1. Epiphysiodesis for skeletally immature – open growth plate, gradual correction 2. acute shortening for adults Infant: birth – 2 years Most rapid growth after birth Upper limbs grow faster than lower limbs Foot grows disproportionately in lower limbs Half adult height around 2 years High amounts of subcutaneous fat Gross motor development Gait immature Wide based, unstable and irregular High centre of gravity Low muscle to body weight ratio Immature nervous system and posture control mechanisms Child: 2-adolescence Growth and development at slower rate than infancy Many developemental variations occur Physiological variations in growth patterns Genu valgum (a condition where the knees angle in and touch one another when the legs are straightened_ Genu varum (a deformity marked by medial angulation of the leg in relation to the thigh, an outward bowing of the legs, giving the appearance of a bow) Flat feet In toe gait Adolescent Beginning of puberty – skeletal maturity Certain conditions occur in adolescence Scoliosis Slipped upper femoral epiphysis Psychological factors play greater role Obesity Fractures Childs bone is more “porous” Childs bone more flexible Cortical thickness increases in childhood Mature bone has lower collagen content Mature bone has a higher calcium content ADULT BONE = GREATER TENSILE STRENGTH AND LOWER FLEXIBILITY