Chapter 1 - NHS Grampian
advertisement

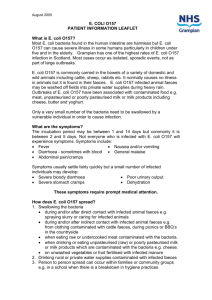
REPORT ON THE OUTBREAK OF E COLI O157 IN CHILDREN ATTENDING MACDUFF PRIMARY SCHOOL, ABERDEENSHIRE JUNE 1999 Compiled by: Dr Arun Mukerjee Consultant in Public Health Medicine (CD&EH) Grampian Health Board Jayne Leith & Fiona Browning Communicable Disease Nurses Grampian Health Board Colin Houston Specialist Officer (Food) Aberdeenshire Council JULY 2000 TABLE OF CONTENTS Chapter Subject Page No 1 Summary/Conclusions & Recommendations 3 2 Introduction 4 3 E coli O157 5 4 Epidemiology 6 5 Environmental Investigations and Results 8 6 Microbiological Investigations and results 9 7 Veterinary sampling and results 10 8 Control measures 11 9 Communication 12 References 13 Appendix 1– Outbreak Control Team Membership Appendix 2 – Sample Enteric Form Appendix 3 – Aberdeenshire Council’s Enteric Investigation Form Appendix 4 – Letter to Parents 1 June 1999 Appendix 5 – Letter to Parents 2 June 1999 Appendix 6 – Grampian Health Board’s E Coli O157 patient information leaflet 14 15 24 26 27 28 Appendices 2 Chapter 1 SUMMARY Four confirmed cases of E coli O157 were notified to Grampian Health Board’s (GHB) Communicable Disease Team and three further cases of enteric illness among children attending one class (3B) of Macduff Primary School, Banff. An outbreak was declared by the Consultant in Public Health Medicine on 2nd June 1999 and an Outbreak Control Team was convened (See Appendix 1 for Membership of Outbreak Control Team). The potential risk factors identified by the Communicable Disease Team included a visit to Duff House, Banff for a class outing and picnic on 19th May. They had also consumed home-made goats’ cheese in class on 26th May. The Communicable Disease Team arranged for the 30 class children to be screened. 3 adults who had consumed the cheese were also tested. Environmental samples from kitchen utensils and refrigerators where the cheese had been kept were submitted for microbiological examination but no organisms where isolated. The cheese had all been consumed therefore none could be submitted for testing. A sample of raw goats’ milk was tested and grew coliforms suggesting environmental contamination. E coli O157 was not isolated from the goats milk. Faecal samples from various animals on the smallholding where the cheese was produced, including the goat, were positive for E coli O157. Both human and animal samples were phage type 21/28 and indistinguishable from each other by pulsed-field gel electrophoresis. Between 27th May and 4th June, 24 children in the class and 3 adults who ate the cheese were confirmed positive for E coli O157 (96%). The high attack rate among the cheese tasters, the shape of the epidemic curve and illness in an adult who did not visit Duff House but tasted the cheese strongly suggests that the cheese was responsible for the illness. The outbreak was controlled by taking joint action with the Aberdeenshire Council Environmental Health & Consumer Protection Service, Aberdeenshire Council Education Service, veterinary section of Scottish Agriculture College and local General Practitioners. Epidemiological information was collected and recorded on the appropriate questionnaires (Appendices 2&3). GHB’s Communicable Disease Team regularly updated families of positive cases, health professionals and the school. Daily press updates after the outbreak control meetings were held. Secondary cases were prevented by strictly adhering to exclusion criteria for positive cases, advising about potential transmission routes of E coli O157 and emphasising the importance of hand hygiene. The outbreak was successfully controlled within a fortnight. CONCLUSIONS AND RECOMMENDATIONS. 1. Consumption of contaminated goat’s cheese was presumed to be the most likely cause of the outbreak of E coli O157 although in the absence of microbiological evidence this could not be confirmed. 2. The risks associated with preparation, storage and service of foods entering educational establishments should be assessed. 3. More research should be focussed on immunity and susceptibility to E coli O157 infection. 3 Chapter 2 INTRODUCTION Grampian Health Board’s Communicable Disease Team received notification from the Medical Microbiology Department of Grampian University Hospitals Trust on Tuesday, 1st June 1999 that a child from the Macduff area of Aberdeenshire had been admitted to Royal Aberdeen Children’s Hospital (RACH) with confirmed Escherichia coli (E coli) O157. The hospital had also admitted another child from the same area with gastro-enteritis on 31st May and a further three on 1st June. These five children reported that their symptoms started between Friday, 28 th May and Sunday, 31st May. Therefore by June 1st the total number of hospitalised children from the Macduff area was 5. The parents of the children were interviewed in hospital on 1 st June at which time Grampian Health Board’s enteric surveillance forms were completed (Appendix 2). Various common risk factors were identified including a class outing and picnic, to Duff House on 19th May and a class tasting of home produced goats’ cheese on 26th May. Duff House, Banff, is a local historic house with grounds that are open to the public. The visit to Duff House was excluded as a causative factor of the gastroenteritis because the first child did not become ill until twelve days after the visit. This is outside the usual incubation period of E coli O157. It was further noted that the families concerned tended to socialise together, and although a communal barbecue had been held on Sunday, 30th May, this was discounted as a causative factor as some pupils’ symptoms pre-dated the barbecue. During the course of the interviews the parents intimated that other children were also absent from class 3B at Macduff Primary School. On 1st June Macduff Primary School was advised that Grampian Health Board’s Communicable Disease Team were treating this incident as a possible outbreak. The Scottish Office, Scottish Centre for Infection and Environmental Health (SCIEH), Glasgow and Grampian Health Board’s Press Team were briefed accordingly. By 2 nd June four of the five children hospitalised were confirmed positive for E coli O157. At this time there were three further suspected cases in RACH. An outbreak was officially declared on 2nd June 1999 and the first meeting of the Outbreak Control Team (OCT) was convened at 2pm that afternoon at Summerfield House. 4 CHAPTER 3 E COLI O157 Escherichia coli (E coli) bacteria are found in the digestive tracts of most humans and animals. There are hundreds of different strains of E coli and usually these bacteria cause no harm (Pennington 1997). The strains of E coli that are capable of producing toxins are described as Vero cytotoxin producing E coli (VTEC). One VTEC strain that is able to cause serious illness in humans is E coli O157:H7 which can be further sub-typed to assist with epidemiological investigation. The bacteria are capable of invading the gut and can produce a toxin that may affect the kidneys leading to haemolytic uraemic syndrome (HUS). Over 15% of healthy cattle and 2% of sheep may carry E coli O157 in their gut. Animals are usually unaffected by E coli O157. However a small number may become ill. Animal faeces contaminated with E coli O157 may in turn contaminate water and soil. It is, at present, unknown how long E coli O157 can survive in particular environments but research indicates that it can survive in soil for several weeks (Maule 1999). E coli O157 can be transmitted to humans in a variety of ways including eating under cooked meat that is already infected, consuming unpasteurised milk or milk products or contaminated water. Transmission can also occur through inadequate hygiene after contact with contaminated soil. Person to person transmission can also occur by faecal-oral route. Inadequate hand hygiene following contact with any of these vehicles can lead to the ingestion of the bacteria. E coli O157 needs very few bacteria to cause infection in a susceptible individual. The incubation period for E coli O157 varies between 1 and 14 days, usually 3-4 days. The symptoms caused by E coli O157 can vary considerably depending on how the individual reacts to the organism. The individual may be asymptomatic but is more likely to have stomach cramps and diarrhoea. This may resolve but occasionally the disease progresses to the next stage where the diarrhoea becomes bloody. A small number of individuals may develop more serious complications including kidney failure (HUS). The disease tends to be more serious in young children and the elderly. Diagnosis is made by culture of stool specimens and typing of the bacteria or by demonstration of rising antibody titre in blood serum. Since the majority of Scottish E coli O157 isolates share the same phage type (21/28), other typing techniques must be performed to distinguish potential outbreak samples from the background of unrelated sporadic cases occurring at the same time. Pulsed- field gel electrophoresis is a DNA fingerprinting technique that subdivides isolates within a particular phage type, thus characterising them more accurately. 5 Chapter 4 EPIDEMIOLOGY The Incident The Head Teacher of Macduff Primary School confirmed that on the 24 th May one pupil brought a cheese into the school for class 3B to taste. The cheese was made from goat’s milk. It was produced on Sunday, 23rd May by the owner of the goat, stored in a refrigerator overnight and taken to school on Monday, 24th May. The cheese was kept in the school refrigerator overnight and taken home by a member of staff on Tuesday, 25th May to be kept in her domestic refrigerator. The cheese was then brought back to school on Wednesday, 26th May, for consumption by class 3B. A small amount of cheese was put onto a biscuit for each pupil. It was ascertained that not all the pupils had eaten the cheese (Table 2) School investigation The Head Teacher confirmed that class 3B comprised of 31 children, one of whom was on holiday throughout the incident (Table 1). She reported that 12 children (39%) were absent from Class 3B on 1st June out of a total of 31. She confirmed that this was unusually high and that no other class was similarly affected. Class lists were faxed identifying children who were absent and who had eaten the goats cheese (Table 2). It was reported that 3 children were on holiday and 2 children had tonsillitis. This left 7 children off with “tummy upsets”. 30 children were present on 26 th May however only 25 tasted the cheese. Upon further inquiry it became obvious that the children started to fall ill from 27th May. Table 1 Composition of Class 3B (All born between March 91 - February 92) Children in class Male 13 Female 18 Total 31 Table 2 Relationship between cheese tasting and infection in children of class 3B ( N=30) Cheese tasters Total who Cases ate cheese positive Attack rate 25 96% 24 Non cheese tasters Total who Cases refused positive cheese 5 0 Attack rate Relative risk 0% Table 3 Relationship between the children tasting the cheese and illness (N =25) Cheese tasters Symptomatic 19 Non cheese tasters Total 25 Attack rate 76% Symptomatic 0 Total 5 Attack rate 0% Relative risk Table 4 Relationship between cheese tasting and illness and infection in adults (N=3) Adults who ate cheese Total 3 Symptomatic 3 Positive 3 6 Attack rate 100% By 4th June a total of 19 children had become ill (Table 3). In addition 3 adults, who also consumed the cheese, developed illness (Table 4). All symptomatic cases were confirmed as E coli O157 positive. One child developed haemolytic uraemic syndrome (HUS) four days after becoming ill which is within the median range of the reported interval for the onset of HUS (EuroSurveillance 2000). None among the cheesemakers household or contacts, including the pupil in class 3B, complained of illness and all were microbiologically negative. Incubation period. Figure 1 Date of onset of symptoms Macduff Outbreak 9 8 Cheese tasted Nos of cases 7 6 5 4 3 2 1 9 9 6/ 9 /0 04 9 6/ 9 /0 03 9 6/ 9 /0 02 9 6/ 9 /0 01 9 5/ 9 /0 31 9 5/ 9 /0 30 9 5/ 9 /0 29 9 5/ 9 /0 28 9 5/ 9 /0 27 5. 9 /0 26 25 /0 5/ 9 9 0 Date of Onset Symptoms developed between 1-9 days after tasting the cheese in those who became ill. This is within the extended incubation period of E coli O157. An incubation period of up to 14 days has been reported in certain incidents (Marsh et al 1992, Kohli et al 1994). All but one child of class 3B visited Duff House 12 days before the first reported illness which is also within the extended incubation period of E coli O157. However, the shape of the epidemic curve (Fig I), the high attack rate among the cheese tasters and illness in one adult who did not visit Duff House but tasted the cheese strongly suggests that the cheese was responsible for the illness. This could not be confirmed by microbiological tests because a sample of cheese was not available although the goat’s faeces were positive for E coli O157. 7 Chapter 5 ENVIRONMENTAL INVESTIGATIONS AND RESULTS The incident was reported to the Specialist Officer (Food) for Aberdeenshire Council on 1 st June 1999. Information was gathered on which pupils consumed packed lunches or school meals. The school kitchen was inspected and the food handlers questioned. The investigating officers were satisfied with the conditions in the school kitchen and with the answers provided by the staff. There was no evidence that the goat had been ill and the owner stated that the teats had been cleaned with anti-bacterial wipes prior to milking. The owner stated that the goat's milk was boiled for one minute before adding the rennet to make the cheese. The milk obtained from the goat to make this cheese was all used in its production. The rennet was only used to make this specific batch of cheese. During a later interview with the producer of the cheese it was confirmed that the milk was not boiled but warmed up. Samples of milk from the goat and the rennet used in the cheese were submitted for examination and reported as negative for E coli O157. The sample of milk did not comply with the Dairy Products (Hygiene) Regulations 1995. The milk contained a total viable count /gm at 30 degrees of 1.3 X 107 and a coliform count /gm at 30 degrees of 1.6 X 102. The cheese was a domestic product, and was not commercially produced for wider consumption. General household implements were used to make the cheese. Accordingly these were swabbed and submitted for examination. Swabs from the washed bowl that contained the cheese were submitted for examination. Swabs from the producer’s refrigerator, the pupil’s refrigerator, the staff member’s refrigerator and the school refrigerator were submitted for examination. The producer’s premises were on a private water supply and water sample was also submitted for testing. Results of all these swabs and samples were reported as negative. 8 Chapter 6 MICROBIOLOGICAL INVESTIGATIONS AND RESULTS Environmental Health Officers from Aberdeenshire Council contacted the head teacher of Macduff Primary School and interviewed the pupils of the class in the presence of their parents using the outbreak investigation form of Aberdeenshire Council (Appendix 3). Faecal sample pots were given to all pupils and teachers of class 3B including those who were absent. A GHB letter and information leaflet about E coli O157 (Appendices 4&6) accompanied the faecal sample pots. Faecal sampling was extended to include three people who were identified as people who regularly drunk the goat’s raw milk. Thirty-one children were registered in the class. One child was on holiday throughout. 30 children in class 3B submitted faecal samples. The adults who consumed the cheese also submitted faecal samples. Table 5 shows that 27/28 (96%) of the samples were positive for E coli O157 but only 22/28 (79%) individuals were symptomatic. Asymptomatic infection with E coli O157 has been reported in investigation of outbreaks (Heuvelink et al 1999) The cheese brought into the class room was small and children only received a small quantity (about a teaspoonful each). Five children were microbiologically positive but did not exhibit any symptoms. At this time little is known about differences in susceptibility and immunity. Table 5 showing the microbiological results Male Female Total Ate cheese 12 16 28 Negative Positive Symptomatic Asymptomatic Propn. +ve 0 1 1 12 15 27 10 12 22 2 3 5 100% 94% 96% One child, not in class 3B, who regularly consumed raw milk from the same goat, was asymptomatic but tested positive for E coli O157. All household contacts of positive cases were tested as per local policy revealing secondary infection in four adults and four children. The E coli O157 Reference Laboratory, Aberdeen reported that all the human samples were phage type 21/28, verotoxin 1 negative, verotoxin 2 positive and they were indistinguishable by pulse field gel electrophoresis. Some cases agreed to take part in a research project running in Grampian at the time of the outbreak. As part of this project, individuals were asked to submit a faecal sample daily for 10 days. Those who did not take part in the research or those who were still positive at the end of 10 days were sampled weekly. The final negative faecal sample was received twelve weeks after consuming the cheese. 9 Chapter 7 VETERINARY SAMPLING AND RESULTS Scottish Agricultural College (SAC) Craibstone was contacted on 2 nd June to arrange faecal sampling of the goat and other animals at the cheesemakers smallholding (Table 6). However the owner had already approached her own vet to do this who liased with SAC. Table 6 Results of microbiological tests on farm animals. Sample type Goat faeces Ewe faeces Lamb faeces Goose / Duck faeces Hen faeces Total no of animals No of samples taken 1 6 5 4 geese / 5 ducks 13 9 9 7 7 No of samples positive for E coli O157 7 8 6 2 3 0 All the positive veterinary samples were E coli O157 phage type 21/28 verotoxin 1 negative, verotoxin 2 positive. The E coli O157 Reference Laboratory reported that the animal samples were indistinguishable in type from each other and from the human isolates by pulsed-field electrophoresis. 10 Chapter 8 CONTROL MEASURES Removal of risk at source During the course of the investigation it became apparent that the most likely source of infection was the homemade goats cheese. After investigation Environmental Health advised that the cheese making operation was not commercial and that the cheese maker only had one goat from which one small cheese was made specifically for the school. All the cheese was taken to school and consumed therefore no sample could be obtained. No other cheese had been made therefore there was no ongoing risk. Case definition A ‘case’ was defined as any individual who tasted the cheese and either developed symptoms of diarrhoea or became positive for E coli O157 by stool examination. Ascertainment of cases All class members including the teacher were asked to submit a faecal sample for testing. Arrangements were made to sample the household members of positive cases in accordance with local policy. Exclusion of cases On 1st June it was agreed that anyone who had diarrhoea or “upset tummies” should be excluded from school until their faecal test results were available. It was agreed at the outbreak control meeting on 4th June to close class 3B. When sufficient children screened negative the class would reconvene. Asymptomatic children from class 3B who tested negative would be re-tested during the week beginning 7th June, with a view to returning to school on 14th June, if the result of the second test was negative. Symptomatic contacts of positive cases were asked to remain at home until the results of their faecal sample tests were available. All positive individuals were excluded from school/work until they had submitted two consecutive negative faecal specimens twenty-four hours apart. The last individual became negative 84 days after consumption of the cheese. Macduff School The OCT recommended that hand hygiene was promoted throughout the school and that sufficient soap and hand-drying facilities were available and that the school toilets be cleaned four times a day. The class was closed on 4th June, as most of the pupils proved positive. It reopened on 14th June. Counselling of contacts The Communicable Disease Team prepared information to be sent home with the pupils of class 3B including routes of transmission of E coli O157 and preventative measures. All parents of positive cases were contacted by the Communicable Disease Team and advised on the precautions to be taken to prevent secondary spread. 11 Chapter 9 COMMUNICATION General Practitioners Local General Practitioners (GPs) and Grampian Doctors On-call Service (GDOCS) were advised of the outbreak by fax. A GP from the locality was invited to become a member of the OCT. Parents A Grampian Health Board letter and information leaflet about E coli O157 accompanied the faecal sample pots that were given to all children of class 3B on 1st June 1999 (Appendix 4 & 6). A second letter addressed to all parents of children at Macduff School was issued on 2 nd June explaining the situation and precautions to be taken to prevent secondary spread (Appendix 5). The parents telephoned the Communicable Disease Team for the results. results were given advice on how to prevent secondary spread. All those with positive School Regular contact was maintained with the school during the outbreak. Advice was freely sought and given. Advice centred on the routes of transmission of E coli O157 and how to prevent secondary spread. Sickness absence in school was monitored. When the class reopened the school were updated daily on who were still excluded. Helpline It became apparent from the number of telephone calls received by the Communicable Disease Team that a dedicated telephone helpline was needed. This was started on 7th June and was manned by trained Health Board Staff. Thirty-seven calls were answered by the helpline although more were received and dealt with by the Communicable Disease Team. Press Parents and Environmental Health Officers in Macduff reported that the press were waiting in the streets and asking residents and parents for comments. It was reported that this was hindering the Environmental Health Officers and causing the parents further distress. The Public Relations Officer from Grampian Health Board reported that the press were anxious for information and telephoned regularly. A press conference was held daily after the Outbreak Control Meetings. The OCT agreed that the Chairperson would be the only spokesperson for the team. 12 References EuroSurveillance, 2000, Surveillance of haemolytic uraemic syndrome in children under 15 years of age in France in 1998.vol 5, June Heuvelink et al 1999, Verocytotoxin producing Escherichia Coli O157 infection in household members with haemolytic uraemic syndrome in the Netherlands. Paed Inf Dis J, 18:709-14 Kohli et al. 1994. A severe outbreak of Escherichia Coli O157 in two psycogeriatric wards. Journal of Public Health Medicine,1994; 16:11-15. Marsh et al. 1992. A restaurant associated outbreak of Escherichia Coli O157 infection. Journal of Public Health Medicine. 114:78-83, Maule A. 1999. Environmental aspects of Escherichia Coli O157. International Food Hygiene .9:21-3 Pennington Group 1997, Report on the circumstances leading to the 1996 outbreak of infection with E coli O157 in Central Scotland, the implications for food safety and lessons to be learned. 13 Appendix 1 Outbreak Control Team membership Dr John Curnow, Chairman, Consultant in Public Health Medicine (CD&EH), Grampian Health Board Dr Jon Cresswell, Consultant in Public Health Medicine, Grampian Health Board Dr Stuart Watson, Registrar in Public Health Medicine, Department of Public Health, Aberdeen University Dr Helen Howie, Senior Registrar in Public Health Medicine, Grampian Health Board Ms Izzy Swanston, Public Relations Team, Grampian Health Board Mrs Shaunagh Kirby, Public Relations Manager, Grampian Health Board Mrs Fiona Browning, CD Nurse, Grampian Health Board Mrs Jayne Leith, CD Nurse, Grampian Health Board Ms L Robertson, Aberdeenshire Council Public Relations Team Mr K McGowan, Aberdeenshire Council Education Department Dr R Hobson, Registrar, Medical Microbiology Department, GUHT Dr I Auchterlonie, Consultant Paediatrician, Royal Aberdeen Children’s Hospital Dr Diana Webster, Consultant Public Health Medicine, Grampian Health Board Mr Colin Houston, Principal Environmental Health Officer, Aberdeenshire Council Dr Fiona Thomson-Carter, Consultant Microbiologist, GUHT Dr A Barbour, Macduff Practice Secretariat Mrs Alison Jones, Grampian Health Board Mrs Diane McGregor, Grampian Health Board 14 APPENDIX 2 GRAMPIAN HEALTH BOARD ENTERIC DISEASE SURVEILLANCE FORM Communicable Disease Team Summerfield House, 2 Eday Road DISEASE TYPE DATE OF NOTIFICATION NOTIFIED BY: DATE OF INTERVIEW LABORATORY CONFIRMATION A PERSONAL DETAILS CHI NO_________________(For office use only) SURNAME FORENAME(S) ADDRESS_________________________________________________________________________ _________________________________________________________________________________ POSTCODE_____________________________TELEPHONE__________________________________ DATE OF BIRTH_______________________ AGE_____ SEX______ OCCUPATION______________________________________________________________________ _________________________________________________________________________________ PLACE OF WORK/SCHOOL___________________________________________________________ _________________________POSTCODE____________________TELEPHONE______________ IF UNDER 5, ATTENDANCE AT PRE-SCHOOL GROUP________YES/NO ADDRESS________________________________________________________________________ POSTCODE____________________TELEPHONE ________________________________________ GP _________________________________________________________________________ ADDRESS________________________________________________________________________ ____________________________________________________________________________ POSTCODE_______________TELEPHONE_____________ ADMITTED TO HOSPITAL DISCHARGED 15 DATE OF ONSET OF SYMPTOMS TIME_______________ SYMPTOMS (Please tick) SYMPTOM YES DATE & TIME 1 DIARRHOEA 2 NAUSEA 3 VOMITING 4 FEVER 5 STOMACH PAIN 6 LOSS OF APPETITE 7 JAUNDICE 8 BLOODY STOOLS 9 HUS* 10 DIC* 11 OTHER * For Office Use Only DURATION OF ILLNESS __________ DAYS PRESENTLY SYMPTOMATIC ___________ YES/NO TREATMENT (DRUGS) ______YES/NO TYPE __________________ REGULAR DRUGS (OTHER) ANTIBIOTICS 3 WEEKS PRIOR TO ILLNESS __________________ OTHER ILLNESS_________________________________________ NOTES: 16 NO NOT SURE LABORATORY RESULTS 17 C HOUSEHOLD AND OTHER CONTACTS DETAILS OF HOUSEHOLD MEMBERS (NOT CASE) IN THE PRECEDING 3 WEEKS BEFORE CASE ILLNESS NAME S E X D O B RELATION SHIP OCCUPATION OR SCHOOL/ NURSERY SYMPTOMS D=DIARR V-VOMIT J=JAUND N=NONE DATE OF ONSET OTHER PERSONS WITH SIMILAR ILLNESS NAME D S E X D O B RELATION SHIP OCCUPATION OR SCHOOL/ NURSERY SYMPTOMS D=DIARR V=VOMIT J=JAUND DATE OF ONSET ANIMAL CONTACTS DOMESTIC YES/NO TYPE ___________________________ FARM YES/NO TYPE ___________________________ SICK ANIMALS YES/NO TYPE ___________________________ DETAILS - KNOWN CASES OF SIMILAR ILLNESS AMONGST CONTACTS OF ANIMALS NAME S E X D O B RELATION SHIP 18 OCCUPATION OR SCHOOL/ NURSERY SYMPTOMS D=DIARR V=VOMIT DATE OF ONSET E RECENT TRIPS TO THE COUNTRY YES WHEN F NO WHERE FOOD/DRINK CONSUMED HOLIDAYS/BUSINESS TRAVEL HOLIDAYS (LAST 3 MONTHS) - PLEASE TICK YES NO ABROAD WHERE __________________________________________ WHEN __________________________________________ FLIGHT OR FERRY NUMBER__________________________ HOTEL_________________________ TOUR OPERATOR_________________________ G DATE FOOD HISTORY FOR FOOD NOT PREPARED IN HOUSEHOLD WHERE FOOD EATEN 19 OTHERS ILL IN PARTY? ANY HIGH RISK FOOD (REFER TO SURVEY FORM) DATE H WHERE WHAT EATEN BY OTHERS? HISTORY OF BAR-B-QUES OR PICNICS YES DATE I WERE THEY ILL? WHERE NO WHAT EATEN HOW COOKED OTHERS ILL? WATER SUPPLY (ALL SOURCES) PUBLIC MAINS PRIVATE IF PRIVATE, SOURCE __________________________________WATER SUPPLY ZONE (Office use only) RECENT PROBLEMS _________________________________________________________________________________ CONSUMPTION OF BOTTLED WATER BRAND __________________________________ _______YES/NO SPRING/RIVER WATER CONSUMED IN LAST 3 WEEKS _______YES/NO WHERE__________________________________________________________________________ 20 J HOBBIES/ACTIVITIES & OUTDOOR SPORTS Y/N WHERE DATES OTHERS ILL? SWIMMING BOATING FISHING CAMPING OTHER K BLOOD DONOR YES REGISTRATION NO NO BLOOD GROUP _________________________________________________________ DATE OF LAST DONATION_________________________________________________________ PLACE L _________________________________________________________ SPECIFIC RISK FACTORS YES NO DETAILS Bird pecking of milk bottle tops Farm visits Nail biting/thumb sucking or the like Children playing with raw vegetables Animals on kitchen surfaces Smoking COMPLETED BY____________________________________ DATE_______________________ LOCAL AUTHORITY________________________________ Revised April 1994 21 FOOD SURVEY FORM FOOD REGULAR SUPPLIER OCCASIONAL SUPPLIER SOURCE IN WEEK PRIOR TO ILLNESS RED MEAT POULTRY:FRESH FROZEN MINCE & SAUSAGES BURGERS DELICATESSEN FOODS COOKED MEAT (COLD) MEAT PIES FISH/SEA FOOD EGGS:HEN OTHERS MILK:PASTEURISED UNPASTEURISED SALAD VEGETABLES FRUIT ICE CREAM OTHER FRIDGE STORAGE DEEP FREEZE 22 TEMPERATURE FOOD HISTORY ONE WEEK PRIOR TO ILLNESS NAME__________ FOOD TYPE DATE OF ONSET_______________ CONSUMED PREPARED MEAT POULTRY MINCE BURGERS SAUSAGES DELICATESSEN FOODS COOKED MEATS (COLD) MEAT PIES SANDWICHES FISH/ SEA FOOD EGGS:CHICKEN OTHERS MILK:PASTEURISED OTHER SALAD VEGETABLES FRUIT ICE CREAM MAYONNAISE 23 NORMALLY STORED WHERE? EATEN OUT WHERE? REMARKS APPENDIX 3 ABERDEENSHIRE COUNCIL ENVIRONMENTAL HEALTH & CONSUMER PROTECTION SERVICE OUTBREAK INVESTIGATION FORM Investigating Officer(s) Ref. No. Date Case Name ………………………………………………. GP……………………………. Address………………………………………………. Telephone No………………………………………………. Postcode……………………… Age …………………..Date of Birth ………………… M/F Occupation…………………………………………………………………………………………………………. Address ……………………………………………………………………………………………………………. Date and time of onset of illness Date ………………………. Symptoms Diarrhoea Time…………………………….. Fever Vomit Nausea (Circle) Severity and duration of illness ……………………………………………………………………………………. Contacts with similar illness and family contacts Name Address Telephone No 1. 2. 3. 4. 5. 6. Overseas Travel YIN If Yes, details: Places and Times of food and drink consumed Name Address 1. 2. 3. 24 Time Food Consumed Type of Food Location Specimen data Report compiled by: Officer……………………………………… Witness…………………………………….. Address of Office ………………………….. ……………………………………………… ……………………………………………… Tel: …………………………… Fax: …………………………... E-mail:…………………………………….. 25 Date/Time Appendix 4 Letters to the Parents 1 June 1999 TO ALL PARENTS OF CHILDREN IN PRIMARY 3 OF MACDUFF PRIMARY SCHOOL Dear Parent We have become aware of 2 children from Primary 3 who have been admitted to hospital with severe diarrhoea. Tests have shown that the illness has been caused by E coli O157. Our experience in the past has shown that the illness is very variable in how it presents and may cause little or no symptoms or just a minor stomach upset. Very occasionally however it can produce severe or bloody diarrhoea and in this case it is important to visit your general practitioner. Because of the variability of symptoms we would like to sample the whole of Primary 3 and we are including with this letter a sample kit for your child. Instructions of how to use the kit are contained in the pack. We would emphasise that the two cases are confined to one class only. The cause is being urgently investigated by the Communicable Disease Team. Symptoms of E coli O157 include diarrhoea, vomiting, stomach cramps and in more severe cases, bloody motions. The organism if often spread from person to person in family groups and it is very important to ensure that children wash their hands after going to the toilet or before handling or eating food. It is also necessary to ensure that individuals suffering gut symptoms should not go to school or work until 48 hours free from symptoms. Experience has shown that only a small proportion of individuals exposed to the bacteria actually become ill. We will endeavour to keep you informed about developments with this incident. If you have any concerns or questions, please contact your GP, but in the meantime we enclose an information leaflet which might be helpful. Yours sincerely, DR JOHN CURNOW Consultant in Public Health Medicine (Cd&EH) 26 Appendix 5 Letter to Parents 2nd June 1999 TO ALL PARENTS OF CHILDREN AT MACDUFF PRIMARY SCHOOL Dear Parent As you are now doubt aware, there have been some cases of E coli O157 at Macduff Primary School. At present, it appears that pupils in only one class are at risk. However, as a precaution against secondary spread of this illness, which usually occurs person to person within households, we advise the following measures: Everyone should practice thorough handwashing and drying after visiting the toilet and before handling food or eating. If anyone develops any symptoms such as stomach cramps, diarrhoea or vomiting they should remain at home and consult their GP. As always, with any diarrhoeal illness we advise that the person affected should stay off work or school until they have been free of symptoms for 48 hours. Many thanks for your assistance. Yours sincerely, DR JON CRESSWELL Consultant in Public Health Medicine 27