High-Risk Antepartum Case Studies: Oralia & Lola
advertisement
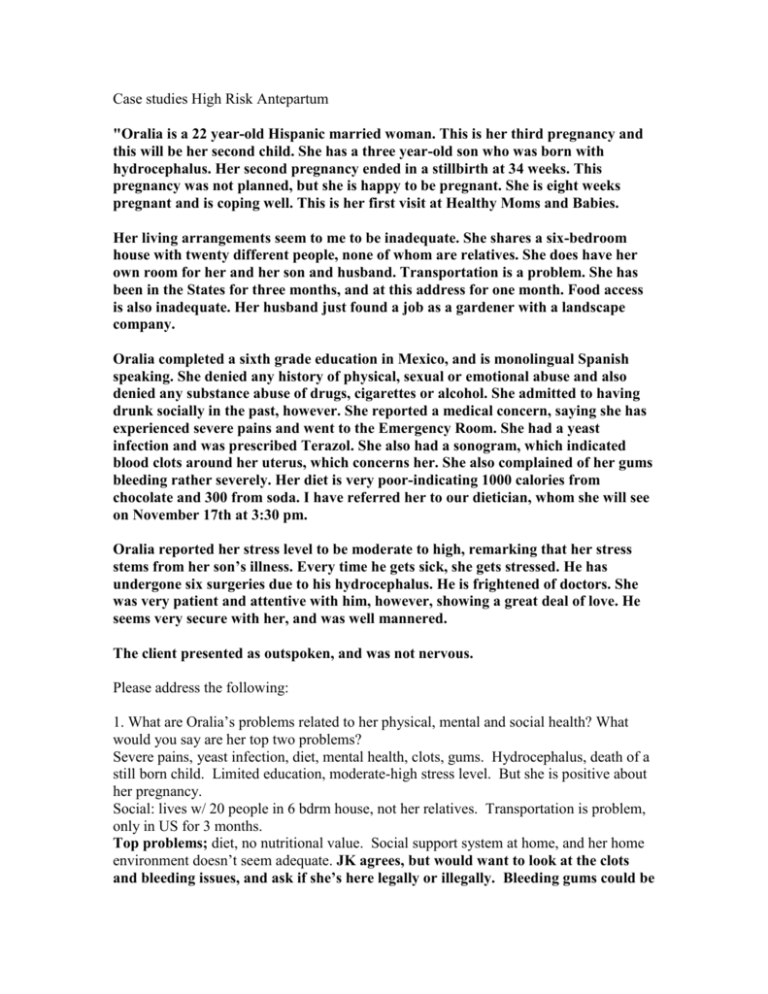
Case studies High Risk Antepartum "Oralia is a 22 year-old Hispanic married woman. This is her third pregnancy and this will be her second child. She has a three year-old son who was born with hydrocephalus. Her second pregnancy ended in a stillbirth at 34 weeks. This pregnancy was not planned, but she is happy to be pregnant. She is eight weeks pregnant and is coping well. This is her first visit at Healthy Moms and Babies. Her living arrangements seem to me to be inadequate. She shares a six-bedroom house with twenty different people, none of whom are relatives. She does have her own room for her and her son and husband. Transportation is a problem. She has been in the States for three months, and at this address for one month. Food access is also inadequate. Her husband just found a job as a gardener with a landscape company. Oralia completed a sixth grade education in Mexico, and is monolingual Spanish speaking. She denied any history of physical, sexual or emotional abuse and also denied any substance abuse of drugs, cigarettes or alcohol. She admitted to having drunk socially in the past, however. She reported a medical concern, saying she has experienced severe pains and went to the Emergency Room. She had a yeast infection and was prescribed Terazol. She also had a sonogram, which indicated blood clots around her uterus, which concerns her. She also complained of her gums bleeding rather severely. Her diet is very poor-indicating 1000 calories from chocolate and 300 from soda. I have referred her to our dietician, whom she will see on November 17th at 3:30 pm. Oralia reported her stress level to be moderate to high, remarking that her stress stems from her son’s illness. Every time he gets sick, she gets stressed. He has undergone six surgeries due to his hydrocephalus. He is frightened of doctors. She was very patient and attentive with him, however, showing a great deal of love. He seems very secure with her, and was well mannered. The client presented as outspoken, and was not nervous. Please address the following: 1. What are Oralia’s problems related to her physical, mental and social health? What would you say are her top two problems? Severe pains, yeast infection, diet, mental health, clots, gums. Hydrocephalus, death of a still born child. Limited education, moderate-high stress level. But she is positive about her pregnancy. Social: lives w/ 20 people in 6 bdrm house, not her relatives. Transportation is problem, only in US for 3 months. Top problems; diet, no nutritional value. Social support system at home, and her home environment doesn’t seem adequate. JK agrees, but would want to look at the clots and bleeding issues, and ask if she’s here legally or illegally. Bleeding gums could be associated w/ diet, but if she’s preg she’s on medicare and can get dental care—but she was here illegally. Also wants to know if this husband is also the father of her first two kids. 2. What are Orelia’s top two strengths? Positive attitude. She is getting prenatal care. 3. What would you like to accomplish at this first prenatal visit? List your top three priorities and give a rationale for why you picked each of these. 1: nutrition for healthy body and baby 2: transportation for prenatal visits, grocery store, etc 3: living arrangement and social support: needs friends in a new country, she has a sick son at home, dad is probably working, who will help? 4. What would you like to know about her pregnancy history? What country did she live in? What prenatal care did she receive with her first pregnancies, did docs state any health concerns in those pregnancies? What’s up with her kid—was he term, vag or C/S, where did she give birth, issues with infertility. Second pregnancy: stillbirth @ 34 weeks, but we’d like to know how the pregnancy went and psych coping after the loss. Any HTN, n/v? What was her nutrition like with her other pregnancies? How much social support did she have w/ her first pregnancies? Did she work or stay home? 5. What would you like to know about her family history? Did she have CHD or DM in her family, who is she living with? What’s it like at home, what work does she have to manage at home, who else is around for helping her w/baby. Does she have family around? Do she or her husband have jobs? 6. What would you like to know about her social history? What country is she from, where’s her family. How involved is her husband? How does she handle groceries, getting out of the house? What does she do to manage stress? How does she get along with people in her household, how many BR are there and are they clean? Does she have access to the kitchen to cook? She was also fatigued and would wake up at 4 am and pack her husband’s lunch. About the US: as RN we don’t interpret but we need to tell MD/NP that the results are there. Yeast infections are not treated with antibiotics but w/ antifungals. She was part of ‘healthy moms and babies’ program. Outcome: did develop gest DM, managed it well w/ diet. Did go into preterm labor, at 33 weeks went to USCF, labor stopped and she delivered at 37 weeks. Happened at same time as Prop 187—when providers were told not to provide care to illegal immigrants. Which providers certainly wouldn’t do. This house didn’t have a stove, but had a hotplate and a microwave. This mommy had medical, even though she’s illegal. That law may change. You can get presumptive medical before you’re even proved as a legal citizen, and get care, and then disappear. High Risk Antepartum Case Study #2: Pregnant woman with pre-gestational diabetes Lola, a 23-year-old newly married woman, was diagnosed with diabetes when she was 16 years of age. Her diabetes has been fairly stable for several years, although she occasionally experiences glucose control problems requiring re-evaluation of her insulin dosage and diet. Lola and her husband are planning to become pregnant in about a year. 1. Explain why Lola and her husband Anthony should seek preconception care as soon as possible. To improve outcome, need to control DM pre-conception, give education, and assess for vascular problems. 2. Identify the maternal and fetal/newborn risks and complications associated with pregestational diabetes, especially if glucose control is not maintained within an acceptable range. What are some of those risks? Risks for mom: poor glycemic control leads to miscarriage. Incr in fetal macrosomia in women w/ vascular disease, leads to more shoulder dystocia, C/S, instrumental birth. Higher risk of preeclampsia and hydramnios [which leads to PPH, etc]. Fetal: stillbirth, congen malformations in CNS, cardio and skeletal systems. Microsomia. Risk for shoulder dystocia and resp distress. 3. One year later, Lola does become pregnant. She is now 4 weeks pregnant. Describe what Lola can expect regarding her insulin needs during pregnancy. 1st tri: insulin will be reduced. 2nd tri: insulin needs are increased 3rd: insulin needs may double or quadruple 4. At her second prenatal visit, Lola's glycosylated hemoglobin was 5%. Explain what this finding indicates. This means: over past 3 months, she has been in good control [within 2.5-5.9%, fair=up to 8, with DM, over 8 means they need help] 5. How should Lola's diet be modified to meet the requirements of pregnancy? Insulin has changed from 1st tri to third, so her diet will also change to manage hyperglycemia. Need to remember her food habits, ethnic background, lifestyle, knowledge, pre-preg weight. Goal is to make her preg as normal as possible. Recommend 3 meals, 2-4 snacks, depending on individual needs. Esp bedtime snack to prevent hypoglycemia in night. Less refined sugar, don’t skip a meal, etc. Less fat and cholesterol, high fiber, no ETOH or caffeine. 6. Lola may experience increased stress as a result of the change in her diabetes associated with pregnancy. What measures could you use to help prevent or reduce Lola's level of stress? Cheers: your blood tests look good, give info about changes in insulin and diet over preg, assess social support and ensure she feels like she has help. 7. During the third trimester Lola asks what she can expect related to her birth. What will you and her physician tell her? Be thorough! You can use bulleted points! No reason to think things will go funny, but we’ll have an IV in her, we’ll manage her fluids and her blood sugar during labor. WE don’t want hyper glygemia during labor b/c then baby is hyperglycemia at birth. CFM. Needs to be in side lying position during labor. She may have a large infant (macrosomia?) or a lot of fluid in her bag of waters. She will likely be able to have a normal birth, but if the kid is really big may call a C/S. If she wants to schedule a C/S, she should do it in AM for better glucose control, her MD will give her specific orders, like when to take her insulin, and NPO. Want epid anesthesia b/c need her awake to assess her blood sugars. JK says: about preconception care, we want her on folic acid. Hopefully all people come for preconception care, but esp w/ DM pts. We want to check with her endocrinologist to make sure her glucose is in really tight control—why? Make sure she can manage it during preg, and if not in control at conception, the rates of miscarriage and fetal anomalies incr. Good control means she’s more at risk for hypoglycemia. Exercise decreases her insulin needs. During labor she’ll be burning sugars and her insulin needs will go down. Pt education; good to talk about changing insulin needs---esp to warn them if their insulin needs are going down at end of pregnancy they need to call MD b/c kid is compromised. OB’s don’t like DM pts going past 38 weeks—incidence of big kids and stillbirth goes up at that point. OB is likely to induce at that point. Breastfeeding and insulin requirements: BF decr insulin requirements. Outcome: vag birth, LGA kid, kid had blood sugar control probs and needed some formula. High Risk Prenatal Case Study #3: Woman diagnosed with ruptured ectopic pregnancy and endometriosis Background: Hillary, a 30-year-old woman with a history of endometriosis, is admitted to the emergency room complaining of severe unilateral lower abdominal pain referred to her shoulder. She is accompanied by her husband John. Hillary is restless and apprehensive and states that she feels lightheaded. Her pulse is rapid, and she is slightly hypotensive. A small amount of vaginal bleeding is noted. To assist with diagnosis a vaginal ultrasound and pregnancy test were performed. A diagnosis of ruptured (tubal) ectopic pregnancy is made. Endometriosis: uterine glands grow outside the uterus. 1. What factors may have placed Hillary at risk for ectopic pregnancy? Mainly the endometriosis, but also she’s 30 yo and we don’t have a lot of medical hx on her—she could have had prev pelvic surg, fertility tx, utero-tubule oddities, and exposure to DES [causes lesions in vag and cervix, and problems in the offspring of women who took DES: incompetant cervix etc, testicular and ovarian CA, etc etc.] We don’t know if she smokes TOB which is another risk factor. 2. Identify the major care management concern related to Hillary's diagnosis. Ruptured ectopic=emergency situation, needs surg, laparotomy to repair tissue damage and hemorrhage. Make sure we prepped blood transfusions, fluids, warmth, positioning. Lie her on back w/ feet elevated to keep hemorrhange controlled. Want to monitor S&S of hemorrhage post op. Ectopic preg are leading cause of tri1 maternal morb& mortality, may cause more miscarriages or infertility. Needs help coping with the loss. Needs advice about having kids in the future or not. 3. State two priority nursing diagnoses for Hillary. High risk for hemorrage [def fluid vol AEB hypotension, tach vaginal bleeding] Pain r/t rupture AEB pt report of pain in shoulder Anxiety r/t emergency situation. 4. Hillary is scheduled for surgery to remove the affected tube. Describe the preoperative and postoperative nursing care measures Hillary will require (be complete.. you can use bulleted points). Informed consent, tell her whats gonna happen NPO VS q 15 Start IV and IVF as ordered Cath if ordered Labs: blood type and Rh factors. Check her serum Hcg, give rhogam if needed Give her time to verbalize her loss Post op: Airway Turn, cough, deep breath Safety [bedrails, anesthesia etc] Methotrexate if ordered: dissolves remaining tissue post op Community referrals for support 5. Hillary and John are devastated by the diagnosis. They tell you that they had been trying to have a baby for 2 years now and thought they had succeeded despite Hillary’s problem with endometriosis. How could you help this couple deal with their loss? Referrals, counseling, support group, educate that this can be great for their relationship or bad for it. Warning about feelings of guilt, anger about loss. Ask about visit w/ a chaplain or advisor. 6. Before discharge Hillary asks you if her endometriosis had anything to do with her ectopic pregnancy. What should you tell Hillary about endometriosis and its effect on fertility and pregnancy? Puts her at risk for ectopic preg b/c of scarring in fallopian tubes. Egg cannot get thru fertilized tube. Both these put her at risk for infertility. In vitro might help get her pregnant again. 7. After Hillary's recovery her primary health care provider places her on Synarel for her endometriosis. This is the first time Hillary will be taking this medication. What would you teach Hillary about this medication? Synarel: synthetic Gonadotropin releasing hormone. Will inhibit development of her endometrium that’s causing trouble—she also won’t menstruate. It’s inhaled—spray into each nostril 1 day after start of menses? Store it somewhere coolish and dark. SE: cramps, hot flashes, bloating, dec libido, vag dryness, etc. Look out for breakthrough bleeding—means she has missed some doses. Needs a barrier contraceptive during this treatment. JK says: if you ever have a woman of childbearing age, on any unit, you need to ask her when her LMP was. Ectopic preg: LMP might have been a missed period, might not be regular periods, or a common sign of ectopic: they have a ‘light period’ recently. RH factor is very important for miscarriage and ectopic. Synarel: right on. It basically put people into menopause. We’ll have her on synarel for 6 mo to decr endometrial scarring and may shrink it. After that if she doesn’t want to get preg, put her on birth control pill b/c that keeps down endometrium. Outcomes: one woman had an IUD, called MD and said she had spotting, and felt weird. Her blood preg test came back negative. She started having abd and shoulder pain (pain likes to refer to the shoulder from under the diaphragm) came to ED and her VS was fucked up, her preg test was positive now. She nearly coded— bled massively into peritoneum, actually lost 5 units of blood, did surg on her w/o anesthesia b/c she was so gone. She did make it. She’s on a surg floor, and no nurses talked to her like she lost a baby b/c they acted like she had an appendectomy. High Risk Case Study # 4: Pregnant woman at risk for preterm labor Background: Keisha is a 24-year-old unmarried multigravida (4-0-1-2-1) woman. She is 15 weeks pregnant and has finally come to the women's health clinic for her first prenatal visit since she is afraid she will have another premature baby. Her first two pregnancies resulted in miscarriages at 13 and 14 weeks. Her third pregnancy resulted in the birth of her 4-year-old daughter at 30 weeks’ gestation. Keisha smokes one pack of cigarettes every 1 to 2 days. Her health history reveals that she has been hypertensive since 20 years of age and often experiences bladder infections. Her stress level has increased since her boyfriend, the father of the baby, has started to “pick fights with her and hit her.” She cannot understand why he is doing this since he never hit her before when he would get angry. Questions: 1. What risk factors associated with preterm labor and birth does Keisha's history reveal? • Keisha has many risk factors that would predispose her to preterm labor: the most common being her multiple pregnancies before 20 years of age (3): 2 resulted in miscarriages and 1 preterm; unmarried; socioeconomic status (poor-I’m guessing); other factors include hypertension; cigarette smoking; frequent bladder infections; high level of stress; being non-white woman (inferring); previous history of inadequate prenatal care; possibility of escalating abuse. Other factors in her life that would increase her probability are excessive physical activity, poor nutrition, uterine anomalies such as fibroids or irritability or cervical incompetence. (p926). Research indicates a link to preterm births and an increased level of prostaglandins released by pathogenic bacteria as with UTI’s. Also, getting lab results for her blood glucose levels (increases risk for HTN), proteinuria, electrolytes, folic acid • As nurses, we would like know what her support system is like? Is there anyone who is able to care for her- extended family, friends, other relatives? We need to address the many factors present in her life and her health that deem her an effective candidate for preterm birth. • (this relates to q. #3) Part of our responsibilities would be to teach Keisha early recognition patterns of preterm symptoms: uterine contractions q 10 min or more, lasting 1 hr or more; lower abdominal cramping and may have diarrhea, dull intermittent painmenstrual like cramps, suprqapubic pain or pressure, pelvic pressure or heaviness, urinary frequency; vaginal discharge that is thicker (mucoid) or thinner (watery) than usual, bloody, brown, or colorless, perfuse, and has an odor, rupture of membranes 2. You recognize that violence has become part of Keisha's relationship with her boyfriend. How would you address this problem with her? Why is he “picking fights” with her when she is pregnant? 3. Keisha asks you what to look for in terms of signs that preterm labor is occurring. “With my daughter, everything seemed to happen so fast without any warning.” What should you teach Keisha about the signs of preterm labor and what to do if she detects them? Her obstetrician did a fetal fibronectin test and it was positive. What does this mean? Keisha needs to watch for the following signs: - uterine contractions occurring every 10 minutes or more and persisting for longer than one hour (painful or painless) - lower abdominal cramping similar to gas pains; may be accompanied by diarrhea - dull, intermittent low back pain (below the waist) - painful, menstrual like cramps - pelvic pressure or heaviness – feeling like the baby is pushing down - urinary frequency - change in character or increase in amount of discharge (either thicker or thinner, change in color or odor) - rupture of water It is important to contact her doctor or NP immediately if she experiences any of these signs – even if she feels like they are just normal symptoms of pregnancy. If she is going into preterm labor it is best that it be caught early so that it can be monitored and slowed down if possible. It is also important that it be caught early so that antenatal corticosteroids can be given to help develop the baby’s lungs. A preterm infant has higher risk for respiratory distress syndrome and intraventricular hemorrhage. Do not wait to see if the symptoms subside or go away, do not attribute them to another cause, do not write them off as normal symptoms of pregnancy. Explain to Keisha that onset of preterm labor is sometimes hard to detect and that she is asking the right question as it’s important she knows the signs! For this reason it’s also important that she comes to all of her prenatal visits! Her obstetrician did a fetal fibronectin test and it was positive. What does this mean? Fetal fibronectins are biochemical markers (proteins) that are used to try and predict risk of preterm labor. They are a protein produced during pregnancy that functions to attach the fetal sac to the uterine lining. Fetal fibronectins are normally present in vaginal secretions until about 22 weeks of gestation and in most pregnancies they are not present again until the end of the 3rd trimester, about one to three weeks prior to labor. The fact that she has them at 15 weeks is normal. If she had them between 24 and 34 weeks we would be more concerned as this could predict preterm labor. Unfortunately, they are better at predicting who will NOT go into preterm labor than who will go into preterm labor. So while a positive test indicates increased risk for preterm labor, it does not guarantee it. On the other hand, a negative test would indicate that in all likelihood she would NOT have preterm labor (94% predictive value). Because she is high risk for preterm labor, a positive test between 24 and 34 weeks would definitely be of concern. A good use of this test for Keisha would be if she were developing symptoms of preterm labor. At this point the test could be redone, and a negative result could help to rule out preterm labor as the cause of her symptoms. 4. Keisha goes into labor at 24 weeks’ gestation. Conservative measures fail to suppress labor, necessitating admission to the hospital. Tocolytic therapy with magnesium sulfate is successful and Keisha is discharged to home care. Home uterine monitoring (HUAM) and nursing telephone consultation has been arranged. How would you prepare Keisha for discharge? How about increasing the effectiveness of HUAM? What kind of life style modifications and activities would you recommend? First of all, I would want to fully understand Keisha’s living situation. If she lives with the abusive boyfriend, I would want to find out if she has supportive parents or if another family member or friend can help to take care of her and her daughter. I would also be sure to set up consultations with a social worker (if she doesn’t already have one). Keisha will also need to be educated regarding placement and use of the home monitoring device – it consists of a pressure sensor that is held against the abdomen by a belt and a recording/storage device that is carried by a belt or hung from the shoulder. Uterine activity is typically recorded for 1 hour, twice a day while performing routine activities. The stored data is then sent by telephone to a nurse and a receiving device prints out the data. The nurse will then call Keisha to discuss results. The effectiveness of HUAM is still controversial and I couldn’t find much in the way of suggestions to increase effectiveness, but there are a few common sense interventions to increase success. First, be sure that Keisha understands what the device measures and can demonstrate proper placement. I would also instruct her to try to use the device consistently – place the sensor on her abdomen in the same way every time, use the same time of day (to help her remember), use in a quiet room (to eliminate interference from background noise). Life-style modifications / activities: There are so many issues for Keisha to manage. If bed rest is required, she will need help caring for her 4-year old daughter. I would educate or re-educate regarding the increased risks she is putting herself and her baby through by smoking, and encourage her to stop or reduce the amount of cigarettes she smokes. I would discuss nutrition, particularly with regard to her hypertension (lots of fruits and veggies, lean meat, limit salt and refined foods). I would discuss the importance of limiting external stress (the boyfriend) and see if she has other support. As far as activities go, I would find out what kinds of quiet activities she likes and suggest ways to organize her day. I would suggest a schedule to help alleviate boredom. Hygiene, dressing, uterine monitoring, and eating meals will probably consume a lot of her day. Examples of quiet activities might be reading, puzzles, journaling, artwork or crafts of some kind, or movies. 5. Keisha comes into the hospital in labor at 30 weeks gestation. She has pre-term premature rupture of the membranes (PPROM). She s given a dose of betamethesone. Why was given this medication? She is also asked if she would like to transfer to UCSF or stay here. How would you facilitate her decision-making about transferring or staying put? What kind of information would you give her? Betamethasone is: a corticosteroid that is used off label, it stimulates fetal lung development by causing the baby to release enzymes that in turn cause surfactant to be made. Not always recommended in women with PPROM. It is a jump start to the kid’s lungs, and if it can be given 24-48 hours prior to labor, then it has a chance of preventing respiratory depression, intraventricular hemorrhage and necrotizing enterocolitis. About transfer to tertiary center: preterm births have better maternal/fetal outcomes. However, this can lead to more anxiety, and can make it hard for family to visit. In this woman’s case, it may relief some stress to get away from her man for a bit. She may have some stress about money, and should be made aware that UCSF has a Financial Hardship form available (that requires a tax return). I would tell her that the choice to transport may be stressful, but that it is the best choice for her daughters’ survival. Not to mention that the view from UCSF L&D is worth the trip for herself and her family. JK says: Risks: DV (domestic violence), premature prenatal care. Do abortions/miscarriages put her at risk? Yes, if they happened after tri 1. Mandating reporting: we have to report what? If you read the law it’s really fuzzy on reporting what she admitted, her report of DV. You have to report rape, you have to report if you treated her for an injury, but she didn’t have an injury, and so we don’t really have to report it. The issue is also that she will likely stay with this guy, and that the incidence of death is higher if interventions are made or she leaves. But one factor is that the more people know that she’s being beaten, she’s less likely to be killed. WWJD? JK would talk to her about it and say it’s not ok, and that she doesn’t have to report it, but what can be done etc. Reporting is to the police w/in 24 hours. If there’s a gun in the house, JK really loses it and will work w/ the woman to get out or get the gun out. Also animal abuse goes in this party. Usually the kids are also abused. There is a relationship btwn preterm labor and DV. Kicks to abd are more common DV injuries when a woman is pregnant. 8% of preg women are beaten according to the book—BUT JK thinks that’s much higher. Most women who are killed have seens a health care provider in the last 6 months. Yes, there is a connection btwn substance abuse and DV, but its like a chicken and egg issue. Some PCP’s won’t report b/c they have to be called to testify, they lose money, it’s stressful, etc. Sign of preterm labor: “Do you have a ‘balling up’ feeling in your lower abd?” That’s a really predictive question/sensation for preterm Home monitoring: does it do any good? Let’s remember that she has a 4 yo kid who doesn’t want her to lay around. Also, does she have support to get groceries and stuff if she’s on bedrest. Indicator that they are on bedrest: they hate you when they come for her visit—if they are all happy they aren’t really staying in bed. Outcome: she did fine! She delivered at 32 or 33 weeks. Stayed with the partner, don’t know what happened at follow up b/c her medical ran out. High Risk Pregnancy Case Study # 5 Unplanned pregnancy with spotting Background: Ruby is a 45 year old G4P2T1A0L3 divorced woman. Her youngest child is 23 years old. Ruby is an art teacher at a local middle school. She had been having unusually heavy, irregular periods for approximately 6 months and her previous MD told her she was probably in "the change of life." She has not had a period for 3 months. During that time she has been fatigued and experiencing nausea and vomiting at least twice a day. She is 5'4" tall and weighs 140 pounds. Despite her nausea and vomiting, she thinks she has gained about 5 pounds in the last 3 months. Visit today: She comes to your clinic today to get information on menopause and to find out why she is feeling so sick. You convince her that a pregnancy test would be a good idea and to her shock it comes back positive. Her physical exams revels a 16 week size uterus and a FHR of 148. She is also having some spotting. She is going to get into nursing school in the Spring and so has just finished her series of the HepB vaccine. Questions: 1. What is the most likely reason Ruby had heavy periods? Over ½ of women over 30 have heavy. Means change tampon/pad 2x hour. Often eggs are released immature and lots of estrogen goes with them and builds up the uterine lining. The egg matures and usually spits out progesterone to stop the buildup, but in older women their eggs don’t mature and so their lining grows big. 2. What are the risk factors associated with this pregnancy? Age, chromosomal abn. Miscarriage, previa, fetal distress, LBW, growth restriction, HTN, preeclampsia, gest DM, C/S, instrumental birth. Basically at risk for everything. 3. What screening tests are available to screen for congenital anomalies? Early dx: intrauterine surg, termination, etc. US: limited, helps assess gest age, amniotic fluid, etc. Specific measures oligo or polyhydramnios AFI: amniotic fluid index: how much juice ya got in there Amniocentesis: after 14 weeks, find alpha-fetal protein means NTDs, spina bifida, abd wall defects, and metabolic d/o CFS: remove a little placenta transcervically or abdominally. PUBS: “pubes?” Fetal blood sample from the unbilical cord. MRI: soft tissue abn, metabolic abn, etc. 4. List five common symptoms and signs of menopause. Mood swings, hair chages, insomnia, hot flashed, dryness, heavy bleeding, fatigue 5. What information could you use to try to determine Ruby's due date? Hasn’t had period for 3 mo, if she remembers first day estimate with Nagel’s Rule. Only 5% of women deliver on this due date, but most are born w/in 10 days of due date. If she has irregular periods or don’t remember date, a US will help. Baby can be measured as early as 5-6 weeks. Best time to estimate w/ US is 10-18 weeks of preg. 6. Ruby's uterus is bigger than how many weeks pregnancy she is. Name at least two possible reasons for this discrepancy. Incorrect date of conception could make a big difference—most common reason. Incr amniotic fluid, or have a big uterus. Multiple gestations. Endometriosis thickening the uterus (this is a new one to JK), or fibroids [benign tumors]. 7. Give some possible reasons for her spotting. Sometimes ya just do. Or b/c of fibroids, threatened miscarriage, yeast infex, vaginosis, beta strep, partial previa, chlamydia 8. Are there risks associated with getting the HepB vaccine during pregnancy? It is ok to get it b/c it’s not a live virus. CDC says it’s not contraindicated but that there’s not a ton of data. Preg women at risk in preg should be vaccinated. SE: redness, swelling at site, a little fever. Jk say: 1/40 change of chrom abn in women at this age. Last period was 3 months, so go straight to US. Outcome: b/c of abn periods, her MD put her on HRT b/c of menopausal symptoms, then she said she felt really really weird, and it was the pregnancy. HRT during pregnancy can be a risk factor for fetal abn. You can get preg on HRT. Yay! Amniocentesis, baby was normal boy and they got married, delayed RN school for a year, her partner had a vasectomy, and everything was happy.