Congenital anomalies of the lower urinary tract
advertisement

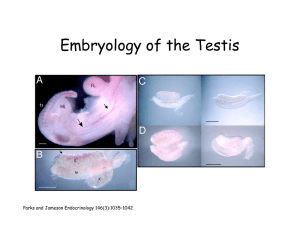
Congenital anomalies of the lower urinary tract Male epispadias is a rare anomaly, with a reported incidence of 1 in 117,000 males. Most male epispadias patients (about 70%) have complete epispadias with incontinence (Gearhart and Jeffs, 1998). Epispadias is explained by a defective migration of the primordium of the genital tubercles, which migrates toward the midline superior to the cloacal membrane to form the genital tubercle at about the 5th week of gestation. Surgical Management The objectives of repair of penopubic epispadias include achievement of urinary continence with preservation of the upper urinary tracts and the reconstruction of cosmetically acceptable genitalia. The surgical management of incontinence in penopubic epispadias is virtually identical to that in closed bladder exstrophy. In patients with complete epispadias and good bladder capacity, epispadias and bladder neck reconstruction can be performed in a single-stage operation. Urethroplasty formerly was performed after bladder neck reconstruction (Kramer and Kelalis, 1982a; Arap et al, 1988). However, results with the small bladder associated with exstrophy (Gearhart and Jeffs, 1989a) and the small bladder associated with epispadias (Peters et al, 1988) have led us to perform urethroplasty and penile elongation before bladder neck reconstruction. A small, incontinent bladder with reflux is hardly an ideal situation for bladder neck reconstruction and ureteral reimplantation. Before bladder neck reconstruction there was an average increase in bladder capacity of 95 ml within 18 months in those patients with a small bladder capacity initially associated with epispadias and a continence rate of 87% after the continence procedure (Peters et al, 1988). In a recent series by Ben-Chaim and colleagues (1995b) composed exclusively of patients with complete male epispadias, bladder capacity increased by an average of 42 ml within 18 months after urethroplasty. Nine (82%) of 11 patients were dry day and night after an average of 9 months. Neuropathic Dysfunction of the Lower Urinary Tract At least 25% of the clinical problems seen in pediatric urology are the result of neurologic lesions that affect lower urinary tract function. As pediatric urology developed in the latter half of the 20th century, urinary diversion initially was the mainstay of treatment for these children with either intractable incontinence or normal or abnormal upper urinary tracts (Smith, 1972). Before a urodynamic study is performed, it is important for the child and the family to have full knowledge of the procedure. Therefore, an explanation of the test and a questionnaire are sent to each family before the appointment. A booklet is provided so that parents will know what to expect and can explain the test to their child, or the child can read about it if he or she is old enough. Attempts are made to minimize anxiety in children who are able to understand what will happen by providing reasons for specific portions of the test and explaining exactly what the child will experience. The questionnaire tries to elicit information about the mother's pregnancy history, the child's birth and development, his or her current bladder and bowel habits, and any other information that might be pertinent at the time of the procedure. A small balloon catheter is passed into the rectum at this time to measure intra-abdominal pressure during the cystometrogram to identify artifacts of motion and monitor increases in abdominal pressure during the filling and emptying phases of the study (Bates et al, 1970; Bauer, 1979). Uninhibited contractions and straining to empty can be clearly differentiated by this maneuver. Before the bladder is filled, a urethral pressure profile is sometimes obtained by infusing saline through the side-hole channel at a rate of 2 ml/min as the catheter is withdrawn at a rate of 2 mm/sec (Yalla et al, 1980). Another way of determining maximal urethral closure pressure is by measuring the leak point pressure at various stages of bladder filling as well as with a bladder contraction or Valsalva maneuver (Ghoniem et al, 1990; Homma et al, 1999). When the maximum resistance is known, the catheter is positioned so that the urethral pressure port is located at that or any other point of interest. This area can then be monitored throughout the urodynamic study. Urethral pressure profilometry (UPP) measures the passive resistance of a particular point within the urethra to stretch (Gleason et al, 1974). Many factors contribute to this resistance, including the elastic properties of the tissues surrounding the lumen and the tension generated by the smooth and skeletal muscles of the urethra, which are constantly changing during the micturition cycle (Fig. 64–1) (Abrams, 1979; Evans et al, 1979). Nocturnal Enuresis Enuresis is defined as involuntary voiding; when it occurs at night it is termed nocturnal enuresis, and daytime incontinence is termed diurnal enuresis. Because urinary incontinence occurs normally in infants and young children, its significance depends on the age of the patient, parental expectations, and social and cultural factors. Approximately 15% of children still wet at night at age 5 years. Although NE persisting after this age or until the child enters school generally causes concern, it is not until age 7 years that most parents, peers, and physicians begin to expect dryness, because the NE interferes with socialization (Moffatt, 1994). In contrast, diurnal enuresis that persists or recurs after toilet training may be a problem. More girls than boys are dry both day and night by the age of 2 years, and NE is 50% more common in boys than in girls. NE has a spontaneous resolution rate of 15% per year, so that by age of 15 years it persists in only 1% of the population (Table 64–11). More than 80% of enuretics wet only at night and have no other abnormalities in their urologic history; they are classified as having monosymptomatic NE (MNE). This subgroup of patients with MNE have such unified features that they must be clearly distinguished from patients who have both nighttime incontinence and daytime symptoms (urgency, frequency, or incontinence). Most nocturnal enuretics have never been dry; their incontinence is termed primary enuresis. Unfortunately, the development of urinary control is not always final. Approximately 25% of children who attain initial nighttime dryness by 12 years of age relapse and wet for a period averaging 2.5 years. These children have secondary enuresis. MNE is a symptom rather than a disease. A number of theories have been proposed to explain why children with MNE fail to recognize or respond to their full or contracting bladder during sleep. Although these theories, which include behavioral, genetic, developmental, neurologic, psychological, urodynamic, and organic causes, are diverse and may be able to explain selected cases, there is no single explanation for this symptom, and in each individual multiple factors may be operative. Clearly, the vast majority of children with MNE do not suffer from psychiatric, neurologic, or urologic disturbances, and investigation and treatment along these lines is both inappropriate and unrewarding. Treatment A number of treatment modalities have been used for NE, but their effectiveness, even in controlled studies, has been difficult to assess because of the high spontaneous annual remission rate (15%) and the extremely high placebo improvement effect, which can exceed 65% (Mishra et al, 1980). Proven, reproducible, and effective therapy has evolved along two lines: drug therapy and behavioral modification. Effective pharmacologic therapy exists for MNE but does not include sedatives, stimulants, or sympathomimetic agents. Anticholinergic therapy has likewise been relatively disappointing, with an effectiveness ranging from only 5% to 40% (Person-Junemann et al, 1993; Kosar et al, 1999). Although anticholinergic agents have been shown to increase the functional capacity of the bladder, improvement in enuresis after therapy to expand the bladder occurs in fewer than half of these cases (Johnstone et al, 1977). However, anticholinergic agents are extremely effective for certain subgroups of enuretics; they are very effective (87.5%) in treating patients with combined day and nighttime wetting and those with proven bladder instability (Kass et al, 1979). Imipramine, typical of a class of tricyclic antidepressants, has been effective in a large number of well-controlled clinical studies. It can cure enuresis in about 40% to 50% of cases and results in improvement in another 10% to 20%. However, discontinuation of medication causes relapse in up to 60% of patients. Clinical response has been shown to correlate with plasma levels (Jorgensen et al, 1980; De Gatta et al, 1984). However, routine measurement of imipramine or its metabolites is not clinically useful (Devane et al, 1984), because normal or even high plasma levels do not ensure a response. The usual recommended dose of imipramine is 25 mg for children between 5 and 8 years of age and 50 mg for older children (0.8 to 1.6 mg/kg/day), given as a single dose shortly before bedtime. This produces a therapeutic plasma concentration in only 30% of patients. Care must be exercised when prescribing higher doses because of potential toxicity. Desmopressin (DDAVP) . Reduction of urine output at night is theoretically attractive for treating bedwetting. However, simply limiting fluids or using diuretics during the daytime to produce relative dehydration at night has not been effective (Scott and Morrison, 1980). In contrast, manipulation of antidiuretic hormone (ADH) levels has proved to be useful because some enuretics demonstrate reduced nocturnal vasopressin concentrations and have nocturnal polyuria (Norgaard et al, 1989c). DDAVP, an analogue of vasopressin and free from its dangerous and unpleasant side effects, has been shown to have a significant, albeit temporary, antienuretic effect because it produces a state of nocturnal antidiuresis. It can be given intranasally or orally, it has no pressor or smooth muscle activity in the therapeutic dose range, and its effect lasts 7 to 12 hours. In double-blind studies, DDAVP was more effective than placebo in treating enuresis. The usual clinical dose ranges between 20 and 40 μg per night for the nasal spray and between 200 and 400 μg per night for the tablet; response may be dose dependent. Efficacy is similar in oral and nasal formulations (Fjellestad-Paulsen et al, 1987; Matthiesen et al, 1994; Skoog et al, 1997). Phimosis At birth, there is a physiologic phimosis or inability to retract the foreskin in the majority of neonates because natural adhesions exist between the prepuce and the glans. During the first 3 to 4 years of life, as the penis grows, epithelial debris (smegma) accumulates under the prepuce, gradually separating the foreskin from the glans. Intermittent penile erections cause the foreskin to become completely retractable. By 3 years of age, 90% of foreskins can be retracted, and fewer than 1% of males have phimosis by 17 years of age (Oster, 1968). Early forceful retraction of the foreskin generally is not recommended, because recurrent adhesions between the de-epithelialized glans and foreskin may occur, and a cicatrix may form at the tip of the foreskin, causing secondary phimosis. However, in boys older than 4 or 5 years of age and in those who develop balanitis or balanoposthitis, application of a topical corticosteroid cream (e.g., 0.1% dexamethasone) to the foreskin three to four times daily for 6 weeks loosens the phimotic ring in two thirds of the cases and usually allows the foreskin to be retracted manually (Monsour et al, 1999). Topical corticosteroids are beneficial even if the foreskin is involved with balanitis xerotica obliterans. Formal lysis of adhesions is rarely indicated. In uncircumcised boys older than 7 or 8 years of age with phimosis that is resistant to topical corticosteroids and in boys with phimosis that causes ballooning of the foreskin or recurrent balanitis, strong consideration should be given to performing a circumcision or dorsal slit. In pediatrics, few topics generate as much controversy as whether the newborn male should undergo a circumcision, perhaps because it is the most common surgical procedure in the United States and because it is usually performed for cosmetic reasons. In 1975, the AAP declared, "There is no absolute medical indication for routine circumcision of the newborn" (Thompson et al, 1975). This stance was supported by the American College of Obstetricians and Gynecologists. Reasons given in support of circumcision include prevention of penile cancer, urinary tract infection (UTI), sexually transmitted disease (STD), and phimosis, as well as lessening of the risk of balanitis. The Undescended Testis The cause of cryptorchidism is multifactorial. The undescended testis can be located anywhere between the abdominal cavity and just outside the anatomic scrotum. Less commonly, the testis can also migrate to ectopic positions outside of the scrotum, not along the normal path of descent. Cryptorchidism is a term that has been used interchangeably with the term undescended testis. Both terms refer to an abnormally positioned testis, but cryptorchidism literally means "hidden testis." Therefore, undescended testis may be a more appropriate term, because most testes that are not within the scrotum at birth are detectable by palpation. In order to fully appreciate the diversity of this congenital disorder, one must concede that this is not a single disease process with a common pathogenesis but a group of commonly recognized clinical abnormalities with multiple etiologies. Isolated cryptorchidism is one of the most common congenital anomalies at birth, affecting upward of 3% of full-term male newborns (Scorer and Farrington, 1971; John Radcliffe Hospital, 1992; Berkowitz et al, 1993; Thong et al, 1998). Unilateral cryptorchidism is more common than bilateral cryptorchidism, which occurs in 1.6% to 1.9% of boys. Classification By definition, cryptorchidism is a developmental defect in which there is failure of the testis to descend into the scrotum. Although this is a useful general definition, there is considerable anatomic variation among cryptorchid testes. In addition, classification by anatomic position alone no doubt underestimates the variable anatomy, physiology, etiology, and natural history of the undescended testis and skews many published studies. Anatomic variation in testicular size and consistency, epididymal and vasal anomalies, and associated patent processus vaginalis or inguinal hernia should be taken into account. These factors reflect the dimorphic nature of male sexual differentiation and suggest that multiple etiologies may be responsible for the variations in phenotypic expression. Tenets of Treatment The important tenets for the treatment of a child who presents with an undescended testis include the following: Proper identification of the anatomy, position, and viability of the undescended testis Identification of any potential coexisting syndromic abnormalities Placement of the testis within the scrotum in a timely fashion to prevent further testicular impairment of either fertility potential or endocrinologic function Attainment of permanent fixation of the testis with a normal scrotal position that allow for easy palpation No further testicular damage resulting from the treatment Definitive treatment of the undescended testis should occur before 1 year of age. Because spontaneous descent occurs in most boys by 3 months of age and uncommonly thereafter, consideration for earlier intervention should be made to theoretically prevent complications of cryptorchidism that may be manifested before 1 year of age. Approach and timing should be predicated on the anatomic position and whether both testes are undescended. There are two types of medical treatment for the undescended testis: exogenous hCG and exogenous GnRH or LHRH. The mechanism of action in both cases increases serum testosterone production by stimulation at different levels of the hypothalamic-pituitary-gonadal cascade. This therapy is based on experimental observations that descent is androgen mediated, involving testicular synthesis of the active metabolite in high local concentrations (Rajfer and Walsh, 1977). hCG stimulates Leydig cells directly to produce testosterone, whereas GnRH stimulates the pituitary to release LH and thereby promote testicular production oftestosterone. Serum testosterone levels during therapy for cryptorchidism in prepubertal boys are much higher with hCG than with GnRH (Rajfer et al, 1986). Surgical Treatment It is very useful to examine the child after the induction of general and regional anesthesia to reaffirm testicular position, or to attempt to establish testicular position in the case of a previously nonpalpable testis. With anesthesia, the anterior abdominal musculature relaxes, offering the surgeon the opportunity to perform a more thorough physical examination in the occasional case in which the initial examination was complicated by body habitus, uncooperative behavior, or guarding. In general, success rates for orchiopexy are directly related to anatomic position of the testis. The 1995 analysis of surgical therapy for undescended testes by Docimo revealed an orchiopexy success rate of 92% for testes below the external ring, 89% for inguinal testes, 84% for microvascular orchiopexies, 81% for standard abdominal orchiopexies, 77% for staged Fowler-Stephens orchiopexies, and 67% for standard Fowler-Stephens orchiopexies. Varicocele Dilated and tortuous veins of the pampiniform plexus of the spermatic cord are found in approximately 15% of male adolescents, with a marked left-sided predominance (Steeno et al, 1976). Approximately 90% of varicoceles are left-sided. Because retrograde flow of blood in the internal spermatic vein is responsible for venous dilation and tortuosity, differences in the configuration of the right and left internal spermatic veins and their embryologic origins are thought to contribute to this marked left-sided predominance. The left spermatic vein enters the left renal vein at a right angle, rather than entering obliquely into the vena cava as the right internal spermatic vein does. The insertion of the left renal vein into the vena cava is 8 to 10 cm more craniad than the insertion of the right internal spermatic vein. As a result, the left internal spermatic vein has an 8- to 10-cm greater head of pressure, and its effluent faces a relatively slower flow of blood. Treatment Alternatives When varicocele ablation is determined to be appropriate, several therapeutic options must be considered. Because most of the available techniques for varicocele ablation have proved to have very nearly the same efficacy, it is imperative that the relative advantages and disadvantages of each technique be reviewed with particular attention to the unique circumstances posed by adolescents. Currently, it appears that multiple different techniques are applied clinically, with the choice of technique guided by the experience of the surgeon and taking into account the age, body habitus, and peculiarities of the patient and varicocele in question. Inguinal ligation (opening of the external oblique aponeurosis) is performed through a small incision over the inguinal canal that follows the skin lines. The inguinal canal is opened through the external inguinal ring along the direction of the fascial fibers to gain access to the cord just below the internal ring. The cord is isolated over a Penrose drain, excluding the ilioinguinal nerve, and is delivered into the wound. With optical magnification and the help of Doppler ultrasound, the testicular artery should be located and preserved. The veins of the cord, except those associated with the vas, are doubly ligated with 4-0 silk and divided. Attention should be paid to lymphatic vessels, which should be preserved when possible. The inguinal approach is best avoided when a prior inguinal surgical procedure has been performed. The subinguinal approach involves a transverse skin fold incision below the inguinal ring at about the level of the pubic tubercle, with isolation and delivery of the testis as in the inguinal approach. The inguinal canal is not opened. At this level, a larger number of veins will be encountered and the testicular artery may be more difficult to identify. Dissection of the cord should follow the technique described for dissection within the inguinal canal. When either the inguinal or the subinguinal approach is used, a cord block or caudal block may provide adequate postoperative analgesia (Ogura et al, 1994).