NS330 Quiz 3 - WordPress.com
advertisement

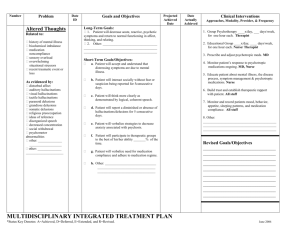
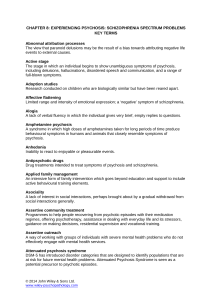
DEPRESSION Minor Depression: sustained depressed mood w/o full depressive syndrome; pessimistic attitude & self-pity required for dx; may be chronic & complicated by superimposed major depressive episode Major Depressive Disorder (MDD): experience substantial pain & suffering; psychological, social & occupational disability; significant change in functioning Subtypes: specifiers w/ MDD -psychotic features- break w/ reality (hallucinations, delusions) -catatonic features- peculiar voluntary mvmt, echopraxia or echolalia, negativism -melancholic features- anorexia, wt loss, diurnal variations w/ symptoms worse in am, early am awakening -postpartum onset (w/in 4 wks postpartum)- severe anxiety, possible psychotic features -seasonal features- generally occurring in fall or winter & remitting in spring; tx w/ light therapy -atypical features- appetite changes, wt gain, hypersomnia, extreme sensitivity to perceived interpersonal rejections Dysthymic Disorder (DD): early & insidious onset, chronic depressive syndrome usually present most of day, more days than not, for at least 2 yrs, often cannot be distinguished from person’s usual pattern of functioning Biological Theories: -genetic factors- inc’d heritability is assoc’d w/ earlier age of onset, greater rate of comorbidity & inc’d risk of recurrent illness -biochemical factors-serotonin (dysfunction result in poor impulse control, low sex drive, dec’d appetite, irritability); -norepinephrine (dec’d anergia, anhedonia, dec’d concentration, diminished libido) -dopamine, acetylcholine, GABA also believed involved -alterations in hormonal regulation -sleep abnormalities Cognitive theory: Beck proposed people acquire psychological predisposition to depression through early life experiences -Beck’s cognitive triad-negative, self-deprecating view of self -pessimistic view of world -belief that negative reinforcement will continue in future Learned Helplessness: Seligman- although anxiety is initial response to stress, it is replaced by depression if person feels that self has no control over outcome of situation Symptoms: depressed mood, anhedonia, anergia, anxiety; may experience delusions of being punished or being a terrible person; psychomotor agitation or retardation; vegetative signs (change in bm & eating habits; sleep disturbances; disinterest in sex); pain; hopelessness (negative expectations for future, loss of control over future outcomes, passive acceptance of futility of planning to achieve goals, emotional negativism) & despair; suicidal ideation; feelings of anxiety, worthlessness, guilt, helplessness, hopelessness, anger & irritability, guilt BIPOLAR marked by shifts in person’s mood, energy & ability to fxn; episodes of mania, hypomania, depression, concurrent mania & depression Bipolar I- classic; at least 1 episode of mania alternating w/ major dep Bipolar II- hypomanic episode(s) alternating w/ major dep Cyclothymia: hypmanic episodes alternating w/ minor dep (at least 2 yrs duration) Rapid cyclers- >4 episodes in 12 mos Mania- elevated irritable or expansive mood; talkative, excitable, energetic, rapid changing conversation, inflated self esteem Mania characteristics: -mood- euphoric; may change to irritation & quick anger; irritability, belligerence; cheerful @ inappropriate times; boundless energy & self confidence -behavior- sexual indiscretion; constantly push limits; voracious appetites; too busy to sleep -thought process- flight of ideas; speech is rapid, verbose & circumstantial, loud; grandiosity -cognitive fxn- impaired Mixed episodes: Dysphoric mania-sense of unhappiness, fearfulness, depression, accomp’d by high energy levels, racing thouths, pressured speech Exalted depression- dep’d w/ symptoms but still have delusions of grandeur Things that mimic mania: steroids, levadopa, catapril, meth, cocaine, syphilis, HIV, lyme disease, hyperthyroid, tumors, brain injuries SCHIZOPHRENIA Affects thinking, language, emotions, social behavior, ability to perceive reality accurately Onset- typically late teens/early twenties Subtypes: Paranoid type- hallucinations, delusions, Disorganized type- disorganized speech & behavior, inappropriate affect Catatonic type- motor immobility (waxy flexibility or stupor) Undifferentiated type- active-phase symptoms, no one presentation dominates Residual type- no longer has active-phase symptoms, some persistent symptoms noted Schizoaffective disorder- uninterrupted period of illness w/ major depressive, manic or mixed episode, concurrent w/ symptoms that meet criteria for schizo. Other psychotic disorders: Delusional disorder- nonbizarre delusions, ability to fxn not markedly impaired nor is behavior obviously odd or bizarre Schizophreniform disorder- essential features of schizo except total duration is >1mo but <6mos Brief Psychotic disorder-sudden onset of symptoms or disorganized or catatonic behavior; lasts >1day but <1mo Shared Psychotic disorder (folie a deux)- individual close to another who has disorder w/ delusion comes to share the delusional beliefs in total or in part Induced or Secondary Psychosis- caused my substances or general medical condition Theories: Neurobiological-inc’d dopamine; serotonin; glutamate Genetic- inc’d rate w/ h/o relatives Neuroanatomical- enlarged lateral cerebral ventricles, third ventricle dilation &/or ventricular asymmetry; cortical atrophy; cerebellar atrophy; atrophy of frontal lobe; inc’d size of fissures; reduced grey matter esp temporal & frontal lobes Nongenetic- prenatal risk from viral infection, poor nutrition or starvation, exposure to toxins, lack of O2 during birth; stress Signs of schizo: the fours A’s -affect- flat, blunted, inappropriate, bizarre -associative looseness- haphazard & confused thinking manifested by jumbled & illogical speech & reasoning -autism- thinking not bound to reality, reflects private perceptual world of individual; delusions, hallucinations, neologisms -ambivalence- simultaneously holding two opposing emotions, attitudes, ideas or wishes toward person/situation or object Course of disease: Acute: periods of florid positive symptoms (hallucinations, delusions) & negative symptoms (apathy, withdrawal, lack of motivation) Maintenance: acute symptoms decrease in severity Stabilization: symptoms in remission, there may be milder persistent symptoms Prepsychotic early symptoms- may appear a month to year before first psychotic break -acute or chronic anxiety, phobia, obsessions compulsions -feelings of rejections, lack of self-respect, loneliness, hopelessness -withdrawal increase feelings of isolation & inability to trust -preoccupied w/ religion, matters of mysticism, metaphysical causes of creation, speech characterized by obscure symbolism -sexual activity altered; preoccupation w/ homosexual themes (most prominent in paranoid schizo); exaggerated needs, altered performance; fears of intimacy Positive symptoms: hallucinations, illusions, delusions, bizarre behavior, paranoia, positive formal thought disorder & speech patterns Alterations in thinking: Delusions- false fixed beliefs that cannot be corrected by reasoning (ideas of reference, persecution, grandiosity, somatic sensations, jealousy, control) -thought broadcasting-others can hear your thoughts -thought insertion- you hear others thoughts -thought withdrawal- thoughts have been removed from mind -delusion of being controlled- body/mind controlled by outside agency Concrete thinking-overemphasis on specific details & impairment of ability to use abstract concepts Alterations in Speech: Associative looseness- thinking is haphazard, illogical, confused Neologisms- made up words Echolalia- pathological repeating of another’s word Echopraxia- mimicking movements of another Clang association- meaningless rhyming of words Word salad- jumble of words that is meaningless Alterations in Perception: Hallucinations- sensory perceptions for which no external stimulus exists -auditory- hearing voices or sounds -visual- seeing persons or things -olfactory- smelling odors -gustatory- experiencing tastes -tactile- feeling bodily sensations Command hallucinations- voices command person to do something Personal boundary difficulties: Depersonalization- nonspecific feeling that person has lost identity, self is different or unreal Derealization- false perception by person that environment has changed Alterations in Behavior: Extreme motor agitation- excited physical behavior Stereotyped behaviors- motor patterns that originally had meaning but are now mechanical & lack purpose (sweeping floor, washing windows) Automatic obedience- performance by catatonic client of all simple commands in robotlike fashion Waxy flexibility- seen in catatonia, excessive maintenance of posture Stupor- catatonic client is motionless for long periods & may appear to be in coma Negativism- equivalent to resistance, client does opposite of what told to do Negative symptoms: affect flat, inappropriate or bizarre; alogia; avolition, apathy; anhedonia, asociality; attention deficits, anergia cognitive symptoms- difficulty w/ attention, memory or executive fxns; disorganized thinking depressive & other mood symptoms Stages of Relapse Stage I: overextension Stage II: restricted consciousness Stage III: disinhibition Stage IV: psychotic disorganization Stage V: psychotic resolution INTERVENTIONS FOR ALL DISORDERS: Phase I: Acute- (6-12 wks)- client safety & medical stabilization (well hydrated, maintain stable cardiac status, maintain tissue integrity, sufficient sleep, thought self-control, no attempt at self harm); hospitalization if client is danger to self or others, refusing to eat or drink, too disorganized to provide self care; reduction of symptoms & restoration of psychosocial & work fxn, Phase II: Maintenance- helping client adhere to med regimens, understand disease, health teaching, psychoeducational classes (disease process, medication, consequences of substance addictions, early s/s), support groups or therapy, communication & problem solving; relapse prevention skills Phase III: Stabilization- target neg symptoms: ability to participate in social, vocation, self care skills training, involvement in socializing groups; prevention of relapse & limit severity & duration of future episodes: learning interpersonal strategies, participate in therapy (CBT, family, psychotherapy), support groups -maintain regular sleep pattern; reduce alcohol, drug & caffeine intake; keep in touch w/ supportive friends/family; stay active; have routine daily & weekly schedule; take meds regularly Basic level interventions: milieu management (protection from suicidal acts, supervised environment for regulating meds, ECT), counseling, promotion of self care activities, psychobiological interventions, health teaching, health promotion & maintenance, case management Acute: acute psychoparm tx; supportive & directive communications; limit setting; psych, med & neur eval Milieu Therapy: Seclusion for Bipolar- provides comfort & relief- reduces overwhelming stimuli; protects client from injuring self, others or staff; prevent destruction of property -warranted when- substantial risk of harm to others or self; u/a to control actions; problematic behavior is sustained; other measures have failed Advanced practice interventions: Med maintenance most important in preventing relapse Individual therapy: social skills training, cognitive remediation, cog adaptation training, CBT, Group therapy Family therapy