The Heart
advertisement

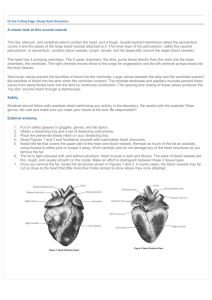
The Heart Location: thoracic cavity, between lungs, size of clenched fist, 2/3rds on left side of sternum Pericardium: double layered serous membrane Outer layer: parietal pericardium, pericardial sac Inner layer: visceral pericardium or epicardium Pericardial cavity: fluid filled space between the pericardial layers Heart Chambers Atria: receiving chambers for blood Right atria: incoming blood from superior vena cava Drains blood from superior portions of body And inferior vena cava/ blood from regions below the heart Coronary sinus: drains blood from heart wall UNOXYGENATED Ventricles: provide the force to push blood out of the heart Myocardium much thicker in ventricles than atria Forcefull contractions Right ventricle : pulmonary trunk then to lungs Left ventricle : into aorta which branches Oxygenated blood to body Valves of heart: permit blood to move in one direction Atrioventicular valves: 2 to 3 flaps(cusps), point down, located between atria and ventricles Tricuspid valve: between right atria and ventricle Bicuspid valve: between left atria and ventricle(mitral valve) Heart murmur: if valves aren’t anchored properly to muscular wall of ventricle(chordae tendinae) Blood re -enters atrium when ventricle contracts Semilunar valves: located between ventricles and vessels carrying blood away from heart(shaped like 3 half moon bowls, convex side facing ventricle) Pulmonary valve: right ventricle to pulmonary trunk Aortic valve: from left ventricle to aorta Blood flow through heart: Unoxygenated blood from superior and inferior vena cavae, coronary sinus to RIGHT ATRIUM - tricuspid valve – RIGHT VENTRICLE – pulmonary valve – to Pulmonary Trunk – pulmonary arteries -LUNGS – OXYGEN Pulmonary veins(4) – LEFT ATRIUM –mitral valve – LEFT VENTRICLE – aortic valve –AORTA to all body(except lungs) Anatomy of Heart Tissue Location: thoracic cavity, between lungs, size of clenched fist, 2/3rds on left side of sternum Pericardium: double layered serous membrane Outer layer: parietal pericardium, pericardial sac Inner layer: visceral pericardium or epicardium Pericardial cavity: fluid filled space between the pericardial layers Pericardial cavity: between epicardium and serous layer Filled with serous fluid Pericarditis: pericardium becomes infected Fluid production stops Increase friction Decrease heart function Heart Wall: Epicardium: serous membrane Fat deposits along channels of BV which Provide oxygen to heart wall Myocardium: bulk of heart wall Cardiac muscle cells : striated b/c of Intercalated discs Points of attachment between cardiac Muscle cells – facilitates conduction, so that all cells function together Contracts to propel blood Bundles of cells interwoven with CT CT= “fibrous skeleton Endocardium(endothelium) Smooth white membrane Lines heart chambers and is continuous into BV and heart valves Heart Chambers Heart Chambers: 2 thin walled atria = receiving chambers 2 thick walled ventricles = pumping chambers Left wall is thicker than R wall(WHY?) Atria: very little myocardium External structure = auricle(little ears) Help to increase volume of atria Underlying endocardium = pectinate muscles Resemble teeth of comb Interatrial septum: separates both atria Posterior wall = fossa ovalis = remnant Of foramen ovale= hole in septum To allow fetal blood to bypass lungs Right Atrium: incoming blood(unoxygenated) 3 sources: superior vena cava Inferior vena cava Coronary sinus Left Atrium: collects blood from 4 pulmonary veins From lungs(oxygenated) Ventricles: inner walls – trabeculae carnae (ridges of muscles) and Papillary muscles(individual cones) which assist valves – “tug on heart strings” once these muscles contract they “tug” on chordae tendonae which open the valves Interventricular septum: separates ventricles Interventricular sulcus: exterior groove Coronary sulcus: exterior groove separates Atria from ventricles Both grooves lines with fat and BV Pectinate muscles: Atria:: Trabeculae carnae: ventricle Right atria Receives blood From body Left Atria receives blood from lungs(PV) Right Ventricle Sends blood To lungs Pulmonary trunk to LPA and RPA Left Ventricle sends blood to body Aorta Blood Pressure: The force exerted by blood against the interior walls of the BV Highest in arteries and arterioles Negligible in veins, venules, and capillaries Skeletal muscle, valves, and respiratory Activity moves blood back to heart Arterial Blood Pressure: Arterial Blood Pressure: Pressure gradient: move from high P to low P Systolic Pressure: (120mg) (contraction) From heart to Aorta Elastic walls of aorta Diastolic Pressure: (relaxation) (70-80mg) Beyond the junction of heart and aorta Sphygmomanometer: measures bp Brachial artery compressed Release valve on cuff allows blood to flow through brachial artery Stethoscope picks up tapping sound as blood moves back through Brachial artery (systolic pressure) Once the tapping becomes inaudible (diastolic Pressure) Regulation of BP Factors that control BP: nervous system, endocrine system, kidney function Nervous system: Medulla oblongata – vasomotor center Supplies the nerves that innervate smooth muscle of arterioles to control vasoconstriction or dilation Receives info from baroreceptors in aorta and carotid arteries – also chemoreceptors send info on oxygen content and pH levels Endocrine system: epinephrine and norepinephrine Secreted during stress From adrenal medulla(above kidneys) Epinephrine – increases cardiac output Norepinephrine – increases peripheral resistance Antidiuretic hormone: hypothalamus Stimulates kidneys to conserve water(increase Blood Volume, ie, blood pressure) Atrial natriuretic factor: secreted by atria Reduces Blood volume Stimulates kidneys to excrete Na+ and water Kidney Control: Arterial blood pressure drops – kidney cells secrete RENIN- Renin triggers AGIOTENSIN II a vasoconstrictor Triggers ALDOSTERONE produced by adrenal gland(above kidney) causes Na+ to be reabsorbed by blood – results in water also moving into BV, increases Blood Pressure Factors that INFLUENCE BP: (1) Cardiac output: heart rate and stroke volume (2) Blood Volume: Plasma volume and hematocrit (3) Peripheral resistance: BV diameter and viscosity 1,2,3 determine blood pressure which influences Blood Flow Work together to ensure proper blood volume