Hey everyone - The Sophie Davis Survival Guides
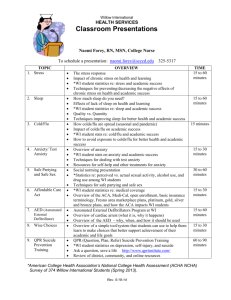
advertisement

HOW TO SURVIVE th 5 Year Image taken from: http://www.punyajokes.com/cartoons/stress.gif FALL 2007 A SDSG PUBLICATION “How to Survive” Guide – 5th Year 1 TABLE OF CONTENTS Hello everyone! This is the first study guide for 5th year classes, and as such, we do not have enough advice to make individual guides for each class. In this guide, you will find advice for each class you have to take, including neuropsychiatry, systemic pathology, epidemiology, and pathophysiology. And, last but certainly not least, the much dreaded, much feared USMLE Step 1. Good luck. Topic Pages Neuropsychiatry – Advice 2 Neuropsychiatry – Exam 1 Information (from Akeem Marsh) 3-11 Neuropsychiatry – Exam 2 Information (from Akeem Marsh) 12-20 Systemic Pathology 21-22 Epidemiology 23 Pathophysiology 24 Physical Diagnosis 25 Comprehensive Basic Science Exam 26 The Final Step of Sophie: USMLE Step 1 27-31 How to Survive: 5th Year Galina Borodulina (Class of 2007) Barry Ladizinski (Class of 2007) Akeem Marsh (Class of 2007) Shayla Syed (Class of 2007) “How to Survive” Guide – 5th Year NEUROPSYCHIATRY- ADVICE AND INFORMATION Advice from Akeem Marsh The name Neuro-Psychiatry, doesn’t that sound very sophisticated and medical professional-ish. Well that it certainly is, but not one course, much like it’s predecessor Behavioral Medicine, that you will not have to lose sleep over. In many ways, this is just an extension of Behavioral Medicine so advice is really not necessary. I can say nothing at all and half of you, maybe more will still get A’s haha. Having said that, I will still provide some information that those of you that like this sort of thing may find helpful. What you learn in this class mostly is about psychiatric illnesses (dementia, psychosis, schizophrenia, attention deficit disorder, …) and how to treat all these diseases. I think this class, unlike Behavioral Medicine, was completely lecture notes oriented. Your written exams will be in the same format as they were in behavioral medicine, about 30-50 multiple choice questions and you will find them to be very easy. I have some notes compiled together and they are derived from all of the lecture notes. You may find these helpful because it condenses everything together sort of succinctly and I added in some mnemonics as well. The best books to use for this course are in my opinion Behavioral Science BRS and PreTest in Psychiatry (yes, Step 2 psychiatry). I think that is the MOST relevant for both your coursework and your miniboard. The Behavioral Science PreTest is a shameful book in the pretest series and those of you that decide to invest in it, and I know some will unfortunately, will probably regret that purchase as it is completely irrelevant. PreTest in Psychiatry is good for both coursework and for the miniboard. I have heard of two different versions of the miniboard, either one heavily centered on ethics questions and one with a lot of drug questions. In any case, if you even study for your Neuro-Psychiatry course at all, you should be well prepared for your miniboard. The ethics questions will be like Patient Doctor all over again asking questions about how one should interact with patients (common sense) or the drug filled exam, which you should be ready for anyway because that is mostly what NeuroPsychiatry is about. Enjoy this “vacation” while it lasts because when you get hit with the real stuff, i.e. pathology, you will have to work a bit harder than you did for this course. If you care to use them, the notes that I made are attached to this file in the following pages. Happy Studies! Advice from Shahla Syed The hardest part of neuropsych is learning the drugs - if you can do that, you will be just fine, and I would recommend going back to Katzung again for this. Of course you have to learn the psychopathology as well, but I found that less difficult than learning drugs (I've always had trouble with pharm). 2 “How to Survive” Guide – 5th Year NEUROPSYCHIATRY- EXAM 1 MATERIAL Marijuana increases weight (associated munchies). Leptin signaling blocked by suppressors of cytokines. Leptin signaling stops in severely obese pts. Signaling center is located in the arcuate nucleus of the hypothalamus. leptin = weight by stimulation of appetite. Leptin is produced by the ob gene. Orixegenic - appetite. Anorixegenic - appetite. Anorexia xtreme weight loss, refusal to eat despite normal appetite. Bulimia however involves binge eating, tooth enamel erosion. Trx anorexia: TCA’s (imipramine), 5HT – fluoxetine, phenfluoramine, heterocyclics: isocarboxazid, phenelzine, and trazodone. Long term Trx for obesity: ObeSity – Orlistet and Sibutramine Short term Trx for obesity: a short obese girl named Zoe Torp. Zonisimine and Torpiramate SSRI - weight for 6 mos. Antidepressants - glucose levels Phase 3 of clinical trial antidepressant. Endocannibinoid receptor block (Radafaxine is Rad b/c it stops ur high.) Selective 5-HT2c Agonist – Rimonabant and phenfluoramine CeFiLIstat blocks absorption of Fat by inh. LIpase. Mutation in mahogany mg gene is what es weight. Having a fxning mg gene doesn’t work well at weight control. Mg gene related to agouti pigment gene, and nearly identical to attractin produced by activated T cells that stimulates attraction between cells. ADHD – Impulsivity, fidgeting, distracted ez, difficulty following directions. at least 6 mos. Occurs b4 age 7. impaired behavior in at least 2 settings. 3 types: combined, inattentive, hyperactive-impulsive. All more common in boys. Girls get inattentive type. Pts r at risk for drug abuse, accident, and dropout. Caused by possible reticular activating system (frontal lobe) or in NE. Strong genetic component; multigene disorder (D4 receptor, DA transporter, synaptosomal-associated protein 25). Stimulants calm children with ADHD. There are different affects between children and adults with ADHD b/c there is more DA released in adults for their lack of autoreceptor activity. Trx Dextroamphetamine and Methylphenidate (both indirect acting sympathomimetics), Pemoline (liver fxn tests shud be done b/c jaundice) and Modafinil (1B agonist). [Dexter Must Make Peace.] Drugs can also trx narcolepsy, weight loss, and rarely supplement PD. Side effects include GI symptoms, headache, muscle twitch, and hallucinations. Cocaine affects DA release and reuptake. Conduct Disorder – Aggressive behavior and infringement upon the rights of others > 12 mos. Usually comorbid with ADHD, ODD, learning disability. More common in boys. Same risks as ADHD. Multifactorial etiology. Trx multimodality, psychotherapy, and drugs: antipsychotics, SSRIs, and ithium 3 “How to Survive” Guide – 5th Year Affects on DA release: amphetamine > Ritalin > caffeine ODD – Disobedient, hostile, defiant behavior to authority > 6 mos. More common boys, may lead to development conduct disorder. Multifactorial or unknown etiology. Trx no drugs, just psychotherapy and behavioral management skills. Psychoanalysis Psychoanalytic Psychotherapy Supportive Psychotherapy Cognitive Behavioral Therapy Depression: Monoamine depletion by unknown disease process, stress, drugs. MAO inh. (isocarboxazid, phenelzine, tranylcypramine) Relieve depression by monoamine. TCA’s inh monoamine transport. Same affects as MaoI. 3 main neurotransmitters are DA, 5-HT, NE. Prozac 5-HT. MAO destroys NE, NE reuptake pump terminates axn of NE, NE receptors react 2 NE release. 4 groups of treatment: 1) TCA’s 2) Heterocyclics 3) SSRI (prozac) 4) MAO: side effects tyramine (cheese, wine, pickled pigs feet, aged meats, beer) and hypertensive crisis, serotonin syndrome (muscle rigidity, CV collapse, hyperthermia) Biological basis of Schizophrenia is unknown. Mesolimbic DA pathway: ventral tegmentumnucleus accumbens. Associated with this pathway pleasure, reward, reinforcing behavior, drugs of abuse, and chocolates. Hyperactivity ( DA) here gives +ve psychotic symptoms (emotional behaviors, auditory hallucinations, delusion, thought disorder) and plays a role in aggressive/hostile behavior in schizo. *all known antipsychotic drugs are capable of treating +ve psychotic symptoms are blockers of DA receptors (D2).* Mesocortical DA pathway: ventral tegmentum limbic cortex . –ve schizo symptoms (5 A’s: attention deficit hyperactivity, affective flattening, alogia, avolition, anhedonia) could be localized to dorsolateral prefrontal cortex. –ve symptoms due to burnout of neuronal symptoms excitotoxic overactivity of glutamate systems. DA deficit (-ve symptoms schizo) can be 1 or 2 (inh by excess 5-HT OR antipsychotic blockage of D2 receptors). Nigrostriatal DA pathway: sub nigra basal ganglia (striatum). EPS and motor control. Deficiencies Parkinson’s (Rigidity, Akinesia/bradykinesia, Tremor) and Akathisia (restlessness), dystonia (twisting movements). Blocking D2 receptors mock deficiencies. Chronic blockade causes Neuroleptic-induced tardive dyskinesia. Hyperactivity of DA – chorea, dyskinesias, and tics. Tuberinfundibular DA pathway: Hypoth Ant Pit. Active inh prolactin release. Postpartum, activity is ed. ed prolactin causes galactorrhea, amenorrhea, sexual dysfxn. ed prolactin occurs after chronic blockage of D2. 4 “How to Survive” Guide – 5th Year Schizo onset late teens/early 20s. Symptoms; odd behavior, es facial expression, moderate depression, elevated HVA in body fluids. Incidence s in pts w/ fetal obstetrical complications. Anatomic features include wide sulci, ventricle size, frontal and medial temporal lobes (gliosis) and hippocampus (disordered orientation of pyramids). Causes: 1) toxic or genetic result 2) poor neuronal migration (occurs in epilepsy as well) 3) inadequate synaptic selection (mutations in synapsin 1:2, possibly D2) 4) poorly innervated *synapsin sux in schizo. D2 antagonists worsen symptoms (Give GABA to epileptics, but NOT glutamate. GlutamateGABA (Glut. Decarboxylase) GABA Glutamate (GABA Transaminase) Glutamate is excitotoxic by inducing apoptosis/cell death. HaloPEridol – Has Potency and EPS. SDA (serotonin DA antagonist) – block both 5-HT2A and D2. Clozapine blocks histamine and cholinergic as well. Less EPS than typical used as Trx for Tardive Dyskinesia and has agranulocytosis as a side effect. Anxious pts trx w/ antidepressant. Venlafaxine drug of choice. Mood in depression and anxiety of GAD. Venturous for trxing 2 disoders. Clomipramine (TCA) and Fluvoxamine (SSRI)– trx OCD High comorbidity of depression and anxiety. SSRIs (fluoxetine, paroxetine, sertraline, fluvoxamine) are used for pts with depression, anxiety disorder subtypes, panic disorders and social phobia. Buspirone – 5-HT1A partial agonist is a generalized anxiolytic. Other 5-HT1A agonists are flesinoxan, sunepitron, adatanserin, ipspapirone. Advantages vs BZDs include no interaction with EtOH, BZDs, sedative hypnotic agents, absence of drug dependance with long term use, ease of use in therapeutic onset for antidepressants. Used preferentially in chronic/persistant anxiety comorbid with substance abuse, and elderly pts. -Buspirone best for 4A’s: Anxiety (chronic/persistent), Abuse (comorbid substance), Aged (elderly), and Autoreceptor Agonist. Mechanisms of action of drugs 5-HT1A agonist Antidepressants BZD anxiolytics Adaptive neuronal and Adaptations in Occupy BZD receptors receptor events neurotransmitter receptors ALL 5-HT1A agonists have presynaptic axns for anxiety and postsynaptic axns for nausea/dizziness. GAD + MDD = MAD. Subsyndromal anxiety + subsyndromal depression = subsyndromal mixed anxiety depression (anxious dysthymia). MDD + subsyndromal anxious depression. GAD + dysthymia = GAD w/ depressive symptoms Enkephalins – are mood altering Orthoquinone (free radical) produced from DA. Neurodegenerative from L-Dopa. Brain derived neurotrophic factor: - sensory neurons: nodose, dorsal root ganglion - spinal motor neurons, basal forebrain cholinergic neurons, substantia nigra DA neurons, facial motor neurons, retinal ganglion cells 5 “How to Survive” Guide – 5th Year Nomifensine and Bupropion help depressed by blocking reuptake pump. Pargyline is a Mao inh. Pramipexole is a D2 agonist. Idocoxane, Clonidine, Reserpine, Yohimbine ALL have 2A autoreceptor axn. ICaRYs is an automatic flight machine. Serotonin can be found in intestine and pineal gland. Gastric carcinoid syndrome contains excess 5-HT, and the test for this checks levels of 5-HIAA. Fenfluramine enhances 5-HT release. CisApride s Appetite in Children. Drugs involved in cholinergic transmission: -hydroxybutyrate – Gaba B receptor inh NE release Vesamichol – inh Ach storage Physostigmine, donepezil, galantamine AchE inh Troxypyrrolium/hemicholinium inh uptake of choline by presynaptic membrane Bungarotoxins + botulinum inh Ach release at presynaptic terminal Curare/Rabies nAChR Vigabatrin inhibits GABA Transaminase and is used to treat childhood epilepsy. Spastic paralysis is a GABA B disease, and Baclofen trxs. *Flumazonil is the only antagonist for BZD. *Flumazonil says F#ck BZD! Lennox Gestaut Syndrome – mixed seizure and MR. Tonic seizure activity in sleep. Trx Toperamide, Filbarmate, Lamotipine. West syndrome muscle contraction and MR. 1-2 sec duration, peaks faster. Trx Topiramide, vigabactrin, corticosteroids. Diazepam (Valium). Good Anxiolytic. IV for Status Epilepticus. Tetanus. - makes you take A STEp. Chlorazepate and Oxazepam are BZDs that live forever in your body and produce metabolites that live forever. Alprazolam (xanax)– anxiety and depression. Like venlafaxine Triazolam – pts will experience “rebound” insomnia after discontinued use after long trx. Zolpidem/Zolepion – work on BZ1 receptor. Trx sleepwalk - sedatives (anxiolytics) anxiety and exert a calming effect while hypnotics produce drowsiness and encourage “natural sleep”. Sedatives at high doses can have hypnotic effects. BZDs are MOST imp sedative hypnotics. Barbiturates are sedative hypnotics that cause undesirable psychologic and physiologic dependance. Other sedative hypnotics include: piperidinediones, propanediol carbamates, alcohols (EtOH, chloral hydrate, paraldehyde), buspirone, zolpidem. Sedative effects can be obtained w/ blockers, clonidine, antipsychotic tranquilizers, TCAs, and anti-histamines. *Redistribution of drug from CNS 2 other tissues is an imp feature of the biodisposition of sedative-hypnotics. Thiobarbiturates are RAPID. Sedative hypnotics are detectable in breast milk. (can depress CNS in nursing infants) 6 “How to Survive” Guide – 5th Year Anxiety is an expected, normal, and transient response to stress. Pathological anxiety requires 4 criteria: 1) autonomy (no recognizable triggers) 2) intensity (> pts capacity to bear discomfort) 3) duration (persistent symptoms) 4) behavior (impairs coping) Anxiety differs from fear which is a sense of dread and foreboding that occurs in response to an external threatening event. Symptoms include autonomic arousal, “going to die” or “lose control”, avoidance or compulsions, and worry/apprehension/obsessions. Etiology is central NE systems (locus coerulus) and GABA (limbic), modulated by serotonergic and neuropeptides. Is most prevalent psychiatric disorder. risk among pts with 1st degree relatives w/ anxiety. Physical, psychosocial, and quality of life affected. Organic causes of anxiety: thyroid, NE, drugs (cocaine, caffeine, EtOH, narcs, sedhypnotics). Panic disorder – recurrent unexpected panic attacks (episodes of intense anxiety peak w/in 10 mins) More common in women. Late teens – 30 y/o. Runs in family. Hard to diagnose b/c symptoms include cardiac, pulmonary, GI, neurological, autonomic arousal, psychological. Trx antidepressants (paroxetine, sertraline) and high potency BZDs (alprazolam/clonazepam). Agorophobia seen in some pts w/ panic disorders. Anxiety abt or avoidance of places or situations from which escape might be embarrassing. GAD – excessive anxiety/worry. Occurs more days than not > 6mos. More common in women. Child or adolescent. 3/6 (restlessness, ez fatigability, difficulty concentrating, irritability, muscle tension, insomnia). Trx cognitive behavioral therapy and antidepressants, BZDs, buspirone. Phobia – persistent, excessive unreasonable fear of situations or objects. 10% gen pop. Exposure to stimulus provokes anxiety. Trx BZDs to anxiety and cognitive behavior therapy. - social phobia (fear of public scrutiny). Trx SSRI, BZDs, blockers. OCD – recurrent, intrusive, unwanted thoughts or compulsive behaviors/rituals. Four criteria: 1) intrusive/inappropriate 2) not simple worries 3) attempts made to ignore/neutralize 4) obsession recognized as a product of his/her mind OCD is Trx w/ ClOmipramine b/c it has an O and C. Cognitive Therapy is good as well. PTSD ntense fear, helplessness, or horror b/c of an experience that was a threat of death, injury or severe harm. 1% prevalent in gen pop , and higher among those who experience trauma. Symptoms > 1 mon. subtypes include acute (<3mos), chronic (>3mos), delayed onset (onset >6 mos). Trx only sertraline, paroxetine and Exposure based log therapy. Antipsychotic drugs Parkinson’s patients need L-Dopa + a cholinergic antagonist. Typicals are all D2 antagonists. Phenothiazine derivatives: suppress hiccups 1) aliphatic – chlorpromazine [sleepy, less EPS than haloperidol b/c has antichol activity] 7 “How to Survive” Guide – 5th Year 2) piperadine – thioridazine 3) piperazine – trifluoperazine and thiethylpiperazine (motion sickness) Haloperidol is a butyrophenone and causes MOST EPS b/c it lacks antichol activity. Thiothixene is a thixanthene. Neuroleptics cause psychomotor and affective indifference. Sedation caused by phenothiazines. Sedation caused by phenothiazine derivatives involves minimal motor coordinations. Known as “tranquilizers” b/c calm, ↓ agitation/hyperactivity w/o ↓ wakefulness. Chemoreceptor trigger zone of reticular formation has D2 receptors blocked by neuroleptics. Neuroleptics ↓ nausea from other drugs, pregnancy, radiation, cancers but NOT nausea 2° to bowel obstruction or motion sickness. **Side effects occur in ALL neuroleptic pts Apomorphine and bromocriptine (AntiPD) have structure similar to DA. Chlorpromazine and Haloperidol (neuroleptics) have structural overlap. Chlorpromazine, thioridazine, Molindazine, Loxapine, Trifluoperazine, Thiothixene, Haloperidol, Fluspirilene. Of the previous drugs listed: From left to right, ↑ risk of orthostatic hypotension, and at the top have high dose/low potency. From right to left, you have ↑ risk of developing PD symptoms and low dose/high potency. Neuroleptic induced Parkinsonism (EPS): Rigidity, Akinesia, Tremor. Neuroleptic Dyskinesias and Dystonias (involuntary motions of hip, jaw, tongue). Acute dystonia needs diphenhydramine for trx. Neuroleptic induced Akathisia (tremendous restlessness despite rigid stiffness). Mechanism of above symptoms: Neuroleptic drug offsets the normal balance b/w cholinergic and DA inputs into the neurons of the striatum. Anticholinergic such as Procyclidine, Trihexylphenidyl, and Benztropine restore lost balance. Balance could also be restored with L-Dopa, but this would antagonize the neuroleptic and induce psychosis. *when the Rat Does Act, Pet The Belly.* After 1 to 2 mos of neuroleptic therapy, most pts will develop tolerance to side effects and won’t need the anticholinergic but 25% of pts will. Tardive Dyskinesia (“chewing gum motion”). Long term DA receptor blockade. Striatal nerve cells synthesize more DA receptors, thus making the cells supersensitive to small amts of DA. Trx w/ clozapine (D2/5-HT2A receptor agonist) Phenothiazine induced obstructive jaundice is due to a hypersensitivity. Dermatitis/Photosensitivity: pts sensitive to sunlight, exaggerated sunburn. UV light readily oxidizes chlorpromazine. Drug accumulates in melanin containing tissues (eye, skin, sub nig). Prolactinemia (breast swelling, galactorrhea) All atypical antipsychotics act on and cause weight gain and diabetes xcept Ziprasidone. Clozapine: Atypical antipsychotic. “closes” many receptors (antihist, antichol, antiα adren). Agranulocytosis seizures (high dose) side effect. SDA: low EPS, tardive dyskinesia, and –ve symptoms of schizo. D4 receptor axn! riSPeridOne: Schizo, Psychotic Old people. (age associated psychosis and dementia) SDA that elevates prolactin. Low doses atypical, high doses typical 8 “How to Survive” Guide – 5th Year OLAnzapine: GranOLA makes you fat and sleepy. Improves mood in phases of bipolar and schizo. Quetiapine: Crazy ass PD pts w/ schizo. Queso w/ cholesterol biosynthesis inhibited (animals not humans) Ziprasidone: Zerotonin 1D antagonist, 1A agonist. Inh reuptake of both 5-HT and NE. No significant weight gain. Aripiprazole: DA2 antagonist and partial agonist Mood disorder – disturbance in emotional state. Pt can feel dysthymia, depression, hypomania, mania. *no differences in ethnicity, education, marital status, income. I. Primarily Depressive Major depressive – 2 wks depressed mood or loss of interest Dystymic – Depression NOS – depressed mood, anhedonic, appetite, sleep *In major depression w/ psychotic features, the delusions and hallucinations R congruent. -5-10% MDD pts develop mania -up to 15% of MDD will die by suicide during the recovery phase, mood↓ while energy↑. Double depression is dysthymic disorder and precedes MDD. Dysthymic disorders depressed mood for at least 2 yrs. II Depressive disorders w/ mania Bipolar I. Dx simple are manic or hypomanic episode. Elevated, expansive, irratible. ↓ sleep, talkative, distractibility, rambling thrush, and period of 7 days. Mania. Hypomanic →manic → psychotic Mixed presentations- suicidal. 1° manic then followed by depression. Mean age of onset early 20s. 90% individuals w/ manic episode will have successive reps. Early onset – worse progrnosis *Bipolar is the MOST inheritable psychotic disorder. Bipolar II and hypomanic – unlike mania – delusions/hallucinations cannot be present. Inflated self esteem does not reach a delusional grandiose level. 4 days of symptoms Depression common psychiatric disorder. Pure depressive yndromes are the 2D’s: Depression (recurrent symptoms >2 wks). Dysthymia (>2 yrs). Depression associated w/ mania includes Bpolar disorder and cyclothymic disorder (cycle b/w depression and mania). Depression can be 1) reactive or 2° (most common; response to real stimuli of grief, illness…) 2) endogenous (genetic; can’t experience ordinary pleasure) 3) manic depressive disorder (bipolar) Best trx is psychological trx and meds. ECT is used for MDD pts that don’t resond to antidepressants. Symptoms of depression SIG Energy Capsules** 9 “How to Survive” Guide – 5th Year TCA’s: mixed inh NE and 5-HT reuptake pumps. “off switches” of amine transmission. -“I’m Am 3 circles” Imipramine (enuresis/anorexia) and Amitryptyline. Axns of antimusc, antihist, anti adreno only contribute to toxicity. Nortryptiline used for Nordic migraines. Migraines result as a deficiency of 5HT in blood vessels in brain (vasodilation). Heterocyclics: 2nd gen – insomnia side effect. “MTA in Boston” Maprotiline, Trazodone (5 HT autoreceptor block; ↑ 5HT release; priapism) Amoxapine (severe neurotroxicity w/ seizure) and Bupropion. 3rd gen – “Vanessa Nancy Mirtaz” Venlafaxine, Nefazodone, Mirtazapine. *azodone cousins 2nd letter/term of both mnemonics Short ½ life Trazodone/Venlafaxine b/c Travis and Vern are short. SSRI can’t be used to OD. Fluoxetine – anorexia. Minimal autonomic toxicity, demethylated active metabolite Norfluoxetine. MaoI – axn allows more amines to accumulate presynaptically and more to be released. Hydrazide “make you a Phene (fiend) for Is (ice)”. Phenelzine and Isocarboxazid. Nonhydrazide “make you a transsexual”. Tranylcypramine Inhibition persists after drugs are no longer detectable in plasma. Great for atypical depression. Consider tyramine side effects and mixture with SSRI can cause 5HT syndrome. Clinical indications of Antidepressants. “Are DOPE Stuff Baby Girl” ADHD, Depression, OCD, Pain/Panic disorder, Enuresis, Social phobia, Bulimia, GAD. Antidepressants are most successful in trx pts that r: 1) slow (psychomotor retardation) 2) sleepless (sleep disturbances) 3) sexless (↓ libido) 4) satiety less (weight loss/poor appetite) TCA’s and 2nd/3rd gen agents differ in degree of sedation and antimusc effects. Li and antidepressant can trx depression, Li by itself prevents relapses. Blood plasma drug level determination should be obtained in postabsorptive state. When evaluating the state of pts (abt 1/3) that don’t respond to antidepressants, consider the 5 D’s: Dx, drug, dose, duration of trx, different trx. Inhibition of P450 3A4 can occur at high [] of Nefazoodone and Fluvoxamine. Can lead to fatal arrhythmias. TCA OD can include; coma, resp depression, agitation, neuromuscular irritability, hyperpyrexia, bowel/bladder paralysis. MaoI OD can include agitation, delirium, neuromuscular excitability, obtunded consciousness, seizures, shock, hyperthermia. Li prevents mood swings in pts with bipolar affective disorder. Pts w/ cyclic attacks of mania have many symptoms of paranoid schizo. Gradiocity, Bellicosity, Paranoid thoughts, overactivity. “manics @ G.O.P.B.” 10 “How to Survive” Guide – 5th Year Li affects electrolytes and their transport (inh Na+/H+ exchange), same for neurotransmitters (inh NE/DA release), and 2nd messengers (PLC, IP3 pathway inh) Li carbonate preferred Trx for bipolar affective disorder and can also trx EtOHism, aggression, some childhood episodic changes of mood aggression, and also can produce nausea/tremor. It is easily measured in body fluids, NOT metabolized, and interacts with diuretics, new NSAIDs, all neuroleptics xcept clozapine. Side effects are on ion dep. Systems like kidney, heart, thyroid. Can lead to diabetes insipidus (polydisia, polyuria) Therapeutic OD common. Li toxicity in newborns is manifested by lethargy, cyanosis, poor suck and moro reflexes, and hepatomegaly. -can be substituted by carbamazipine or valproic acid (used 4 epileptics). Amoxapine, fluoxetine, and venlafaxine can all act on DA, NE, and 5HT reuptake pumps. Uric acid is found in brain tumors. Ascorbic acid found in human uterine cervical cancers. Carbamezipine block Na+/K+ channels used 4 trigeminal neuralgia. Thinking (have ideas n make new ones) vs language (encode ideas into symbols) Disorders of Thought process or form: loose associations, word salad, racing thoughts, flight of ideas, circumstantiality, tangentiality, neologisms, clang associations, thought blocking. Disorders of thought content: delusions, ideas of reference, poverty of content, overvalued ideas, obsessions, phobias, suicidal ideas, homicidal ideas. Psychosis – break w/ reality Table 11-4 from BRS Schizo subtypes: disorganized (disheveled appearance, inappropriate emotions), catatonic (bizarre posture, lack of coherent speech), paranoid (delusion of persecution), undifferentiated (symptoms of more than 1 type), residual (1 previous schizo episode) ***** make sure that you know your axes as there were questions on both exams about them!!!!! Axis 1 Axis 2 Axis 3 Axis 4 Axis 5 11 “How to Survive” Guide – 5th Year NEUROPSYCHIATRY - EXAM 2 MATERIAL Trx of Dementia Cholinesterase Inhibitors: Improvement of cognitive function, global clinical state, ADL and behavior. Mechanism: ACh concentration, Dual action meds (tacrine and rivastigmine) may contribute to rapid rise of ACh (more side effects & greater effectiveness) Side effects: gastric acid secretion (dose dependent), Heart Block. Central activity (nausea, vomiting, weight loss and sleep disturbance). May exacerbate asthma/pulmonary conditions. OD mimics organophosphate poisoning. Donepezil - Reversible AchE, nicotinic receptor density–associated with enhanced synaptic strengthening through long term potentiation Galantamine - Reversibly and competitively inhibits AchE, Nicotinic cholinergic modulator– affecting NE, 5HT, GABA and Glutamate. Neuroprotective by inducing antiapoptotic proteins and calcium signals. Nicotinic receptor density–long-term potentiation. Found naturally in daffodil bulbs. Rivastigmine - AChE and Butyrlycholinesterase(BuChE) Inhibitor (equal affinity) Psuedoirriversibly inhibits AchE Possibly more effective in late stage AZ– more potent with GI AchE. More region specific (greater GI) than other AchEs. Severe vomiting/esophageal tear if not titrated slowly. Only AChEI to demonstrate efficacy in Parkinson’s Disease Dementia Tacrine: AChE and BuChE inhibitor– reversible. Also myalgia, rash, and liver toxicity -clinically indicated for Alzheimer’s Disease– mild to severe (as per cognition and behavioral impairment), Vascular Dementia, Mild Cognitive Impairment, Traumatic Brain Injury, DLB, Down’s Syndrome, ADD, etc. Memantine: NMDA receptor antagonist (noncompetitive) 5HT3 receptor antagonism (hence absence of GI complaints) For Moderate to Severe Dementia (AZ) Also for MCI, vascular dementia, HIV/AIDS, etc May be used with AChE Interferes w/ glut activity in AZ. Dizziness, headache, constipation, seizure, and thought disorganization/psychosis. Unproven therapies: NSAIDs, estrogen replacement, vitamin E, b-amyloid vaccinations Delirium (Toxic-metabolic encephalopathy): Disturbance in consciousness. Reduced ability to focus, sustain, shift attention, impaired cognition and memory impairment. Hallucinations and absence of insight and judgment. Affects terminally ill pts > post surgical pts > hospitalized pts. Risk factors: age, hx of cns/AIDS/drugs, dementia Most patients recover and delirium lengthens hospital stay, increases risk for complication. Caused by generalized dysregulation of neurotransmission; GABAGlutamate dynamic. NMDA receptor up regulation seen in Alcohol Dependence associated with withdrawal syndrome. elevated levels of Acetylcholine Trx: Address the underlying medical condition atypical antipsychotics at low dose. Avoidance of both Benzodiazepines and Anticholinergics recommended 12 “How to Survive” Guide – 5th Year Cognitive Disorders: Dementia – disorder of thought; slow insidious onset w/o attributable cause. irreversible - memory impairment, aphasia, apraxia, agnosia, or disturbance of executive fxn Delirium – disorder of sensorium; sudden onset w/ attributable cause. Transient Diagnosis of Cognitive disorder involves clinical features, history, and MMSE. Normal aging: memory impairment, decreased attention span, slowed learning, Retained: vocabulary, language ability, and general information. EEG changes: slowing of background alpha rhythm (<8 Hz) Minimal Cognitive Impairment: memory impaired but social/occupation normal. Can progress to dementia, and progress can be delayed by cholinesterase inh. Esp w/ APO-E4 Dementia is associated with: Alzheimer’s (most common), Diffuse Lewy Body, Vascular, Wernicke-Korsakoff, Neurosyphilis, Lyme Disease, AIDS, Frontotemporal, CJD, nvCJD Alzheimer’s Disease: Insidious onset, 1st- short term memory, capacity to adapt. 2nd – dramatic memory deficit, delusions, depression, hallucinations… Avg clinical course 8 to 10 yrs. Neurofibrillary tangles (TAU- binds microtubular protein), neuritic senile plaques (accumulation of amyloid b-peptide plaques), loss of Ach neurons at basalis of Meynert/frontal/temporal lobes MRI: hippocampal & temporal/parietal atrophy. Risk factors: age, down syndrome, 1st relative w/ AZ, Apo-E (APO-E binds to Bamyloid and becomes incorporated into the neuritic plaque; also risk 4 dementia in PD & TBI traumatic brain injury) Enhanced neuronal injury: free radical, vascular, head trauma Diminished neuronal repair: ApoE4 loading, defect in processing of APP amyloid precursor protein, hypothyroidism Chromosomes involved: 1 (presenilin 2), 14 (presenilin 1), 19 (APO-E), 21 (APP) Dementia w/ Lewy bodies: (2nd to AZ as cause 4 Dementia) Lewy bodies are intracytoplasmic inclusions and concentrations correspond to degree of dementia. Characterized by cognitive impairment, visual hallucinations, depression, EPS, & delirium like episodes. Unresponsive to L-dopa & worsened by typical neuroleptics. Frontal Lobe disorders: personality change, absence of spontaneity, disinhibition. Frontotemporal dementia (Pick’s disease): language disturbance, change in personality, loss of executive function, Kluver-Bucy, no apraxia/visual-spacial deficits. Frontal/Ant Temp Lobe atrophy, sometimes Pick bodies found. Risk factors include: family history, EtOH, ECT. 13 “How to Survive” Guide – 5th Year Cortical dementia - loss of cognition w/o significant movement disorder Subcortical dementia – comorbid w/ loss of motor fxn. PD and Huntington’s Vascular Dementia – associated with focal CNS lesions and focal neurologic signs (visual field cuts, hemiparesis). Risk factors: HTN, Diabetes, age, male sex, smoking, cardiac disease. Small vessel disease, Multi-infarct, cerebral hypoperfusion, stroke, vasculitis, subarachnoid hemorrhage. Normal pressure Hydrocephalus – gait ataxia (magnetic), urinary incontinence, dementia. Can be Idiopathic, or follow meningitis or subarachnoid hemorrhage. Ventricle enlargement. Wernicke-Korsakoff syndrome – WE (confusion, ataxia, nystagmus) KS (severe anterograde & retrograde memory deficits). Associated with EtOHism, Vit B1 deficiency, grossly affected are mamillary bodies, 3rd ventricle and aqueduct of Sylvius. Onset marked by global confusion and associated w/ confabulation. Neurosyphilis – cause is spirochete Treponema Pallidum. AIDS has impacted the course of this illness. Insidious onset. Symptoms include depression, mania, moderate dementia, & personality change. Sometimes Argyll-Robertson pupils and tabes dorsalis. Lyme Disease – cause is spirochete Borrelia burgdorferi/deer tick bite. Dementia, depression, psychosis. Creutzfeldt-Jakob Disease CJD – triad of dementia/myoclonus/”burst suppression” on EEG. Progressively severe dementia, rapidly fatal course (6 mos). CSF neuronal protein found in almost every case. Prion infection causing “transmissible spongiform encephalopathy”. Transmitted iatrogenically by growth hormone, EEG electrodes, cornea transplant. Fatal familial insomnia is a genetic disease, due to a specific mutation in the PrPc gene. Affects the thalamus, interferes with sleep and leads to mental deterioration. NvCJD – “human mad cow disease”. Young adults. One-year course. Behavioral disturbances, thought disorder, anxiety, painful peripheral disturbance, ataxia. No “burst suppression” AIDS Dementia – triad is Progressive cognitive decline, motor dysfunction, and behavioral abnormality. Anemia, weight loss, low CD4 count, opportunistic infxns. Rapid course. Loss of concentration, memory, social interaction. May mimick depression. Pseudodementia – depression mimicking dementia. Prior episodes of depression. Cognitive impairment w/ affective/vegative disturbance and w/o disorientation 14 “How to Survive” Guide – 5th Year Sleep – a regular, recurrent, reversible state characterized by quiescence and an increase in the threshold of response to external stimuli relative to the waking state. 2 types: nonREM and REM Non-REM – peaceful state relative to waking. Slow pulse, reduced blood flow. Episodic, involuntary movements. REM – highly active brain, originating in pontine reticular formation. Inhibited sensory and motor input. Vivid dreaming. Sleep serves a restoration, homeostatic fxn, and is required for normal thermoregulation and energy conservation. Circadian rhythm is the fluctuation of certain physiological fxns, such as core body temp, serum cortisol levels over 24 hr cycle. Suprachiasmatic nucleus of hypothalamus (melatonin when light low and when light high). Entrainment is the process of adjusting circadian rhythms to environmental rhythms. Dyssomnias – problems in timing, quality, and amt of sleep. (sleep apnea, narcolepsy, insomnica, etc) Parasomnias – abnormalities in physiology or in behavior associated w/ sleep (bruxism, sleepwalking, sleep terror etc) common in children Narcolepsy – Excessive daytime sleepiness and intrustion of REM sleep during wakefulness, occurring daily for at least 3 mos. Cataplexy, sleep paralysis. Hypnagogic (at sleep onset) or hypnopompic (when awaking) hallucinations. HLA-DR2 as well as deficiency in hypocretin (appetite/alertness stimulant) Trx: naps, amphetamine/methylphenidate, clomipramine/imipramine 1 insomnia - sleeplessness that is not attributable to a medical/environmental cause 2 insomnia - sleeplessness that is attributable to a medical/environmental cause Psychophysiological insomnia – pt develops conditioned arousal associated w/ attempts to sleep Insomniacs at risk of accident, depression/anxiety, higher arousal, longer sleep latency, metabolic rate, more beta EEG activity at sleep onset. Etiology is stress, aging, medical disorders, anxiety, caffeine, withdrawal, schizo. Trx is BZDs, melatonin, and Ltryptophan. Discontinue stimulants Breathing-related sleep disorders is characterized by sleep disruption leading to excessive sleepiness (hypersomnia) or insomnia that is due to a sleep-related breathing disturbance. Sleep Apnea and Central Alveolar Hypoventilation. 15 “How to Survive” Guide – 5th Year Sleep Apnea pts stop breathing for 10 to 30 secs at a time while sleeping. Obstructive is most common type. Blockage of the trachea. Central apnea is related to CNS fxn. Obstructive is associated w/ middle age, male, obese, snoring. Central is associated w/ elderly. Trx is CPAP (continuous positive airway pressure), weight loss, avoid supine, surgery, tracheostomy. Pickwickian Syndrome is a related condition in which airway obstruction results in daytime sleepiness. Treatment is focused on weight loss and increased physical activity. Medroxyprogesterone may help improve the condition. Disturbances of Sleep wake schedule: Jet Lag Shift work Delayed Sleep Phase Syndrome Advanced Sleep Phase Syndrome Night terrors Nightmares Sexomnia Basal ganglia (nuclei) deep in the subcortical white matter of the frontal lobes that organize motor behavior. Basal ganglia provide communication b/w the cortex and thalamus via a feedback loop. Sensorimotor information from the cortex is processed by the basal ganglia, which consists of the striatum, the internal globus pallidus (GPi), the external globus pallidus (GPe), the subthalamic nucleus (STN) and the substantia nigra pars reticulata (SNr). Cortical information is relayed to the striatum (the “input” nuclei) via glutamatergic neurons. This cortical information is regulated within tight controls by a constant dopaminergic input from the substantia nigra pars compacta (SNc). Therefore, adequate amounts of dopamine are key for the proper functioning of this complex neuronal network. Direct pathway D1 receptor (facilitatory) / Indirect Pathway D2 receptor (inhibitory) DLPC: executive fxns, attention, - head of caudate Anterior Cingulate: “limbic” motivation, action-related symptoms (OCD, apathy, mania, depression) – ventral striatum/olfactory tubercle Lateral OrbitoFrontal: empathy, socially-adequate behavior, akinesia – Ventromedial/caudate Oculomotor: eye movements – central and caudal putamen Sensorimotor: reaching movements, posture Loops may mix together in danger situations 4 chemical reasons to help PD pts escape! 16 “How to Survive” Guide – 5th Year Parkinson’s Disease: Incidence/Prev ↑ w/ age, more common male. Has genetic component: defective genes Park 1 – 10. α-synuclein/Park 1 chrom 4 (chrom also imp. 4 HD). Parkin/Park2. Familial PD has earlier onset than sporadic. Environmental toxins: MPTP, generic pesticides, rural living, well-water drinking, farming, head injury, occupation (physicians, teachers, miners, loggers b/c of infectious agents/environment toxins. Post encephalitis Caffeine inverse relationship associated w/ risk of developing PD. Thru adenosine receptor antagonism ↑ central DA tone. Protective effects of estrogen on DA system and paraxanthine (caffeine metabolite) PD loss of pigmented SNc neurons. Accumulation of Lewy bodies. Pet scan for nonclinical Dx. Results from deficits in the direct pathway. Greater input to inh pathway, thalamus works more, enhanced cerebral cortex loss of movement & other fxns Dx Motor signs (Pure EPS; tremor, bradykinesia, rigidity). Nonmotor (PD personalityDepression, cognitive impairment, sensorimotor integration, sleep, memory impairment, 1 visual, olfactory systems) -vision – dark light adaptation, perceptual probs, can’t percept middle to high frequency perception. Deficient in DA amacrine cell. Dopa can correct these probs. Posterior parietal cortex visual integration. -Sleep – can be worsened by DA therapy. Insomnia, difficulty falling asleep, frequent arousals, sleep breathing probs, daytime sleepiness, REM sleep behavior, panic/sleep attacks. sleep latency EEG. Cell loss in locus coerulus, raphe nuclei, tegmentum area, parapontine nuclei. SWA () (). Dopa partial normalization for but NOT . Probs consolidating memory related to sleep probs. -Depression. Atypical, apathetic nonsuicidal. Orbitofrontal cortex -Cognition. Attention deficits (dorsolateral prefrontal) DDx – progressive supranuclear palsy (PSP) similar to PD but has oculomotor deficit AND does NOT respond to L-Dopa Physical exam: cogwheel rigidity, abnormal posture reflexes Pharmacologic Trx: neuroprotective. Symptomatic bradykinesia. Early PD: Amantadine, Selegiline, anticholinergic, L-Dopa, DA agonists Selegiline: selective MaoB inh. Enhances L-dopa by slowing oxidation. May L dopa side effects of dyskinesia & psychiatric. Amantadine: antiviral w/ mild antiPD. DA release, inh DA reuptake, stimulate DA receptor, NMDA antag. Best 4 short term & mild disease. Good w/ dopa. DA agonists: directly stimulate DA receptors. Ergot agonists – bromocriptine & pergolide, non-ergot – pramipexole & ropinirole. Require no conversion, no AA transport, No neuronal uptake/release,. Longer axn compared to L-Dopa. Side effects: nausea, vomit, orth hypo, personality, may be neuroprotective w/ antioxidant effects L-Dopa not a cure. Symptomatic trx. Initiate when symptoms disabling. Combine with carbidopa – peripheral decarbox inh. Thus combo prevents nausea, vomit, and orth hypo; amts of Dopa required. Entacapone/tolcapone inh COMT peripherally to enhance LDopa ova BBB & have less L-Dopa transformed peripherally. Side effects: dyskinesias, dystonias, fluctuations in motor fxn. 17 “How to Survive” Guide – 5th Year Antichol drugs: DA depletion produces chol sensitivity. Useful for pts <70yo w/ disturbing tremor. Not 4 elderly. Blocks SLUD. Memory impairment, confusion, hallucinations Progression of PD: [] of DA becomes more dependant on plasma L-dopa levels. Hallucinations can occur n r trx w/ atypicals (quetiapine, clozapine) Sustained release Sinemet in early stages of wearing off phenomenon Deep Brain Stimulation: Pacemaker-like technology delivers electrical pulses to targeted structures in the brain. STN DBS leads to long-lasting (5 years) improvement of parkinsonian motor signs especially tremor and rigidity. STN DBS does not do better than the best that can be obtained with levodopa, especially speech, postural stability and gait freezing, with the exception of tremor. However, STN DBS reduces off-medication painful dystonia and on-medication dyskinesia Drug Abuse: Non-medical or non-accepted recreational use of a drug. Tolerance and physical dependence are biological phenomenon resulting from frequent drug use and can occur in an individual who is not addicted to the drug. Heroin is highly addictive. Tolerance typically lost in 2 weeks, due to effects of drug. Types of tolerance include: microsomal enzymes, cellular changes, behavioral (learned and conditioned), cross (occurs w/in drug class), inverse (sensitization) Physical dependence: inferred from occurrence of abstinence syndrome upon abrupt drug withdrawal. Due to occurance of cellular tolerance (altered gene expression). Type of withdrawal depends on drug category. Environmental stimuli elicit w/drawal symps. -NOT a criterion for addiction. Craving is what separates an addict from a patient! Drugs abused b/c of reward/euphoria produced in DA mesolimbic system. Biological event shared by all animals. High rapid rise of plasma drug [] and very high intoxication levels of a drug carry a higher risk of addiction. Alcohol and barbiturates: Depress excitatory (glutamate) actions at the NMDA receptor and enhance inhibitory (GABA) actions at the GABA-A complex. Benzodiazepines: Enhance inhibitory (GABA) actions at the benzodiazepine modulatory site of the GABA-A complex. Opioids: Act at the m-opioid receptor. Cocaine: Blocks the DA transporter in CNS. AMPHETAMINES: Presynaptic release of DA in CNS. CAFFEINE: Antagonists at the adenosine receptor. NICOTINE: Agonists at the nicotinic receptor in brain. LSD and LSD-like hallucinogens (LSD, DMT, MDMA, ETC): Agonists at the 5-HT2A receptor. Phencyclidine (PCP): Noncompetitive NMDA calcium channel blocker.Marijuana: Agonist at cannabinoid CB1 and CB2 Receptors. Methadone can be used to trx heroin addicts b/c it is slow-acting, long half-life so it is asymptomatic ova 24 hrs, no “high” nor w/drawal symptoms. 18 “How to Survive” Guide – 5th Year Stroke: Frontal – behavioral planning, working memory, affective processing, attention. Parietal – attention, special location, body image, xfer of sensory info to motor sys. Temporal – declarative memory, emotional processing, receptive language Lenticulostriate Arteries Supply the Basal Ganglia and Internal Capsule Anterior circulation – internal carotid arteries. Posterior circulation – vertebral arteries Ischemic Stroke: Mechanisms and Treatment Inadequate blood supply to a region of the brain for long enough time to cause death of brain tissue Refers to both hemorrhagic events and ischemic infarction In an embolic infarct a piece of material, usually a blood clot, forms in one place and then becomes lodged in a downstream vessel. In a thrombotic infarct a clot forms locally on the vessel wall, usually at the site of an atherosclerotic plaque, causing occlusion. In addition to focal neurologic deficit, headache is common. Seizures also occur fairly regularly in stroke. Stroke Risk Factors Imaging of brain should be done ASAP to rule out hemorrhage. Infarct will often not be visible on early CT, but hemorrhage will. Once hemorrhage is ruled out then thrombolytic agents can be used including tissue plasminogen activator. Heparin can also be used in those who cannot receive TPA. Middle Cerebral Artery -arm or face-arm-leg sensorimotor deficits Anterior Cerebral Artery semiautomatic movements of contralateral arm Posterior Cerebral Artery lateral sensory loss/weakness (ICap infarct) Watershed Infarcts: When decreased blood flow in adjacent cerebral arteries occurs the regions at the borders of the two vascular territories are affected most. These border zones in vascular territories are called watershed zones. MCA-ACA Watershed Proximal arm and leg weakness Aphasia syndromes if dominant hemisphere affected MCA-PCA Watershed Higher order visual deficits Stroke: diminished/disrupted blood supply in the brain (ischemic & hemorrhagic) 19 “How to Survive” Guide – 5th Year People who have had one stroke are, in most cases, at an increased risk for recurrent strokes Prevent Recurrent Strokes: 1.Work with the Physician (med management, proper trx of related conditions, endoarteriectomy) 2.Use Medications as Prescribed (antiplatelets; aspirin/ticlid/plavix, anticoagulants; warfarin/heparin, statins, insulin/hypoglycemic drugs/-glucosidase inh/Thiazolidinediones, antihypertensives) 3.Follow a Healthy Diet (low fat, sodium, high fruits/vegs/fiber/omega-3) 4.Exercise Regularly (control Bp, relieve stress, “burn” fat, dec risk of CVD) 5.Quit Smoking 6.Manage Your Weight and Stress 7.Know the Warning Signs of Stroke (numbness, weakness, paralysis of one side of body) Transient ischemic attack (TIA): acute loss of focal brain or monocular function symptoms lasting <24 hrs due to inadequate cerebral or ocular blood supply. Stroke same as above but >24 hrs. -mechanism of stroke: Infarction (cerebral atherothrombosis, cardiogenic embolism, penetrating artery disease, other) > hemorrhage Acute Intervention: IV tPA, Briding tPA, IA tPA, MERCI, 20 “How to Survive” Guide – 5th Year SYSTEMIC PATHOLOGY Advice from Akeem Marsh: Systems systems systems. After having completed Step 8, Host Defense, Infection and Pathogenesis successfully, you all must be experts in general pathology so I totally commend you on that. That is a very good thing, and necessary as Systems Path is a whole new ball game. Fear not though, having made it to fifth year this is one of the last barricades that you have to overcome, and that you will do. The course as the name implies is organized according to systems, just like histology, physiology, and pharmacology. In approaching this course, most definitely keep an open mind and study it very well as it will be great preparation for the upcoming USMLE exam. The subject itself is very integrative and it will bring back elements of all those subjects that you thought you forgot including biochemistry, immunology, microbiology, etc. It is integrative in such a way that if you forgot it from before, you will relearn it this time around and remember it better because it will fulfill any empty gaps that you have had in learning (i.e. learning exactly what SSPE associated with measles virus really is). How to study for this class? The single most important resource is WebPath. WebPath, WebPath, and more WebPath… haha. Make sure that you read something to get a good foundation of the material, this is necessary for you will need to know this information for step1 and your future career. I suggest reading through Robbins, or little Robbins. There’s also BRS and class notes, as I did, not as a lazy way out but the only way that I found useful given what I could get done effectively. A better text than BRS may be Goljan Rapid Review, since Goljan is the man! I did not use it myself as I didn’t discover Goljan until after pathology course was done, but you should invest in that if you need a review book and haven’t gotten one yet. There is also a huge syllabus of materials that looks like it was photocopied from papyrus. I would not recommend spending a lot of time on that as it is very verbose and boring. Ultimately do as you please but make sure that before all of your written exams you go through the WebPath questions twice and make sure to go through the pictures on WebPath as they almost certainly will be some repeats. The format of your written exam will be very similar to that of Step8 except that you will not have as many questions per exam. There will be probably a total of I think maybe 60-70 questions and of that, like 10 or 15 will be pictures (double check the syllabus just to make sure). As long as you keep up with the material in class and make sure to utilize your WebPath resources you should be very fine for this class. Miniboard Exam: Overall, this miniboard though covering a lot of information was not one of the more difficult miniboards. Basically, if you studied Pathology, that was what was tested on and you would do fine. Having said that, the best resources for this exam to me where BRS Pathology and Kaplan Questions. I did not do PreTest myself, but I heard that it was good from many people. Do not sleep on general pathology at all, as it will make up a good portion of your exam. First Aid section of Pathology was really good for this exam as well. 21 “How to Survive” Guide – 5th Year One more thing, Goljan audio! I did not discover Goljan until after path was over with, but I found it to be an excellent review and learning tool for pathology. I would recommend that you listen to his files as an adjunct to your own studying, so that all the while preparing for course exams you will be preparing yourself for the miniboard as well. Also, the way he explains things, you are bound to learn a good amount of pathology. Happy Studies. Advice from Shahla Syed: Robbins is an INCREDIBLE book - if you read at a decent speed, this is excellent. Also, the class notes are quite good as well, and everyone recommends reading BRS for the miniboard and for the Step 1, so I guess I would recommend that as well (though I never read it, it is supposedly the best to use) so at least you have an idea of what it is like before you start reviewing for the boards. Advice from Barry Ladizinski: As you probably already know, in sophie, class notes are the name of the game, luckily though by 5th year students arent the only lazy ones. Some extra tips though, for pathKNOW THE WEBPATH MCQs and pictures for the written, you WILL see them again. For the practical listen to what Dr. Lipper emphasizes, they’re usually on and if not just focus on the most common pics, ie SCC RCC SEMINOMA etc. Also , while BRS is great and all GOLJAN (RAPID REVIEW SERIES) and his lecture notes are way more fun! Advice from Galina Borodulina: I recommend reading the small version of Robbins. BRSing it alone is not going to cut it. If you really want a good understanding of the material you need to read a text, and the big robbins/rubin is just not possible. Get the robbins question book if you don’t already have it, it is GREAT for review and has great questions, better than BRS or pre-test questions. As for the syllabus (which is thick enough to be called a book itself), I read it sporadically, but honestly if you’re reading the book there really is no need to read those papers, however, be aware that once in a while some questions come from the syllabus (like the breast pathology questions) which were too detailed for little Robbins. But this is a very rare occurrence when profs want to be picky. 22 “How to Survive” Guide – 5th Year EPIDEMIOLOGY (CLINICAL DECISION MAKING) Advice from Galina Borodulina: For epi all the exam questions come from the material covered in class and in the syllabus. its all there, and the recommended readings show up on exams, even though they are just "recommended" . this is yet another SD epi course, brace yourselves.. Advice from Barry Ladizinski: Blah dont bother you’ve learned the material 1000x and compared to Dr. Sekhobo its a breeze. Advice from Shahla Syed: Don't worry, just pay attention in lecture, Dr. Lubetkin thoroughly goes over everything you need to know for that class. If you want to read the textbook, its short and quick, but if you don't, don't worry because Dr. Lubetkin is quite good. Advice from Akeem Marsh: There are summary/review sheets given before each exam, so that will further help guide your studies. 23 “How to Survive” Guide – 5th Year PATHOPHYSIOLOGY Advice from Akeem Marsh: This is a very good course to take before step1. It is systems based, and is a very integrative review of what you have learned so far plus it integrates well clinical information. Studying for this class is in effect like studying for the boards, they go hand in hand so well in fact, many people when studying a particular system for an exam in this course would review as well the relevant materials specifically for the step. Anyway, I don’t really have much to say for this class except that I thought that the exams were tough in relation to the material lectured on. There was no particular textbook recommended, so researching information related to some lecture topics was challenging. Nevertheless, a good majority of the class was able to do very well. However, some people did run into academic difficulty. So I will suggest that nobody sleep on this course, as on paper it appears very easy to pass. It is only to your benefit if you take the course seriously and prepare for it because you need to know this information as a doctor plus it will help you in your preparation for the USMLE step1 exam. You will have a few written exams and a miniboard. Best advice for the written exams, study your lecture notes and you can read up in this book, Pathophysiology for the Boards and Wards. It is a small handheld book that is really helpful for this particular course. I would recommend reading it along with your pathophys course, but the only problem is that it is information dense and a lot to take in, but at the end you will be very knowledgeable on the important information. It is of course, no substitute for the notes, but only meant as a complement. There’s also a pretest for Pathophysiology that many people used to test themselves while studying for the course exams. I think that it was somewhat helpful, and worth doing to test your knowledge. It like other pretests and sophie classes does not particularly correlate, but can’t hurt. The miniboard exam for this course is basically a practice comprehensive step1 exam. They call the miniboard for this course, Intro to Clinical diagnosis, but basically if you know your basic sciences well (the material that you should have been reviewing for step1) and if you actually paid attention in physical diagnosis class then you should have absolutely no problems with this. In preparation for this, there is no particular book that was useful, I mean some people did Intro to clinical diagnosis pretest, but I’m not sure how helpful that was as I did it myself and didn’t really see much correlation there. For this test, if you like doing lots of questions the Pathophys pretest may be good, but I do not think that it gives any particular advantage because the material tested was more related to the step1 material than anything else. Advice from Barry Ladizinski: You’ve learned the material already and studying for step 1 is more important by then anyway... 24 “How to Survive” Guide – 5th Year PHYSICAL DIAGNOSIS Advice from Akeem Marsh: Physical diagnosis is a very easy class. It pretty much is like if you show up you will pass. The entire purpose of it is to teach you diagnostic techniques that will make you a competent physician when you hit the wards, upon transferring to the medical school. The task of performing an entire physical exam may seem daunting at first with all the little parts that you have to do, but this is what everyone has to go through as a medical student… it is part of the rite of passage so you just have to suck it up. Plus, I found this to be fun actually, especially if you have really cool friends or family that would let you use them as test dummies. You will be told to read Bates textbook. It really is a good book, may I chime in. But, I’m not particularly a fan of Bates Book so I would recommend instead you get the pocket size edition that is much smaller and can be used as a quick reference. You will have workbook assignments, but they do not require the textbook to do. As for the tools that you will need, you don’t really need to buy the otoscope or ophthalmoscope, as those usually are present in hospitals but you should get them if you want to practice on your own, for you will have to be proficient with them when doing rotations in the third year of med school (at least peds, and medicine). You definitely should get the stethoscope (but it’s unnecessary to get the most expensive fancy one, just get the recommended unless you like the expensive fancy stuff), also tuning forks, reflex hammer, and a pen light. Additionally, they do not recommend this but I urge everyone to get a Maxwell Quick Reference ISBN: 0964518135. It is really cheap and will come in handy for the rest of your life as a doctor. It has a bunch of goodies on it like a mini physical exam outline, history outline, mental status exam, normal lab values… etc. GET IT !! lol Besides that, you just need to show up and you will do fine. Here are some websites where u can listen to heart or lung sounds and/or observe the physical exam done by professionals for your own review. At the end of the class you have a practical and a written exam. For the practical, you know what to expect, basically know how to do your physical exam. Practice on each other, and review the steps on index cards or a review sheet. The written exam, make sure you know what the signs on the physical exam are, such as McBurney’s point or Chvolstek’s sign. You will learn about these. Neurological exam: http://edinfo.med.nyu.edu/courseware/neurosurgery/ Comprehensive physical exam: http://medicine.ucsd.edu/clinicalmed/links.html Modules on developing bedside manners: http://depts.washington.edu/physdx/ Heart sounds: http://www.sci.sdsu.edu/multimedia/heartsounds/ Lung sounds: http://www.rale.ca/Repository.htm Advice from Barry Ladizinski: For physical diagnosis the exam comes from the homework’s you get and the tools are a waste of money unless you direly need a ten dollar eye chart but learning the physical exam is key as you will do it 1000x in the future.. 25 “How to Survive” Guide – 5th Year COMPREHENSIVE BASIC SCIENCE EXAM Advice from Akeem Marsh: Early on during the spring semester of your fifth year, you will be given a Comprehensive Basic Science Exam. This is basically a comprehensive miniboard, containing 200 questions in the same format as all of your miniboards and it is sort of a glimpse of how step 1 should be, in terms of integrating the different subjects together and not having them in any particular order. Since the exam shows up somewhat abruptly, people get all worked up and nervous. Having read this text from me, it may not be so abrupt but you will still have some of those feelings of nervousness and anxiety. Fear not though, for you should take it for exactly what it is intended to be: a diagnostic. I think that it is very good that the school provides this for the students, for it shows you early on exactly where you stand in terms of knowledge and gives you insight into what you should get up on. For instance, the test showed me that I was strong on subjects as biochemistry, genetics, and neurology (can’t explain the last one) but I was weak on the subjects of respiratory system and microbiology subject. [The results of this exam are displayed in such a way that you can see the breakdown of how you did both by system and by subject.] After learning of the results, I began my USMLE step1 studies with a read through of Microbiology Made Simple and extensive review in first aid, along with a review of the respiratory system from anatomy, physiology, pathology, and pharmacology. This ended up coming in handy actually because there was a good amount of microbiology questions on my exam that I may not have known otherwise had I not had the insight to study it from this test. So bottom line is, take the test to be a diagnostic tool as to where you stand and let it guide your studying from there on! Note, obviously you know if you do well on a subject/system on the diagnostic test, that doesn’t mean overlook it (ie. behavioral science). I mean, you have to weigh things according to how you feel comfortable but by no means, do not overlook any particular subject or system because that might come back to haunt you. 26 “How to Survive” Guide – 5th Year THE FINAL STEP OF SOPHIE: THE USMLE STEP 1 Advice from Shahla Syed: I have a lot more advice for Step 1 - don't overburden yourself with reading too many books, because that will probably lower your score rather than raise it. Pick a select few and stick to those. My recommendations are learn Micro, Immuno, Behavioral, and Pharm from First Aid. For anatomy, if you have BRS, go through the chapter summaries and clinical outlines at the end of each chapter because First Aid isn't enough. For biochem, well I never understood biochem to begin with, so pick any review book and learn it if you didn't already. First Aid is a good review of biochem if you already know biochem, but you can't learn it from first aid. Pathology - many people say use BRS, but I hear even better than that is Rapid Reivew written by Goljan who is awesome. The book is lengthy, but incorporates a lot of the other topics into it, and I think it also has questions which is nice. I haven't read it, but I believe it may also incorporate the biochem you need to know, in which case you may not need a biochem review book. Also, Goljan has a 100 page path outline which is excellent, and a shorter 36 page high yield packet if you don't have time for the 100 page packet. I'd recommend using those. People also say use BRS or Costanzo for learning physio - take your pick, I didn't read either of them so I wouldn't know. I also would advise not using the Kaplan books because they actually miss a lot, and I didn't do QBank either but I heard it is not very similar to the exam. I hear USMLE World is a lot cheaper and a lot more effective at covering the concepts covered on the exam, so that is a better choice. It's also more difficult that QBank but people say is more like the real exam. So bottom line - First Aid, Anatomy BRS, Rapid Review for path, Physio review book, and Goljan packets. That's all :) I hope this helps, and I wish I had known these things before I started studying!! Advice from Barry Ladizinski: And for step 1 the basics/general principles are really important... first aid is okay but just really try to understand everything this last year ("WHY something happens, NOT WHAT") anyway hope this helps you’re about to join the real world so really enjoy your last year as a professional student... Advice from Akeem Marsh: Anxious, nervous, freaking out? Well Certainly don’t do any of those things, actually you can do a little of it . It is a big exam, and carries a lot of weight, plus it will be with you for a while. Read through the beginning chapter in first aid for USMLE step 1. That should clear up any qualms you have about the exam itself, such as how many questions, how is the format, how is it graded… Once you have done that and have your understanding, it is time to tackle studying. Now, with all the material you have learned thus far, it is very easy to become completely overwhelmed in exactly what you NEED to 27 “How to Survive” Guide – 5th Year know for the exam. The amount of material that you have processed in the past few years is just mind-boggling, but let me tell you that you know more than you think you know. Some people will swear up and down that they forgot EVERYTHING or at least some things, but everyone remembers much more than they think that they know. Also, we all have our strong subjects and our weak subjects. The weaker subjects you should probably devote more time to. I recommend that everyone begin studying months in advance, but not too early. I would say about 2 or 3 months before the Step, because I believe this time period to be ideal. You will become sick of studying after a time, so be forewarned. That is why I suggest not starting the study specifically for the step too far in advance, plus the courses that you take systems path and pathophys are good prep 4 the board. The most important subjects to study vary by board as self-reported from after the exam people would say, that their exam emphasized certain topics. Each person said different topics. This could be a big bias tho, because people tend to remember what they got wrong and in turn would lead them to say that their weak subjects were emphasized when in fact there were relatively few questions on it. I found the best way to describe it was like a really long miniboard, but the questions were not long, they were like 2 or 3 lines but required much more thinking! I would say, however you choose to study for the step, integrate it with first aid. Review the relevant sections of first aid when you complete a subject, or system, and write stuff in when you feel necessary (that is why they have those huge margins). At the end of your studies, you should have read through first aid at least 2-3 times before taking the step, and you would definitely get at least your passing score which is the most important thing (but probably a lot better). As for what specific books to use, I recommend that you use whatever books had worked for you in the past when studying for miniboard exams. Actually, you can use more condensed versions of them if possible. For instance, for physio, the Costanzo text is great, but if you don’t feel like reading all of it then the BRS is more than sufficient. I would recommend at least reading a book for physio (ie BRS), for path (ie BRS or Goljan Rapid Review), and for any other subject that you are weak on! For all other items, first aid by itself, along with the question bank that you choose certainly would be more than sufficient. As for what question bank to use, I would recommend using USMLEWORLD or USMLE RX (preferably world). From personal testimony of those that used it, it was most similar to the exam in terms of content and format. As for Kaplan Qbank, I would say if you want to do that please don’t spend $$ on it, borrow someone else’s. I personally felt that it was way over rated, because it was very nitpicky and basically just tested whether or not you read the Kaplan review books. DO LOTS OF QUESTIONS, AS I AM SURE THAT YOU ALREADY PLAN ON DOING!! DO THEM VERY FREQUENTLY, AND I WOULD RECOMMEND THAT YOU USE THEM AS A TOOL TO TEST YOURSELF. For instance, when you complete neurology, you should do a question set in neuro. This information is explained in that first chapter of first aid, but I thought I’d reiterate it here to bring the point home. Another thing that you absolutely have to do is go over both the NBME form exams, and the NBME released items. Those in fact are the most similar of anything to the USMLE. The only problem is, there is only maybe 800-1000 or so questions amidst 28 “How to Survive” Guide – 5th Year them, so you certainly will need a qbank to test yourself. Check the student government computer, there is a huge compilation of USMLE materials left behind, courtesy of yours truly. Overall, take heed to Shahla Syed’s advice because I think that it is excellent, I am pretty much repeating/paraphrasing what she said, except that the bolded items listed above are what I think to be important for you to do that she did not mention. One the SDSG computer, there is a file called Imagebank, and I found that to be a very good review for the boards, like a week before the exam especially for those of you who like me, did not really look at any pictures while studying LOL. One last item, I found Goljan (pathology) audio files to be excellent! Especially for those of you that like to exercise and/or are commuters, you can just put on some Goljan audio and listen and learn. His teaching style is amazing, the way he explains things and integrates items from other subjects is right on point. Not everyone found his files to be that good, but I think that if you just listen to them more than once (and the 2nd time around, speed up the audio) it would be good. Especially for those particular systems that you are weak on, as I listened to those files several times. [I even played it in my sleep to get subliminal messages lol, not sure if it worked but hey can’t be a bad thing!] I think that you guys having made it to the fifth year (yay) are well on pace to do well on this exam. Just keep the faith in yourself, listen to the advice of the upperclassmen and study diligently as you always do, and I believe that you all have the potential to set a record in sophie in terms of first time pass rate. Let that be your guiding light, not just because you want to pass and move on to the next level, but because you all want to and will become great doctors for your patients!!! That is essentially who we are really working for in medical school. Hope that this advice has been helpful and, feel free to contact me again about anything, same email or u can contact akeem.marsh@downstate.edu my new email . Some other stuff that I found on the internet that you may find useful: Concentration/anxiety tips: Your inability to focus is likely just due to anxiety. One simple method that seems to help others minimize how often their mind wanders that you might want to try involves a simple tallying procedure. Each time you notice that you aren't focusing on the task at hand, make a tally mark on a separate sheet of paper. The mere act of having to tally the instances gradually reduces the frequency, probably due to some subtle process of negative reinforcement. At any rate, it's worth a try and actually has decreased the problem for many who have tried it. But don't expect this to be an instant fix. You have to keep making yourself keep the tally for a number of days or even a few weeks to begin to see the impact. You may also need to vary your study mode more frequently, switching from just review reading to trying some questions or to summarizing key aspects because each mode switch reawakens attention. Others find that taking short breaks more frequently in a long study day helps them stay focused. Here are some tips on handling anxiety: Tip 1 Some weeks or days prior to the exam, use an index card to list several of your greatest personal strengths and attributes. Examples: I am an intelligent and caring person. I react well under pressure. I am going to be a great (fill in career goal). Keep the card handy so that whenever negative thoughts intrude while you are studying or practicing, you can pull the card out, read each statement and reflect on your abilities. Luxuriate in the calm, positive feelings that are associated with each of these true statements. Fairly soon, you won’t even need the card because you will know the statements by heart and be able to mentally review them as an antidote to the welling up of negative thoughts. 29 “How to Survive” Guide – 5th Year Tip 2 Keep a master tally sheet nearby each time you sit down to study. Make a tally or hash mark each time you find yourself engaging in negative thinking, daydreaming or otherwise mentally escaping from the study situation. For many students, the mere act of tallying reduces the frequency of these behaviors and they find that their daily tally decreases over time. This is really a mild form of behavior modification that you can apply to your own study behavior. Though simple, it works well for many people. Tip 3 Months (or at least a few weeks) prior to the exam, spend some quiet time thinking back in your life to recall an event in which you were the hero of the situation. Perhaps you walked in on a serious fight between two friends and were able to bring it to a peaceful resolution. Perhaps you administered CPR successfully to someone or orchestrated a successful fundraising event for a charitable cause during high school or college. Whatever life event you select, it must be a situation in which your abilities and actions solved a problem or saved a bad situation. Now spend at least 10 minutes each day in a quiet place reliving this event, trying to bring back the memory in as much detail as possible. What time of year/day was it? What were you wearing? What was the setting like? As you practice, it will take less and less time for you to get back the memory in graphic detail. The purpose of this exercise is to allow you to mentally revisit the event quickly, because stored with this event memory are all of the associated feelings of being in control, being a successful problem solver, being confident, being a winner. When used as part of a time-out in an exam, these associated emotions then act to counteract the negative emotions associated with the test-taking process. Tip 4 During the actual test, have a thought-through pacing plan that you used in practice testing in the final week or two. By knowing what time you have to complete each section of a test, you can establish 1/4, 1/2 and 3/4 points before you even begin answering questions. Then, when you reach a time marker item, check your time use. Worrying about running out of time contributes to anxiety and often leads to time-wasting behaviors such as checking the clock every couple of minutes--a nervous habit that actually increases the time it will take you to finish the booklet because frequent glances at the clock continually interrupts your thought process and often results in the need to re-read once you look back at the question. If you do run short of time toward the end of a block, use question "triage." In other words, scan the remaining items to find ones that are easier and mark these on your grid sheet first (taking special care to find the right bubbles to mark). Then return to the remaining items and mark an answer for all of them. Remember that no answer is an automatic error, so never leave items blank. Pacing problems will be far less likely to occur if you work through lots of sample tests during your preparation. With practice, you will sense the right pace and so be able to walk in on test day confident that you can handle it because you have already done so in practice mode. If you do this, the test setting will feel more familiar and less strange, and the more familiar it feels, the less anxious you will be. Tip 5 If you feel anxiety welling up during the exam that is interfering with your ability to concentrate on the questions, shut your eyes, lean back, roll your neck and rotate your shoulder muscles. Take several slow, cleansing deep breaths and exhale slowly. This "mental time out" helps break the cycle of anxiety and will usually help you return to the task at hand with a greater sense of calm and better concentration. Note: If you experience significant anxiety symptoms such as muscle twitching, insomnia, nausea, or chest tightness when you think about taking exam or during them, then these tips may not be enough to help you overcome the problem. If this happens, seek professional help from either a psychiatrist or a cognitive psychologist who is experienced in helping people overcome situational anxiety. Therapies can include anti-anxiety medications, self-hypnosis instruction, etc. But don’t delay because each of these treatments requires time to become effective. In seeking a professional to help you, don’t see just anyone. The professional needs to have experience in treating this type of problem, so not just any therapist will do. How to Study Actively One of the most common problems when people are studying for long periods of time is that they fall into passive, almost mindless mental habits. Eyes dutifully move over the lines of print, but not much goes into long term memory. Even worse, if the information is being reviewed, it already looks familiar, so you can 30 “How to Survive” Guide – 5th Year easily fool yourself into thinking 'Yes--I remember this--I know how this works.' Unfortunately, following along when the information is all laid out on the page and being able to call the relevant information from memory when you are dealing with a question on that material later are not the same thing. Even when you know a lot, you may apply the wrong information to an item, or get confused about what applies from what you recall. Here are some tactics that you can use to study more actively, which all require doing something with the information, rather than simply reading through it with the intention to remember. Look over some practice questions on a topic you are about to review first. If it's been a while since you studied a topic, you may not actually be able to answer the items yet, but just reading the question, to get a clear sense of what's being asked is your goal here. After you finish looking at the items, traces of what was called for by the items will linger in your memory, making the questionrelevant information jump out once you begin reviewing this content. Make key aspects and relationships stand out in your study notes. Most people take notes when they review. But if you aren't careful, it's easy to just write down without really thinking about the information. To make those study notes really work for you, take a few minutes to look over the kind of material you are about to review. Is it describing several disorders that present similarly? Are there key lab tests that tell you which disorder you are dealing with? Do the disorders hit different groups of patients (the very young, post-menopausal women, certain ethnic groups, for example)? Can you generate a way to compare and contrast the varieties of disorders, showing how they are similar and different from each other? Once you have a clearer sense of the kind of information you are dealing with, decide how to represent the key aspects on paper in a way that highlights these aspects. Techniques for doing this can include: 1. Using boxes with arrows to show the ordered steps of a process or sequence of events. 2. Color highlighting your notes, e.g., pink for lab data information, blue for presenting symptoms, yellow for incidence (who gets it), green for morphological changes, etc. Now when you look over pages of notes, you can scan all the pink to see how the anemias differ in terms of their labs, for example. 3. Use a tape recorder to make summary notes instead of paper. You can even ask yourself questions, leaving a pause after for later listening and self-quizzing. By forcing yourself to articulate what you want to remember in your own words, you are more likely to remember the key points and you have a portable study aid to plug into later, in the car stereo while you are driving or using a Walkman to listen to while you do chores or take a walk. 4. Make charts of related groups, such as the types of meningitis. Rows for each type, columns to show the bug, presenting findings, typical lab results, prognosis, etc. Color code as necessary to make exceptions and shared features and key aspects stand out. Switch activities to stay mentally alert. If you are sitting at your study table and find that you are just spinning your mental gears, stop what you are doing and do something else. You might switch to a different kind of material as a break (shift from internal medicine to psychiatry, or from Microbiology to Physiology, for example). Look at a clinical website on the study topic for a change of pace. You can also try doing a few practice items on the material, then look up the related material in your review source to understand the correct and each incorrect answer. Now, what you read is relevant to an actual question and this will help you take in the information because it is perceived as more meaningful than just reading page after page in the book. Find a study partner to do questions out loud. If you are enrolled in a Kaplan Center, find someone who is willing to sit with you for an hour or two several times a week. Agree in advance what topic you want to focus on, then take turns doing items out loud, reading the stem out loud, stating what you think is being asked, and talking through your reasoning as you evaluate all the possible answer choices. The other person should listen for reading or reasoning mistakes and give feedback. Then switch roles and you give the feedback. Don't get bogged down in fine details while dong this, however. The goal of the session is to refine how you interpret and reason with what you already know, not to worry about checking out every little detail. Use the question explanations when you get stuck because neither of you recalls, or just skip that question and move on. This is an excellent way to practice applying what you know and to improve your accuracy in understanding and reasoning through test questions. 31