1) - Christine Peterson
advertisement

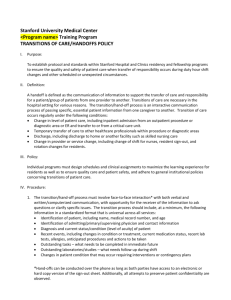
Running head: HANDOFF COMMUNICATION Developing a Standardized Handoff Communication Christine Peterson Azusa Pacific University HANDOFF COMMUNICATION 2 ERRORS IN PATIENT CARE RELATED TO POOR HANDOFF COMMUNICATION The process of handoff report varies from hospital to hospital, floor to floor, and often from nurse to nurse. Few hospitals today have a standardized shift report that every nurse uses. Handoff report may take place in multiple locations, use multiple different tools, and vary in the order it is given. Poor handoff reports have been found to be a significant cause of errors in patient care. Developing a standardized handoff report may prove to reduce errors in patient car. Current handoff environments vary and include hallways, nurses’ stations, and patient rooms. The tools used in hand off reports may include patients’ electronic medical record, nurses’ own SBAR forms, and blank pieces of paper. The people involved in this process are the nurse from the previous shift and the nurse from the oncoming shift. Handoff reports may also involve the patient and their families. Differing processes and orders of handoff reports contribute to missed information and subsequent errors in patient care. The goal of this intervention is to develop and implement a standardized handoff communication tool and checklist for end of shift report. A standardized handoff routine will be implemented including bedside report at every patient handoff. Risk Analysis In an article by Berkenstadt et al. (2008), the authors discuss a study implemented as a result of an error in patient care. A patient who was admitted to a medical step-down unit experienced severe hypoglycemia after receiving an incorrect insulin dose. Following this event facts were collected regarding the event and how it occurred. The error identified was during handoff report. The nursing handoff report took place at the nurses’ station as opposed to the bedside, which was the hospital’s policy (Berkenstadt et al, 2008). The authors observed 224 nursing shift handoff reports and based on the analysis of the data collected along with structured HANDOFF COMMUNICATION 3 interviews with senior nurses, developed a standardized handoff process. The intervention in the study included a checklist and protocol for handoff and the use of simulation in order to practice its proper use. The authors then observed handoff reports after and recorded their observations. The results showed that after the intervention, “there was an increase during the handoff process in the number of nurses indicating the patients’ names, ages, diseases, and the reasons for admission” (Berkenstadt et al, 2008). Furthermore, there was an increase in nurses describing events that occurred during the previous shift. There was also a 100% adherence to presenting treatment goals for the next shift, as opposed to 88% before the intervention (Berkenstadt et al, 2008). In 2006, goal 2 of the Joint Commission was to “improve the effectiveness of communication among caregivers”. In a review of sentinel events, the joint commission found that from 1995 to 2006 the leading cause was poor patient handoff communication (The Joint Commission, 2006). Open communication between nurses and patients is an important factor in fostering a safe patient care environment. Patient satisfaction with nursing communication may improve patient disclosure and ensure a safer environment. In a study by Kimberly Radtke, the author sought to determine if standardizing shift report would improve patient satisfaction with nursing communication (2014). The study implemented a pilot bedside shift report process on a medical surgical unit. The author noted that nurses voiced frustrations related to information that they received during shift report. Getting a poor hand off report can make nurses feel behind before they start their shift. Complaints by nurses that were noted in the study included, “I didn’t hear that report,” and “Medications were not given,” The intravenous fluids weren’t right/ wrong rate.” The study found that patient satisfaction in nursing communication rose from 75 to 87.6 percent (Radtke, 2014). HANDOFF COMMUNICATION 4 The World Health Organization (WHO) suggests that organizations ensure health care organizations implement a standardized approach to handoff communication between staff, change of shift, and between patient care units during a transfer (2007). Furthermore, WHO recommends that components that should be included in such standardized handoff communication are the use of the SBAR, allocation of sufficient time, information about the patient’s status, medications, treatment plans, advance directives, and any significant changes, and finally, limiting the exchange to only what is necessary to provide safe patient care (2007). WHO also suggests that hospitals utilize proper training on effective handoff reports to hospital staff (2007). Process Analysis People Materials Patients Nurses Nurses own SBAR form EMR Errors in Pt Care R/T poor handoff report Effect Hallway No standardized handoff Nurses Station No organized process Environment Current Process Figure I. Poor handoff report has been found to contribute to errors in patient care. There are several factors that contribute to poor handoff report. Figure I describes factors involved in handoff report that may contribute to these errors. The current people involved in handoff communication are the nurse from the ending shift, the nurse from the oncoming shift, and in HANDOFF COMMUNICATION 5 certain circumstances, the patient and their families. Materials involved in handoff are the electronic medical record and nurses’ own SBAR forms. Forms used by nurses may include a nurses’ own developed format, a standard form developed by each unit, or a blank piece of paper. Environments in which handoff communications occur are the nurse’s station, hallways, and patient rooms. Finally, the current process varies from nurse to nurse and unit to unit. The lack a standardized handoff routine and checklist contribute to patient care. In examining the contributing factors in figure I, the nurses involved in the handoff report as well as the process and environment have the greatest impact on the problem. Giving handoff report at the bedside can improve handoff report as well as include an additional person, the patient, in the process. Including the patient in the handoff communication allows them to be a part of their care as well as fostering a trusting nurse/patient relationship. The handoff communication tools such as the electronic medical record and report forms are one area in which nursing staff has great control over. Working together, nursing staff can develop a standardized form for handoff communication, which will improve the ease and effectiveness of change of shift report. According to the world health organization (2007) possible barriers to implementing a standardized bedside report include resistance to change behaviors, time pressures, training and cost of time to implement new processes, low health literacy, staffing shortages, and lack of knowledge about how to improve systems. Another barrier to consider is that different units may have different requirements for a standardized handoff form. Older units also do not have a computer in the rooms, which may make it difficult to have the electronic medical record open during report. It may be necessary to require nurses to bring a computer on wheels (COW) into the room when they are giving handoff report. HANDOFF COMMUNICATION 6 Recommendations for Change Two theories described in Radtke’s study include Peplau’s interpersonal relations theory and Lewin’s theory of changing practice. These theories point to the need for a change in handoff communication practices to one that is done to involve the patient to enhance the nurse/patient relationship as well as to improve its effectiveness and provide a safe patient care experience. Radtke describes Peplau’s interpersonal relations theory in her article (2014). Peplau’s interpersonal relations theory describes nursing as therapeutic. He notes that while knowledge and practice of nursing are important, they are secondary to interpersonal relations. Peplau states, “Nursing is an educative instrument, a maturing force that aims to promote forward movement of care” (Radtke, 2014). Nurse patient relationships is a vital part of the nursing process and is necessary in assessing, planning, and intervening on behalf their patients. Allowing for therapeutic relationships in nursing care is an important part of safe and effective care. Providing bedside report helps to promote this therapeutic relationship and also builds patient satisfaction with the nursing care. Providing a therapeutic relationship also helps the patient to trust nursing staff and therefore allow for effective care. An effective bedside report enhances trust, mutual understanding, open communication, and mutual goal setting (Radtke, 2014). HANDOFF COMMUNICATION 7 Figure II. Additionally, Radke describes Lewin’s planned change theory, which describes changing practice as a daunting practice that includes a “realization that change is required and acceptance that it can bring improvement” (Radke, 2014). The theory points out that change should be instituted when there is a need for it to improve patient care, however it should not be instituted simply for the sake of changing things. Instituting changes in shift report in order to ensure a standardized bedside shift report can improve patient safety and care. Lewin describes change as a process that involves an unfreeze, change, and refreeze. The change implemented in order to better the healthcare environment should become permanent. Figure III. Klee, Latta, Davis-Kirsch, and Pecchia (2012) discuss the benefit of using continuous performance improvement methodology in order to standardize nurse handoff communication in order to improve patient safety, increase patient and family involvement, and decrease end-ofshift overtime. Continuous process improvement methodology (CPI) consists of discipline, daily HANDOFF COMMUNICATION 8 practices, and tools that will help to establish and maintain improvement (Klee et al, 2012). By the completion of the study 93% of nurses followed the standardized handoff sequence. Standard nursing handoff communication will be given at the bedside. Nurses should involve patients in the handoff report whenever possible. Nursing practice council will work together to develop a standardized shift report form. Some forms may need to be specialized to meet the needs of different departments, such as postpartum units. Each unit will have a standardized report form to be utilized at each patient handoff. The handoff form will be utilized in order to give report in a consistent ordering. Furthermore, nurses will fill out handoff sheets before change of shift communication and give the report form to the oncoming nurse. Nurses will also have the electronic medical record open during handoff report. After development of a standardized handoff report form and implementation of bedside report, nursing staff will participate in simulation exercises to practice proper handoff communication. Nursing staff satisfaction with the perceived effectiveness of the new handoff report form and format. Errors in-patient care and sentinel event rates will then be compared to previous rates in order to determine if errors have been reduced. Implementation Plan Implementation of standardized handoff communication tool and format will take place over one year. Beginning January 2015 observation of nurses’ handoff communication as well as data collection. After 2 months of data collection a handoff communication checklist and communication tool will be developed. Beginning May 2015 mandatory bedside report will be strictly enforced. In June, nurses will begin reviewing new handoff documentation. After time for nurses to review, simulation will begin at the August. Nurses will participate in an in-service simulation in order to practice the shift handoff reports. Finally at the beginning of October, the HANDOFF COMMUNICATION 9 new handoff communication format will take full effect and should be strictly enforced by December. Over the next year errors in patient care should be analyzed in order to determine if they were caused by the handoff communication. The effectiveness of the standardized format will then be evaluated. A timeline of the stated plan is outlined in figure IV. Jan Feb March April May June July Aug Sept Oct Nov Dec Data Collection Checklist Development Mandatory Bedside Report Review of Handoff Documents In-service Simulation Implementation and begin of longitudinal review Figure IV. HANDOFF COMMUNICATION 10 Evaluation In examining the effectiveness of the new standardized handoff communication tool and format nurses will initially be observed during an in service simulation. The simulation will work both to allow nurses to practice the standardized handoff format as well as to allow for observation. Following simulation and implementation of the new handoff format nurses will be observed on the unit by a trained observer. Observations will be recorded and compared with documentation taken during pre intervention observations. In examining the effectiveness of handoff communication in preventing errors in patient care, it is necessary to examine the cause of errors both before the implementation as well as after. The new handoff communication tool and format will be shown to be effective if there is a decrease in errors in patient care, especially sentinel events, following implementation. The difference in rates of adverse patient events will be assessed for a minimum of one year following the final implementation phase. Finally a survey of experienced nursing staff will be given in order to determine nurse perception of new handoff communication format and decipher any necessary adjustments. The survey will seek to determine nursing satisfaction as well as the nurses’ perception of the effectiveness of bedside report in enhancing nurse/patient relationships. HANDOFF COMMUNICATION 11 References Berkenstadt, H., Haviv, Y., Tuval, A., Shemesh, Y., Megrill, A., Perry, A., & ... Ziv, A. (2008). Improving Handoff Communications in Critical Care Utilizing Simulation-Based Training Toward Process Improvement in Managing Patient Risk. Chest, 134(1), 158162. doi:10.1378/chest.08-0914 Evans, D., Grunawait, J., McClish, D., Wood, W., & Friese, C. R. (2012). Bedside Shift-to-Shift Nursing Report: Implementation and Outcomes. MEDSURG Nursing, 21(5), 281-292. Joint Commission on Accreditation of Healthcare, 2005 Joint Commission on Accreditation of Healthcare. (2005). Improving America's Hospitals, A Report on Quality and Safety, (pp. 1--139). Retrieved from www.Jointcommissionreport.org Klee, K., Latta, L., Davis-Kirsch, S., & Pecchia, M. (2012). Using Continuous Process Improvement Methodology to Standardize Nursing Handoff Communication. Journal Of Pediatric Nursing, 27(2), 168-173. doi:10.1016/j.pedn.2011.08.005 Radtke, K. (2013). Improving patient satisfaction with nursing communication using bedside shift report. Clinical Nurse Specialist: The Journal For Advanced Nursing Practice, 27(1), 19-25. doi:10.1097/NUR.0b013e3182777011 World Health Organization, (2007). Communication During Patient Handovers. Retrieved from http://www.who.int/patientsafety/solutions/patientsafety/PS-Solution3.pdf