Introduction to Safer Sign Out
advertisement

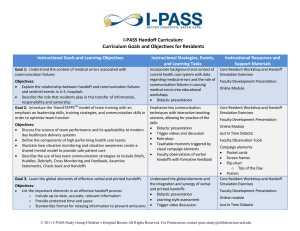
Safer Sign Out Physician Handoff Communication Achieving High Reliability Through Patient-Centered, Team-Based Innovation v5 Drew C. Fuller, MD, MPH, FACEP Board of Directors / Education Committee Past Chair, Quality Improvement & Patient Safety Section (QIPS) (Synergy Interest) Director of Safety Innovation Safer Sign Out • Patient Centered • Team Based • Risk-Focused • Physician (Frontline) Developed • Method for Structured Physician Handoffs National Patient Safety Goal 2E (2006) Standardization of Handoff Communication “Sign out is the most dangerous procedure in the Emergency Department” Charles “Chaz” Schoenfeld, MD (1950-2010) Why Structure? • Up to 80% of serious medical errors involve miscommunication during handoffs (TJC) Up to 24% ED malpractice claims related to handoff (Cheung 2010) Progress • Nursing profession – Leading with Models/Methods • Few Physician Models Emergency Departments - High Risk ED Factors – Potentiate Errors • • • • • • • • • • • Production/Time Pressure High Noise Levels High Acuity Multitasking Time Sensitive Conditions Rapid Turnover Frequent Interruptions New/Unknown Patients Undifferentiated Diagnosis Wide Clinical Variation Increasing Complexity Handoffs - High Risk Points of Potential Failure • • • • • • Neglected/Missed Information Unclear Transfer of Responsibility Team Unaware of Transfer/Issues Patient/Family Unaware Change in Status Lack of Mechanism for QA Why Structure is Critical High Risk Process + High Risk Environment Mandates High Reliability High Reliability • Structured • Workable • Predictable • Measurable Industries Committing to High Reliability Pilots Committed to Standardized Communication “Quick” Handoff Practice (To view the video, click https://vimeo.com/68618147) Name that Handoff Hit & Run? “Typical” Handoff Practice (To view the video, click https://vimeo.com/68618456) Name that Handoff “Hopeful Handoff” What’s Missing? Typical ‘Hopeful’ Handoff • Critical items conveyed? • Safeguards? (Checklist?) • Current clinical status? • Patient aware/Involved? • Nurse aware/involved? • QA ? Hope Model for Safety • Hope nothing goes wrong • Safe By Luck or Design? • Unstructured – No Standard • Not High Reliability (High Vulnerability) • Poor Strategy for Safety Designing a Better Way • Focus on areas of RISK • Practical implementation • Scalable • WORK for Clinicians EMA Safety Leadership Group Physician Representation 12 Hospital/Clinical Sites: Maryland Virginia Washington, DC West Virginia American College of Emergency Physicians (ACEP) Quality Improvement & Patient Safety (QIPS) • White Paper on Improving Handoffs by Dickson Cheung, Jack Kelly et al • 20 National Clinical & Safety Experts • Recommendations for Best Practice Frontline Input • Sign Out Safety Survey • 104 ED Physicians & 50 PAs • Directors’ Guidance • ACEP QIPS leaders • Executive Input • Nursing Input & Feedback “The Essential Connections” Physician to Physician Patient/Family Nurse (Team) Key Components Safer Sign Out 1) Record - Critical Data & Pending Items 2) Review - Form & Computer Data 3) Round – Bedside, Together 4) Relay to the Team – Nurse Collaboration _____________________________________________________________________________________________________ 5) Receive Feedback – Clinical/QA Use a Recordable Form • Clear transfer of responsibility • Prompts to identify Key items • Checklist & Reference Tool Safer Sign Out Form (v16) Check if No Patients Signed Out Patient Name & Age Off-Going Clinician: _________________ Receiving Clinician: _________________ Date (Shift Started)___________ Problem List & Key Issues Diagnosis/CC: Room Key Issues: Pending Items Disposition Home__________ _______ __________________ Receiving Clinician’s Notes Rounded on Patient Included/Informed Nurse Admit__________ ______________ Transfer________ ______________ NH____________ Potential Safety Issues or Precautions? TBD___________ Diagnosis/CC: Room Key Issues: Home__________ _______ __________________ Rounded on Patient Included/Informed Nurse Admit__________ ______________ Transfer________ ______________ Potential Safety Issues or Precautions? NH____________ TBD___________ Diagnosis/CC: Room Key Issues: Home__________ _______ __________________ Rounded on Patient Included/Informed Nurse Admit__________ ______________ Transfer________ ______________ NH____________ Potential Safety Issues or Precautions? TBD___________ Diagnosis/CC: Room Key Issues: Home__________ _______ __________________ Admit__________ ______________ Transfer________ ______________ NH____________ Potential Safety Issues or Precautions? TBD___________ This form is a Quality Assurance Tool and is NOT part of the medical record Rounded on Patient Included/Informed Nurse Back of Sign Out Form (Reinforces Protocol) Safer Sign Out Success Patients to Sign Out It#is#recommended#to#Sign% out% ALL% patients% that% remain% in% the% department#including#admitted#patients#yet#to#have#admission#orders Key Components Best Practices 1. Record • Patient, Critical Details, Follow-up Items 1) Pre-Round (Off-going clinician) Informing the patient prior to S.O. may help: · Better prepare the patient. · Increase efficiency · Save your colleague’s time 2. Review · SSO Form & Computer/chart Data 2) Confirm Mutual Understanding 3. Round Together • Meet the Patient & Assure a Plan Complete the sign out with: “What Questions Do You Have?” 4. Relay to the Team • Confirm the Plan with the Nurse/Team 3) Minimize Interruptions 4) Establish a Reliable QA process 5. Receive Feedback • Use SSO Form for Clinical Follow-up & Process QA · Collect & review forms · Encourage Peer Coaching Credits: The Safer Sign Out process was originally developed by the Safety Leadership Group of Emergency Medicine Associates, PA, PC of Germantown, Maryland and will be advanced with the following innovation and research partners: ! ! ! ! ! ! (Safer Sign Out Form Back Page) Joint Focus - Form & Data • Done at a computer Access to lab/rad results • Assure Shared Understanding Purposeful time for Q & A Bedside Round - Together • Status -“Eyes on the patient” • Introduction/Update • Team Communication Communicate with the Nurse – Transition/Updates • Opportunity for input/feedback • Assures team understanding • Before, during or after rounds Form as a Feedback Tool • Clinical Follow Up • Quality Assurance Tool Quality Assurance ✔ ✔ Built-in tool to help with QA Initial Hospital Sites Initial SSO Development Team • • • • • • • • • • • • • • • • • Don Infeld, MD (EMA President) Jackie Pollock, CEO (EMA) Nicole Bergen, Dir. of Op. (EMA) Martin Brown, MD, CMO (EMA) John Schnabel, MD Chris Morrow, MD Tim Hsu, MD Richard Ferraro, MD Karla Lacayo, MD Cameron Cushing, MD Michael Kerr, MD Steven Smith, MD David Jacobs, MD Jennifer Abele, MD Drew White, MD, MBA Michael Silverman, MD Marney Treese, MD • • • • • • • • • • • • • • • • Justin Green, MD Napoleon Magpantay, MD Kurt Rodney, MD Sora Chung, MD Matt Sasser, MD Jon D’Souza, MD Todd Larson, MD Junior Williams, MD Larry Mack-Wilson, PA-C Eric Parvis, MD Chris Morrow, MD Kala Scoggin, PA-C Elizabeth Cook Drew Fuller, MD, MPH Kilole Kanno, MD Nadia Eltaki,MD Rapid Cycle Improvement What We Learned • Physician Champions (Key) • Ease of implementation • Educate & support • Initial resistance resolves • Use QA to sustain Engaging Physicians “Protect Your Patients, Support Your Colleagues” • Appeal to their interest • Performance => how it ’Occurs’ to them • Listen, support & reassure Understanding Adoption Readiness for Change “Start Where They Are” Physician Feedback “ This is so much better than what we use to do” “ I was initially resistant but now I get it” “I sleep better at night” Committed to Collaboration • Share the Process • Teach Others • Seek Understanding • Pursue Refinement • Regionally/Nationally Quality Improvement & Patient Safety Section Website First Featured Safety Project Emergency Medicine Patient Safety Foundation (EMPSF) • Voice for Safety in Emergency Medicine • National Collaborator • SSO Flagship Safety Tool • Dedicated SSO Website • Consultation Service SaferSignOut.com Toolkit (Web-based) • • • • • • Education Downloads Forms Posters Strategy/Best Practices Videos & More Logo AMA Handoff Resource Listing • Handoff Resource (RFS) • Description and links to SaferSignOut.com AMA Handoff Resource Listing • Handoff Resource (RFS) • Description and links to SaferSignOut.com Agency for Healthcare Research & Quality (List SaferSignOut.com as a Resource) SSO in the Press SSO in the Press ABEM MOC PI Tool • Help your physicians meet their MOC PI requirement • Easily Utilized • To be featured on ACEP’s Handoff education tool Collaborative Synergistic Innovation (CSI) • Model for Innovation • Open Resource • Clinician Driven • Best Practice Refinement • Supports Research, Distribution, Education Innovation Partners Leading the Way 1. 2. 3. 4. 5. Use EMPSF as a resource Enlist “Champions” Build the case for a structured method Launch as a Team based approach Monitor the process & give feedback Atul Gawande "Better is possible. It does not take genius. It takes diligence. It takes moral clarity. It takes ingenuity. And above all, it takes a willingness to try.” Make the Commitment 1963 Speech at NASA Throw Your Hat Over the Wall SSO “Stand Up for Safety” Video https://vimeo.com/65199210 We Stand Committed to Safety Further Information Dianne Vass Drew Fuller, MD, MPH, FACEP Executive Director Emergency Medicine Patient Safety Foundation (EMPSF) Folsom, California Director of Patient Innovation Emergency Medicine Associates, PA, PC Germantown, Maryland EMAOnline.com Dvass@EMPSF.org Drewfuller@mac.com