empowerment of the diabetic inpatient through - HPH
advertisement

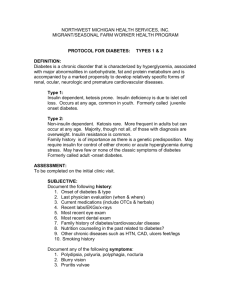
13th International Conference on Health Promoting Hospitals, “Empowering for Health: Practicing the Principles” Dublin, May 18-20, 2005 Virtual Proceedings EMPOWERMENT OF THE DIABETIC INPATIENT THROUGH NURSING CONSULTANCY Ganassi, Marco (nurse, Medicina 2), Manicardi, Enrica (physician, Medicina 2), Lince, Maria Paola (head nurse, Medicina 1), Dipartimento Medicina 1 Reference: Ganassi Marco, Ambulatorio diabetologico, Medicina 2, Dipartimento Area Medica 1°, Viale Risorgimento N° 80, 42100 Reggio Emilia, tel 0522-295913 fax: 0522 295896 ganassi.marco@asmn.re.it The prevalence of diabetes among adult inpatients is estimated to be between 12.4% and 25% , depending on the sensitivity of the method used to identify these patients (1). Diabetics who were unaware of their condition prior to hospitalization must also be added to these estimates (5), as well as patients with hyperglycemia secondary to hospitalization. Most diabetics are hospitalized due to a clinical problem that is either directly caused by their condition or is complicated by it, and the subsequent hyperglycemic state exposes these patients to an elevated risk of increased morbidity and mortality(6). A timely and aggressive correction of hyperglycemia improves hospitalization outcome and reduces mortality both in hospital and over the long term (2,3,6). The realization of this fact has increased interest in optimizing the management of hyperglycemia during hospitalization, leading to a need for health care standardization. Hospitalization provides the opportunity to evaluate the efficacy of patients’ self-management and can also be an important moment for the patients to learn ways to improve their future lifestyle; as all of their attention is focused on their health while in hospital, they fully appreciate the importance of this. All of the critical components of basic diabetology education – diet, insulin, drugs, glycemic monitoring, skin and feet care – can be transferred to the hospital care setting so that no opportunities for patient learning are missed. In those centers where the quality of diabetes management is a priority there is a willingness and an openness to educating patients on their disease; roles are clearly established and quality is monitored, with results confirming that educating inpatients correlates to earlier hospital discharge and better post-discharge outcome. In order to transform hospital care and improve glycemia management it is necessary to adopt a multi-level interdisciplinary approach, starting with protocols on the management of hyperglycemia by means of insulin that are developed by diabetologists and the specialists in the various operative units of the I.C.U. and the medical and surgical departments where a diabetic patient may be hospitalized; also needed are quality controls of glycemica performed on capillary blood and the standardization of patient education. In order to standardize the education of diabetic inpatients the position of a “diabetes nurse” was created in our hospital; the idea was that this nurse, after adequate in-depth training both in diabetes and in education methodology, would be able to carry out structured bedside instruction sessions aimed at giving the patient the skills necessary to ensure safe, risk-free hospital discharge. This instruction would also respect the exigencies dictated by costs based on the diagnosis-related group (DRG), case management, and other strategies aimed at containing costs and reducing the average length of hospital stays. The patients to receive instruction are identified by the medical and nursing staff of all the operative units; staff members request a consultation, either by telephone or by computer, based on the 1 13th International Conference on Health Promoting Hospitals, “Empowering for Health: Practicing the Principles” Dublin, May 18-20, 2005 Virtual Proceedings urgency of the need for instruction. First to receive instruction are those patients who are to be discharged after having started insulin therapy during hospitalization, and their family members. The instruction session takes about 90 minutes and begins with an evaluation of what the patient knows about his/ her disease, of his/ her psychomotor skills, and of his/ her practices relating to self-management and their impact on the reasons why the patient is presently hospitalized. The instruction session is tailored to the results of this initial evaluation, and the nurse adapts his or her speaking style and language to the patient’s ability to process the information provided. The nurse checks the patient’s real comprehension of this information at each phase of the session. The following topics are treated: 1) the correct technique to be used to perform insulin therapy with a pen (time of administration, posological correction based on current glycemic levels, site and correct technique to administer insulin); 2) the correct way to determine glycemia on capillary blood with reactive strips; 3) how to keep a glycemia diary; 4) what hypoglycemia is, how to recognize it, how to treat it, and how to prevent it; 5) what hyperglycemia is, how to recognize it, how to treat it, and how to prevent it; 6) the right diet for a diabetic patient. Immediately after having explained all of these points to the patient and given a step-by-step demonstration on how to take insulin and how to measure glycemia, the nurse-instructor then watches on as the patient goes through the same procedures in order to verify that the patient has indeed understood. After this the patient receives a “survival kit” made up of the material needed for self-management of the disease. There is enough material in the kit to last until the patient passes on to the Provincial Outpatient Diabetology Service; the kit includes information on how to get to the outpatient clinic, a learning evaluation test, and a discharge report that documents the instruction session. CONCLUSION: The presence of a “diabetes nurse” who can consult patients on their disease is an operative proposal whose objectives are to standardize the education of diabetic inpatients so that their discharge will be safe and risk-free and to provide the most urgently needed information to patients who have started insulin therapy while in hospital. Additional structured instruction concerning the complications of diabetes that can lead to hospitalization would also be beneficial and could rely on the full attention of those diabetic patients who are concerned about their health. This latter type of instruction requires not only a knowledge of diabetes but the collaboration of health care workers in all the operative units involved, where the experience here illustrated could be employed. 1. Clement S, Braithwaite SS, Magee MF, AhmannA, Smith EP, Schafer RG, Hirsch IB, American Diabetes Association Diabetes in Hospitals Writing Committee: Management of Diabetes and Hyperglycema in Hospital. Diabetes Care 27: 553 – 591, 2004 2. Malmberg K for the Digami Study Group: Prospective randomised study Group: Prospective randomized study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus BMJ 314: 1512 – 1515, 1997 3. Melin J, Hellberg L, Larsson E, Zezina L, Fellstrom N: Prespective effect of insulin on ischemic renal injury in diabetes mellitus Kidney Intern 61: 1383 – 1392, 2002 2 13th International Conference on Health Promoting Hospitals, “Empowering for Health: Practicing the Principles” Dublin, May 18-20, 2005 Virtual Proceedings 4. Szabo Z, Hakanson E, Svedjeholm R: Early postoperative outcome and medium – term survival in 540 diabetic and 2239 nondiabetic patients undergoing coronary artery bypass grafting Ann Thorac Surg 74: 712 – 719, 2002 5. Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE: Hyperglycemia: an indipendent marker of in hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab 87: 978 –982, 2002 6. Van den Berghe G, Wouters P,Weekers F, Verwaest C, Bruyninckx F,Schetz M, Vlasselaers D,Ferdinande P, Lauwers P, Bouillon R: Intensive insulin therapy in critically ill patients N Engl J Med 345: 1359 – 1367, 2001 3