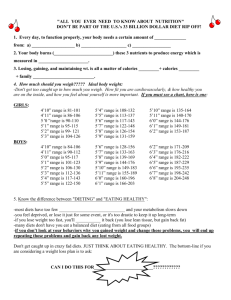
DIETARY TREATMENT OF OBESITY
advertisement

DIETARY TREATMENT OF OBESITY Chapter 18 - Johanna T Dwyer, DSc, RD and Kathleen J Melanson, PhD,RD,LD September 24, 2002 INTRODUCTION There is a great deal of misinformation about weight control in this country today. Self-initiated approaches to weight reduction are often not effective . People often believe that there is a quick and easy remedy for curing obesity. In fact there is no easy way. The only way to keep off excess weight is through lifelong behaviors involving physical activity, balanced with a healthy diet. [1]However, health professionals can help people be more effective at doing this. Obesity is gradually gaining recognition as a chronic medical condition requiring long-term or life-long therapy to achieve improved health outcomes [1, 2]. Health professionals often ignore obesity because they regard it as being unlikely to improve with therapy. However, recent data indicate that that modest (5-10%) weight reduction in obese persons are attainable and result in clinical improvements of several health-related parameters, even if the individual remains clinically obese [35]. These results should be encouraging to health professionals and patients, since now they need not be overwhelmed by the inability to meet excessively ambitious or unrealistic weight loss goals [3]. Weight management counseling of overweight and obese patients deserves reconsideration because it carries a great potential for health benefits. Obese patients receiving weight reduction advice from their physicians are significantly more likely to embark on weight loss attempts than those who do not, and yet in recent surveys only 42% of obese individuals reported that they received weight loss recommendations from their physicians[6] This finding underscores the need for increased physician and health professional involvement in obesity treatment [2, 7]. When physicians are appropriately trained and include recommendations for lifestyle changes when counseling their obese patients, results are promising [8, 9]. This chapter briefly reviews steps health professionals can take to help their patients manage their weight more effectively. RATIONALE FOR DIETARY TREATMENT OF OBESITY The growing propensity to overweight in the United States indicates that attention to weight control and maintenance are not matters that should be confined to those who are already overweight. Weight control has health advantages, and therefore maintaining or achieving a healthy weight is important for all Americans. In weight control, an ounce of prevention is worth a pound of cure. Once weight has surpassed healthy levels it is difficult to reduce it. Therefore it is important for health professionals to monitor the weights of all their patients and to provide anticipatory guidance so that those who are already at healthy weights remain so. The Dietary Guidelines for Americans stress aiming for a healthy weight and physically active life as the foundation of a healthy lifestyle [10].One simple tool for doing so is by keeping a record of body mass index (BMI). Increases of more than a BMI unit signal the need for instituting preventive measures. Assess Body Fat Burden and Health Status Before any patient is placed on a reducing diet, medical assessment of his weight, fat distribution and health risks is essential. Measure Body Mass Index as an indirect measure of body fat burden Weight should be measured without clothing on an electronic scales, which provides accurate weights even for heavy patients. Height is best measured with a wallmounted stadiometer. Body fat is difficult to measure directly in office practice, so the body mass index (BMI), which provides a better measure of fatness than weight alone, is calculated. The following formula is used: BMI= (wt, pounds x 703)/height, inches squared Table 1 presents classifications of BMI scores for adults. The higher the BMI, the higher the health risk. Individuals over BMI 25 are considered overweight, those over BMI 30 are classified as class 1 obesity, those over BMI 35 as class 2 obesity, and those over BMI 50 as extreme obesity. Table 1. Classification of Weight Status by Body Mass Index (BMI) Classification BMI (Kg/m2) Underweight <18.5 Normal weight 18.5-24.9 Overweight 25-29.9 Obesity Class 1 30-34.9 Obesity Class 2 35-39.9 Extreme Obesity Class 3 >40 Measure waist circumference to quantify risks related to body fat distribution The distribution of fat on the body as well as its sheer amount also alters risk. Excess abdominal fat in the viscera, characterized by an accumulation of fat centrally (sometimes referred to as android "apple" or abdominal fat distribution) is associated with greater risk than a peripheral fat deposition pattern (gynoid "pear" or lower body fat pattern). Abdominal visceral fatness is difficult to measure directly in office practice, but the waist circumference, taken at the level of the umbilicus with a plastic measuring tape, is a reasonable proxy for assessing it. The cut points for increased risk are a waist circumference of greater than 35 inches in women or greater than 40 inches in men. Table 2 shows how risks of weight related conditions such as type 2 diabetes, hypertension, and cardiovascular disease increase with greater BMI and waist circumference. Patients at high risk need increased treatment and monitoring of blood pressure, blood cholesterol and other cardiovascular risk factors. Two other factors that increase risk still further are physical inactivity, which exacerbates the severity of the other risk factors that are present as well as possibly increasing risks itself, and elevated serum triglycerides, which are another marker for increased cardiovascular risk. Although weight loss can help to lower elevated blood pressure, blood glucose, total and LDL cholesterol and triglyceride levels, and raises low HDL levels in those with abnormal values, additional pharmacologic therapy may also be necessary. Table 2. Classification of Risk of Type 2 Diabetes, Hypertension and Cardiovascular Disease Associated with Weight Classification of Fatness Increase in Disease Risk for Type 2 Diabetes, Status by BMI and Waist Hypertension and Cardiovascular Disease Over Normal Circumference Weight and Waist Circumference Waist circumference Waist circumference Women <35 inches Women >35 inches Men < 40 inches Men > 40 inches Underweight (BMI <18.5) Normal (BMI (18.5-24.9) Overweight 29.9) (BMI 25- Increased High Obese Class 1 (BMI 30- High 34.9) Very high Obese Class 2 (BMI 35- Very high 39.9) Very high Extreme Obesity Class 3 Extremely high (BMI >40) Extremely high Document other risk factors and comorbidities that increase risk and have other implications for therapy The presence of other risk factors or clinically evident diseases further increases the health risk of obesity. Table 3 lists the major signs, symptoms and conditions that must be considered. These conditions further add to the adverse health effects of the obesity and also are problems that must be managed themselves in addition to weight control. Table 3. Risk Factors and Comorbidities that Increase the Risks of Overweight Level of Risk Conditions High Absolute Risk Established coronary heart disease or other atherosclerotic disease Type 2 diabetes Sleep Apnea High absolute Risk if 3 or More of These Hypertension Risk Factors are Present Cigarette smoking High low-density lipoprotein cholesterol Low high density lipoprotein cholesterol Impaired fasting glucose Family history of early cardiovascular disease Age: >45 in men or >55 in women Increased Risk Osteoarthritis Gallstones Stress incontinence Gynecologic problems such amenorrhea and menorrhagia as Determine if the patient is a candidate for weight loss All individuals with a BMI over 25 and those at lower BMI's with high waist circumferences and two or more of the risk factors listed in Table 3 are potential candidates for weight reduction. The goal is reduction and maintenance of a lower body weight over the long term. It this is impossible at least prevention of further weight gain should be attempted. Assess the patient's readiness and willingness to lose weight Unfortunately those who are most concerned about their weights are not necessarily those who are at the highest health risk. The procedures described above provide a reasonable assessment of the health risks associated with obesity and the potential health benefits accruing from weight loss. Now these risks need to be communicated to the patient. Those who are at high health risk are often unaware of how serious their problems are. Once this has been done, a plan for dealing with the condition needs to be jointly devised with the patient. Weight control requires behavioral change and requires patient consent and "buy-in". Therefore patient readiness needs to be ascertained. Some patients are ready to start a treatment program immediately. Others are unable or unwilling to embark on a weight reduction program, but they are willing to take steps to avoid further weight gain or perhaps to work on other risk factors such as cigarette smoking, and they should be encouraged to do so. For those not ready to act, the issue should be deferred and brought up at the next visit. Other normal weight patients who wish to control their weight may also ask for help. They can be counseled to avoid weight gain and provided with helpful information on healthy eating and physical activity levels, which is summarized at the end of the chapter. Decide if Dietary Treatment is the Appropriate Option Weight reduction with dietary treatment is in order for virtually all patients with a BMI 25-30 who have comorbidities and for all patients over BMI 30. Prescription drugs may also be considered for those with a BMI of 27-30 if comorbidities are present, and for heavier patients even in their absence if they are unable to lose weight with dietary measures alone. Only two prescription drugs are currently approved for long-term use in weight reduction. Sibutramine (Meridia) is an appetite suppressant that works centrally to decrease appetite. Its advantages include slightly greater net weight losses and longer maintenance of losses than diet and physical activity alone. Disadvantages include variable increases in blood pressure and cost. Orlistat (Xenical) is a drug that operates at the level of the gut to inhibit pancreatic lipase and fat absorption. It also increases net weight losses, at least over the short run compared to diet alone. It also may foster adherence to low-fat reducing diets because of the fat malabsorption it induces. Its disadvantages are malabsorption sometimes, accompanied by anal leaks, and decreased absorption of fat-soluble vitamins. Dietetic counseling is helpful in managing the drug's effects. The drugs are costly. Patients who are likely to respond to drugs do so within the first month of therapy and if they fail to lose about 5lb in the first month, the drug is unlikely to be effective. Surgical options such as gastric bypass and gastroplasty are recommended only for patients with BMI 35 with comorbidities and are beyond the scope of this chapter. Clarify Reasonable Goals and Define Successful Outcomes for Weight Reduction, Set a "Healthier weight" target for the patient The approach to setting goals and treating [11] obese patients must be non-judgmental and focused on an acceptable weight for good health outcomes rather than solely on body weight [12]. Everyone wants to be healthy. By concentrating on improving health and risk factors, rather than simply on loss of weight, excessive focus on the aesthetic and cosmetic aspects of weight can be avoided[13]. Begin therapy by working with the patient to set a healthier weight. From the medical perspective, the goal is to maximize health related effects while minimizing insults to the patient's quality of life. The physician is uniquely qualified to define and communicate what a "healthier " weight is to the patient since weight reduction targets vary depending on the patient's weight and comorbidities. Progress toward healthier weight goals should involve a gradualist approach that minimizes health risks that is timed to patient readiness and motivations and that provides reachable short-term targets. A reasonable target: 10% of body weight over about 6 months The target is usually to achieve a loss of about 10 percent of body weight over a period of six months, and to keep weight at this lower level thereafter. It is moderate enough to be achievable and reduces fat and weight enough to decrease obesityrelated risk factors. After about 6 months most patients have difficulty-sustaining adherence, and weight plateaus as resting metabolic rate and energy output decrease. This target can be achieved with a caloric deficit of 500-1000 Calories a day or 1-2lb a week. A weight reduction plan of about 1000-1200 Calories for women or 12001600 Calories for men along with increased physical activity and behavioral modification will usually produce this. With a caloric deficit of 500-1000 Calories a day after 6 months with perfect adherence losses would theoretically be between 26 and 52 pounds, but in actuality losses are usually about 20-25 pounds, since adherence is never perfect. A BMI unit is approximately 10-15 pounds depending on height and weight and a decrease in 2 BMI units over 6 months is another way of starting the goal. Reductions of this magnitude decrease risk factors and thus result in "healthier" weights. If further weight reduction is necessary after 10% of body weight is lost, it can be attempted after weight has been maintained for several months at a healthier level. Adopt realistic goals that include health objectives Many overweight patients have already tried in the past to lose on their own. For example, in the United States nearly half of women, and more than a third of men report that they are attempting to lose weight [11]. However, with self-directed efforts, their reasons are often aesthetic or social rather than health-related, the goals they adopt are often unrealistically ambitious, the information they obtain on weight management is often inaccurate, and the support their receive is frequently inadequate. Solo efforts may fail and lead to discouragement and a sense of futility[14]. The vital role of the physician is to provide the motivation, information, counseling and support patients need to be more successful. Patient weight goals are often very different from those of their healthcare providers. In general, patient's ideal for weight reduction are two or three times the 8-15% losses that motivated patients usually achieve [15]. Patient weight goals depend on their motivation, the salience of weight as an issue to them, their perception of health risk, and other priorities in their lives. Some patients simply are not motivated to lose weight, or are motivated but are not willing to do so at present. It makes no sense to give an unmotivated patient a goal he cannot achieve. It is far better to come to agreement about the steps he/she is willing to take now to begin to deal with their health problems. For patients who are already highly motivated or become so when they are told about the related health risks, the physician's job is easier. These patients' weight targets are often unrealistically low (e.g. targets of 30% or more of body weight) and their time frames for achieving losses unrealistically short (e.g. weeks rather than months). For them, advice and counseling on more realistic targets and time frames is helpful. Patients are often unreasonably hard on themselves and believe that if they are to undertake weight reduction, drastic measures are called for. A healthy weight goal consisting of an initial loss of 1-2 BMI units is often much less extreme than the weight loss patients think of as ideal, but it is much more likely to be achievable. A loss of 10% of body weight, if sustained, significantly reduce risks for coronary heart disease and other comorbidities. The physician plays an important role by giving patients permission to adopt more realistic and achievable targets. Define Success in Broader Terms than Weight Loss Alone Definitions of the success are patient-specific. The reduction of risk factors, even if weight is not lost, is "success" from the health standpoint. For some patients, prevention of further weight gain after years of slow, steady increase is progress. The maintenance of a reduced weight, even if it is still within the range of clinically defined obesity is also "success" since it reduces health risks. Thus the definition of successful obesity treatment must be broadened to encompass goals other than weight loss, and these broader goals need to be communicated to patients. For example, outcomes to target may include improved metabolic profiles, reduced blood pressure, fasting blood lipids or glucose, increased daily physical activity and fitness, greater consumption of fruits, vegetables and fiber, reduction in dietary fat, changes in specific unhealthful habits as well as enhanced self-esteem, self-efficacy, quality of life and functional capacity [1, 16]. Individualize the Diet and Treatment Program Evidence-based reviews of successful weight control techniques increasingly emphasize the importance of individualized, multidisciplinary care, a health-outcomes focus, realistic goal setting and making permanent lifestyle change[5]. The specific underlying factors that induce a chronically positive energy balance and thus the development of obesity differ among individuals. Furthermore, daily lifestyle, environment, resources and social situations may vary considerably. Thus, it is appropriate to individualize the weight reduction strategy in order to promote adherence , and thus success [16]. Different specific dietary approaches for maximizing adherence are successful to varying degrees in different individuals. No single approach is appropriate for everyone, and so those who are embarking on diets should discuss the approach that best suits their needs with their physician and/or dietitian. In addition to energy content, individual food selections and meal frequency, other factors that may make a diet suit the individual. These include cost, convenience, treatment of co-existing health conditions, strategies for adapting the reducing diet to different social situations and a continued plan for healthful life-long weight maintenance [17]. Throughout the weight loss and management program, it is vital that the patient be counseled on making proper dietary choices, thus allowing for independence and self-efficacy in forming daily eating patterns. Representative dietary education topics are listed in Table 4 The National Institutes of Health, the American Dietetic Association and other organizations provide materials, checklists, guidelines, menus and recipes to assist in such patient education [5, 16]. Patients should be encouraged to maintain daily records of food and beverage intake, since this often increases awareness of consumption, and promotes dietary adherence. Table 4. Nutrition Education Topics for Weight Management Energy values of different foods Food composition (fats, CHO, fiber, protein) Reading nutrition labels The Dietary Guidelines for Americans Standard portion sizes compared to portions usually eaten Usual portions and calories in commonly consumed fast foods New habits of food purchasing Food preparation for healthier intake Avoiding overconsumption of foods with high energy content and density Adequate water intake Portion size reduction Limiting alcohol consumption Eating strategies for restaurants and social situations Awareness of physiological hunger and satiety cues Awareness of physical activity levels (use of pedometer and activity diaries may help) Adapted from NIH Obesity Guidelines 1998 PLAN THE ENERGY DEFICIT GENERAL PRINCIPLES PHASE OF WEIGHT CONTROL For the individual who is already overweight, successful weight control requires a phase in which dietary energy intake is reduced while energy output is increased or at least not decreased. This phase is referred to as the energy deficit phase. The essential components of weight reduction are decreased energy intake, increased energy output through physical activity, behavioral modification of lifestyles, and alterations in the larger environment that foster these measures. Although this chapter focuses on dietary measures in the treatment of obesity, all reasonable treatment programs for overweight should include the full complement of these measures. CALORIC DEFICIT NEEDED TO LOSE WEIGHT Obesity results from the accumulation of excessive body fat as adipose tissue. Numerous experimental studies under controlled conditions have established that it takes approximately 3500 Calories for an overweight person to lose a pound of fat. Although compensatory changes in resting metabolism, the energy cost of work, and discretionary physical activity may occur that sometimes alter this figure by 100-200 Calories, over the long term this relationship holds quite well. Thus the size of the energy deficit between actual energy needs and the energy output determines the slope of decline in fatness over time. GOAL OF ENERGY DEFICIT PHASE The goal of the dietary treatment of obesity in the energy deficit phase is to decrease body fat stores without unduly depleting the lean body cell mass that includes skeletal muscle and the vital organs. During weight loss some lean tissue is always lost along with the fat. While weight is being lost, stores of other nutrients such as vitamins, minerals and electrolytes must be maintained. Fortunately, dietary and other strategies are available to minimize loss of lean tissue and other nutrients, and these must be incorporated into sound dietary treatment plans. TROUBLESHOOTING WHEN DIETS DON'T SEEM TO WORK Some of the money factors that contribute to patients losing less weight than they expect to while on reducing regimes are described below. 1. Food intake varies greatly from day to day. People vary in their eating patterns from day to day. Weight reduction prescriptions are sometimes made by suggesting a caloric deficit of approximately 500 Calories per day to achieve a weight loss of about a pound a week. This is an abstract goal that is difficult to remember. However, since most people vary greatly in their food intake from day to day, they have great difficulty recognizing whether in fact they are eating less than before. For this reason simply urging people to "eat less" of certain foods is unlikely to help. 2. Self -reports of energy intake are underestimated. The average healthy adult American male consumes approximately 2800 Calories per day, and the average female about 1800 Calories, yet such intakes are seldom actually reported. The reporting of energy intakes is difficult even for individuals who have been trained to report accurately. Many days of observation are necessary since energy balance is only achieved over weeks, not days. Thus a report from any given day is certain to contain considerable random error if it is used to estimate usual caloric intake. However, more serious errors also are present. Underreporting of energy intakes is common and large (e.g. 20%) in virtually all people, and it is particularly common among the overweight. Recent studies with objective biomarkers of energy output such as doubly labeled water indicate that underreports may be as great as 1200 Calories per day in obese persons [18]. Indeed, subjective reports of energy intake are often so low that those who report them should be losing weight when in fact they are gaining. This is biologically implausible. A more common problem is that weight loss is less, not more than expected. This too is a result of underreporting. When overweight people report their intakes by recall they often underestimate their intakes by 30-40%. They are likely to make similar mistakes in underestimating their intakes on reducing diets because of difficulties in portion size judgment, forgetting, the social desirability of reporting adherence to the prescribed regime, and other factors. Thus on a 1200 Calorie diet actual consumption may approximate 1600 Calories . Methods for assisting dieters to decrease these errors include the use of household measures or weighing scales to determine amounts eaten more precisely, the use of food diaries to help in self-monitoring of food intake and making them more conscious of what they are eating, the use of portioncontrolled liquid meal replacements, frozen low calorie entrees, and other foods which are fixed in their portion sizes. Underreporting is especially pronounced in the severely obese, women, smokers, those of low educational and socioeconomic status [19]. Those who are under- reporters tend to be so consistently [18, 20]. Thus consistency in reporting does not necessarily mean that the report is accurate. In spite of these limitations, self-reports are useful to the patient and counselor for obtaining clues on dietary patterns and portion sizes that may be helpful in counseling the patient. However it is important to recognize their limitations 3. Self -reports of energy output are also underestimated. Self-reports of energy output as measured by physical activity questionnaires have also been validated using doubly labeled water methods. Lengthy questionnaires used for research purposes are quite good[21] However, the variability of most questionnaires of the type that are used clinically is high, and they are not accurate for individuals [22] . However, as is the case with dietary reports, they are still useful for self-monitoring but are inaccurate for prescribing or assessing energy intakes or outputs. Uniaxial accelerometers such as the Caltrac that measure the degree and intensity of movement in a vertical plane, or triaxial monitors like the Tracmore are more accurate and are now often used as selfmonitoring tools[23]. These are very helpful to some patients. 4. Compensatory decreases in energy output occur on most reducing diets, particularly if they are very restrictive in energy. As a rule of thumb, for every 500 Calorie deficit, compensatory decreases in energy output due to decreased resting metabolic rate, discretionary physical activity and the energy cost of work involving moving the body are approximately 165 Calories, leaving only 335 Calories that actually contribute to weight loss. Thus the caloric deficit again may prove to be less than anticipated and predicted weight loss is less than expected [24] Some data suggest that energy balance is more strongly defended during energy deprivation than it is during energy surplus, impeding weight loss to a greater extent than weight gain [25-27]. In part, these retarding effects weight loss may be due to alterations in resting metabolism and non-obligatory physical activity.. 5. Shifts in water balance obscure true decreases in body fat and overestimate fatrelated weight loss. Dramatic alterations in weight often occur on reducing diets, particularly in the first few weeks on a severely hypocaloric regime with deficits of 1000 Calories per day, and on ketogenic diets [28]. These fluid shifts are larger on some reducing diets than others, depending on their caloric level and macronutrient composition. They are also more apparent on hypocaloric regimes that are very low in carbohydrate (<100gm and especially <50 gm). Shifts in water balance may cause very dramatic deviations from a linear slope of weight loss. They may also result in very rapid weight accumulation over a few days during periods of non-adherence that result from storage of glycogen and water with carbohydrate refeeding. 6. Fat and weight loss do not always track over the short run. Over the long run, fat loss and weight loss parallel each other. But this is not necessarily true over the short run. The amount of weight that is lost over time , particularly over the short run of several days depends not only on the energy deficit from current needs but on adherence to the weight reduction plan, which is never perfect, and on shifts in water balance, which may be considerable over the short run. These shifts may accentuate or obscure the fat loss that is actually occurring. Such considerations, which are often unrecognized by patients make many skeptical about whether such predictions actually apply to them. 7. Non-adherence to reducing regimens also decreases both fat and weight loss. In addition to the physiological factors that have already been mentioned, many psychological and environmental factors also play a part in determining the degree of adherence to a reducing diet. The many factors involve are discussed at length elsewhere [29]. CALORIC LEVEL OF THE REDUCING DIET From the clinical standpoint, hypocaloric diets must be defined in terms of the energy needs of the individual, since it is the size of the energy deficit that will determine the physiological effects expected. Formulas for estimating energy needs of individuals are provided in Table 5. Table 5. Formulas for Estimating Energy Needs of Healthy Individuals Resting Metabolic Rate Males= 900+10 (body Females 800+7 (body weight, kg)=RMR weight, kg)= RMR Activity Factors for Estimating Energy Expenditure Due to Physical Activity Resting (sleep, Sedentary light Very Light Moderate Heavy activity (manual labor 7.0) Total Energy Sources:[24, 101, 102] Need= RMR reading) activity activity activity (activity 1.0 1.2 1.5 2.5 5.0 factor) The major determinants of weight loss on reducing diets is size of the actual, not the prescribed, caloric deficit. All diets that reduce caloric intake to about 1400-1500 calories in most adult Americans result in weight loss if they are adhered to, regardless of their macronutrient composition [30]. Therefore the caloric level of the diet requires attention first and foremost, and then other characteristics of the diet can be considered. Diets that reduce caloric intake result in weight loss. The optimal diet for weight loss of sedentary people in the absence of alterations in physical activity is one that provides roughly 1000 to 1600 Kcal/day, depending on sex , weight, and physical activity level, regardless of its macronutrient composition. Low calorie diets LCD (100-1200 Calories females, 1200-1600 Calories males) Low calorie diets of 1000-1200 Calories for women and 1200-1600 Calories per day for men are currently recommended by the National Institutes of Health for weight loss in most individuals [5]. The rationale is that on such regimens a deficit of approximately 500-1000 Calories per day will be created, which should result in slow, progressive weight loss of 1-2 pounds per week. The dietary composition is similar in macronutrients to that of the National Heart, Lung and Blood Institute's (NHLBI) Step 1 diet to decrease risks of high blood cholesterol and blood pressure. Two sample menus and other materials at 1200 and 1600 Calories and many aids to assist the physician are provided in the monograph [5]. It is important to recognize that when using fixed 1200 to 1600 Calorie reducing diet plans such as these that even with perfect adherence, individuals can be expected to vary greatly in their weight loss. This is because their resting energy needs and physical activity, and thus their energy outputs, often differ markedly. The National Institute of Health's Obesity Initiative recently sponsored an evidencebased review of low calorie diets. It found that on the average diets such as these reduced body weight by an average of 8% over 3-12 months of treatment, and that the losses were accompanied by decreases in abdominal fat, which is the type of adipose tissue deposition that is associated with highest chronic disease risk. However, no improvements were noted in cardio respiratory fitness as measured by VO2 max unless the dieters also increased their physical activity [1] 1. Dietetic Advice and Individualized Eating Plans Many physicians lack the time that obese patients require for successful weight control therapy. Referral for dietary counseling to a registered dietitian (RD) is useful for many patients who need to control their weights, particularly those who have comorbidities that also require medical nutritional therapy. a. Available programs. There are over 67,000 registered dietitians in the United States practicing in hospitals, health centers and the community. Registered dietitians accept patient referrals from physicians for a variety of health problems that require dietary modification. Some formal weight control programs staffed by dietitians are available in hospitals and health centers. Individual counseling is also available. b. Candidates. Patients who have many comorbidities requiring medical nutrition therapy or other medical or surgical intervention, those on multiple medications, and those with complex and involved health problems that have dietary implications do poorly on usual dietary advice of a general nature, are the prime candidates for dietetic therapy, Patients who have had poor outcomes in weight control efforts on their own , who have special dietary preferences (vegetarian, ethnic cuisines) and who need extensive education and assistance in implementing their eating plan are also particularly likely to benefit. c. Advantages. Registered dietitians are able to read and interpret medical records and are equipped to adapt weight loss prescriptions to the particular needs of patients. Their knowledge of food habits, food preparation, and food products on the market makes them a good resource for helping patients to adopt the general weight control prescription to the patient's particular circumstances. A particular advantage of dietetic involvement in patient care is that dietitians often work in medical settings, and have access to patient charts and other health professionals. Registered dietitians are helpful for dealing with patients on drug therapy or on high-risk weight loss strategies such as very low caloric diets and post gastric bypass counseling in collaboration with physicians. Some dietitians have advanced certification in weight management, and are especially well equipped to counsel patients with complex and involved medical problems. Some insurance companies and health maintenance organizations may pay for obesity treatment, when it is part of a larger therapeutic program for diabetes or some other conditions and is provided by a dietitian who is a certified Medicare provider by Medicare and. d. Disadvantages. The patient's out-of pocket costs for dietary counseling vary, depending on insurance coverage and comorbidities. e. Safety and Effectiveness of Therapy. Registered dietitians are health professionals who are licensed in most states and who have medical , legal and ethical obligations to their patients. Their education includes formal educational requirements of at least a baccalaureate degree, supervised clinical training and mandatory continuing education. Dietitians are trained to be conservative and to alert physicians when untoward events arise. Thus counseling tends to be safe. The effectiveness of dietetic counseling, like that of physician counseling for weight control, has seldom been evaluated. The American Dietetic Association, the dietetic professional association, is currently developing and testing clinical guidelines for weight reduction and management of various obesity-related conditions. 2. Commercial Weight Loss Programs Commercial nonmedical weight control programs are popular and widely available in the United States and Canada. a. Available programs. Commercial programs include large chains such as Weight Watchers, Jenny Craig, LA Weight Loss and many regional ventures. These programs vary, but generally include advice on a structured low calorie diet, exercise, lifestyle modification coupled with group support (Weight Watchers) and/or individual counseling (Jenny Craig). Usually the program is administered by a layperson trained by the program that is often a successful graduate. All of these programs are for profit entities and charge fees [31]. b. Candidates. Moderately obese persons with few risk factors and co-morbidities are good candidates for these programs. Those who find that they need continued motivation, monitoring and social support with a structured regimen may particularly benefit from the program. c. Appropriate Use. These programs are not substitutes for physician concern or monitoring of patients. The programs are not equipped to deal with patients with multiple and involved comorbidities of a medical or psychological nature. Those patients are better treated by a program and therapists that are more closely connected to the health care system, such as registered dietitians or weight control programs in medical facilities. d. Advantages. The major chains offer well crafted, nutritionally adequate and behaviorally sound programs that are reasonable therapies. Some concerns such as Weight Watchers also offer frozen entrees and other weight control products which can be purchased in supermarkets and that are keyed to the recommended eating plan, making adherence easier. Since 1997 most of the large commercial concerns have joined the Partnership for Healthy Weight Management, a voluntary association. Members provide, on a voluntary basis, publicly available information to help potential participants meet their needs. Criteria for membership require that concerns disclose staff qualifications and essential program components, the risks associated with overweight and obesity, other details about the provider's program or product, and program costs[32]. e. Disadvantages. Although a physician approval is required by most programs before participants can enroll, there is no guarantee of the quality of the health assessment that has been carried out. For some individuals, especially those at very high risk, more intensive medical supervision may be required. The cost of the programs is another obstacle. Many of the poor who are obese do not have the resources to purchase these services, even though they might benefit from them. Discounts or waivers of fees for those in financial hardship are rarely available. The companies have become more active in developing programs catering to those who have lost weight to help them maintain their losses in recent years, but incentives for staying in maintenance programs may still not be sufficient. f. Effectiveness and Safety. The major firms provide a program and products which are safe when directions are followed. However, in spite of the fact that millions of Americans have purchased these services, their effectiveness in bringing about weight loss or sustaining lower weights has rarely been studied. The sole exception is Weight Watchers, and even for it , large-scale studies of its efficacy are not available [33]. 3 .Formulas and Meal Replacements Many meal replacement and formula products for weight control are now available in supermarkets and drug stores that patients can purchase on their own. Unlike very low calorie diet formulas, which are medical foods that are usually provided as part of a medically supervised treatment program, such as HMR or Optifast, these products can be purchased by anyone. a. Available products. Meal replacements now include not only powders like Slimfast that are mixed with milk or other liquids, but drinks bars and frozen entrees . Formulations and nutrient content vary. Most liquid meal replacement products provide about 220 Calories per serving and are relatively high in protein, vitamins and minerals but low in fat. The health bars and frozen entrees vary in their caloric content, but are generally between 200-400 Calories and have a more complete profile of nutrients than most other single foods. The entrees, which include offerings such as Lean Cuisine, Healthy Choice, and Smart Ones (a product geared to the Weight Watchers program) all share characteristics such as discreet portion sizes that are relatively low in calories (usually 300 calories or less). Smart Ones is manufactured by HJ Heinz, which also operates the Weight Watchers commercial diet program. Its packages are prepared to fit into the food plans for the Weight Watchers program. All of the meal replacement products are designed to be eaten with additions of conventional foods that supply dietary fiber, other nutrients, additional calories and fluids. b. Candidates. Individuals who are healthy but moderately overweight (BMI 25-30) who wish to lose less than 5% of their body weight or who wish to use these products for one meal a day to assist in their weight maintenance efforts may find these products helpful. The products provide an easily prepared and relatively modest caloric load that slakes hunger. For those who are susceptible to environmental triggers (such as being involved in meal preparation , eating in cafeterias or fast food restaurants) and respond by overeating, these products offer a safe and palatable option. c. Appropriate use. Portion controlled liquid meal replacements such as Slim Fast (and many other products) are recommended for two meals and a snack with a small meal of conventional foods and low or no calorie beverages. The entree choices are suitable for lunches or dinners. d. Advantages. The main advantages of meal replacements are built-in portion and calorie control, widespread availability, convenience, composition that is fairly dense in other nutrients while remaining low in calories, ease of preparation, and, for some of the dry or canned products, portability. The meal replacements simplify food choice decisions. They are lower in calories than many snack foods that people eating away from home might substitute for them. Also they are convenient, rapidly and easily prepared options that can be eaten anywhere, allowing eaters to avoid "high risk" eating environments. e. Disadvantages. The major disadvantages of these products are their cost, monotony, low taste, and limited variety. From the nutritional standpoint, the products vary but are often quite high in sodium. Perhaps their major disadvantage is that they are ineffective unless they are used as part of an overall low calorie-eating plan. If they are used as sole sources of food they are nutritionally inadequate not only in energy but several other nutrients and water. f. Effectiveness and Safety. The major safety concern with these products, especially the formulas, is that some dieters will use them to create their own very low calorie diets and embark upon them without appropriate medical supervision. These products are nutritionally inadequate when they are used as sole sources of food and fluids. When the products are used according to directions on the label or in package inserts, they are safe. [34] When used as part of a weight loss program these single meal replacements are effective during the weight loss phase [35], and also when they are used for one meal or snack a day as adjunctive therapy during the weight maintenance phase [36]. The advantages may be due in part to easier control over portion size on meal replacements[37]. 4. Prepared Delivered Meals Commercial catering concerns in many parts of the country have begun to offer prepared, delivered meals that are appropriate for weight reduction programs. No large chain or franchise is currently providing such offerings. However in the late 1980's several major food companies attempted to provide a line of portion controlled meals that also incorporated nutrient profiles in line with the NIH's National Cholesterol Education Project's type 1 diet plan to assist individuals in controlling their weights and other chronic disease risk factors. One such effort which was particularly well evaluated was the Campbell Soup Company's Intelligent Cuisine line. This was a prescribed, portion-controlled line of foods constituting 1200-1400 Calories a day provided to dieters directly by mail. The products were to be used with additional foods such as fruits and vegetables, salads, and fluids that the dieter supplied himself. Marketing was done not to patients directly but to their physicians, who provided medical back up and additional reinforcement. Evaluations of the line were compared to self-selected diets of conventional foods. After 2.5 months, those on the portion controlled IQ diet had lost more weight (4.7 vs. 3.1 kg) than controls and a number of risk factors for chronic disease were also decreased [38]. Unfortunately, in spite of these positive findings, the business plan was not successful and the products are no longer sold on the market.. 5. Weight Loss Books and Manuals The quality of self-help books on weight control ranges from the sublime to the ridiculous. Among the better books currently on the market are the LEARN Program for Weight Management, which is a sound 15 week course that is usually administered with in a treatment program [39]. The book is effective when it is part of the treatment program. However, the charges for such a program are considerable and the program is not available in all parts of the country, and the effectiveness of self directed efforts using the book by itself has not been evaluated. 6. Web-Based Treatment Programs and Resources The internet provides some excellent resources for those who want and need more information. a. Programs available. Two types of programs are available; those that primarily provide information and others that actually counsel the individual and provide low calorie diets and other advice. Sound internet resources that can help those who are trying to control their weights are listed in Table 6. The surfer needs to beware that not all sites proffering advice and information are sound. It is best to trust the sites sponsored by government, professional and voluntary associations with some standing and expertise in the weight control field. Table 6. Internet Resources for Weight Control Type of Site and Name Internet address and Comments Advice and Information on nutrition and weight control American Dietetic Association http://www.eatright.org/ Shape Up! America http://www.shapeup.org/ American Obesity Association http://www.obesity.org/ National Institutes of Health http://www.nutrition.gov/ Web-Based Aids for Dieters Cyberdiet.com http://www.cyberdiet.com/ Access is free, and e-counseling is $30 plus $10 per month thorough www. Diet-watch.com by a registered dietitian. Free website includes nutritional profiles to calculate target calorie levels and a food planner to choose meals, with a shopping list, and a chat room. WebMD Nutrition Resources http://www.mywebmd.nutrition.com/ Provides a BMI calculator, calorie counter, fitness and diet journal, chat rooms and a large database, charts that can be personalized. Ediets.com http://www.ediets.com/ Provides a Pyramid based reducing diet and food list, fitness information, charts and dieting tools. Cost is currently $35 for the first 3 month and $10/month thereafter Weight Watchers Online http://www.weightwatchers.com/ Self-help version of Weight Watchers program provides a diet plan and fitness information with exercises. Cost is $29.95 per month for 3 months. A new entry into the weight loss arena in recent years is the web-based weight control program[40]. These resources include chat rooms, diet and exercise information, and often products that are for sale. For example, Nutritisystem.com requires the purchase of prepackaged foods. The e-diet.com website charges for a visit to its site, which provides shopping lists from which consumers self select foods, and also it provides general advice. These web-based commercial offerings vary in their quality, some are very good and others are not [41]. b. Candidates. Those who are moderately obese with few risk factors and who need additional support and information after they have been screened by a physician on weight reduction may find these resources useful. They are not freestanding and need to be administered in conjunction with some additional health and dietary counseling. c. Advantages. The internet is widely available at all times of the day or night, at low cost. d. Disadvantages. High-risk patients, especially those who lack economic resources, may attempt to use these sites for the primary treatment of their condition. Also, some sites provide inappropriate or wrong advice. There is little supervision or support of the dieter. e. Safety and Effectiveness. The safety and effectiveness of internet sites for weight reduction has not been established. At present, only recommended sites should be used. 7. Voluntary Self Help Programs Self-help programs led by laypersons are voluntary programs that charge very low or no fees. National organizations include TOPS (Take Off Pound Sensibly), OA (Overeaters Anonymous) and others. These programs are designed primarily to provide group support to those who have weight problems, rather than to provide and supervise weight reduction diets Very Low Calorie Diets (VLCD) <800 Calories ( often as low as 400-500 Calories) Any diet, regardless of its caloric level, that provides less than half of an individual's energy needs is a VLCD for that individual. Virtually all adults have energy needs that exceed 1000 Calories a day, and therefore any diet below 500 Calories, and for many individuals, diets below 800 calories are VLCD. But other regimens that are higher in Calories may also be VLCD using this same rule of thumb; for example, a 1200 Calorie diet prescribed to a man whose usual intake is 3000 Calories would also qualify as a VLCD. 1.Uses and Candidates for Therapy These diets are reserved for special uses and for individuals at high risk because of their potential for greater metabolic effects and the consequent need for more extensive medical monitoring. VLCD are often used when the health risks from obesity are particularly acute and threatening. Other individuals can usually reduce just as well on a LCD with less risk and discomfort. Individuals with BMI's >30 or those with lesser degrees of overweight but many comorbidities (BMI>27 with comorbidities) and who have failed to lose weight with more conservative approaches are candidates for therapy. Medical contraindications include recent myocardial infarction, cardiac conduction disorder, history of cardiovascular disease, renal or hepatic disease, cancer, type 1 diabetes and pregnancy. Behavioral contraindications to their use include bulimia nervosa, major depression, bipolar disorder, substance abuse, and acute psychiatric illness. The advantages of the VLCD for patients include a rapid improvement in blood pressure, blood glucose, serum lipids and often-psychological status. For those who require surgery, the rapid loss of weight may improve their surgical risks. 2. Formulations Available The hallmarks of the VLCD are their low calorie level and relatively high percent of protein (never less than 28% Calories and often much higher). Protein needs are elevated on VLCD because in the hypocaloric state the efficiency of protein utilization for maintaining the body's lean cell mass is lessened. Also, very heavy people who often are candidates for the therapy have a larger lean body mass as well as much more fat than their smaller peers, and even after adjustment for their greater fatness, total protein needs, which are most highly associated with the size of the lean body mass, are elevated. Therefore higher protein levels may help to preserve protein nutritional status. VLCD also have, relatively low carbohydrate levels, making them ketogenic, and extremely low fat content. Without special formulation or supplementation, the VLCD is inadequate in several vitamins and minerals, especially potassium, calcium, iron, zinc, vitamin B6, copper and possibly other nutrients. There are two major types of VLCD currently in use; commercial preparations and "home made" regimens. The commercial preparation include powdered products rich in egg or milk based proteins that are mixed with water and consumed 4-5 times daily. The commercial products must provide at least 70 gm by law and often contain much higher amounts of high quality protein (70-100 gm), 50-100 gm carbohydrate, and up to 15 gm fat per day, plus vitamins and minerals in amounts to meet the Recommended Dietary Allowances. These products are formulated under Food and Drug Administration regulatory specifications . These products are convenient and have a predictable and adequate composition when used as directed. Their major disadvantage compared to home preparations is their higher cost. The formulas or prepackaged meals are relatively choice-free and help dieters avoid contact with conventional foods, which in some cases may facilitate dietary adherence and remove temptation. Several commercial weight loss programs are available that provide an entire program of VLCD plus the other essential aspects of a sound weight control program, including dietetic advice, exercise, behavioral modification, and pre-and post VLCD phases provided with supervision. The choices include the programs of HMR (Health Management Resources) and Optifast (Novartis Nutrition). These programs employ health professionals who are trained in weight management and a structured program that encourages adherence. The major disadvantage is that they are expensive ($2500$3000) and costs may not be covered by health insurance. Also there is the uncertainty that weight which is lost will remain so over the long run. Therefore an investment of effort in long-term weight management is mandatory. The "home-made" VLCD regimens are sometimes referred to as protein sparing fasts, or protein sparing modified fasts (PSMF). They are usually based on lean meat, fish or poultry and a few other foods plus supplements of 2-3 gm potassium chloride and a multivitamin/multimineral supplement in amounts approximating the Recommended Dietary Allowances; without such supplementation they may be inadequate. When patients are provided with appropriate dietetic counseling, health supervision by a physician who is experienced in the use of VLCD, and other aspects of a complete weight reduction program, these formulations are also safe and generate rapid weight loss. The extremely hypocaloric versions of VLCDs which are also often low in carbohydrate and sodium promote a mild ketosis that gradually leads to a diuresis and rapid loss of weight in the first several days on the diet. 3.Use Evaluation of general health and cardiac status is important prior to the institution of VLCD. Physician monitoring during the regimen is also important. Many practitioners begin the regimen with a 2-4 week LCD phase to assess ability to comply with a restrictive regimen and to begin the weight loss process. This is followed by a 12-16 week VLCD phase; the regimen is limited to this amount of time to avoid excessive loss of lean tissue. The VLCD phase is followed by a 4-6 week refeeding phase of transitioning back to usual foods and gradually increasing caloric levels; this helps to avoid rapid weight changes due to refeeding with restoration of glycogen stores and shifts in water balance. The refeeding phase also provides a time for assisting the dieter to plan a maintenance diet on conventional foods and to solidify a physical activity schedule. VLCD are most effective when administered as part of a more general weight control program that includes physical activity, nutrition education, behavioral modification and attention to decreasing other risk factors. If additional weight loss is needed, it is recommended that several months elapse before another VLCD phase is instituted [42]. 3.Safety The VLCD induces semi-starvation, which has both benefits and risks to the patient. Occasionally, with inadequate commercial products, such as one sold in the 1970's consisting of hydrolyzed collagen, an incomplete protein, with inadequate amounts of electrolytes, vitamins and minerals, deaths occurred [43]. Today commercial products are better regulated and more nutritionally complete. However, they can still be misused. Some physiological effects are inevitable on VLCD. Mild ketosis increases risks of dehydration, although this can be avoided by ample fluid intake. Electrolyte imbalances may occur, and so may nutrient deficiencies if measures are not taken to prevent them on "home made" VLCD by used of appropriate supplements. Minor physiological problems that occur even with appropriate physician monitoring of cardiac and general health status include fatigue, dizziness (due to orthostatic hypotension), muscle cramps, gastrointestinal distress, and cold intolerance. The risk of gallstones is increased, and seems to be particularly high when weight loss is very rapid (e.g.>1.5 kg/week). 4. Effectiveness Because these VLCD diets are so low in energy, they usually produce a greater initial weight loss than LCD; usually 10-25% over 12-16 weeks of treatment in randomized studies. However, in comparisons of VLCD with energy levels of approximately 800 Calories versus diets at lower caloric levels of 400-500 Calories the lower VLCD did not necessarily result in greater weight loss, perhaps because compensatory reductions in resting energy expenditure, discretionary physical activity, and adherence on the lower calorie regimes thwarted weight loss[44] . There seems to be little difference in outcomes between commercial and homemade VLCD. The NIH expert panel review of existing studies found that preservation of weight loss over the long-term (e.g.> 1 year) was no different on VLCD from that of LCD since most patients gained back 30-50% of the lost weight. Therefore their long-term advantage in weight control is unclear. TOTAL FASTING Fasting is contraindicated for weight reduction because it causes excessive breakdown of lean tissue and ketosis. Also , compensatory changes in resting metabolism and physical activity on total fasts are profound. COMPOSITION OF THE REDUCING DIET The composition of the reducing diet influences the composition of the weight that is lost and nutritional status, and therefore it is also important. Several excellent overviews of some popular diets and of the basic principles that must be considered in weight control provide more information[17, 24, 30]. Dietary composition on reducing diets should be geared to decreasing risks for of nutrient inadequacy and diet-related chronic diseases, particularly cardiovascular disease. Accordingly, the diet should be adequate in nutrients, with ample intakes of vitamins and minerals , relatively low in fat, saturated fat, cholesterol and sodium, and high in both soluble and insoluble fiber [1]. Consumption of fruits, vegetables, whole grains, lean sources of protein and water should be encouraged, with emphasis on balance and moderation. Diets that promote extreme restriction or unusually high intakes of any macronutrient or food should be avoided. Recommendations for healthful composition of weight reducing diets are outlined in Table 7, and discussed further in this section. Table 7. Guidelines for Composition of Healthful Weight Control Plans Carbohydrate VLCD: ≥ LCD: ≥ 100g/day Protein VLCD: 1.5 g/kg Body Wt. (≥ 65-70 g/day) LCD: 1.0 g/kg Body Wt. Fat ≤ 30% dietary energy from total fat ≤ 10% saturated fat ≤ 10% polyunsaturated fat ≤ 15% monounsaturated fat Cholesterol ≤ 300 mg/day Fiber 20-30 g/day Water 8 glasses (~ 2 quarts or 2 liters) More needed with exercise and/or heat Vitamins/Minerals Supplements desireable on diets < 1200 kcal/day to levels specified in Dietary Reference Intakes, with special emphasis on iron, calcium and folic acid in women of reproductive age Sodium chloride ≤ 1000 mmol/day (approx. 6 g/day) Calcium 1000 - 1500 mg/day Alcohol Minimal to none MACRONUTRIENT DISTRIBUTION 50 g/day The macronutrient composition of the diet does not appear to play a major role in overall weight loss. However, there is one exception. Over the short term, low carbohydrate diets are ketogenic and cause a greater loss of body water than body fat (at least in the first few days on the diet). Water weight is regained when the diet ceases or carbohydrate levels increase. When any reducing diet is maintained over the long term, if it remains hypocaloric, it results in a loss of body fat. Because there is currently so much interest in the macronutrient composition of reducing diets, positive and negative aspects of the major variations are described below. With respect to weight loss, overweight individuals who consume moderate-fat, balanced nutrient weight loss diets (approximately 25% fat, 15% protein and 60% carbohydrate) lose weight because they consume fewer calories than they expend. There is some evidence that these diets may produce weight loss even when they are consumed ad libitum, but more research is necessary on this point, since it may be that other factors, such as variety or caloric density are more important. However, other diets also produce weight loss. Overweight people who consume low and very low fat diets lose weight, probably simply because they consume fewer calories. It is also possible that lifestyle factors play a part in this weight loss, including increased energy expenditure, decreased fat and energy intake or all of these maneuvers. It is less certain whether overweight persons who self- select high fat, low carbohydrate diets consume fewer calories and lose weight under free-living conditions, although under experimental conditions they do so. The nutritional adequacy of diets of different calorie levels and macronutrient composition for weight loss and weight maintenance varies. The lower the reducing diet is in calories, and the more unbalanced the macronutrient composition is from usual levels, the greater the risk of nutrient inadequacy. Moderate fat, balanced nutrient reduction diets are nutritionally adequate for the most part. Very low fat diets tend to be deficient in vitamins E, B12, calcium, iron and zinc. High fat, low carbohydrate diets are nutritionally inadequate and require supplementation to make them nutritionally adequate. The metabolic effects of various popular diets also differ considerably. In general, metabolic profiles with respect to blood pressure, blood lipids, blood sugar, and serum insulin improve with energy restriction and weight loss, regardless of the macronutrient composition of the diet. However, there are some differences. Moderate fat balanced nutrient reduction diets lower low-density lipoprotein (LDL) cholesterol, normalize plasma triglycerides, and normalize ratios of HDL/total cholesterol. High fat low carbohydrate diets result in ketosis. Low and very low fat diets (e.g. 15-20% of calories) reduce low-density lipoprotein (LDL) cholesterol, and after a transient rise in triglycerides may also decrease plasma triglyceride levels, depending on diet composition. Low carbohydrate diets (e.g. <100 gm carbohydrate) that result in weight loss may also cause a decrease in blood lipids, decreased blood glucose and insulin level, and decreased blood pressure. However they are often high in saturated and total fat and in cholesterol. They have the disadvantage of increasing uric acid and potential risk of gallstones. Moreover, they are ketogenic, and often cause signs and symptoms such as dizziness, halitosis, fatigue, weakness, hypotension and malaise. The proponents of various popular reducing diets in diet books each claim that their regimen is optimal for quality of life, but as yet there is little objective information on this point. Hunger and adherence may vary on the different diets, and also from one individual to the next, but again little objective evidence is available for comparing them. Many factors affect hunger, appetite and subsequent food intake, including interactions between physiological and non-physiological factors. There does not appear to be any one optimal diet for reducing hunger. Long-term compliance is likely to be a function of psychological issues rather than macronutrient composition itself. At present little is known about the nutritional or other characteristics of diets that maximize adherence. PROTEIN 1.Protein Needs During Weight Reduction The Recommended Dietary Allowance for protein is 0.8 gm/kg/day, but most Americans eat approximately 15% of their total caloric intakes from protein, or about 1.2 gm/kg per day. Protein requirements do not decline and may actually rise on hypocaloric diets, and especially on VLCDs, when protein needs sharply increase above the levels needed for energy balance. When energy intakes are insufficient, some amino acids are used to maintain blood glucose levels and others must be used for energy, so overall protein requirements increase [45]. Fortunately the hormonal milieu in hypocaloric states spares nitrogen and causes preferential use of fat for energy, but inevitably along with loss of adipose tissue some lean tissue and consequently some nitrogen is also lost. Losses of water, calcium, phosphorus, potassium, and vitamins follow the loss of lean tissue. Excess losses of lean body mass can be hazardous, affecting cardiovascular function, exercise tolerance, and possibly immune responses, and thus should be avoided. As a rule of thumb, a minimum of 65 to 70 gm of protein is needed daily. On a VLCD, 1.5 gm of high quality protein per kilogram of ideal body weight per day is desirable, with intakes no less than 65-70 gm daily . Intakes may need to be even higher if the dieter suffers from certain diseases or is physically stressed, since nitrogen losses may rise further in these states. On diets providing 600-1200 kcal per day, daily protein intake should be at least 1 gm per kg ideal body weight. Reducing diets over 1200 kcal per day should supply at least 0.8 gm protein per kg ideal body weight. Levels should remain this high after weight loss has stopped and maintenance has begun. 2. High Protein Weight Loss Diets High protein reducing diets are those that provide more than 1.6 gm/kg/ideal body weight per day. Self-prescribed high protein reducing diets varying in their composition from about 28-65% of energy, providing 71-162 gm of protein per day, are currently popular as a new strategy for losing weight. They are usually quite low in their carbohydrate content. Some are clearly ketogenic and severely limit carbohydrates to below 50 gm per day, such as the Doctor's Quick Weight Loss Diet[46] and Dr. Atkins' Diet Revolution[47]. Others are extremely high in protein , very low in carbohydrate and ketogenic but also very high in fat, such as Protein Power[48]. Two other high protein diets with enough carbohydrate so that they are not likely to be ketogenic areThe Zone [49], and Sugar Busters [50]. All of the high protein diets include elaborate instructions that prescribe strict, structured eating schedules, and involve limited food variety and dietary flexibility. The high protein diets that are ketogenic also induce quick initial weight loss because of their low caloric level, their diuretic effect owing to glycogen depletion, sodium and water loss, and possibly the loss of appetite that is associated with the ketosis. For some patients these constraints may help them to achieve and maintain low calorie intakes at least over the short run. A recent comparison of a low carbohydrate diet with a low fat diet in patients with severe obesity found that patients on the low carbohydrate diet lost more weight than patients on a calorie-restricted, fat-restricted diet, and had greater improvement in insulin sensitivity and triglyceride levels (Samaha, FF; Iqbal, N; Seshadri, P; Chicano, KL; Daily, DA; McGrory, J; Wiliams, T; Williams, M; Gracely, EJ; Stern L. A lowcarbohydrate as compared with a low-fat diet in severe obesity. N Engl J Med 348 20742081 2003). A second study also found a similarly greater weight loss using a low carbohydrate diet without adverse effects on lipids, glucose, or insulin ( Brehm, BJ; Seeley, RJ; Daniels, SR; D’Alessio, DA. A randomized trial comparing a very low carbohydrate diet and a calorie-restricted low fat diet on body weight and cardiovascular risk factors in healthy women. J Clin Endocrinol Metab 88 1617-1623 2003). Both diets are associated with reduced caloric consumption, of course. Popular high protein reducing regimens are not risk-free. . Many of these diets advocate very high intakes of protein from meat and other foods that are also often high in saturated fat, cholesterol and sodium while they are low in dietary fiber, potassium, calcium, and magnesium, increasing cardiovascular risk. The purine content of meat, poultry, seafood, egg, seeds and nuts is high and increases uric acid levels and risk of gout in susceptible persons. The high protein load may increase urinary calcium loss if it is not buffered [51]. In patients with diabetic nephropathy, very high protein diets may speed progression [52]. The extremely low carbohydrate diets also increase ketosis. Finally, and perhaps most important, there is no objective evidence that indicates that these diets promote greater weight loss or that the weight loss is better sustained later. There is only one study of ad libitum diets on fat loss that suggests such effects and the effects in that study may not have been due to the protein but rather to other aspects of the regimens that were being compared[53] For these and other reasons the American Heart Association does not recommend high protein diets, and cautions that if used at all, they be limited to a short period of time [54]. FAT 1. Fat Needs During Weight Reduction Even on reducing diets, needs for small amounts (e.g. 3-6 gm) of essential fatty acid (linoleic or arachidonic acid) are present, and some fat is also necessary as a carrier for the fat-soluble vitamins. Therefore the diet should not be devoid of fat. However, because fat is calorically dense, it is usually decreased to increase bulk and reduce energy. 2. Fat in reducing diets a. Moderate to low fat balanced deficit reducing diets. In general, levels of dietary fat, saturated fat, polyunsaturated fat, monounsaturated fat and cholesterol should follow guidelines from the American Heart Association on weight reduction diets. While lower levels may be appropriate in some cases, these levels amply meet requirements while supporting cardiovascular health [1]. Balanced deficit weight reduction diets that are moderate to low in fat (20-30% calories) are so called because maintain a reasonable balance between macronutrients similar to that recommended in the Food Group Pyramid and the Dietary Guidelines for Americans[55]. They tend to achieve most of the caloric deficit by reducing fat from the typical level in North American diets of about 34% or more of calories to 2030% fat, 15% protein, and 55-65% of calories from carbohydrates. Some examples of balanced-deficit diets are the Weight Watchers Diet (about 25% fat, 20% protein and 55% carbohydrate, with 26 gm dietary fiber), Jenny Craig, the National Cholesterol Education Program Step 1 diet (25% fat) , diets based on the Food Group Pyramid, the DASH diet, Shape Up and Drop 10 diet of Shape Up! America and the Nutrisystem diet. These dietary patterns have been extensively reviewed and appear to be optimal for weight reduction on low calorie diets for most individuals. 3. Very low fat reducing diets (<20% fat calories) Very low fat diets such as the Pritikin diet [56] and the Ornish diet [57], are advocated not only for weight reduction but also for improving cardiovascular risk profiles. The Ornish diet, which is very low in fat (13% of calories) and saturated fat, very high in carbohydrate (81% of calories) and very high in fiber (38 gm) with a program that includes nonsmoking, exercise and behavior modification was shown to reduce some cardiovascular risk factors in a limited long term study [58]. For those who can adhere to them they may be helpful. 4. High fat diets for weight reduction (55-65% fat) High fat reducing diets are usually also low or very low in carbohydrate (<200 gm carbohydrate per day). Some current examples include Dr. Atkins' Diet Revolution, [59]Dr. Atkins' New Diet Revolution[47], Protein Power[48], the Carbohydrate Addict's Diet[60], Dr. Bernstein's Diabetes Solution [61], Life Without Bread[62], and the Pennington Diet[63]. There is some evidence that free-living overweight people who self-select high fat low carbohydrate diets which they eat ad libitum consume fewer calories and lose weight. Also overweight people who consume such diets under experimental conditions lose weight.[30] When high fat low carbohydrate reducing diets are fed they also tend to cause ketosis. They may also result in decreased blood lipids, decreased blood glucose and insulin and decreased blood pressure, but only if weight is lost. Over the short term (a few days or a week) high fat, low carbohydrate, ketogenic diets cause a greater loss of body water than body fat, but water balance is restored when carbohydrate levels increase or when the diet ends. High fat, low carbohydrate diets are often nutritionally inadequate and require some supplementation. If such high fat levels are continued after weight is lost, they are likely to increase dietary risks for coronary artery disease. CARBOHYDRATES AND THE GLYCEMIC INDEX 1. Carbohydrate needs in weight reduction Carbohydrate needs are at least 50 gm per day. At least 100 gm carbohydrate, and preferably 55% or more of total energy intake should be provided for diets that are over 800 kcal per day. On reducing diets under experimental conditions with equicaloric reducing diets, both diets very high in sugars and diets very high in complex carbohydrates as starch have similar effects in bringing about weight loss [64]. However, from the practical standpoint, since many products that are high in sugar are also high in fat and calories, sugars are usually limited on reducing diets. 2. Low Carbohydrate diets (< 100 gm carbohydrate) Any diet under 100 gm carbohydrate per day and especially diets under 50 gm carbohydrate per day are ketogenic. This can become a problem on some popular diets that are very low in carbohydrates, such as Dr. Atkins' Diet Revolution, [59]Dr. Atkins' New Diet Revolution[47], Protein Power[48], the Carbohydrate Addict's Diet[60], Dr. Bernstein's Diabetes Solution [61], Life Without Bread[62], and the Pennington Diet[63].. Also, VLCDs containing fewer than 100 gm per day are ketogenic and may lead to excessive protein breakdown to maintain blood glucose levels unless protein intakes are increased. When the body must rely on degradation of protein's carbon skeletons to preserve blood glucose levels (via gluconeogenesis), the catabolism of the protein is accompanied by loss of water. For every gram of protein (or glycogen) that is broken down, 3 grams of water are released, causing rapid weight loss but also a state of relative dehydration [28]. Relative dehydration caused by ketosis and failure to drink adequate amounts of fluids is not only undesirable for health reasons, but it also does not address the primary purpose of the weight-reducing strategy, which is to decrease excess adipose tissue. 3. Low Glycemic Index diets The Glycemic Index (GI) is a dietary concept, originally developed for the therapy of diabetes, which has recently become popular in weight management.. The GI is a property that describes the blood glucose response resulting from consumption of a defined amount of carbohydrate (usually 50 grams) from a given food, relative to the same amount of carbohydrate from a control food (usually white bread)[65]. The basic premise is that more moderate blood glucose and metabolic responses will sustain satiety and energy balance to a greater extent than would larger metabolic shifts over the course of the day. One example of such a diet is "Sugar Busters" a popular book that advocates the use of a low GI, high fiber, high protein diet in weight reduction [50] . The problem is that the regimen is low in a number of nutrients, includes many odd recommendations of questionable utility (e.g. not eating fruit with meals) and it is also inadequate in several nutrients (calcium, vitamin D, E, pantothenic acid, copper, and potassium). Moreover, no evidence of its efficacy is available. Most of the research on low GI diets in weight reduction has been conducted over relatively short time periods of a few days or weeks. The effects of low GI carbohydrates may help to prevent excess weight gain, but before low GI diets can be advocated as a weight-loss strategy, more research must be done on their longer-term efficacy[66]. However, consumption of whole grain cereals, which are low in GI, is helpful in meeting fiber goals as well and may be helpful. A well balanced, hypocaloric low glycemic index diet may prove to be effective in properly educated, adherent patients who do not misuse it by consuming excess fat or protein, or by completely excluding healthful high glycemic foods such as carrots and potatoes. However, it is still unclear if the glycemic index offers sustained advantages to patients in planning menus and in learning to control food intake compared to other weight reduction methods. Any reducing diet must be viewed as a whole. Focusing on only one aspect , whether it is the glycemic index, the sugar content, carbohydrate, fiber, protein or fat, is not a solution in itself. WATER 1. Water needs on reducing diets Ample fluid intake is extremely important on weight reduction diets to avoid dehydration, especially if diets are ketogenic, very low in calories , or being undertaken in hot climates or with physical exertion. As mentioned earlier, losses of body glycogen and protein are accompanied by losses of body water. Intake of lowcalorie or calorie-free fluids such as water should be emphasized[67]. Beverages containing caffeine and alcohol should not be encouraged, since they increase diuresis. When the individual who is losing weight engages in very vigorous physical activity, electrolytes and water need special monitoring. The fatigue that some dieters associate with hypocaloric diets is often due in part, to dehydration, especially if they have also increased their physical activity and exercise regimes dramatically. Body water losses of as little as 2% have been associated with decreased physical and mental performance, and impaired thermoregulation [67]. The daily recommendation of at least 8 glasses of water is especially important for dieters, and they often require even more. Thus, a fluid intake plan should be incorporated in every weight loss regimen. ELECTROLYTES Electrolyte levels are of particular concern on VLCD, since occasionally cardiac arrhythmias have resulted from hypocalemia on such regimens [42]. Since hypocalemia can be fatal, electrolyte levels must always be monitored on VLCD. VITAMINS AND MINERALS 1. Needs During Weight Reduction Vitamin and mineral nutrition is critical during weight reduction and maintenance. The recommended dietary allowance for an individual's age and sex must continue to be met even on reducing diets . The lower the diet is in calories, the more likely it is that essential vitamins, minerals and electrolytes such as potassium, magnesium, vitamin B6, iron, and calcium are likely to be low. As a rule of thumb, diets below 1200 kcal/day are likely to require vitamin and mineral supplements in amounts approximating the Recommended Dietary Allowances[45]. Above 1200 kcal/day, women in the reproductive age groups may still need iron, calcium and folic acid supplements since their needs for these nutrients are high, but most other nutrient needs can be met by a well-balanced diet that follows the Dietary Guidelines for Americans [55]. For this reason, foods with high micronutrient density, but low energy density are especially important to include on a reducing diet. They include lightly processed fruits, vegetables, and whole grains. DIETARY FIBER 1. Needs on reducing diets Dietary fiber is chemically similar to carbohydrate in most of its forms but is virtually noncaloric. It, should also be included in the LCD reducing diet at levels of about 2035 gm per day if for nothing else than to facilitate normal laxation. Both soluble and insoluble dietary fiber may also modify hunger and help to sustain inter-meal satiety [68, 69]. Inclusion of five or more servings of fruits and vegetables daily, with plenty of whole grain breads and cereals can help to meet the goal of obtaining both soluble and insoluble fiber on the reducing diet. On a VLCD, it is also important to include at least some fiber.. As dietary fiber intake increases, water requirements also increase, and intakes of fluid should also be substantial. Adequate fiber and water are essential for maintaining the softness of the digestion and thus normal laxation. ALCOHOL Alcohol (ethanol) contains approximately 7 kcals per gram, providing more energy per unit of weight than carbohydrate or protein (each ~4 kcals/gram), but less than fat (~9 kcals/gram). Alcoholic beverages tend to be a source of non-nutritive energy, or empty calories. If protein, carbohydrate and/or fat are consumed at the same time as alcohol is ingested, their oxidation will be suppressed (most notably, fat oxidation), since alcohol is preferentially oxidized, and the other macronutrients will be stored[70]. Therefore, consumption of alcohol can lead to a positive fat balance through the sparing effect of alcohol on fat oxidation, leading to increased fat storage. Chronic overconsumption of alcohol thus can lead to fatty liver and dyslipidemia. Another important consideration concerning alcohol's influence on energy balance is its effects on energy intake. Alcohol is positioned at the bottom of the hierarchy of satiating efficiency of metabolic fuels consumed by humans. Generally, it is accepted that the fuels satiate to degrees from lowest to highest: alcohol, fat, carbohydrate (depending on type), and protein[71]. Alcohol energy is additive to the diet, producing no compensation in energy intake under most ad libitum situations, and in fact alcohol may stimulate appetite[72, 73]. For these reasons, alcohol consumption is usually contraindicated on weight-loss diets. ENERGY DENSITY Energy density is the calories provided per unit weight of food eaten. A low energy density of foods in the diet appears to have effects on satiety and satiation that may aid in weight reduction[74] When the composition of a diet of usual foods is decreased in fat, the energy density of the diet tends to fall since the total weight of food consumed remains constant [75, 76]. It is possible that some of the beneficial effects of low fat diets in weight loss and maintenance are due to energy density rather than to fat itself. SUMMARY Current guidelines for the composition of weight reducing diets, as discussed above, are outlined in Table 7. CONSOLIDATE LOSSES IN THE WEIGHT MAINTENANCE PHASE NUTRIENT NEEDS Once the obese individual has lost body fat, this healthier weight must be maintained. Thus the energy deficit phase is followed by the weight maintenance phase. It involves alterations in dietary intake and physical activity from levels prior to the onset of the dietary treatment. Paradoxically, the slimmer individual's energy needs are lower to stay in energy balance than they were prior to weight reduction. The primary reason for this is that some loss of lean as well as fat tissue inevitably occurs on reducing diets. Thus metabolically active tissue is reduced and resting metabolism is decreased. Also, it takes less effort to move the lighter body, and the energy cost of physical activity is thus reduced. The implications are that a slight decrease in energy intake from prior levels and an increase in energy output will be necessary during weight maintenance. Thus there is a need for continued attention to these factors on the part of the physician and patient. All too often the weight maintenance phase is neglected or ignored, and weight is regained over the long term[77]. RECOMMENDATIONS The best way to maintain energy balance in the face of lower energy needs over the long term is an important question that still has not been answered satisfactorily. Some factors that seem to be associated with long-term successful weight maintenance include continued regular exercise and, to a lesser extent, use of low calorie, low fat diets relatively high in fruits and vegetables. Also, continued selfmonitoring of the amount and type of food consumed and of physical activity levels may help[78] Although energy needs are less during weight maintenance, the requirements for protein, essential fatty acids, carbohydrate, dietary fiber, vitamins and minerals are similar to those of any normal adult, and should be provided. The Dietary Guidelines for Americans and the USDA's Food Group Pyramid describe the sorts of choices that are most healthful and useful . The Food Group Pyramid's macronutrient composition provides approximately 24% fat, 18% protein, 59% carbohydrate, and 22 gm dietary fiber; with advice that added sugars and fats are to be used sparingly[79]. The Dietary Guidelines for Americans recommend that all Americans, including those who are watching their weights, to adopt the following habits [55]: Aim for a healthy weight Be physically active each day Let the Pyramid guide your food choices Choose a variety of grains daily, especially whole grains Choose a variety of fruits and vegetables daily Keep foods safe to eat Choose a diet that is low in saturated fat and cholesterol and moderate in total fat (e.g. <30% of calories) Choose beverages and foods to moderate your intake of sugars Choose and prepare foods with less salt If you drink alcoholic beverages, do so in moderation. There is currently much dispute about the ideal macronutrient distribution in diets for weight maintenance, but at present very few long-term studies are available. Little is known about the effects of the diet's macronutrient content on weight maintenance. However, recent data suggest that a combination of a physically active life and moderation in dietary intake are key. 1.Carbohydrate A recent study of the self-selected diets of free-living American adults found that diets high in carbohydrate (above 55% of calories ) were lower in energy and in the calories per gram of food they supplied and were associated with lower BMI's than those consuming less carbohydrate. The nutrient density (amount of the nutrient per calorie consumed) was also higher for vitamins A, C, carotene, folate, calcium magnesium and iron, but lower in vitamin B-12 and zinc than those with lower intakes of carbohydrates. Also, the high carbohydrate group ate more low -fat foods, grain products and fruits and had the lowest sodium intakes of the groups studied [80]. 2. Energy density Other studies suggest that energy density of the diet rather than the macronutrient composition of the diet affects energy intake the most markedly [81-83]. One recent review found that low fat, high fiber diets were the most effective in promoting weight loss, and that their effects appeared to be associated with their energy density[84]. Whether this is also true in weight maintenance remains to be determined. There may be macronutrient effects on hunger and satiety that operate through endocrine and metabolic mechanisms such as leptin, insulin, adiponectin and other hormones only now being discovered that regulate food intake and that differ depending on these dietary characteristics . The macronutrient composition of habitual diets also affects health risks, and these must also be considered. Other effects of usual diets on weight maintenance may be genetic. Finally psychological and behavioral factors may vary on different macronutrient combinations. . Currently these topics are the subject of much debate, but research is needed to clarify what and which nutrient composition is optimal and how best to help people modulate their energy intakes regardless of dietary composition. . 3. Fat Although much remains to be discovered about the optimal dietary pattern for weight maintenance, a strong case can be made for keeping dietary fat levels below 30% of calories. In studies in which dietary fat was reduced from 35% to 25% of calories with no other recommendations, energy intake was reduced and weight was lost [85]. It was estimated that reducing fat by 10% to within the range of 20-30% of calories would result in a loss of about 16 gm of body fat a day owing to reduction in energy intakes. However, moderation in caloric intake is also in order, since in studies of free-living humans ranging from 11 weeks to 1 year in duration, fat restriction on ad libitum dietary patterns in the absence of other dietary changes produced only modest body weight losses of about 1-3 kg [69, 86, 87]. Low fat diets consumed on an ad libitum basis tend to be high in carbohydrate, but LDL-cholesterol decreases, plasma triglycerides tend to normalize, and so do HDL/total cholesterol ratios[88]. Serum insulin and blood pressure are usually decreased, and also hunger seems to be less[89]. Finally, weight control may be easier[90]. 4. Dietary Fiber Although the influence of dietary fiber on energy regulation is still not clear, increases of dietary fiber of about 15 gm appear to be associated with decreased energy intakes and body weight losses of about 2 kg over several months, and the effects may be greater in overweight persons[68].Since dietary fiber intakes are currently low, only about 15 gm per day in most Americans, and recommendations are for nearly twice that much, increased fiber levels seem to be appropriate.. LESSONS FROM LONG-TERM MAINTAINERS: IMPORTANCE OF INCREASED PHYSICAL ACTIVITY Long term follow up of health outcomes demonstrates the need for permanent changes in weight toward healthier levels. The relative lack of effects of temporary downward fluctuations, underscoring the need for long-term weight maintenance. Data collected from individuals successful at weight loss and maintenance have enhanced our understanding of the most effective strategies in the prevention of relapse and long term maintenance of healthier weights. Attention to moderation in dietary intake and the maintenance of high levels of physical activity are vital [91-94] . Behavioral and attitude adjustments are also important. Encouraging data suggest that behaviors associated with maintenance of weight loss require less effort and become more pleasurable over time[95]. In a recent telephone survey, 48% of individuals who had ever lost >10% of their body weight had maintained this loss for at least one year, and 26% had maintained for at least 5 years [96]. Although these data are self-reported, they suggest progress in the avoidance of relapse and weight regain. CONCLUSIONS: IS DIETING "WORTH IT"? About 39% of women and 21% of men in Western countries have ever tried to lose weight, and approximately 24% of women and 8% of men report that they currently are on a "diet". In contrast, about 25% of men and 30% of women report that they are watching what they eat to avoid weight gain or to maintain their weights at current levels[97]. Hypocaloric diets to induce loss of body fat therefore appear to be a common component of the weight control efforts of many people. Most individuals appear to be aware of and to use recommended measures, such as increased physical activity, decrease fat intake, decreased food portions, and decreased energy intakes. The problem is that they do so, but not for enough of the time. However, it is also true that dieting efforts often fail, and weight is often rapidly regained, probably negating predicted health benefits. Chronic dieters tend to be food-preoccupied, distractible, emotional, binge-prone, and unhappy, particularly when the diets are very restrictive [98]. Also, there are concerns about the connection between dieting and later eating disorders. Although dieting does not cause eating disorders, it may be one of a number of factors increasing its appearance. [99]. These realities and disadvantages have rightly led to questions about whether dieting is "worth it", and whether the treatment is worse than the disease. This chapter has stressed the role of the dietary treatment of obesity as a part of a comprehensive program of weight control that includes increased physical activity, lifestyle modification, appropriate intakes of other nutrients to minimize chronic disease risk, and eating patterns that maximize quality of life. Such dietary treatment in those with mild to moderate obesity helps to decrease risk factors over the short run and may decrease weight gain at least temporarily, although most individuals revert to their baseline weights after five years. Therefore some health benefit, although it is limited, may be present. However, the health risk/benefit may be negative when dieting entails a cycle of rapid loss followed by equally rapid weight gain. From the standpoint of quality of life and mental health, psychosocial problems do not appear to be inevitable accompaniments of weight loss[100]. Therefore, on balance, dietary approaches to obesity management do appear to be worthwhile, if , and only if, they are viewed as only one component of a long term weight control program to keep weights and risks at healthier levels. Weight control is "worth it".