Evaluation Options - Heart and Stroke Foundation of Ontario
advertisement
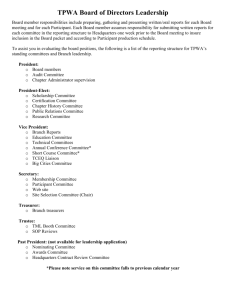
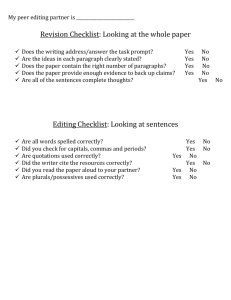
National Institutes of Health Stroke Scale Workshop Evaluation Options There are many evaluation options included in the introduction of the NIHSS into practice. The first two relate to clinical competency in performing and scoring the NIHSS. The last three refer to system and program evaluation. Evaluation tools are provided for Options 1 & 2. Evaluation Tools for Options 3, 4,& 5 should be developed to meet the organization’s needs and goals. Option 1: Self-Assessment (Knowledge and Skills) Using Self-Assessed Competency of Neurological Assessment Techniques particular to the NIHSS form (see page 3). This self assessment is designed to be completed at the following points: Pre-NIHSS education session 6 months post-NIHSS education to identify learning needs Option 2: Clinical Performance Competency The workshop is designed to provide the participant with knowledge and skills required to confidently use the NIHSS in the clinical setting. Competency is obtained through practice and interaction with the trainers/resource people in the clinical setting. Evaluation of competency in performing and scoring the NIHSS is done at the bedside using the Bedside Evaluation for Clinical Competency form (see page 9). Option 3: Evaluation of the Implementation Process Designated focus group sessions or one on one discussion with manager and/or educator can be used for this evaluation component. Some topics to cover at this time can include: Satisfaction, practice issues, and challenges. Perceived impact of the NIHSS on communication between nursing colleagues, physicians and patients/families. Perception of consistency, reliability and validity in the use of the NIHSS. Perception on the effect of the NIHSS on quality of care for patients. Option 4: Evaluation of Compliance Chart audits assessing compliance, documented communication of neurological decline, documentation of associated interventions and follow-up can be completed at 6-9 months after implementing the NIHSS in practice. Option 5: Evaluation of Sustainability Based on the evaluation components chosen, a formal review by team members of all information gathered is important to identify issues for ensuring a sustainability plan. NIHSS Evaluation Options, 2008 2 Option 1: Self-Assessed Competency of Neurological Assessment Techniques It is recognized that each person engaging in these education sessions comes with a foundation of knowledge and skills acquired from experience. The purpose of these education sessions is to build on current abilities, facilitate professional development and performance enhancement, and provide updated information regarding current best practices. To facilitate an understanding of your strengths and areas for skill development, we ask you to complete the Self Assessed Competency of Neurological Assessment Techniques. It is advisable to repeat this assessment in 6 months to identify ongoing learning needs and the impact of the education that was received earlier. NIHSS Evaluation Options, 2008 3 Self-Assessed Competency of Neurological Assessment Techniques Circle one of the following: Pre-NIHSS Education Questionnaire OR 6 months Post-NIHSS Education Questionnaire Name: Years working: Categories Used in This Self-Assessment Use the following levels to determine your level of skill and knowledge in performing the competencies identified. LEVEL EXPERT SKILL & KNOWLEDGE Analysis, synthesis, application, *highly skilled performance PROFICIENT Extensive exposure, with deep understanding of situation Able to rapidly and consistently identify actual and potential assessment changes Able to rapidly change priorities under all conditions Able to keep personal values in perspective and therefore able to encourage and support patient and family choices Conceptual understanding, *proficient performance Extensive exposure in most situations Able to anticipate potential assessment changes Able to prioritize in response to changing situations Able to interpret the patient and family experience from a wider perspective and can envision possibilities NIHSS Evaluation Options, 2008 4 LEVEL COMPETENT SKILL & KNOWLEDGE Conceptual understanding and skill performance *competent ADVANCED BEGINNER Varied exposure to many situations Able to identify normal and abnormal findings Able to prioritize under stable conditions Increased awareness of patient and family viewpoints Conceptual understanding, minimal clinical experience Limited exposure to clinical situations Able to identify normal findings Guided by what they need to do, rather than patient responses NOVICE Marginal conceptual understanding, minimal clinical experience Seeks assistance in making clinical decisions Benner, P. (1984). From novice to expert: Excellence and power in clinical nursing practice. Menlo Park: Addison-Wesley NIHSS Evaluation Options, 2008 5 Stages of Competency N C P E P= Proficient AB E= Expert C= Competent AB= Advanced Beginner N=Novice CLINICAL SKILLS, CRITICAL THINKING AND PROFESSIONAL BEHAVIOUR 1. I use a variety of neurological assessment techniques to collect data pertinent to my patients. (a) I am able to accurately determine the patients’ level of consciousness. (b) I incorporate neurological examination techniques to complete a comprehensive assessment when assessing stuporous or comatose patients. (c) I am able to accurately assess the mental status of my patients including the patient’s orientation, awareness, attention and concentration level, comprehension, memory, reasoning and judgment. (d) I have the skills and knowledge to assess the patients’ gaze and extraocular movements. I can determine a normal and abnormal response. (e) I am competent in the assessment of gross visual fields. I have the skills and knowledge to determine a normal and abnormal response and identify hemianopias. (f) I am able to accurately assess facial palsy. I incorporate testing into my assessment to determine if the patient has motor weakness of the lower face only or both the upper and lower face. (g) I am competent in the assessment of motor strength and drift. I utilize various NIHSS Evaluation Options, 2008 6 LEVEL SKILL & KNOWLEDGE assessment techniques to determine subtle weakness and changes in the patients’ motor strength. (h) I am able to accurately assess limb ataxia. I use assessment strategies to determine cerebellar impairment. I assess limb movement abnormalities in relation to sensory or motor dysfunction. (i) I am competent in the assessment of sensation. I utilize light touch as well as sharp/dull testing assessment techniques when appropriate based on the patients diagnosis and situation. (j) I am competent in the assessment of expressive and receptive communication deficits. I am able to perform a general assessment to determine the patients’ ability to understand the spoken and written word and to express thoughts orally and in writing. (k) I am competent in the assessment of dysarthria. I evaluate the patients’ clarity of speech. (l) I have the skills and knowledge to assess the presence or absence of “neglect”. I assess inattention to aspects of the patients’ senses including visual and tactile stimuli. I use assessment techniques to determine if a patient is not aware of (or is unable to identify) physical deficits. NIHSS Evaluation Options, 2008 7 LEVEL SKILL & KNOWLEDGE Stages of Competency N AB C P P= Proficient E E= Expert C= Competent AB= Advanced Beginner N=Novice CLINICAL SKILLS, CRITICAL THINKING AND PROFESSIONAL BEHAVIOUR 2. I use a variety of assessment techniques and information sources to collect data pertinent to my neuroscience patients. (a) I determine the right data collection method based on my patient’s condition (e.g. interviewing, listening, consulting, auscultating, percussing, observing, palpating, inspecting, monitoring, measuring) (b) I use identified patterns/trends to direct further assessment needs and synthesize all data to make care decisions (c) I identify potential and actual situations of patient risk based on assessment results and take action to ensure patient safety (d) I communicate changes in patient condition and document situations and outcomes to the appropriate authority in an objective and timely manner 3. I identify and prioritize nursing interventions. NIHSS Evaluation Options, 2008 8 LEVEL (a) SKILL & KNOWLEDGE I create a plan of care in collaboration with the patient and other team members that is based on patient priorities (b) I develop a written plan of care (c) I identify interventions and modify the plan of care based on actual or potential problems 4. I exercise professional judgment in decision-making. (a) I assess the risks and benefits of the required actions based on my patient’s condition, determine the actions to be performed and can provide a rationale for my decisions (b) I consult with others when I reach the limits of my knowledge and skill 5. I use problem-solving skills when responding to critical and ongoing situations. (a) I identify problems based on my patient’s condition and determine if the problem is within my scope of practice (b) I decide appropriate actions considering possible risks and benefits and collaborate with appropriate health care providers as necessary NIHSS Evaluation Options, 2008 9 Option 2: NIHSS Bedside Evaluation for Clinical Competency Circle yes/no as appropriate. Shaded areas to aid evaluator Identifies frequency of full assessment: YES NO 1) TID during the first 72 hours after admission for stroke (or as per institutions guidelines) 2) With any decline in neurological status 3) When the patient is received from ER, ICU, or PACU onto unit Name: _____________________ 4) After the 72 hour period - with any changes in neurological status Date: ______________________ S CATEGORY Description Correctly identifies the following: c o r 1a. Level of consciousness ***(Patients who score 2 or 3 on this item, should be assessed using the Glasgow Coma Scale) Alert e 0 Not alert 1 Not alert 2 Totally unresponsive 3 Pt keenly responsive Pt requires minor stimulation to obey, answer, or respond Pt requires repeated or painful stimulation Pt totally unresponsive (except reflexive effects) Identifies correct score: YES NO If pt scores 2 or 3, “Do you continue with this examination or refer to the GCS instead?” Participant identifies the GCS is used INSTEAD of the NIHSS: YES NO **Bedside NIHSS evaluation deferred for another pt. NIHSS Evaluation Options, 2008 If pt scores 0 or 1, “Do you still complete the GCS as well as this document?” Participant identifies the GCS is NOT completed YES NO 10 1b. LOC, questions (month, age) Answers both questions correctly 0 Answers one question correctly 1 Answers neither question correctly 2 1c. LOC, commands (Open/close eyes, make fist, release fist) Pantomime may be used 2. Best gaze (Patient follows examiner’s finger or face through full horizontal field) Performs both tasks correctly 0 Performs one task correctly 1 Performs neither task correctly 2 Normal 0 Partial gaze palsy 1 Forced deviation (not overcome by oculocephalic maneuver) 2 NIHSS Evaluation Options, 2008 Correct response ONLY includes correct Month, Age YES NO “If the pt states their date of birth, corrects themselves, or comes close can you count this as a correct response?” The participant verbalizes such responses are incorrect: YES NO “If pt correctly identifies the year, their date of birth, or the place, does this affect their score on this item?” Participant verbalizes the score for this item is based ONLY on month and age, not other questions such as year, date or place: YES NO Identifies correct score: YES NO “Can you use pantomime in a pt that does not follow commands?” Participant verbalizes pantomime can be used on this item: YES NO “Can you substitute a different one-step command in a pt that is unable to use their hands?” YES NO “Give an example of a one step command you could use.” Participant verbalizes a one step command. YES NO Assesses horizontal gaze (+/- other ocular movements): YES NO Correct score identified (only scores pt as 1/2 if deficits are clearly present: YES NO If unable to follow commands (confused, aphasic) uses tracking techniques to assess gaze: YES NO “Describe how you would assess a pt using “tracking”: Participant able to identify technique for tracking (moving face in front of pt and/ or moving about the room): YES NO “Describe the oculocephalic technique. What would you see in a normal and abnormal response? Able to identify technique for oculocephalic maneuver and is able to state the normal response (eyes move opposite to direction head is turned) and abnormal response (eyes remain fixed in one position when head is turned): YES NO 11 3. Visual (Introduce visual stimulus/threat to patient’s field quadrants) No visual loss 0 Partial hemianopia 1 Complete hemianopia 2 Bilateral hemianopia 3 Tests each eye independently and tests all 4 quadrants of each eye: YES NO Correctly performs visual testing (asks pt to look directly into his/her eyes, asks pt to cover one eye, introduces visual stimulus into each quadrant – visual threat used PRN): YES NO “How do you assess an aphasic pt for visual loss?” Participant identifies how to perform visual threat in a pt unable to follow usual visual testing: YES NO Please fill in the circles to demonstrate the following deficits: Partial hemianopia Complete hemianopia correctly identifies these: YES NO Bilateral hemianopia 4. Facial palsy (Show teeth, raise eyebrows, squeeze eyes shut) Pantomime may be used Normal 0 Minor paralysis 1 Partial paralysis 2 NIHSS Evaluation Options, 2008 Normal Mild asymmetry on smiling (flattened nasolabial fold, fewer teeth on one side with smile) Paralysis of lower face Paralysis of upper and lower face (one or both sides) identifies correct score: YES NO “What is a flattened nasolabial fold?” Participant identifies characteristics of a flattened nasolabial fold: YES NO “Would you use pantomime in an aphasic patient who does not follow commands?” 12 Complete 3 5a. Motor arm - Left No drift 0 (Test each limb independently: Palm Down: Elevate arm to 90 if pt sitting, 45 if pt supine and score drift/movement over 10 seconds) 5b. Motor arm – Right Drift (drifts but does not fall to rest on a support) 1 Some effort against gravity (drifts to fall on support) 2 verbalizes he/she would use pantomime with such a pt: YES NO “Could you use a cotton applicator tip to tickle each nasal passage of an aphasic or lethargic pt to compliment your assessment of facial palsy?” Participant verbalizes he/she can tickle each nasal passage to determining a valid response: YES NO Correctly scores R arm: YES NO Correctly scores L arm: YES NO Asks patient to hold their hands in a “Palm Down” position: YES NO Counts out loud for a full 10 seconds (or until arm hits support): YES NO Tests each arm independently: YES NO Places pt’s arms at 90 if pt sitting, 45 if pt supine: YES NO “If the pt does not follow commands, what could you do to encourage them?” Participant verbalizes he/she can position the pt’s arms at 90, use pantomime and use urgency in his/her voice.: YES NO Correctly scores R leg: YES NO Correctly scores L leg: YES NO Tests each leg independently: YES NO Counts out loud for a full 5 seconds (or until leg hits support): YES NO Places pt’s in supine position and elevates leg to 30: YES NO “If the pt does not follow commands, what could you do to encourage them?” Participant verbalizes he/she can position the pt’s leg at 30, use pantomime and use urgency in his/her voice: YES NO No effort against gravity (trace movement, limb falls immediately) No voluntary movement 3 Amputation, joint fusion etc 4 6a. Motor leg – Left No drift (Test each limb independently: With pt supine, elevate extremity to 30 and score drift/movement over 5 seconds) 6b. Motor leg - Right Drift (drifts but does not fall to rest on a support) Some effort against gravity (drifts to fall on support) X 0 1 2 No effort against gravity (trace movement, limb falls immediately) No voluntary movement 3 Amputation, joint fusion etc 4 X NIHSS Evaluation Options, 2008 13 7. Limb ataxia (Finger-nose, heel down shin) 8. Sensory (Pin prick to face, arm, trunk, and leg – compare side to side) Look at grimace in aphasic patient 9. Best language (Name item, describe a picture and read sentences) Absent 0 Present in one limb 1 Present in two limbs 2 Normal 0 Mild to moderate sensory loss (less sharp/dullness) 1 Severe or total sensory loss (not aware of touch) Correctly performs “finger-nose” testing: YES NO Correctly performs “heel down shin” testing: YES NO Only scores ataxia as being present if it is clearly demonstrated: YES NO “In a patient with severe weakness or aphasia who is unable to follow directions, what score would you give them on this item?” Ataxia is scored as 0 (absent) by the (because it can not be clearly demonstrated that it is present): YES NO Correctly scores sensory exam: YES NO Uses a safety pin to test sensation: YES NO Does not test sensation on hands or feet (rather uses arms and legs related to the incidence of neuropathies in hands/feet): YES NO Only scores the sensation as a 1 or 2 when it can be clearly demonstrated: YES NO “If the patient had sensory deficits not related to the current stroke such as diabetic neuropathy or other pre-existing conditions would you score only their stroke related sensory loss, or also their sensory loss related to these conditions?” Participant verbalizes that ONLY sensory deficits related to stroke are scored: YES NO 2 No aphasia 0 Mild to moderate aphasia (reduced fluency or comprehension) 1 Severe aphasia (communication exchange very limited) Mute, global aphasia 10. Dysarthria (Evaluate speech clarity by having patient read or repeat listed words) Normal articulation Mild to moderate dysarthria (can be understood) Severe dysarthria (unintelligible or worse) 2 3 0 1 Correctly scores best language: YES NO Asks pt to read all sentences and name all items: YES NO “Would you encourage a non-verbal pt to write their responses?” Participant verbalizes patients who cannot verbalize may write their responses: YES NO “If a patient follows simple one-step commands, but does not express themselves using speech, would you score them as a 2 or a 3?” Participant verbalizes the patient would receive a score of 2, because they exhibit some auditory comprehension: YES NO “If the pt does not describe a portion of the picture, how would this affect your assessment of extinction/inattention?” Participant identifies double visual stimulation should be tested: YES NO Correctly scores dysarthria: YES NO Asks pt to read word list: YES NO “If the pt were unable to read from the listed words, would you ask them to repeat after you?” Participant verbalizes they would ask the pt to repeat after him/her: YES NO 2 Intubated or other physical barrier X NIHSS Evaluation Options, 2008 14 11. Extinction and Inattention (Use information from prior testing to identify neglect or double simultaneous stimuli testing) No abnormality (no neglect) 0 Visual, tactile, auditory, spatial, or personal inattention, or extinction to bilateral stimulation in one of the sensory modalities) 1 Profound: more than one modality affected 2 TOTAL SCORE Correctly scores extinction and inattention: YES NO Performs double simultaneous testing of vision (L, R, both – tests upper and lower visual fields) and tactile senses (with pts eyes closed asks “Which side am I touching? L, R, or both?” – tests face, arms, legs): YES NO “What is the difference between a score of 1 and 2?” Participant verbalizes an understanding of the difference between a score of 1 (inattention to one sensory modality) and a score of 2 (inattention to more than one sensory modality): YES NO “What score would you give to a patient who does not recognize their own hand as part of their body?” Participant verbalizes a score of 2 because the pt shows both tactile and personal inattention. YES NO Calculates a total score: YES NO Records only actual patient response (not what he/she thinks the pt can do): YES NO Only uses coaching/pantomime for 1b LOC commands, 4. Facial or 5. & 6. Motor Arm/Leg: YES NO NIHSS Evaluation Options, 2008 15