If I had a stroke…. - the HIEC Stroke Events Website
advertisement
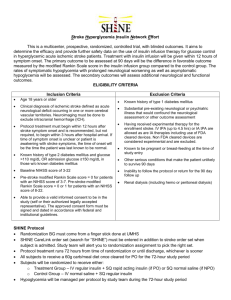
Using stroke scales to assess the patient – Rankin and NIHSS Dr Jonathan Birns Consultant in Stroke Medicine, Geriatrics and General Medicine Guy’s & St Thomas’ NHS Foundation Trust Alive and independent 100 80 Alive but dependent 60 Dead 40 20 0 Thrombolysis Differences/1000: Control 141 extra alive and independent 130 fewer dependent survivors To save 1 patient from disablement NNT is 7 (P<0.01) (P<0.01) Outcome measures/Stroke scales • Pathology • Impairment - abnormality of structure/function • Disability - functional consequence of impairment • Handicap - social consequence of impairment • QOL • Survival Outcome measures/Stroke scales • Valid • Reliable • Reproducible • Relevant • Practical • Sensitive • Communicable Modified Rankin Scale • measures the degree of disability or dependence in the daily activities of people who have suffered a stroke. • originally introduced in 1957 by Rankin (Rankin J. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957. 2: 200–15) • modified by Lindley et al in 1994 (Lindley RI, Waddell F, Livingstone M et al. Can simple questions assess outcomes after stroke?. Cerebrovasc Dis. 1994. 4: 314–24) 3 simple questions (Lindley et al. 1994) No Is the patient alive? 6 Dead Yes 5 Does the patient require help from anybody for everyday activities? Yes 4 Poor 3 No Yes Has the stroke left the patient with any problems? 2 Indifferent 1 No Good 0 Modified Rankin Scale 0 - No symptoms. 1 - No significant disability. Able to carry out all usual activities, despite some symptoms. 2 - Slight disability. Able to look after own affairs without assistance, but unable to carry out all previous activities. 3 - Moderate disability. Requires some help, but able to walk unassisted. 4 - Moderately severe disability. Unable to attend to own bodily needs without assistance, and unable tto walk unassisted. 5 - Severe disability. Requires constant nursing care and attention, bedridden, incontinent. 6 - Dead. mRS 0-3 mRS 4-6 National Institutes of Health Stroke Scale (NIHSS) • 15-item neurologic examination stroke scale • Used to evaluate the effect of acute cerebral infarction on: – – – – – – – – – level of consciousness extraocular movement visual-field loss motor strength ataxia sensory loss language dysarthria neglect National Institutes of Health Stroke Scale (NIHSS) • Provides a quantitative measure of stroke-related neurologic deficit • Originally designed as a research tool • Now widely used as a clinical assessment tool • May serve as a measure of stroke severity • Valid for predicting lesion size, short and long term outcome • Provides a common language for information exchanges among healthcare providers National Institutes of Health Stroke Scale (NIHSS) • Designed to be: – – – – Simple Valid Reliable Administered at the bedside consistently by: • Physicians • Nurses • Therapists • Should take <10 minutes to complete NIHSS Instructions • Administer NIHSS items in order • Record performance in each category after assessment • Do not go back and change scores • Do not repeat assessments within NIHSS • Range: 0-42 1a Level of consciousness 1b Level of consciousness questions What is the month? How old are you? 1c Level of consciousness commands Open and close the eyes. Grip and release the non-paretic hand. 2 Best gaze 3 Visual fields 4 Facial palsy 5 Motor - Arm 6 Motor - Leg 7 Limb ataxia 8 Sensory 9 Language 10 Dysarthria 11 Extinction and inattention NIHSS i NIHSS i NIHSS NIHSS NIHSS Category Pre-thrombolysis Time… after thrombolysis LOC Ia 0 0 LOC Ib 2 0 LOC Ic 2 0 Gaze 0 0 Visual fields 2 0 Facial palsy 2 0 Motor – right arm 3 0 Motor – left arm 0 0 Motor – right leg 3 0 Motor – left leg 0 0 Ataxia 0 0 Sensory 2 0 Language 3 0 Dysarthria 0 0 Extinction 2 0