Steve Sanders, DO - Community Service Council of Greater Tulsa
advertisement

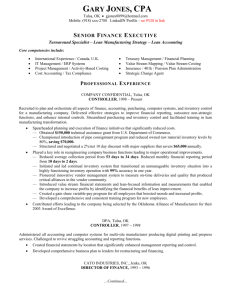
Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE Steve P. Sanders, DO, MBA, FACOI, FACPE, FACP Personal Residence 9640 South Winston Avenue Tulsa, OK 74137–4835 Telephone (918) 488-6053 (Business) (918) 704–3652 (Cellular) Fax: (918) 488-6627 Email: spsanders@saintfrancis.com (Business) spsanders1@mac.com (Personal) Twitter: @spsanders1 Education Masters of Business Administration, with honors, 1994 Oklahoma City University, Oklahoma City, Oklahoma Internal Medicine Board Certification, 1991 American Osteopathic Board of Internal Medicine, Chicago, Illinois Internal Medicine Residency, 1987-1990 Tulsa Regional Medical Center, Tulsa, Oklahoma Rotating Medical Internship, 1986-1987 Tulsa Regional Medical Center, Tulsa, Oklahoma Doctor of Osteopathic Medicine, 1986 Oklahoma State University, College of Osteopathic Medicine, Tulsa, Oklahoma Bachelor of Science, Criminal Justice Studies, 1977 University of Tulsa, Tulsa, Oklahoma Physician Licensure Missouri — Active Illinois — Inactive Texas — Active Oklahoma — Active 1 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE Board and Committee Memberships Board of Directors, CommunityCare Managed Healthcare Plans of Oklahoma, Inc., 2014–Present Board of Directors, MyHealth Health Information Exchange, 2014–Present Clinical Quality Committee, MyHealth Health Information Exchange, 2014 Tulsa Committee on Foreign Relations, Inc. Credentials Committee, Saint Francis Hospital, 2009-2011 Chair, Clinical Protocol Committee, Saint Francis Hospital, 2007–2009 Clinical Documentation Improvement Committee Leadership Team Saint Francis Hospital, 2008–Present American College of Osteopathic Internists, Professional Practice Advisory Council, 2004 Carondelet Health Long Term Care Facilities, Board of Directors, 2006 Leawood Kansas Chamber of Commerce, 2006 Oklahoma Carrier Advisory Committee, 2001–2002 Tulsa Regional Medical Center, Board of Directors, 1994 Tulsa Osteopathic Medical Society, Board of Directors, 1992, 1993, and 1996 Professional Certifications and Affiliations Fellow, American College of Physicians Fellow, American College of Osteopathic Internists Fellow, American Association for Physician Leadership Certified Physician Executive (CPE), Certifying Commission in Medical Management, American Association for Physician Leadership Affiliations: American Osteopathic Association, American College of Osteopathic Internists, American College of Physicians, American Association for Physician Leadership Career Experience December 2013 to Present Saint Francis Health System Tulsa, Oklahoma Vice President Medical Affairs Reported to the Senior Vice President Clinical Services, Saint Francis Health System Accomplishments Medical Director for the Saint Francis Health System Employee Health Services Serve on the Board of Directors for the MyHealth Information Exchange Serve on the Board of Directors for CommunityCare Managed Care Plans of Oklahoma, Inc. Health system Medical Director for the Comprehensive Primary Care Initiative (CPCI) Chair of the Physician Advisory Council 2 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE Warren Clinic clinical lead for the implementation of the EPIC electronic health record June 2013 to November 2013 UnitedHealth Group Tulsa, Oklahoma United Clinical Services Market Medical Director – Oklahoma Reported to the Senior Vice President Clinical Services UnitedHealth Group serves more than 80 million individuals worldwide with health benefits and services. The company has operations in all 50 states in the United States and 20 other countries worldwide. Their 2012 revenues were $110.6 billion. They have a Fortune 500 company ranking at number 22. The company was named the World’s Most Admired Company in the Insurance and Managed Care sector for 2010, 2011, 2012, by Fortune magazine. The company is a member of the Dow Jones Industrial Average. 2006 to 2013 Warren Clinic Tulsa, Oklahoma Internal Medicine Warren Clinic is a physician medical group in Northeast Oklahoma with over 340 physicians in 40 different practice locations. Warren Clinic is affiliated with the Saint Francis Health System. Accomplishments Pilot office within the Saint Francis Health System for the implementation of NextGen electronic medical record Practice site received five-star rating in 2009, 2010 and 2011 by Press Ganey survey Personal patient satisfaction score of 96% by Press Ganey Survey NCQA Level 2 Certified Patient Centered Medical Home Practice selected for CMS CPCI Initiative 2005 to 2006 Carondelet Health Kansas City, Missouri Chief Medical Officer Reported to the President and Chief Executive Officer, Carondelet Health Carondelet Health is a Catholic not-for-profit two-hospital system composed of St. Joseph Medical Center in Kansas City, Missouri and St. Mary’s Medical Center based in Blue Springs, Missouri, with combined gross operating revenues of over $369M. In FY2005, there were 229,022 patient days, 33,814 inpatient admissions and 258,000 outpatient visits with a combined medical staff of 983 physicians and 2,454 FTEs. Additionally, in FY2005, there were approximately 70,066 Emergency Department visits, 10,976 surgical procedures and 2,689 3 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE births. Ascension Health, the 3rd largest Catholic healthcare system in the U.S with over 67 hospitals in 20 states and Washington D.C. and over $11B in revenue, owns Carondelet Health. Responsibilities Full-time senior administrative position with operational responsibility for departments including Medical Quality Assurance, Performance Improvement, Case Management, Carondelet Care Resources (Carondelet Medical Equipment and Home Care Services), Medical Staff Recruitment and Retention, Medical Staff Services including credentialing and marketing, Orthopedic Surgery Residency Training Program and Continuing Medical Education. Senior administrative director for the Clinical Effectiveness Program (CEP) teams with accountability for twelve part-time medical directors. Vice President for Carondelet Long Term Care Facilities, Inc. Position holds accountability for oversight of Carondelet Manor, Villa St. Joseph and St. Mary’s Manor, three long term care facilities within the greater Kansas City area. Serve as member of the Carondelet Health Senior Leadership and Operations Team. Accomplishments St. Joseph Medical Center was cited in 2005 by the New York Times as one of the top five hospitals in the U.S providing evidence-based treatment for 100% of patients presenting with acute myocardial infarction. St. Joseph Health Center was cited in Modern Healthcare (11/14/05) as the top hospital in Kansas City (and the only hospital in the Ascension Health system) for hip and knee replacements, scoring 99.14% in the CMS pay-for-performance demonstration project Recently received an award from the Centers for Medicare and Medicaid Services (CMS) for achieving 1st decile scores in three out of four CMS/Premier/HQI core measures in 2005 for St. Joseph Medical Center and one out of three measures for St. Mary’s Medical Center. This also resulted in increased reimbursement from CMS of over $100,000 Senior Administrative liaison for establishing the first osteopathic orthopedic surgery residency-training program in conjunction with the Kansas City University of Medicine and Biosciences at St. Mary’s Medical Center. Responsible for ensuring the requirements of the OPTI Program and the Centers for Medicare and Medicaid (CMS) are completed and maintained successfully. Restructured the Carondelet Specialty Care Network, a for-profit physician recruitment platform for developing outreach clinical practice sites, to provide one source recruitment, contracting and financial management. Developed the Carondelet Health outreach referral program to extend health care system services to over a 150-mile primary and secondary service area. Member of the Board of Directors for the Carondelet Long-Term Care Facilities, Inc. 4 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE 2002 to 2005 Blessing Hospital/Blessing Corporate Services Quincy, Illinois Senior Vice President Medical Affairs and Chief Medical Officer Reported to the President and Chief Executive Officer, Blessing Hospital Blessing Hospital is a not-for-profit 434-licensed bed community-based hospital. In 2004, there were 74,410 patient days and 14,433 admissions inclusive of the 20 bed Skilled Nursing Unit, with a medical-dental staff of 229 physicians. Additionally, in 2004, there were approximately 40,814 Emergency Department visits, 8,549 surgical procedures and 1,129 births. In 2002, Blessing Care Corporation acquired Illini Community Hospital, a Critical Access Hospital, in Pittsfield, Illinois. Responsibilities Full-time senior administrative position with operational responsibility for total departmental budgets of $4.1M and 103 FTEs. Reporting departments include Quality Management, Organizational Improvement, Health Information Management, Care Management, Clinical Documentation Management Program, Medical Staff Services, physician recruiting/contracting and the East Adams Clinic. Senior administrative lead for coordinating the Southern Illinois University Family Practice Program with Blessing Hospital and member of the Board of Directors for the sports medicine fellowship program. Senior administrative director for eight part-time medical directors. Senior member of the hospital and corporate parent Executive Leadership and Operations Team. Accomplishments Quality initiatives led to Blessing Hospital being named as one of five recipients in Illinois to receive the “Distinguished Hospital Award – Patient Safety” for 2004 by HealthGrades, Inc. Revised the quality management program that fundamentally changed the medical staff and Board of Trustees quality committee structures. Incorporated evidencebased medicine and patient safety guideline recommendations to meet the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) National Patient Safety Goals and the Institute of Healthcare Improvement’s “100,000 Lives Campaign.” Led the medical management team that helped the organization achieve a 94% on the 2002 JCAHO resurvey. This was after the organization was cited with 31 Type I findings from their JCAHO survey in 2001. Led the Quality Management team in the development of the Quality Improvement Plan for our newly integrated cancer program. Achieved a 96% on the accreditation survey of our Cancer Center by the American College of Surgeons Commission on Cancer. The Cancer Center is currently ranked in the top 27% of cancer centers in the United States. 5 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE Developed a “Balanced Scorecard” to establish quality benchmarks for the organization that will be monitored by the Board of Trustees. Reduced the discharge not final billed (DNFB), from medical record coding and analysis, by 83% (11 days to 1.90 days) in 2004. Implemented a Clinical Documentation Management Program estimated to result in incremental revenues of over $1.4M in 2004. Led the Care Management team to deliver over $800,000 in yearly cost savings through reduced length of stay (LOS) Provided senior leadership to implement clinical transformation initiatives resulting in increased revenues or cost reductions of over $8.0M by 2004. Implemented, throughout the health system, a computerized clinical information system (Eclipsys SXA 3.6), with physician order entry. The clinical information system successfully went live in January 2005. Led the team with accountability for developing the clinical information system knowledge-based rules and alerts, developing clinical pathways and physician order sets. Led the initiative for implementing decision support. Assisted the steering committee with implementing the Heart &Vascular Center at Blessing Hospital. For the first time, this brought the availability of open-heart, thoracic surgery and interventional cardiology to the western edge of Illinois. 1999 to 2002 PacifiCare of Oklahoma, Inc. Tulsa, Oklahoma Vice President Health Services and Medical Director Reported to the PacifiCare of Oklahoma General Manager PacifiCare of Oklahoma is a for-profit Fortune 200 Health Maintenance Organization (HMO). From 1999 to 2002, it had over 91,000 commercial members and 31,000 Medicare+Choice (Secure Horizons) members. The PacifiCare HMO was the largest and most profitable health plan in the state of Oklahoma during that time. Generated over $380M in revenues in 2000, producing $24 million (8%) operating profit, where the industry standard is 3%. PacifiCare of Oklahoma represented 31% of the PacifiCare Health Plan revenue and 25.3% of the profit, becoming the most successful business within the PacifiCare Health Services parent company. Responsibilities Full-time administrative operational responsibility for the department of Medical Services with a departmental budget of $4.7M and 48 FTEs. Responsible for development of utilization management programs encompassing two HMO products. Accomplishments Led the development of new referral authorization oversight and catastrophic case management programs, as the contracting methodology changed from global capitation to shared risk. This resulted in a 33% reduction in acute days PTMPY for commercial members and an 18% reduction in acute days for senior members. 6 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE 1997 to 1999 Streamlined provider and facility credentialing, reducing working days required from 90 days to less than 45 days. Led the implementation team for successful National Committee for Quality Assurance (NCQA) “Excellent” accreditation of both the HMO commercial and Medicare+Choice Secure Horizons plans for Oklahoma in July of 2000 (final score of 74.6 out of 75.0). Developed a health improvement program, “Matters On Maternity,” that was published as a best practice in pregnancy management in the Pfizer/NCQA Quality Profiles in 1999. Quality improvement activities and customer service initiatives resulted in PacifiCare of Oklahoma’s receipt of the Award of Excellence for “Best of the Best HMOs – 1999” from the UltraLink 6th Annual National Satisfaction Survey of over 500 health plans. Served on the PacifiCare Southwest Region (Texas and Oklahoma) medical management committee where we developed case management, disease management and utilization review protocols for commercial and senior members. Participated as the Oklahoma representative on the national (corporate) PacifiCare Health Systems (PHS) Pharmacy and Therapeutics committee. We established and refined the PHS drug formulary for the commercial and senior product plans in nine states. Member of the PHS corporate Technology Assessment and Guideline committee. We had responsibility for reviewing and approving new medical technology and treatment guidelines for determining national benefit coverage guidelines. Saint Francis Health System Tulsa, Oklahoma Vice President Utilization Management and Medical Director for CareMed Alliance, Inc. Reported to the President, CareMed Alliance, Inc. Saint Francis Health System is a 900-bed, three-hospital catholic health care institution with revenues of over $450M and 1,500 FTEs. Responsibilities Full-time administrative responsibilities for utilization management, case management, medical economics analysis and quality initiatives at the health system level for over 100,000 managed care lives. Matrix management responsibility for Care Management division (500 FTEs, $20M budget), including home health, hospice, outpatient infusion company, durable medical equipment company, HealthZone physical performance facility, case management, social services, and occupational medicine. Accomplishments Responsible for the initial start-up of CareMed Alliance, Inc., a jointventure subsidiary Management Services Organization (MSO) of the health 7 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE 1995 to 1997 system, encompassing over 200 primary care physicians and 700 specialists. Developed health system utilization management programs encompassing two global-risk products. Developed and recruited the first Hospitalist program at Saint Francis Hospital. Developed policies and procedures including physician performance review tool and bonus program for the Hospitalist Service. Increased Hospitalist physician client list from 15 to 73 in seven months. The Hospitalist program demonstrated a 41% reduction in length of stay and average 23% reduction in ancillary charges for five major DRGs. Co-team physician leader of pharmacy medical action plan team resulting in estimated yearly cost savings of $501,000. Reengineered medical admission process for the Skilled Nursing Facility resulting in single page referral process. Physician champion for congestive heart failure, disease management initiative. Redesigned Saint Francis Hospital’s role in the University of Oklahoma College of Medicine internal medicine residency program. Springer Clinic, Inc. Tulsa, Oklahoma Medical Director Reported to the President, Springer Clinic Springer Clinic was a 90-physician multi-specialty group practice with over 49,000 HMO commercial and senior members and over $50M in annual revenues. Over ten clinical sites in the greater Tulsa metropolitan area and physicianinvestor owned ambulatory surgery center. Responsibilities Approximately 80% of time devoted to responsibilities for the Department of HMO Services including concurrent review, case management, quality assurance and retrospective review. Committee responsibilities: Quality Resource Management (Chair), Finance, PacifiCare Quality Assurance (Chair), Patient Care Committee (Chair), Medical Information Management (Chair), Strategic Planning, Risk Management, CQI Steering Team. Approximately 20% of time devoted to maintaining a clinical internal medicine practice. Accomplishments Created on-going interpretation and updating of medical policy and procedures. Team Leader responsible for full three-year re-accreditation by the Accreditation Association for Ambulatory Health Care (AAAHC). Authored utilization management plan meeting NCQA criteria. Co-authored physician peer review policy and procedure. Reengineered HMO utilization management department and procedures resulting in savings of three FTEs. Developed and implemented dual hospital systems for commercial and senior products. 8 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE 1990 to 1995 Developed a Hospitalist program that successfully lowered senior product days per 1,000 in one hospital network from 1,300 to less than 700; commercial days per thousand were lowered from 260 to 130. Lowered Medicare-risk DME pmpm expenses by 13%. Lowered Medicarerisk home health pmpm expenses by 62% over one year. Member of senior management negotiating team for capital partner relationship (Springer MSO). Director of Urgent Care facility and developed business plan for enhanced marketability. Accountable for physician recruitment and retention. Green Country Physicians Group, Inc. Tulsa, Oklahoma President and Chairman of the Board Green Country Physicians Group was Oklahoma’s first group practice without walls. Began with 15 physicians and grew to 45 physicians with over twelve different practice locations in three years. Responsibilities Maintained full-time internal medicine practice while providing operational leadership for management services and health plan operations. Accomplishments Initiated the first globally capitated managed care product at Tulsa Regional Medical Center with PacifiCare of Oklahoma for both commercial and senior membership. Initiated and conducted merger negotiations with Springer Clinic, Inc., a multi-specialty group practice, resulting in completed merger on 9/95. Maintained a full-time internal medicine practice, providing comprehensive diagnostic and therapeutic clinical services. Faculty Positions 1991–1999 Clinical Assistant Professor, Department of Internal Medicine University of Oklahoma College of Medicine, Tulsa, Oklahoma 1990–1991 Associate Professor of Internal Medicine Oklahoma State University, College of Osteopathic Medicine, Tulsa, Oklahoma Professional Publications and Presentations Covenants of the Medical Neighborhood: How Primary Care Physicians and Specialists 9 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE can “Choose Wisely.” Transforming Healthcare: Surfing the Tsunami of Change. Oklahoma Center for Healthcare Improvement, October 24, 2014. Sanders, SP. “The Silent Request.” Blood and Thunder: Musings on the Practice of Medicine, University of Oklahoma 2011. Sanders, SP. “Rooted in Caregiving.” Medical Econ, 2011;88:68. Sanders, SP. “EMR and the Falling Patient.” The Health Care Blog.com, January 21, 2011. Sanders, SP. “CAHPS measures are as important as profit and loss for hospitals.” KevinMD.com, November, 17, 2010. Sanders, SP. “The Gift.” Blood and Thunder: Musing on the Practice of Medicine, University of Oklahoma 2010. Sanders SP. “A view from the other side.” Fam Pract Manag, September/October 2008;15:14. Sanders SP. “Day 2: What’s Right In Health Care: 365 Stories of Purpose, Worthwhile Work and Making a Difference.” Studer Group, 2007 Sanders SP. “Denial of hospitalization for headache.” Headache, 1999;45:448. Sanders SP. “The future of physician groups in integrated delivery systems.” JMCM, 1997;2:24. Sanders SP. “The best thing I could do for dad: stop being his doctor.” Med Econ, 1997;21:138. (Medical Economics Writing Contest, Grand Prize Winner, 1997) Sanders SP. “This is proper management?” Hosp Pract, 1997;32:25. O-Yurvati AH, Laub GW, Sanders SP, et al. “Reduction in pulmonary microvascular pressure following cardiopulmonary bypass: beneficial effects of dobutamine. Int Surg, 1995;80:231. Yurvati AH, Sanders SP, Dullye LJ, et al. “Antiarrhythmic response to intravenously administered magnesium after cardiac surgery.” South Med J, 1992;85:714. Sanders SP. “Minicomputer software programs aid critical care.” J Am Osteopath Assoc, 1991;91:312. Olivencia-Yurvati AH, Sanders SP. “Sulbactam-induced hyperpyrexia.” Arch Intern Med, 1990;150:1961. Archer RL, Grogg SE, Sanders SP. “Mucoepidermoid bronchial adenoma in a 6-year-old girl: a case report and review of the literature.” J Thorac Cardiovasc Surg, 1987;94:452. 10 Steve P. Sanders, DO, MBA, CPE, FACOI, FACPE Professional Continuing Education American College of Physician Executives (ACPE) — Over 305 hours leading to Certified Physician Executive (CPE) designation by the Certifying Commission in Medical Management. Courses included: Informatics and Meaningful Use of Electronic Health Records Physician in Management I Physician in Management II Principles of Medical Management Managing Transition Three Faces of Quality Managing Physician Performance Managing Change The Certifying Commission in Medical Management Tutorial Health Care Finance Health Law Healthcare Financial Analysis & Cost Management 2000 Executive Leadership Focus Round Table Session I – Keeping your Fingers in the Market Round Table Session II – Evaluating Managerial Performance 2001 Fall Institute CEO Program 2002 Spring Institute Leadership Skills for Medical Staff Officers Conflict Management and Multidimensional Problem Solving Building the Extraordinary Health Care Organization Strategic Sources of Power and Influence ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE ACPE Strategies for Success — National Committee for Quality Assurance (NCQA) Strategic Public-Sector Negotiations Program — John F. Kennedy School of Government, Harvard University Leadership Conference for Trustees, Physicians, and Executives — Governance Institute Executive Leadership Conference — Voluntary Hospital Association (VHA) Joint Commission on Accreditation of Healthcare Organizations (JCAHO) 2004 PreSurvey Update for VSS Participants — VHA VHA Mid-America Physician Leadership Meeting — VHA Ascension Health Leadership Institute — St. Louis University 11