Biochemistry II Guide
advertisement

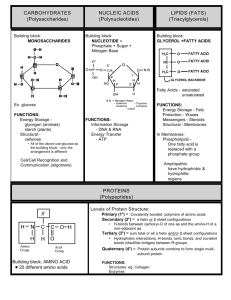
Biochemistry II *1: Lipids Overview *2: Absorption of Lipids *3: Lipoproteins *4: Artherosclerosis *5: Fatty Acids *6: Beta Oxidation of FAs *7: Fatty Acid Synthesis Overview Outline & Notes *8: Lipid Derivatives *9: Ketosis/Ketogenesis *10: Cholesterol Synthesis *11: RAAS & Aldosterone *12: Proteins *13: Amino Acids *14: Urea Cycle *15: Amino Acid Metabolism *16: Henderson-Hasselbach *17: Enzyme Kinetics *18: Nitrogen Metabolism/Opiod *19: Porphyrin Rings *20: Hemeglobin *1: LIPIDS OVERVIEW Lipid Function Fatty acids Metabolic fuel; component of several lipids Triacylglycerol Main storage of fatty acids Phospholipids Comprise membranes, source of arachidonic acid, inositol triphophate and diglyceride for signal transduction Cholesterol Component of membranes, prescursor of bile salts and steroid hormones Bile salts Intercellular signal regulating gene expression Ketone bodies Metabolic fuel A. Fatty Acids a. Saturated: no double bonds (ex: stearic acid) i. Raise “good” (HDLs) and “bad” (LDLs) cholesterol b. Monounsaturated: one double bond forming a cis- structure (ex: oleic acid) i. Raise HDLs and lower LDLs c. Polyunsaturated: multiple double bonds (ex: linoleic acid) i. Maintain HDLs and lower LDLs d. Trans: one or more double bonds forming trans- instead of the normal cisi. Lower HDLs and raise LDLs e. Nomenclature i. The carbon next to the –COOH group is the α-carbon ii. The tail carbon is the ω-carbon f. Essential Fatty Acids i. Linolenic -3 and Linoleic -6 (and Arachidonic Acid only when linoleic is low in the diet) ii. Linolenic is key for growth, development and vision; Linoleic makes Arachidonic for prostaglandins iii. Essential b/c we do not have enzymes to produce double bonds past C9 B. Some trivia facts (for general understanding) a. 100,000 kcal in fat storage. Fat CANNOT be turned into sugar. b. 20,000 kcal in protein storage c. 20 kcal in glucose / 60 kcal in glycogen *2: ABSORPTION OF LIPIDS (concept map on Lippincott’s p. 177) A. Adults ingest between 60 and 150 g of lipids per day, primarily triacylglycerol. Lipid digestion is hormonally controlled. In response to the presence of lipids in the duodenum, mucosal cells secrete Cholecystokinin (CCK; from Greek chole, "bile"; cysto, "sac"; kinin, "move"; hence, move the bile-sac), which causes gallbladder contraction and secretion, pancreatic release of digestive enzymes and decreases gastric motility of the stomach. Secretin, released in response to the low pH of the chyme, causes release of bicarbonate ions (HCO3-) from the pancreas and liver in order to bring pH up to optimal enzyme levels. B. Processing of dietary lipid in the stomach – Acid Lipase from the stomach breaks up triacylglycerols. FYI: Acid lipases are particularly important for neonates, whom primarily consume milk fat, and those with cystic fibrosis, for whom pancreatic lipase is nearly or completely absent. Long chain FAs can injure the mucosal lining of children, reducing bile salt and lipase activity. C. Emulsification of dietary lipid in the small intestine – Bile salts (converted from cholesterol in the liver and stored in the gallbladder) are used as emulsifiers >> substances that increase the surface area of the hydrophibic lipid droplets to aid digestive enzymes, they also prevent the lipid droplets from coalescing >> i.e. “dissolves” them i. Bacteria help cholesterol conversion to bile salts > high antibiotic doses can lead to high cholesterol D. Degradation of dietary lipids by pancreatic enzymes – Triacylglycerol degradation: Pancreatic lipase removes the FAs at carbons 1 and 3 making a mixture of 2monoacylglycerol and free fatty acids. Procolipase is activated in the pancreas by trypsin to make colipase, which binds the lipase and anchors it at the lipid-aqueous interface. i. FYI: Orlistat, an antiobesity drug, inhibits gastric and pancreatic lipases, thereby decreasing fat absorption – Cholesterol ester degradation: most dietary cholesterol is non-esterified, for the 10-15% that is esterified the pancreatic cholesterol ester hydrolases break the cholesterol ester into cholesterol plus free fatty acids – Phospholipid degradation: Trypsin activates phospholipase A2 which, in the presence of bile salts, removes one fatty acid from carbon 2 of a phospholipid, leaving a lysophosphatidic acid b/c of the –OH left on carbon 2. E. Absorption of lipids by intestinal mucosal cells (enterocytes) – Bile salts (require taurine + lysine) combine with free FAs, free cholesterol and 2-MG in the jejunum to form mixed micelles, which approach the brush border membrane of the enterocytes. Short- and medium-(8-12 carbons) chain length FAs, however, can directly cross the intestinal mucosa w/o forming micelles. – Bile salts are reabsorbed and recycled by the liver. F. Re-synthesis of triacylglycerol and cholesteryl esters – At the endoplasmic reticulum, fatty acids are converted into their active form by fatty acyl CoA synthetase (thiokinase). Using fatty acyl-CoA, the 2-MG are converted to triacylglycerols by triacylglycerol synthase and then packaged as chylomicrons. Lysophospholipids are reacylated to phospholipids by a family of acyltransferases, and cholesterol is esterified to a cholesteryl ester fatty acid by acyl CoA: cholesterolacyltransferase, which is also packaged into the chylomicrons. Short- and medium-chain length FAs are released directly into portal circulation and carried by serum albumin to the liver. – Acyltransferase production is also stimulated by a high insulin : glucagon ratio, which stimulates fat storage Biochemistry II Guide Page 2 G. Secretion of lipids from enterocytes – Apolipoprotein B-48 surrounds chylomicrons to aid in increasing its solubility. Chylomicrons then travel in the lymphatic system as chyle (appears milky) and are released into circulation via the thoracic duct. In the blood, HDL transfers to the chylomicron apo C-II, which activates lipoprotein lipase, as well as apo E, which activates endocytosis of the remnant chylomicron by the liver (E2-hard to break down/type III dislipidemia, E3-wildtype, E4-Alzheimer’s). i. Abetalipoproteinemia is caused by defects (d/t gastroenteritis) in the association of lipids to apo-B48 leading to hypochylomicronemia / hypoVLDL / hypoLDL (Sx: streaky stool containing chylomicrons) ii. Clinical note: B48 influences satiety. IV’d food doesn’t produce B48 > no satiety. H. Use of dietary lipids by the tissues – Primarily used in skeletal muscle and adipose tissues, but also all tissues except the brain. Adipocytes secrete lipoprotein lipase and peripheral cells do hormonal sensitive lipase, which degrade triacylglycerol to 3 free FAs and glycerol (can become PGAL). i. Lipoprotein + hormonal sensitive lipase are active when phosphorylated during a high glucagon : insulin ratio and stimulate mobilization of fat >> to go on to TCA ii. Familial lipoprotein lipase deficiency (type 1 hyperlipoproteinemia) results from a deficiency of lipoprotein lipase or its coenzyme, apo C-II, resulting in massive chylomirconemia. – DDT (pesticide), tetrachloroethylene (detergent) and 2,4-dichlorophenoxyacetic acid (weed killer) along with other lipophilic substances become toxic due to uptake alongside lipids. I. Lipid Malabsorption – Results in increased fecal lipids (steatorrhea: large, pale, frothy stools) can result from cystic fibrosis and/or shortened bowel (decreased absorption, caused generally by gluten). The fat-soluble vitamins A, D, E and K along with essential FAs are also affected. Normal excretion is 6g fat / 24 hr period with 95% absorption rate. 1. Tx: low fat diet and hydrolysates of protein and starch Biochemistry II Guide Page 3 *3: LIPOPROTEINS: Complex Lipids Chylomicron Enterocyte B48 VLDL (chylo remnant) Liver B100 IDL Liver B100 & E3 LDL Liver B100 Active Apo. B48, CII & E3 (in blood) B100, CII & E3 (in blood) B100 & E3 B100 Enzyme Activated Remnant CII > hormone sensitive lipase (peripheral cells) B48, E3 (CII reattaches to HDL) Liver > a.a. and VLDL CII > hormone sensitive lipase (peripheral cells) IDL: B100 & E3 LDL: B100 IDL: Liver LDL: peripheral cells ----n/a---- endocytotic LRP-clathrin ----n/a---- ----n/a---- Liver Least dense, largest size Representative of diet B48 + Apo4 = satiety Transports dietary fats Represents primarily endogenous fat. Alcohol limits its production. Carries TGs back to liver Peripheral cells: B100a.a. (cytosol) Cholesterolreduces HMG-CoA reductase Main cholesterol carrier to periphery Formation Nascent Apo. Degradation Other/Roles HDL Liver + Intestine Nascent: A1 (or A2 or A3) Discoidal: A1& LCAT (liver) Pre beta: only A1 in blood st 1 : HDL3:A1, LCAT, CII & E3 2nd: HDL2-larger: A1, LCAT HDL1-ABNORMAL-huge LCAT (its own) ABC-binding protein (peripheral) Liver: HDL2 to SRB1 Kidney: A1 to amino acids Reverse TG+cholesterol transport, donates apolipids, antioxidant A. The chylomicron in summary 1. food enters lumen of intestine 8. nascent chylomicron enters lymph (chyle) 2. Bile salts enter and emulsify fat a. albumin attaches to small+medium FA’s 3. creates a micelle 9. Nascent CM into blood where HDLs activate CM 4. pancreatic lipase removes esters 10. CM attaches to recipient cell via CII receptor 5. lipid derivatives enter enterocytes 11. Lipases break open CM and spills contents into cell 6. ApoB48 production is stimulated 12. Remnant chylomicron never reactivates. 7. re-esterfication occurs 13. Returns to liver for degradation B. VLDL, IDL and LDL – 3-hydroxy-3-methylglutaryl-COA (HMG) reductase Stimulated by insulin to form cholesterol, which goes into bloodstream. In healthy individuals, negative feedback loop with cholesterol inhibits further cholesterol production. In familial hypercholesterolemia, these genes never turn off. Statin drugs inhibit HMG enzymes seriously blocking cholesterol production, which may be a wrong diagnosis if cholesterol uptake by HDL or similar problems can be implicated instead. – Malfunctions Liver disease: fatty liver due to improper packaging of VLDL Biochemistry II Guide Page 4 Other dislipidemias: Malfunction of B100 activation of LPL. Raises serum LDL+IDL+VLDL >>> oxLDL and arthrosclerosis. Most controllable by dietary decrease of cholesterol and carbohydrates >> lowers insulin levels Clatherin malformation (type II hyperlipoproteinemia): LDL unable to undergo endocytosis or negatively feedback HMG >> hypercholesterolemia C. HDL – LCAT (Lethicin cholesterol acyl transferase) – is activated by ABC-binding protein and facilitates the gathering of cholesterol from tissue. a. OPCs found in grapeseed oil facilitate LCAT activity – Malfunctions a. Too few HDLs >> plasma chylomicronemia as activation of VLDLs or CM is impaired. b. Diabetes: high insulin changes surface proteins leading to hyperchylomicronemia due to the inability to release chylomicron contents. C protein is diagnostic test. c. HDL1: Huge cluster engorged with cholesterol and TGs. Associated with patients with sever hypercholestric conditions. This allows for a misleading lab lipid analysis because high HDLs are typically normal, but depending on type of HDLs (i.e. HDL1) a liver condition becomes a consideration. *4: ARTHROSCLEROSIS A. Excessive amounts of LDLs is a MAJOR contributor B. Superoxide Dismutase (SOD) along with nitric oxide oxidize LDL that’s been present in the blood too long >> makes it stick to the endothelium of blood vessels C. Nitric Oxide (NO) – NO is an endothelial lining relaxation factor also used for post-traumatic rehabilitation – L-arginine is precursor to NO The body’s analog of arginine—monoKn L-arginine—also stimulates production of NO. D. LDLox is REDUCED by: – Essential vitamins A (specifically Beta Carotinoid precursors), C and E inhibit/reverse oxidation E. LDLox stimulates monocytes to become macrophages, but the LDLox causes small nicks in the lining of the monocyte/macrophage. When the marcophage subsequently eats LDLs, instead of phagocyzing the LDLox gets packed in foam cells that form a lipid plug. F. The body doesn’t recognize foam cells so antibodies attack the plug, causing platelet aggregationarthrosclerosis. *5: FATTY ACIDS A. B. C. D. Storage of fatty acids is based on Insulin and Glucagon levels. Insulin high fat storage in adipose Breakdown of FAs is stimulated by high glucagon levels Structure of Triacylglyceride: Glycerol backbone + 3 fatty acid chains Lipases: Enzymes that cleaves ester linkages (fatty acids) off glycerol – Lipoprotein Lipase (adipose) / Hormonal Sensitive Lipase (periphery) • cleaves fatty acid off carbon 1 and/or 3 • Active when phosphorylated, i.e. high glucagon : insulin ratio Biochemistry II Guide Page 5 Monoacylglycerol lipase • in adipose tissue, cleaves at the carbon 2 AFTER the lipase – The actions of these two enzymes leave us with a glycerol backbone and 3 fatty acids • The glycerol backbone goes to the blood and liver and becomes glycerol-3-phosphate (remember, this can convert to PGAL) that can then go onto glycolytic and gluconeogenic pathways if needed. • Albumin is a carrier of free fatty acids to the cells for energy. E. Fate of the Fatty Acid: It has to get across the cell membrane first: – Lipophospholitic transfer: Diffusion into the cytosol • Referred to as a Daisy chain effect as one FA replaces another. • The Key point here: the FA going in may not be the FA coming directly out. F. Carnitine Shuttle: movement into mitochondria - VERY important. – 1st Enzyme: Acyl CoA Synthetase. Consumes 1 ATP as it adds a CoA onto a fatty acyl group in the cellular cytosol to allow transport across the outer mitochondrial membrane. – 2nd Enzyme: Carnitine Acyl Transferase 1 (CAT1/CPT1) • Location: outer membrane, regulates β-oxidation. • Adds FA to carnitine, taking off the CoA from the fatty acid and making fatty acyl carnitine. • Carnitine in the liver and kidney is made from methionine + lysine, but skeletal and heart tissue depend on carnitine from the diet (meat) • Nutritionally supplementing with the amino acid substrates of carnitine—lysine or the vit C product 4-butyrobetaine hydroxylase—may be better than L-carnitine for weight loss because these substrates can more easily cross membranes than the polar carnitine molecule. • Also found in short (SCAT), medium (MCAT) or long (LCAT) chain forms • MCAT deficiency: autosomal, recessive disorder that is the most common inborn error of FA oxidation (1:12,000 births in the west, 1:40,000 worldwide), causing a decrease in oxidation and severe hypoglycemia b/c tissue has to rely on glucose for energy. The inability for infants to mobilize medium chain FAs has been linked to sudden infant death syndrome (SIDS), aka Reye’s syndrome. • Tx: carbohydrate rich diet and/or short-chain fatty acid diet rd – 3 Enzyme: Translocase: Transfers fatty acyl carnitine across inner mitochondiral membrane – 4th Enzyme: Carnitine Acyl Transferase 2 • Releases FA from carnitine, re-adds a CoA making fatty acyl CoA which continues through beta oxidation G. Follow a Palmatate 16:0 (Review for understanding) – Palmatate stored in adipose tissue as TAG – Palmatates cross plasma membrane by daisy – Insulin levels drop (and Glucagon high) chain (-1 ATP) – Lipases respond to glucagon/phosphorylation – Carnitine shuttle into mitochondria (-1 ATP) – Palmitate breaks into 3*FA & 1*glycerol – On to Beta Oxidation – Biochemistry II Guide Page 6 *6: BETA OXIDATION A. Location: Mitochondrial Matrix B. Goal: to break up FA into 2 carbon units (acetyl CoA) that can enter TCA C. Product ATP is higher (46ATP/6 carbons) than glycolysis (38ATP/6 carbon glucose) D. Saturated Fatty Acids: – Oxidation > Hydration > Oxidation > Thiolysis (“O,HOT!”) – Energy from Acetyl CoA = [(Number of Carbons / 2) x 12] – Energy from NAD+FAD (Oxidation steps) = [(N/2–1)x 5] • Palmatate 16:0 = divide by 2 (#acetyl coA’s) = 8 • 8 X 12 = 96 ATP (# from cycles of TCA) • Subtract one (#cycles breaking into A-CoA). = 7 • 7*5 (#ATP/cycle of carbon break down) = 35 • Gross = 96+35 = 131; Net = 130 (-1 ATP from carnitine shuttle) or 129 (-2 from both shuttles) E. Unsaturated Fatty Acids – Oxidation > Reduction > Mutase > Hydration > Oxidation > Thiolysis (“ORM HOT”) • Reduction occurs by NADPH because NADPH is independent of body energetics, whereas NADH is regulatory in metabolism. Assume 1 NADPH expenditure per double bond. • Mutase (isomerase) that moves double bond over one segment towards carbonyl (i.e., from 4 to 3, etc.) – Each double bond uses one NADPH (3ATP), so for 16:2, 1st determine gross for 16:0 = 131 ATP. Then, take 131-(3*2 db’s) = 125 ATP gross. F. Odd Chained Fatty Acids (occurs mainly in vegetarians and vegans) – Different BECAUSE left with a 3-C propionyl Coa instead of acetyl CoA – Step 1 = Carboxylation: uses propionyl-Coa carboxylase to get a 4 carbon compound. Use ATP (Mg) and requires BIOTIN. – Step 2 = Racemase by D,L-methylmalonyl CoA. – Step 3 = Mutase, changes it to Succinyl CoA. Needs 5’ adenosyl cobalamin (VitB12) and intrinsic factor (for B12 absorption). • Cobalamin is made up of Cobalt, the active part of the mutase – Enters halfway through the TCA cycle, ~6 ATP formed per TCA cycle. – Calculations: Ex. 7:0; 1st 7-3 = 4, then calculate for 4:0 = 4/2 = 2, 2*12 = 24 + 2*5 = 34 ATP (2 in both b/c 2 Acetyl-CoA), +6ATP for the final propionyl = 40ATP, but subtract 1ATP for the carboxylation = 39ATP gross Biochemistry II Guide Page 7 – Nutritional Considerations • OTC form of cobalamin B12, extrinsic cyanocobalamin, is not useful to body. Requires intrinsic factor from pyloric sphincter to absorb and activate extrinsic B12. After B12 is absorbed, it has to be transported by proteins produced in the liver – transcobalamin I, II, III– so this is another source of B12 deficiency and liver problems • Megaloblastic anemia results if intrinsic factor or B12 are absent b/c odd-chain FAs aren’t metabolized • Copinates could build up, esp for vegetarians, if biotin or B12 are low • Other use of B12 > chronic fatigue syndrome H. Practice – Breakdown of 18:0 >>> gross 148 ATP, net 146 or 147 ATP (for shuttles) – Breakdown of 17:0 >>> gross 125 ATP – Breakdown of 18:3^9,12,14 >>> gross 139 ATP I. Other β-oxidation deficiencies – Methylmalonic acidemia & aciduria: associated with vit B12 deficit resulting in metabolic acidosis and retardation – Zellweger (cerebrohepatorenal) syndrome & X-linked adrenoleukodystrophy: peroxisomal defects leading to very long-chain FA (VLCFA) accumulation – Refsum disease: rare, autosomal recessive; deficiency of α-hydroxylase resulting in phytanic acid accumulation in the plasma. • Sx: neurologic deficiency • Tx: dietary restriction *7: FATTY ACID SYNTHESIS A. Location: All tissue except muscle, but primarily liver and lactating mammary glands B. Occurs w/ high Insulin : Glucagon and requires a lot of niacin (vitB3) and riboflavin (vitB2) C. Primary end product: Palmitate 16:0 (humans do not make odd chain FA) D. The Reactions 1. The mitochondira starts building up citrate >> inhibiting PFK-1 while stimulating F-2,6BPase 2. Citrate moves out into the cytosol 3. Citrate lyase splits citrate into acetate (which CoASH quickly makes into Acetyl-CoA) and cytosolic OAA NADH NAD+ NADP NADPH OAA Malate Pyruvate Cytosolic Malate Dehydrogenase Malic Enzyme* *the NADPH formation is important because NADPH is then used as the phosphate source for FA synthesis -The 3 sources of NADPH in the cytosol are HMP’s 6-phosphoglucanate + G-6-PD & Malic Enzyme Biochemistry II Guide Page 8 4. Insulin simultaneously turns on Acetyl-CoA Carboxylase (aka Malonyl CoA Synthase) in the nucleus -Bicarbonate ions attach to biotin which then attaches to the acetyl-CoA carboxylase while consuming 1 ATP -Acetyl-CoA Carboxylase then makes Acetyl-CoA into malonyl CoA (a 3 carbon compound) Acetyl-CoA Carboxylase Controls: Rate-limiting step Stimulated by Inhibited by Citrate Palmitoyl (long chain) CoA Dephosphorylation Phosphorylation Insulin Glucagon + Epinephrine 5. Malonyl CoA inhibits CAT-1, stopping transport of fats into the mitochondria. 6. Translocase brings the malonyl-CoA and acetyl-CoA into the proximity of Acyl Carrier Protein (ACP) -ACP: Acyl carrier protein (similar to PDH enzyme); aka fatty acid synthase 7. Both CoA’s attach to ACP and go through a series of reactions forming one fatty acid from each end (2 total/ACP) Condensation >> Reduction >> Dehydration >> Reduction >> Repeat –or– Thiolysis --Location of elongation and desaturation: smooth endoplasmic reticulum (but inhibited by trans-fatty acids, people with high trans fat diets need to have this block by-passed with arachidonic acid to lower the triene/tetraene ratio while fixing the diet) --During desaturation the carboxyl group gets pushed out, which is why we can’t form double bonds after carbon 9. This process requires oxygen and NADPH as well as cytochrome B5 and always forms cis- double bonds (most important bonds formed at 9th, 6th, 5th, and 4th position (9 and 6 most susceptible to toxicities)) --Confusing point: you continue adding onto the growing FA by adding a malonyl-CoA (3C) each cycle…but synthesis is supposed to add on 2C units. What really occurs is a condensation reaction with the growing FA that binds only two of the carbons to the chain and the extra carbon is released. That’s why a board question could ask: “C14 labeled carbonate ions are in the cytosol of a cell in rapid FA synthesis. How many carbons of C14 label are found incorporated into a f.a. end product?” The answer is zero b/c it gets cycled out! E. Important Points to Remember *For the production of one palmatate, 8 citrate must cross the mitochondrial membrane (i.e. 2 Carbons / Citrate) *Only 1 acetyl-CoA is used in the formation of any length fatty acid, the rest are all malonyl CoA *How many ATP are diverted in the production of one palmatate 16:0? -145 ATP (or x2 per ACP >>> 290 ATP total) *Rate limiting enzyme: acetyl-CoA Carboxylase F. Calculation of #ATPs diverted in FA Synthesis 1. Number of citrate = number of acetyl CoA = # of Carbons in product / 2 2. Net loss of ATP per citrate = # of citrate x 12 3. Number of cycles: -initial cycle forms a 4 carbon molecule = 1 cycle -remaining cycles adds on by 2 carbons = (# of carbons in product – 4)/ 2 = remaining cycles Total = 1 + remaining Net loss of ATP per cycle = # total cycles x 6 4. Net loss of ATP per malonyl-CoA formation = # of malonyl-CoA formed (same as # cycles) 5. Total loss of ATP per f.a. formed = total net loss per citrate + per cycle + per malonyl-CoA 6. Multiply by 2 per ACP Biochemistry II Guide Page 9 *8: LIPID DERIVATIVES A. Sphingolipids – Serine and Palmitoyl CoA are necessary precursors to ceramide formation (blocked by trans-FAs) – Ceramide is the direct precursor to sphingolipid differentiation – Sphingomyelinase deficiency leads to Niemann-Pick disease: hepato- and splenomegaly & neurodegeneration – Glycosphingolipid enzyme deficiencies lead to an array of neurodegenerative disorders including Tay-Sachs: ganglioside GM2 accumulation, blindness, cherry-red macula, muscular weakness and seizures B. Phospholipids – Comprise membranes, source of arachidonic acid, inositol triphosphate and diglyceride for signal transduction – Phosphatidylethanolamine (PE) and, especially, phosphatidylcholine (PC, aka lecithin) made via CTP are the most abundant phospholipids in most eukaryotic cells. These are further altered and incorporated into surfactant. (Phosphatidylcholine is directly indicative of surfactant levels.) Thus, choline is an essential dietary nutrient (~550mg for men, ~420mg women) to supplement de novo synthesis in order to prevent respiratory distress syndrome. C. Phospholipases: Integral proteins that are specialized to move fatty acids across membranes – PLA1 (C1-acyl group removal) – PLA2 (C2-acyl group removal)** – PLC (breaks glycerol-phosphate bond) – PLD (breaks bond of “head group,” mostly in plants) **Note: The FA usually associated with C2 of phospholipids in membranes is arachidonic acid. PLA2 is associated with many hormones (epinephrine, thrombins, angiotensis II, etc) and is inhibited by glucocorticoids (ex: cortisol). D. Eicosanoids – Family of 20 carbon molecules derived from fatty acids that function similar to hormones – Made in all tissues, but non-systemic (which is why drugs that act on this pathway systemically can have negative effects) – 2 groups: 1. Paracrine 2. Autocrine (NOT ENDOCRINE!) – 5 types: 1. Prostaglandins (PG) 4. Lipoxins 2. Thromboxanes (TX) – induce clot formation 5. Epoxides – made in the brain by Vitamin C 3. Leukotrienes (LT) – mediates allergic responses – Functions: Inflammatory response, Na+ and K+ reg., blood clotting, regulate smooth muscle contraction in uterus and intestine, blood pressure, modulators, vasoconstrictors, vasodialators, bronchoconstriction, bronchodialation, etc. Biochemistry II Guide Page 10 3 Major ways to produce: 1. Omega 6, 2. Omega 3 & 3. Cytochrome P450 (requires Ca++) G. Arachidonic Acid and COX-1 INHIBITORS – Lack of arachidonic acid leads to asthma, BP, neurological problems, and constant inflammation – COX-1+COX-2 inhibitors: anti-inflammatory >> Any molecule that gives off an acetyl group has a tendency to inhibit an enzyme (ex: acetaminophen) – COX-1 functions to maintain healthy gastric tissue, homeostasis and platelet aggregation. COX-2 produces the inflammatory response. Many anti-inflammatory drugs inhibit both pathways. Systemic inhibition of COX-1 can lead to asthma attacks or intestinal bleeding. Specific COX-2 inhibitors (ex: colecoxib) reduce these problems. H. Prostaglandins and medicine – Drug analogs to PGE1 and PGE2 suppress gastric secretion of HCl by blocking type 2 histamine receptors >> increases rate of healing of gastric and duodenal ulcers – Analogs of PGE1 decrease blood flow from the penis >> used in erectile dysfunction – Analogs of PGE2 and PGF2 stimulate uterine muscle contraction and labor >> lowers postpartum bleeding – *9: Ketosis/Ketogenesis A. Ketones are important peripheral tissue energy. There are 3 kinds of ketones: Acetoacetate, 3-hydroxybutyrate & Acetone B. Ketone bodies are: – Very soluble in aqueous solution, can cross all membranes – Produced solely by the liver when excess acetyl CoA’s are available – Used when starving, as a last effort to keep organs alive and send glucose to the brain. (During a fast, the liver is flooded with FAs mobilized from adipose tissue. The resulting elevated NADH and acetyl CoA d/t FA degradation inhibits PDH and stimulates pyruvate carboxylase toward gluconeogenesis, resulting in a channeling of acetyl CoA to ketone body synthesis.) C. Formation of ketone bodies by the liver – Acetoacetyl CoA is first formed from a reverse thiolase. Acetyl CoA Acetone Acetoacetyl CoA + Acetyl CoA HMG CoA* Acetoacetate HMG CoA synthase MG-CoA Lyase 3-HB + NAD+ *HMG-CoA is the de novo precursor of cholesterol I. Use of ketone bodies by peripheral tissues – occurs primarily during fasting in non-hepatic tissue where there’s a low NADH:NAD+ ratio 3-HB acetoacetate + NADH acetoacetyl CoA 2x Acetyl CoA >> TCA cycle** 3-HB Dehydrogenase Thiophorase* Thiolase *Thiophorase is unique to the peripheral tissue (not found in the liver) **The OAA cannot come from glucose (because there is very little), so it comes from amino acids (protein) J. Ketoacidosis; Occurs in diabetes mellitus type-1 or when insulin levels fall d/t prolonged fasting – High fatty acid degradation leads to overproduction of acetyl CoA, and subsequently ketone bodies, while depleting the NAD+ pool and increasing the NADH pool in the liver, which slows the TCA cycle. Ketone bodies also slowly leak protons, contributing to a slightly more acidic environment in the blood – Gluconeogenesis is stimulated and then they become hyperglycemic very quickly, possibly leading to coma. Biochemistry II Guide Page 11 – – • Too much glucose in blood, but no insulin >> Glucose spills into urine and takes K+ with it. They become hypokalemic, causing palpatations and arrethmeas. Sx: a fruity odor on the breath resulting from high acetone levels; dehydration occurs d/t ketone excretion in the urine Tx: Deep breathing in attempt to make body more basic by expelling CO2 and go to the Emergency Room! *10: CHOLESTEROL SYNTHESIS A. Cholesterol precursors: acetyl-CoA and acetoacetyl-CoA. B. Site of synthesis: cytosol, predominantly in the liver and intestine (but not limited to these) C. Other details: HMG-CoA containing isoprene* units is an intermediary. The 3-hydroxy-3-methyl glutaryl CoA reductase (HMG CoA reductase) enzyme is the rate-limiting step and the entire process runs on NADPH (recall HMP’s G-6-PD+6-PG & Malic Enzyme are the sources of NADPH). Eventually, cholesterol is esterified to form bile salts, vitamin D and steroid hormones. – *FYI: Isoprene is the subunit that gives CoEQ10 its lipid-like qualities. CoEQ10 is the only lipid like coenzyme. D. Primary Bile Salts: Cholesterol is a xenobiotic in humans because it cannot be broken down into CO 2 and H2O. Therefore, it must eventually be transported by LDLs and conjugated with glycine and/or taurine* by the liver to become primary bile salts. These primary bile salts then travel down the common bile duct to the duodenum where they become secondary bile acids/salts by the intestinal flora for excretion. Only if lacking intestinal bacteria (i.e. high antibiotic intake) will the cholesterol be reabsorbed. – *Clinical Note: Taurine is synthesized by dietary lysine. Those with hypercholesterolemia need lysine in order to aid cholesterol conjugation. Gallstones form when cholesterol is consumed in such excess amounts that all of the cholesterol cannot be conjugated and some comes out of solution to form aggregates in the gallbladder. i. Tx: High-Intensity Focused Ultrasound (HIFU) E. Vitamin D: the gene regulating “vitamin” – Based on phosphate levels, its primary roles are to up-regulate the gene products that transport calcium out of the cell into the lumen and to aid the work of parathyroid hormone (i.e. vit D increases serum Ca2+ levels when phosphate is low). – In the dermal/epidermal layer, light and heat combine and alter 7-Dehydrocholesterol (7-DHC, Previtamin D3) to cholecalciferol, which then travels to the liver where it is altered to 25-(OH)D by hepatic 25-hydroxylase. The altered 25-(OH)D reaches the kidney, from which active vitamin D (calcitriol, 1,25-(OH)2D) is formed by 1,25dihydroxycholecalciferol hydroxylase. – If the body’s vitamin D needs are low, D3 stays in the skin and becomes super hydroxylated to αglobulins or in the kidney to 24,25-(OH)D, which are eliminated by the kidneys, making it hard to obtain toxic levels of vit D. Biochemistry II Guide Page 12 Clinical Notes: i. Hereditary lack of vitamin D has been linked to colorectal cancer. Such patients need high fiber diets. ii. Low vitD causes rickets in children. Occurs before epiphyseal plates close, so disorientation and hypertrophy of chondrocytes results. iii. Low vitD causes osteomalacia in adults (after epiphyseal plates closed) so it doesn’t cause deformities but does cause osteopenia (decrease in opacity). Skeletal demineralization and deep bone pain ensue. iv. Alkalosis: As Ca2+ is bound to free phosphate in COPD patients, the body thinks it has low levels of calcium and stimulates active vitamin D release from the kidneys. Dx: ionized Ca2+ blood test F. Steroid Hormones – Aldosterone: see the next section G. Cholesterol and Drugs – Drugs used to inhibit cholesterol synthesis include competitive inhibitors of HMG-CoA Reductase. Examples include various statin drugs such as lovastatin (Mevacor) and derivatives (e.g., Zocor), Lipitor, etc. A portion of each statin is analogous in structure to mevalonate or to the postulated mevaldehyde intermediate. H. Calcium and Phytate – In many plant foods, phytates inhibit absorption of some metals such as calcium and iron. Phytates are denatured by heat, thereby allowing absorption of the metals. So, cook your vegetables! – *11: RAAS & ALDOSTERONE RAAS: Renin Angiotensin Aldosterone System: for increasing blood pressure A. 2 organs most associated with blood pressure: Adrenal glands + Kidneys B. What alters blood pressure? – Poiseuille’s Law > tube constriction leads to ↑ pressure – H2O follows Na+, so high Na+ in the arteries increases volume and, therefore, pressure C. The process of RAAS in response to low blood pressure Low BP Renin gene upregulated Angiotensinogen activated – Angiotensinogen is broken down into angiotensin I and angiotensin converting enzyme (ACE) – Angiotensin I is converted to angiotensin II by ACE i. angiotensin II is a vasoconstrictor and stimulates adrenals to produce aldosterone – In the kidney, aldosterone: i. Increases Na+/K+ATPase pump activity >> stimulates TCA cycle to produce more ATP (for pump) >> stimulates Na+ re-absorption back into the blood >> H2O follows Na+, so H2O will flow into capillary, increasing volume and raising BP. D. Oncotic and Hydrostatic pressures – Oncotic pressure is the force exerted by protein (albumin) pushing H2O back into the capillaries Biochemistry II Guide Page 13 Hydrostatic pressure is (essentially) the force exerted by the rate of flow in the capillaries. Hydrostatic pressure pushes H2O out at the entrance of the capillaries. – If hydrostatic exceeds oncontic then the interstitial fluid experiences ascites or edema – If oncotic exceeds hydrostatic then the capillaries swell and experience hypertension E. Clinical Notes: – Common Blood Pressure medications: i. ACE inhibitors: Blocks angiotensin II production, but results in Na+/K+ imbalance. Excess K+ (hyperkalemia) results in cramping, tachycardia, and arrhythmias ii. Anti-Diuretic Hormones (ADH) – removes Na, water follows iii. Beta-Blockers – slows heart beat iv. Angiotensin II receptor blockers – prevent effects of angiotensin II v. Calcium Channel Blockers – keeps blood vessels from constricting – Anionic Gap i. Lab analysis that shows how much of the various proteins and electrolytes are in the blood. ii. The greater the gap b/w anions (phosphate, sulfate, protein, etc) and cations (K+ and Na+), the more likely the pathology of a traumatic internal disruption (renal failure or ketoacidosis). – *12: PROTEINS A. Categories – Structural proteins are those with the primary purpose of producing the essential structural components of the cell. – Soluble proteins are those that stay in solution. B. Protein sources: Egg whites are digestible 97%, most meats are 85% and up, wheat and plant proteins are 75-90% C. Structures: – Primary – translated/assembled sequence, is translated from the amino end to the carboxyl end – Secondary - folding (ie β-sheets and α-helices) by disulfide or H-bonds while side groups attach. This step is where toxicities have their effects, which is especially dangerous in early fetal life when lots of translation is going on. i. Stabilized by: hydrophobic interactions, ionic bonds, H-bonds, Van der Waals forces – Tertiary - 3 dimensional folding – Quaternary - multi subunit (ie hemoglobin and control enzymes) – Clinical Notes i. Amyloidoses: Protein misfolding can result in accumulation of irregular proteins, collectively called amyloids. Such accumulations have been implicated with Alzheimer disease. Misfolding can occur because of genetic, environmental or spontaneous reasons. Most cases of Alzheimer disease are not genetically based, but instead result from proteolytic cleavages from the larger amyloid precursor protein. Secondarily, neurofibillary tangles containing irregular tau proteins form in Alzheimer disease. D. Chromophore: vitamin or mineral added to protein to give color (otherwise colorless) i.e myoglobin, hemoglobin, FAD, FMN. E. Peptide Bond – Joins adjacent amino acids and allows for 360o rotation around the bond (can be hindered by side groups) – Dehydration rxns can occur between the nitrogen and carboxyl Biochemistry II Guide Page 14 F. Nomenclature – Name from amino end (N-terminal) to carboxyl end (C-terminal) – Name all the a.a. except for the final group by dropping the suffix and adding -yl – ie: glycine, arginine, cysteine >> glycylarginylcysteine G. Ways to denature proteins 1. Dehydration 5. Pressure 9. Pesticides 2. Heat/Cold 6. Chemicals 10. Neurotoxins (snake venom) 3. Radiation 7. Vibration energy (microwaves) 4. altered Ph 8. Herbicides H. Zymogen (Proenzyme) System – This is the “daisy-chain” cascade of events necessary to acquire the proper pH’s for various enzymes of digestion that break protein into amino acids – Substances that alter pH (ex: Tums) will seriously affect this cascade. Also, a lowered pH results in low serum pH, which causes Ca2+ to bind to phosphate, leading to “low” serum Ca2+ and eventually osteomalacia d/t active vitD. – Generally, the more nitrogen on a molecule the more basic, and the more side chains the more acidic. The closer the pH is to the isoelectric point, the more likely that a molecule can cross the cellular membrane. (Zymogens help this) – The process: 1. In Stomach a. Parietal cells produce HCL triggered by thought of food. (Not a significant proteolytic substance) c. HCL stimulates pepsinogen secretion from chief cells, which cleaves its peptide bonds to become pepsin (the first active enzyme). Pepsin then sets up a pH gradient for the zymogen system to work. d. Pepsin’s products are referred to as peptones (poly-peptides and oligopeptides) & are at a pH of 1.7-2. e. Leaves stomach as chyme. 2. In Duodenum a. Peptones stimulate release of inactive trypsinogen (the first enzyme in the duodenum) from the pancreas. b. The low pH stimulates secretin, which causes release of HCO3- from the pancreas and Brunner’s glands. c. 3 ways to activate trypsinogen to trypsin i. Low Ph (from HCL) ii. Enteropepsidases – from enterocytes’ own enzymes (trypsin, chymotrypsin, elastase) iii. Autolysis (self activation) – a form of positive feedback d. Trypsin i. Cleaves peptide bonds in which the carboxyl group is contributed by arginine or lysine. ii. Trypsin also activates other proteolytic enzymes like procolipase (>>lipase) & phospholipaseA2 1. Endopeptidases cleave from the center while exopeptidases cleave from the ends Biochemistry II Guide Page 15 *13: AMINO ACIDS A. Amino acids (AA) are easily ionized in aqueous solution as they are a zwitterion (dipolar chemical structure w/ a + and – charge), which makes the AA form crystals w/ a high decomposition temp (>200oC) B. Most life is based on about 20 amino acids and these are the sole source of nitrogen in the body C. Structure – All have the same carboxyl and amino group basic structure except for imino amino acids – Only the L enantiomer is bioavailable to the body, a few A.A. may be converted D>L by the liver D. Transport – Intestinal transepithelial cells are cotransported w/ Na+ – A.A. are pumped in to the cell while Na+ ion is pumped out to the interstitial tissue – Glutamyl-Glutathione cycle is utilized in the kidney and intestine (see diagram) 20 Amino Acids Neutral R Groups Aliphatic Branched Chain Alanine Glycine Valine Leucine Isoleucine A.A.g Glycine (Gly, G) (the simplest) Alanine (Ala, A) Aromatic Group Imino Tryptophan Phenylalanine Tyrosine Hydroxy Group Sulfur Group Basic Group Acidic Group Serine Threonine Cysteine Methionine Lysine Arginine Histidine Glutamate Aspartate Glutamine Asparagine Proline Formed by Acetic acid Essntl? No Pyruvate No Valine (Val, V) Yes Leucine (Leu, L) Yes Isoleucine (ILE, I) Leucine Yes Proline (Pro, P) Glutamate No Phenylalanine (F) Tyrosine (Tyr, T) Alanine Phenylalani Yes Only Biochemistry II Guide with Characteristics Aliphatic, Hydrophobic, Non Polar, Used to conjugate (for detoxing). @ a neutral PH = zwitterion Aliphatic, Hydrophobic, Non Polar. Used to regulate blood sugar levels and/or in gluconeogenesis. Aliphatic, Hydrophobic, Non Polar, Branched Chain AA Aliphatic, Hydrophobic, Non Polar, Branched Chain AA Aliphatic, Hydrophobic, Non Polar, Branched Chain AA Aliphatic, Hydrophobic, Non Polar. Formally not an AA but is an Imino. Neutral, Non Polar, Aromatic Aromatic, Non Polar, Hydrophobic Derivatives *Creatine (w/ Arg), Glycine NT, Glutathione (w/ cysteine + glutamate), and Porphyrin rings. *Interconvertable with serine. *Phenylalanine. *Associated w/ muscle breakdown (2nd most common AA when exercising, 1st = glutamine) *Metabolized in intestine *Generally buried in folded proteins. *Metabolized in intestine. *Interchangeable with isoleucine. *Plays central roles in ligand binding and protein stability. *Metabolized in intestine. *Causes bending in peptide bond bc it cannot donate H. *Rapidly produces tyrosine via hydroxylase enzyme. *Thyroxine (T3,T4>thyroid hormone), Melanin pigment Page 16 ne Tryptophan (Trp, W) (largest) Methionine (Met, M) Alanine Serine (Ser, S) Lysine phenylalanine pathology Yes Yes Non polar, contains sulfur. Necessary for proteins and connective tissue. No Polar, Hydrophilic. Inhibited by alcohol. Polar, Hydrophilic. Inhibited by alcohol. Polar, contains sulfur. Important in connective tissue. Positive Charge, Basic, Polar. Common in enzyme catalyzed rxns. Increases membrane fluidity. Polar, Positive Charge, Least Basic Threonine (Thr, T) Yes Cysteine (Cys, C) No Histidine (His, H) Yes Lysine (Lys, K) yes Arginine (Arg, R) Glutamate semialdehyde Aspartate (Asp, D) OAA Glutamate (Glu, E) Asparagine (Asn, N) Glutamine (Gln, Q) Aspartate Glutamate in peri. tissue Based on Energetics Nonessential Essential Biochemistry II Guide Aromatic. Non polar Yes, young/old and individuals with trauma or pathologies. no Positive Charge, Basic, Polar. no Polar, Negative Charge, Acidic (1 of 2 acidic AAs (aspartate)). Early absorption. Polar, Amide, Neutral Polar, Amide, Neutral. Involved in Ntransport & cellular glucose uptake. no no Polar, Negative charge. Acidic (1 of 2 acidic AAs (glutamate)). Early absorption. *Neurotransmiters: Epi, Norepi, L-Dopa *Hydroxylase, RLE, Protein *2% to formation of NAD+ *TryptophanSerotonin Melatonin *Spermidine and Spermine. *Required for SAMe: Sadenylsyl methionine (to make epi and norepi) *Aids sphingolipid-ceramide production (along with palmitoyl CoA). *Interchangeable w/ glycine *Glutathione *Taurine Can serve as acid or base (depending on protonation of imidazole) >> has N- that are NOT ionizable *Histamines *Participates in active centers of enzymes. *Carnitine and creatine. *Creatine (with Gly), NO * Important role in N metabolism (urea cycle) *Imp in enzymes active centers and in maintaining solubility and ionic character of proteins. *Transaminated to oxaloacetate for TCA. *Good carrier of N, & adds second N to Urea formation *Transaminated to α-ketoglutarate for TCA. *Good Ncarrier (2nd to glutamine). *makes GABA, Proline, Glutamate NT, glutathione *Common site for attachment of carbs in glycoproteins *MOST COMMON AA in the blood. *Major nitrogen carrier *Glutaminase degrades glutamine in the liver. Glucogenic Glucogenic and Ketogenic Ala, Asn, Asp, Cys, Glu, Gln, Tyr Gly, Pro, Ser Arg, His, Met, Thr, Val Ile, Phe, Try Ketogenic Leu, Lys Page 17 Mneumonics The 10 Essential Amino Acids – These Ten Valuable Amino Acids Have Long Preserved Life In Man: Threonine, Tryptophan, Valine, Arginine, Histidine, Lysine, Phenylalanine, Leucine, Isoleucine, Methionine. The Basic Amino Acids – Basically, HIST Are Lies: Histidine, Arginine, Lysine Aromatic Amino Acids HTTP: Histidine, Tryptophan, – Tyrosine, Phenylalanine Branched Chain Amino Acids – Isoleucine, Leucine, Valine Sulfur containing Amino Acids – ScuM: Sulfur, Cysteine, Methionine Aminos with OH side groups – SHOTT: Serine, OH (backwards), Tyrosine, Threonine Hydrophobic Amino Acids – Pro GAV PIL: Proline, glycine, alanine, Valine, Phenylalanine, isoleucine, leucine Hydrophobic Neutral Amino Acids – Girls Are Very Loving If Men Can Prepare Perfect Tea: Glycine, alanine, valine, leucine, isoleucine, methionine, cysteine, proline Positive Amino Acids – Alexander Graham Spoke Through the Telephone: Asparagine, Glutamine, Serine, Threonine, Tyrosine Neutral Aminos – Laurel And Hardy: Lysine, Arginine, Histidine Clinical Correlations (covered later in nutrition) – Branched Chain Aliphatic AA Dehydrogenases (BCAA’s)—improper breakdown in the skin causes serum and urine accumulation that presents with a sweet smell. This is maple syrup urine disease and is testable directly following a meal. a. BCAA’s are also used in Tx of burn victims and supplemented with bodybuilding b/c BCAA’s cause insulin release b. Because creatine is directly related to muscle mass, MS patients can measure creatine levels to indicate treatment progress –or—kidney patients can measure it as a “renal clearance test” to indicate renal function – Glutamine—The MOST COMMON amino acids in the blood. Glutamine is scientifically proven to protect and heal enterocytes > helps prevent damage from chemotherapy. Used in treatment of alcoholics to decrease cravings and help GI tissue. – L-phenylalanine—Makes norepi, which keeps people awake and alert; reduces hunger; antidepressant. DLPA also makes PEA (phenylethylamine)--acts like amphetamine (found in chocolate). Used for pain, depression. a. High concentration (hydroxylase deficiency) can be d/t phenylketonuria (PKU), which is highly neurotoxic d/t specific enzyme activity at the higher concentration. This is the most prolific pathway for genetic disease, including alkaptaneuria (black urine disease). Biochemistry II Guide Page 18 – – – – – – – – – – – b. High concentrations can lead to high BP, which is why statin drugs also work against this amino acid. L-tryptophan—Best to supplement 5-HTP (which is downstream of the NAD+ split and ensures serotonin production)— calmative, helps with appetite, induces sleep (serotonin becomes melatonin—sleep hormone, anticarcinogen, antioxidant). Give with B-6. Cortisol interferes with 5-HTP serotonin. Thus, hard to fall asleep or stay asleep when one is very stressed Lysine—herpes antiviral; helps calcium absorption, helps form collagen. Arginine—bad for herpes, but good to form Nitric Oxide and bring down blood pressure levels or help with erectile dysfunction. Good for muscle growth and repair (so used by body builders). Detoxifies urea. L-carnitine—used to help fat metabolism, especially regarding the heart to give it energy as it brings fatty acids inside the cell to the mitochondria; used for many heart ailments, such as failure, arrhythmias & prolapsed mitral valve. Used also to improve athletic performance; male infertility; DM. 1-4 gms.day. Made from lysine and methionine. L-acetylcarnitine used in Alzheimers Cysteine—needed for liver detoxification, as sulfur donor; also bronchial problems, hair loss. NAC used to create glutathione, main antioxidant in liver and lung (also found in eyes, pancreas, kidneys, etc) and also a mucolytic to decrease mucous build-up in upper respiratory system. Need selenium for glutathione. Cysteine 500-5000 mgs/day. a. Glutathione must be acetylated (with proanthrocyadine) or given as liposomal glutathione (which travels in chylomicrons) to prevent oxidation in the blood b. Glutathione is responsible for transporting proteins and reducing amyloid protein concentrations 1. Amyloids are made from prions when under oxidative stress Glycine—winds up increasing brain glutamate receptors which promote calming effect. Also produces bile salts (help prevent gallstones). Forms glutathione with cysteine and glutamate. Methionine—main sulfur donor in the body: turned into SAMe which is the main methyl donor of the body, needed for production of just about everything—adrenal hormones, neurotransmitters, help liver detox in glucuronidation pathway (recommended therefore in Gilbert’s patients): breaks down estrogens; carnitine, choline, creatine, epi, melatonin and nucleic acid synthesis, degradation of histamine. High in sunflowers and meat products. Methionine metabolism causes the creation of homocysteine, which needs B6/B12/Folic Acid/DMG to be turned into cysteine or back to methionine. Hyperhomocysteinemia is associated with atherosclerosis development and increased risk of CVD. SAMe is used for depression, O/A, Detoxification. Taurine—Another sulfur amino acid. Used to help liver detoxify in CYP 450 system. Used for CHF in patients and other CVD; macular degeneration. Used to help make bile salts (for fatty digestion and toxin excretion). Used as anti-epileptic to stabilize neural membranes. Very helpful in patients with DM as it is involved in all aspects of blood sugar regulation. Cysteine—High in skin and hair. Has antioxidant properties. Histidine—high in hemoglobin and used in some diseases like R.A., allergies, ulcers. Tyrosine—precursor to norepi, epi and dopamine. Needs folate, Vit C and copper. Used for depression, narcolepsy, decreased appetite, thyroid hormone production. Supplement when under high stress. a. Deficiency: low energy, could be indicative of PKU b. Supplementation must be monitored for blood pressure b/c high dopamine causes high BP *14: UREA CYCLE / ORNITHINE CYCLE A. We cannot store a.a. for energy, so proteins are continuously turned over. However, this generates harmful nitrogen. B. Liver, Kidney, and Intestines (250-300g/day or ½lb/day) are the major nitrogen turnover/removal sites. Biochemistry II Guide Page 19 Protein Degradation C. Muscle tissue: – Protein broken down NH4 released while Carbon and Oxygen are used in metabolism – NH4 + α-ketogluterate Glutamate i. Enzyme: glutamate dehydrogenase with NADPH -> NADP+ – Glutamate + Pyruvate Alanine + α-ketogluterate i. Enzyme: Alanine aminotrasferase with Pyridoxal phosphate – Alanine then carries the added Nitrogen in the blood to the liver D. Other tissues: – Protein broken down NH4 released while Carbon and Oxygen are used in metabolism – NH4 + glutamate Glutamine i. Enzyme: Glutamine synthetase with ATP and Mg2+ – Glutamine then carries the added Nitrogen in the blood to the liver for the Urea cycle i. Note: glutamine is the major carrier of N in the blood E. Alanine breakdown in the liver – Alanine + alpha-ketogluterate pyruvate + glutamate + NH4 i. Enzyme: glutamate dehydrogenase with NADPH NADP+ – If acetyl-CoA is high, and therefore so is energy, pyruvate predominantly enters gluconeogenesis – NH4 crosses the Mito membranes to enter the matrix F. Glutamine breakdown in the liver – Glutamine glutamate + NH4 i. Enzyme: Glutaminase – NH4 crosses the Mito membranes to enter the matrix Urea cycle G. When the mitochondrial concentrations of acetyl-CoA, NH4 and glutamate are high, the genes for urea cycle proteins are upregulated (making this a forward-driven reaction) H. Urea diffuses out into the bloodstream and is normally excreted by the kidney I. If Kidney problems are present, urea is diverted to the intestines for excretion – Enteric bacteria produce the enzyme urease that breaks down the urea, but may allow for NH4 reabsorption by the gut Biochemistry II Guide Page 20 J. Pharmaceuticals that block this cycle: – Butamide/Phenylbuterate goes to phenylacetate in the body and binds to glutamine to force excretion – Neomycin kills the enterobacteria to prevent urease activity K. Notes: – Ornithine Transcarbamoylase is the first enzyme in the urea cycle (not CPSI), and it, along with argininosuccinate synthetase are the two most commonly damaged enzymes in this cycle. Such patients should limit protein intake, especially D-form. Secondarily, patients should supplement with arginine. – 3 ATP total are used (2 in matrix, 1 in cytosol) – CO2 comes directly from TCA (Not Bicarb ion) – CPSI is stimulated by high NH4 and N-acetyl glutamate i. Acetate + Glutamate N-acetyl glutamate ii. Enzyme: N-acetyl glutamate synthetase, stimulated by ARGININE (a product of the urea cycle) iii. This is why arginine is used as treatment for hyperaminemia (it removes the nitrogen) – Fate of fumerate – converted to malate OAA PEP Glucose by cytostolic malate dehydrogenase Clinical Correlations L. Cystic Fibrosis – Defect in Cl- channels in pancreatic secretory ducts > causes drying of ducts (inspissation) and inability to absorb fats – S/S: steatorrhea, fatigue, irritability, low albumin and TTR 2º to protein malnutrition – Tx: Enteric coated microspheres of pancreatic enzymes M. Hartnup’s Disease – Genetic disease (autosomal recessive) marked by improper transport of neutral AA’s across cell membranes (gammaglutamyl cycle) in intestines and renal epithelial cells (esp. threonine, cysteine, methionine) – Dx: lack of essential a.a. – Sx: Hypoaminoacidemia + Hyperaminoacidemia d/t amino acids spilling into the urine N. Hereditary Hyperammonemia – X-Linked recessive disease – Sx: Cirrhosis of the liver, hepatitis, HIV etc all d/t inability to clear N – Tx: reduce protein in the diet to monitor the N (give animal protein only, b/c it’s L-form whereas plants are D-form), also supplement with arginine to combat the excess N, limit exercise in order to reduce amino acid breakdown O. Cysteinuria – Genetic defect of transporting cysteine and basic a.a. across brush boarder membranes and renal tubules (esp. cysteine, lysine, arginine, ornithine) – May contract kidney stones d/t the insoluble nature of cysteine (Sx: bleeding and pain) – May not show a.a. deficiencies because we can produce cysteine from CYSox and ornithine from the urea cycle Biochemistry II Guide Page 21 *15: AMINO ACID METABOLISM A. AAs may be broken down and inserted into the TCA cycle or used in production of ketone bodies (picture to the right). AA’s will only be used in this manner under low-energy/fasting states. B. Liver Enzymes in Diagnostics – AST – Aspartate Transaminase: Quickly indicative of liver damage. i. Pyridoxyl Phosphate: (Vit B6) Pyridoxyl phosphate (PLP) is important for this transamination reaction. – ALT – Alanine Tansaminase: Takes 11-14 days after liver damage for this to appear detectable in the blood. – ASP – Alkaline Phosphatase: Are often indicated with duct-related cancers (ex: pancreas) C. Histamine Production – Histidine Histamine and CO2 Brain or Peripheral tissue – Enzyme: Histidine decarboxylase need Pyridoxal Phosphate (PLP) – Three classes of Histamine Receptors i. H1 – associated with allergic responses ii. H2 – associated with stomach ulcers iii. H3 – not sure – Histamine is broken down differently in the brain compared to other tissues. In the brain, histamine is not involved with inflammatory responses or ADDH as some might believe D. Creatine and Creatinine – Dervived from Gly, Arg, SamE: is proportional to muscle mass and provides a quick burst of energy – Creatine in the serum is phosphorylated and quickly becomes creatinine by creatine phosphokinase (CPK) – Creatinine in serum is the dead end metabolite and is excreted by the liver – Kidney Function may be tested by the Creatine Clearance Test (related to glomerular filtration rate): measures creatinine excreted over given period of time – Both CPK and Lactate dehydrogenase (LDH) may be used to indicate time post MI (myocardial infarction) i. CPK is high immediately after, but LDH is slower to rise and doesn’t cross the Ck2 line until after 24 hours ii. Walking heart-attack (very dangerous) – CPK levels beginning to clear, but high LDH…long time post MI B. Tyrosine to Melanin Pigment – Occurs in melanosomes in skin – Requires Cu2+ (also for epi, L-dopa, etc) – 2 Types of Melanin Pigment i. Eumelanins – brown/black ii. Pheomelanins – yellow/red – Increases hormonal status during pregnancy Biochemistry II Guide Page 22 C. Thyroid Hormones (stimulated by Tyrosine) – Metabolic Involvement – Endocrine Involvement i. Fatty acid synthase (Acetyl-l-CoA i. HGH – Human Growth Hormone Synthase) ii. TSH- Thyroid Stimulating Hormone ii. Malic Enzyme iii. TR-Thyroid Hormone Receptor iii. Pyruvate Kinase – Mitochondria Involvement iv. Phosphoenolpyruvate Carboxykinase i. Cytochrome C – Cardiac Involvement – Ion Transport Involvement i. Myosin heavy chain + Calcium ATPase i. Na, K, ATPase – Cholesterol and thyroid hormones are very important in brain development through age 4 (myelination, synaptogenesis) – Hypothyroidism >> iodine deficiency can lead to a goiter and, in extreme cases, cretinism – Hyperthyroidism >> Grave’s Disease *16: HENDERSON-HASSELBACH EQUATION A. B. C. D. E. F. G. pH = pKa + log 10 [A-]/[HA] Henderson-Hasselbach equation Purpose: to see what form a solution’s molecules are in at varying pH. Acids: Proton Donor (-COOH) // Base: Proton Acceptor (-NH2) Buffers: anything that resist pH change (serum proteins are buffers) – ranges from +1 to -1 the pKa (the horizontal part) Isoelectric point (pI) – pH where the net charges on a molecule=zero pHm – pH where the charges on the molecule are maximal (look for total number of charges on each species, NOT the net charge) Calculations: 1. Start with the fully protonated, acidic form of the molecule 2. Given the pKa values of each species, look up the corresponding pH values (Note: usually the alpha-carboxyl, side group, then alpha-amino protons come off in that respective order, but not always…look at pH values) 3. Find the Buffering ranges around each pH value 4. Find the pI value for the reaction -count net charges on each molecule, find the one with the net 0 charge -Add the two pH values that the species falls between and divide by 2 to find that species pI 5. Find the pHM value for the reaction -count the total charges on each molecule, find the one with the maximum -Add the two pH values that the species falls between and divide by 2 to find that species pHM. Clinical Notes – Pulmonary Acidosis – more common in COPD patients, may accompany metabolic alkalosis, Tx: Oxygen – Metabolic Acidosis – may accompany pulmonary alkalosis, serum pH is acidic – Metabolic Alkalosis – Ca2+ binds phosphate at higher pH, this activates vit D and PTH >> osteomalacia Biochemistry II Guide Page 23 *17: ENZYME KINETICS A. Describes enzyme activity that are not allosterically controlled B. Specificity depends on atomic arrangement at the active site C. Michaelis-Menten Equation: km= [S] where Vmax/2 – Km – derived under “ideal” conditions, proportional to [S] – Higher the Km = lower the affinity for substrate – Lower the Km = higher the affinity for substrate – Substrate must be the same for both enzymes D. Vo = initial point of reaction – not absolute, only where we start observations E. Vmax = reaction point where curve levels off, is directly proportional to total enzyme [E] concentration F. Zero vs First Order Reactions – [S] < < Km = 1st order and means [S] is proportional to the velocity (the first part of the curve) – [S] >> Km = zero order and means the velocity is independent of [S] (proportional instead to [E] and Vmax) G. Rate of Rxn: v = k2*[ES] (i.e. velocity is related to the Enzyme-Substrate Concentration) – [ES] does not change with time as equal amounts are formed and broken down simultaneously H. Activation Energy – energy required to get the reaction to go, enzymes decrease the activation energy I. Gibbs free energy of activation: G – -∆G = Exergonic (gives off heat/produces energy: plants are exergonic) – +∆G = Endergonic (requires energy: humans are endergonic) Calculations: Vo/Vmax = [S]/km + [S] 1. Pick a point where change on the graph is quicker for Vo and determine the [S] at that point to plug into the equation 2. Pick a point where graph is beginning to level out for Vmax 3. Plug in all values and solve for km (note: only need to compute 1 time because the km for any given rxn is the same throughout) Lineweaver Burk Plot -linearization of the Michealis-Menten Equation -Plotted as the inverse (so interpret carefully) -y-intercept is the inverse of Vmax; x-intercept is the inverse of Km Types of Inhibition: J. Competitive Inhibition – inhibitor binds to the same site as the substrate (Malonate with succinate) – Reversible, Vmax is same, km increases – Why? – appears as though affinity is decreasing (the absolute is, but relative is not) K. Noncompetitive Inhibition – Changes the architecture of an enzyme (ex: heavy metals) – Reversible, Vmax decreases, km is same – Why? –appears as though there is less enzyme, but the enzyme that is still active will make the reaction occur at the same rate Biochemistry II Guide Page 24 L. Uncompetitive Inhibitor – binds when enzyme-substrate complex is formed [ES] “suicide inhibitor” – Irreversible, Km increases (graph shifts righ on x-axis), Vmax decreases (y-intercept raises) – i.e. Arsenic with PGAL dehydrogenase, 5-fluorouracil or methotrexate i. Methotrexate is a folic acid scavenger, thereby blocking single-carbon (homocysteine - SAMe) metabolism and uracil production. Folate-dependent 1-carbon reactions are important in amino acid metabolism and in biosynthetic pathways leading to DNA, RNA, membrane lipids and neurotransmitters. ii. Side effects: megaloblastic anemia, neutropenia, increased risk of bruising/vomitting, dermatitis iii. Folic acid deficiency presents w/ neurological problems like dementia, Alzheimer’s and Parkinson’s, which contrasts B12 deficiency which can have anemia w/o the neuro probs. *18: NITROGEN METABOLISM / OPIOD GENE NITRIC OXIDE A. Previously termed Endothelium-Derived Relaxation Factor (EDRF) B. Is a gas released by epithelial cells in lumen of blood vessels or by retinal cells C. Paracrine effect – on smooth muscle cells of blood vessels or retinal cells D. Arginine is the precursor – Need: Riboflavin, tetrahydrobiopterin, niacin, thiamine E. Process of effect on tissues – Retinal cells: stimulates guanyl cyclase to convert GTP to cGMP – Non-retinal cells: stimulates protein kinase G, which is a Ser and Tre derived protein w/ an unknown substrate F. Synthesis – Enzyme: NO synthetase (CytoP450-like heme structure) – High levels associated with septic shock (hypotension) d/t vasodilation G. Controls: – Activated by Ca2+/calmodulin and Acetylcholine – Cytokines and bacterial endotoxins produce high levels of NO H. Carbon Monoxide gas – Has similar effect as NO, but is not broken down as fast – found in the brain as a hormone OPIOD GENE A. Opiod peptide biosynthesis occurs in subdermal tissue and intestine B. One opiod gene, but has subgenes that code for different proteins: (contrasts idea of 1 gene per 1 enzyme) – Upregulated by melanocyte stimulating protein, ACTH C. Endorphins/Encalphin relation to mind-body medicine, acupuncture, and homeopathy Biochemistry II Guide Page 25 *19: PORPHYRIN RINGS A. Essential molecular structure in life, used to carry heavy metals (ex: iron) throughout the body B. Structure contains lots of nitrogen and side groups C. Involved in: – Electron Transport Chain – Cytochrome P450/B5 systems (endocrine system, detoxying system) – Plants with photosynthesis – Hemoglobin D. Lead is catastrophic inhibitor in the formation of porphyrin rings (delta-ALA dehydrase) (Sx: chronic fatigue) E. Pathologies: Porphyrias – Erythropoietic (defect in RBCs) or Hepatic (Defect in liver) – Autosomal dominant (All generations show this pathology) F. Synthesis: occurs in the liver mostly, and also in erythrocyte producing cells of bone marrow – Begins in mitochondria as a grouping of glycines and succinyl CoAs delta-aminolevulinic acid synthetase* wraps the chain into a ring on the mitochondrial outer membrane-cytosolic surface iron (Fe) is added to the center of the ring by ferrochelatase in the inner mitochondria i. *delta-aminolevulinic acid synthetase is directly targeted by lead poisoning – Hemin (porphyrin rings w/o iron) is a feedback inhibitor of delta-aminolevulinic synthase (ALA) i. Hyperporphyria presents similar to bipolar/rage w/ or w/o dermatitis disorders, Tx: Hemin IV’d – need pyridoxal phosphate for 1st rxn G. Porphobilinogen is first molecule in cytosol Clinical Disorders A. Hashimoto’s Disease: Autoimmune disease causing hypothyroidism d/t inflammation of the thyroid B. Addison’s Disease: increase in melanin pigment 2º to elevated ACTH C. Albinism: difficulty transporting tyrosine from cytosol to melanosomes in melanin pigment D. Sickle cell anemia – catastrophic destruction of RBCs causing an over burden on liver and spleen (hepatomegaly and splenomegaly) E. Hemolytic Anemia: problems with glycolysis in RBC, ultimately leads to Jaundice – Hemolytic Anemia of the newborn (Erythoblastosis Foetales) F. Myasthenia Gravis – Sx: muscle weakness, may effect ocular muscle and cause diplopia (double vision) – Develop IgG antibodies against nicotinic receptors at neuromuscular jxn G. Hemolytic Jaundice – Is a response to sickle cell anemia that can lead to erythoblastosis foetales d/t glycolytic enzyme deficiencies – The splenomegaly is generally the cause of death (not the hepatomegaly) H. Hepatocellular Liver damage – Cirrhosis, hepatitis – Urine dark, stools pale (liver regurgitates conjugated bilirubin into blood and then into urine) – Elevated AST (SGOT) and ALT (SGPT) Biochemistry II Guide Page 26 *20: HEMEGLOBIN/HEME BREAKDOWN/BILIRUBIN A. Vast majority by bulk in the blood, contains: porphyrin ring, Fe, Nitrogen, (O2) B. Formation requires Fe absorption along with Cu, Ceruloplasmin – Cupric to cuprous (Cu++ Cu+), ferrous to ferric (Fe++ Fe+++) – Requires Vitamin C C. Structure: 4 subunits from 4 genes = α 1 + 2 (chromosome 16), β 1+2 (chromosome 11) with a central porphyrin containing Fe D. Breakdown: NADP/Heme oxidase in the peripheral tissue (when injured), spleen and mostly the liver – Glycophorin is a surface protein that triggers destruction of porphyrin rings – First product is biliverdin (open ring responsible for a bruise’s green hue) and Fe+++ is carried in the blood by transferrin – Biliverdin plus CO yields bilirubin (the red hue in a bruise) in the liver by biliverdin reductase, which requires NADP from the HMP pathway E. Bilirubin – Because bilirubin is a xenobiotic, it requires conjugation by the cytochrome p450 system using glucoronyl transferase, which adds two glucoronyl molecules making the bilirubin water soluble – In the gut, bilirubin produces urobilinogen, which is absorbed by and carried to liver to produce the urobilin, which is responsible for the yellow color of urine – Large intestine has more microbial enzymes that produce stercobilin, which gives the characteristic brown color F. Action: Hemoglobin brings in oxygen at lower partial pressure than the lungs, but higher than myoglobin – Acidity, CO2 and 2,3-bisphosphoglycerate cause release of O2 from hemoglobin i. This constant exchange of gases is called the Bohr effect and it involves carbonic anhydrase, a very zinc dependent enzyme, that facilitates the movement of oxygen from blood and to the peripheral tissue – Myoglobin, in muscle tissue, has a lower partial pressure in order to bind O2 from hemoglobin, it also prevents oxidation by a free radical O2 G. Fetal Hemoglobin – No β-hemoglobin genes in fetus; rather, α/zeta/epsilon/gamma subunits are present that look more like myoglobin and keep a lower partial pressure that allows diffusion of O2 from mother’s blood to fetus – α1+2-hemoglobin subunits are upregulated during development in order to prepare for birth, β-hemoglobin subunits get turned-on only postnatally. If child is born and has persistent fetal hemoglobin, it can be lethal: i. 2 Types of disorders 1. α-thalassemia: more severe, fatal in fetal life 2. β-thalassemia: very common, mixed forms, ranging from negligible to fatal, jaundice Biochemistry II Guide Page 27 H. Hemoglobinopathies: – Hypochromic Anemia – Pale, small RBC’s because low levels of hemoglobin, associated with low iron levels – Hemochromatosis – excess Fe in the blood 2º to saturation of transferrin, NOT a fetal disease although it presents similar to the thalassemias >> recall role of ferrous (Fe++) > ferric (Fe+++) > ferrous (Fe++) forms in the body utilizing copper, transferrin, ferritin and hemosiderin i. 4 levels of hemochromatosis: Genetic marker is ferroportin protein that shuttles Fe intracellularly Nucleic Acid Metabolism A. Provide little energy B. Source: botanicals C. HMP pathway makes ribose sugars Biochemistry II Guide Page 28