Lecture Slides for Fatty Acid Catabolism
advertisement

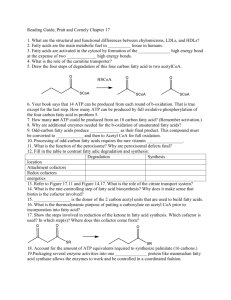
Lipid Catabolism CH339K Fats are stored in lipid droplets Lipid droplets in a rat adipocyte Glucagon Epinephrine Human Serum Albumin • 30-50 g/l of blood • 67 kDal • 585 amino acids • Can bind up to 10 fatty acids • Different binding sites have different affinities • Also binds thyroid hormones FADL – An E. coli Fatty Acid Transporter 1) 2) 3) 4) b-Barrel Transmembrane Protein 14 Antiparallel b-sheets N-terminal “hatch” domain Conformational change on substrate binding opens hatch a) Ribbon drawing of intact protein b) “Hatch” domain c) Cutaway view to show hatch in central channel d) Cytoplasmic space-filling view to show hatch plugging channel van den Berg, B. (2005) Current Opinion in Structural Biology 15(4): 401-407. Fate of Glycerol • Not wasted • Shuttled to liver in blood • Catabolized there Glycolysis Gluconeogenesis Activation of Fatty Acids Overall: Keq = 1589 Keq = 337 Keq = 535,000 Transport into the Mitochondrion (Carnitine-Acylcarnitine Translocase) b-oxidation • Mitochondrial matrix • Oxidizes fatty acyl CoA’s at the b carbon • Sequentially cleaves off acetyl CoAs • Acetyl CoA is processed through Krebs and ETC 2 Systems for b-oxidation • ≥ 12 carbons: • TFP – last 3 enzymes in multienzyme complex • < 12 carbons • 4 soluble matrix enzymes • Palmitate weighs ~256 g/mol (about 42% more than glucose) • Oxidation yields 108 ATPs, versus 32ish for glucose (about 340% more) Monounstaurated Fatty Acids • Need one extra enzyme • Converts double bond 1 Polyunsaturated Fatty Acids • Need two extra enzymes • Reduce conjugated double bonds to a single double bond 1 2 1 Odd-numbered Fatty Acids • • • • Left with 3 carbons Add inorganic carbon Convert to succinate Throw into Krebs Cycle Pernicious Anemia • B12 is produced only by several genera of bacteria, obtained from animal food • daily requirement is about 2-3 mg/day • Gastric mucosa produces a protein called intrinsic factor • Lack of intrinsic factor results in impaired B12 absorption, pernicious anemia, death in 1-3 years • Original treatment (1920’s) was ½ lb. of raw liver daily • Concentrated liver juice (yum) became available in 1928 • B12 isolated in 1948, synthesized in 1973 • Now treated with large doses (several mg) B12 • Sources: fish, meat, poultry, eggs, milk, especially liver and mollusks (clams, oysters, etc.) Liver Juice! Ummm!!! Regulation (ACC = Acetyl CoA Carboxylase) Peroxisomes • b-Oxidation also occurs in peroxisomes (major site in plants) • In critters, peroxisomes are primary organelles for oxidation of very long chain and branched fatty acids (cerotic acid, phytanic acids) Acyl CoA Dehydrogenase Acyl CoA Oxidase Catalase Glucose Catalases • Once again, a heme-containing enzyme • Overall reaction: 2 H2O2 ⇄ O2 + 2 H2O • First step: produces porphyrin cation radical • Second step: HOOH acts as electron donor to produce O2 and return enzyme to resting state. Catalase is a fun enzyme to assay • Mr. Bubble of the enzyme world Staphylococcus aureus Plants don’t store much fat, but seeds often do. Ω-Oxidation •ER of vertebrates •Medium chain FAs a-oxidation Herbivores consume a lot of chlorophyll. Chlorophylls have a long hydrophobic tail. Those tails are split off as part of digestion to form phytanates. a-oxidation (Peroxisomes) Phytanates have bmethyl groups Can’t do b-oxidation Dietary phytanates •Dairy •Fish •Animal fats Refsum’s Disease • Phytanoyl CoA Hydroxylase deficiency • Can also digest phytanic acid by w-oxidation, but only ~10 mg/day • Typical diet contains 50 mg • Builds up in myelin sheath • Also screws up vitamin A metabolism • Demyelinating neuropathy, cerebellar ataxia, deafness, anosmia, cranial nerve degeneration Refsum’s sign Ketone Body Generation • During fasting or carbohydrate starvation, oxaloacetate in the liver is used for gluconeogenesis. • Acetyl-CoA then doesn’t enter Krebs cycle. • Acetyl-CoA converted in mitochondria to ketone bodies, • Ketone bodies are transported in the blood to other cells • Converted back to acetyl-CoA for catabolism in Krebs cycle, to generate ATP. b-oxidation in reverse Diabetic Ketoacidosis • Primarily in Type 1 (insulin-dependent) • Low insulin = low glucose transport into cells • Liver thinks it’s starving • Ketone body production ramps up • Blood pH drops into danger zone