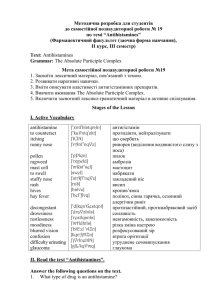
Sympathomimetics, Antihistamines and ENT products Response to
advertisement

Sympathomimetics, Antihistamines and ENT products Response to organ depends on o Specificity of the agonist/antagonist at a given receptor o The absolute number of receptors in that organ or organ system o Ratio of receptors (which is prominent) Alpha 1 = primary receptor for EENT indications: o Stimulation causes: Smooth muscle contraction (lining blood vessels) Vasoconstriction (can help control blood flow) @ a local level (causes vasoconstriction) Decrease in mucous membrane secretions (decongestants) Beta 1 = cardiac stimulation (heart’s a beating) Beta 2 = smooth muscle relaxation (lungs are breathing) SYMPATHOMIMETICS Adrenergic agonists o Mixed acting combine with receptor and produce a response AND: cause NE release or block NE uptake ex: pseudoephendrine ex: phenylpropanolamine (was in Dimetapp but now off the market bc <3 toxicity) o Alpha 1 agonist ex: phenylephrine (decongestant) common uses of sympathomimetics: o Hemorrhage Alpha 1 Epinephrine (Epi) – causes superficial vasoconstriction = controls capillary bleeding; ***used in nasal surgery o Combined with local anesthetics Alpha 1 Epi – causes local vasoconstriction = decreased blood flow which slows absorption and localizes affect of anesthetic Sympathomimetics, Antihistamines and ENT products o Nasal decongestants Alpha agonists Applied locally or orally Constricts swollen (edematous) vessels/tissue Relieves mucosal congestion o Anaphylaxis (acute allergic rxn) Epi Alpha 1 = relieves swelling Beta 1 = some cardiac stimulation (USE WITH CAUTION) Beta 2 = relaxes constricted bronchial smooth muscle o Hypotension – hypotensive crisis (beta one helps in a crisis) Alpha agonists Increased blood pressure via vasoconstriction Causes: o Ischemia in extremities, organs with prolonged administration o Withdraw – taper off agent slowly to prevent recurrence o EENT indications: Nasal preparations Ophthalmic preparations Otic preparations Oral preparations Sympathomimetics, Antihistamines and ENT products Nasal preparations Used to relieve nasal congestion associated with common cold, allergic rhinitis and sinusitis Topical – use as vasodilator (used LOCALLY; not systemically) o Oxymetazolone – active ingredient in afrin; one strength o Phenylephrine – various strength so low doses used for children Sprays o Preferred in adults o Better coverage of nasal mucosa o Easier self administration Drops o Preferred in children o Nostrils are smalle – easily administered by adults o Use lowest strength in children – not for <2 yo Systemic absorption if minimal o Slightly more with drops due to swallowing excess ADRs o Local irritation (burning, stinging, sneezing, dryness) o RHINITIS MEDICAMENTOSA (rebound congestion) Caused by using decongestants for more than 3-4 days; use short term as directed Receptors become desensitized Contraindicated with monamine oxidase inhibitors [MAO-Is] (breaks down catecholamine = severe tachycardia & HTN) Increase in heart rate Can be caused by both oxymetazolone and phenylephrine Patient uses for >3-4 days, desensitization of receptors; does not get relief Starts with bid then tid then qid then 5xd etc. Rebound can be worse than original congestion Sympathomimetics, Antihistamines and ENT products Opthalmic preparations Oxymetazolone Phenylephrine Tetrahydrozaline Naphazoline CAUTIONS: o Contact lens – drops need to be compatible o Narrow angle glaucoma = contraindicated o Greater chance of systemic absorption with eye drops Due to relatively high concentration of medication contained in solution Drug absorbed directly into the tear duct To avoid/lessen the absorption, instruct pt to press on the tear duct when instilling eye drop Sympathomimetics, Antihistamines and ENT products Systemic Preparations: Oral (systemic) Related to amphetamine o Pseudoephedrine (isomer of ephedrine – Sudafed) o Ephedrine (appetite suppressant – CNS stimulation) o Phenylpropanolamine (off the market now; <3 toxicity) Was an excellent decongestant Used in appetite suppressants (dexitrim) o Phenylephrine – also available as an injection Available as single agents o Pseudoephedrine (Sudafed) o Phenylephrine (Sudafed PE) Availavle as combo agents: o Anti-histamine (with brompheniramine in Dimetapp) o APAP (tylenol cold and sinus) o Ibuprofen o Anti-tussive ******* comb of all the above = “complete cold” formulas ADRs o Binding to alpha receptors Systemic effects: Increased HR, BP, palpitations Agitation – irritability Restlessness Insomnia Nervousness Appetite suppression (CNS stimulation Euphoria (~ effects as amphetamines) CNS stimulation – prominent aspect of amphetamines (indirect acting) Tolerance to stimulant properties – leading to drug dependence, especially w/ amphetamines Sympathomimetics, Antihistamines and ENT products Antihistamines Histamine o Produced primarily by mast cells and basophils o Abundant in skin, GI, respiratory tract GI – paracrine cells in fundus (lining) stimulates gastric secretion by parietal cells o CNS neurotransmitter o Released from mast cells by IgE (cromolyn NA blocks this action) o Mast cell degranulation can be caused by : bacterial toxin and drugs (morphine and tubocurarine) – results in flushing and vasodilation when these are given o NORMAL PHYSIOLOGIC EFFECTS Primitive reflex – protective mechanism Vasodilation = decrease BP (relaxation of arteriolar smooth muscle and benules) = hypotension Increased vascular permeability = edema (promotes fluid and plasma out of blood into extracellular spaces) Heart (tachycardia & increased contractility Bronchoconstriction – in lungs (body trying to decrease the amount of allergens entering the lungs) – protective mechanism ANTI-HISTAMINE RECEPTORS o H1 receptor effects Mediates allergic rxns Used in dermatitis, rhinitis, conjunctivitis Activation in skin and mucous membranes causes Vasodilation, increased vascular permeability, erythema, congestion, edema, inflammation Mucocutaneous nerves – pruritis, cough Histamine in circulation – decreased BP, anaphylactic shock o H2 receptor effects GI acid secretions – primarily Allergic reactions H1 and H2 blockers may be used in combo for some allergic reactions (diphenhydramine + famotidine) H2 receptors in heart Increased HR and increased contractility Sympathomimetics, Antihistamines and ENT products o H1 receptor antagonists Block the action of histamine by competitive inhibition at the receptor site Most are capable of crossing the BBB and entering the CNS causing sedation These antihistamines have many other effects NOT due to the histamine receptor There chemical structure is similar to other endogenous agents so they are capable of combining with other receptors in the body to produce a variety of SEs Some effects may be desirable (therapeutic) and others undesirable o EFFECTS OF ANTI-HISTAMINES Therapeutic effects Treatment of allergies Treatment of motion sickness (scopalomine – anti-muscarinic; H1 receptors in vestib. apparatus) Anti-nausea & anti-emetic: central chemotrigger inhibition o Phenothiazines – stimulation of antihistamine to target trigger zone Treatment of insomnia due to sedative side effects ADRs SEDATION Anticholinergic effects (blocks muscarinic receptor causing anti SLUDGE effects) Adrenergic blockade causing orthostatic hypotension (alpha 1 blocker) o Phenothiazines o ANTIHISTAMINES FOR EENT INDICATIONS CAUTION IN THE ELDERLY – ANTICHOLINERGIC SEs Nonselective lipid soluble; cross BBB FIRST GENERATION – used for seasonal or allergic rhinitis Piperazines o Mexlizine – not used for allergic rhinitis; used for vertigo o Hydroxyzine – very sedating Phenothiazines o Promethazine – very sedating; anticholinergic; antiemetic Similar structure binds to other systems = SEs Sympathomimetics, Antihistamines and ENT products FIRST GENERATION ADRs Sedation most common ADR May get paradoxical excitation in children and infants Do not use antihistamine to get a child to sleep Atropine-like ADRs (anti-SLUDGE) o Dry mouth, blurred vision, tachycardia, urinary retention Anticholinergic toxicity – manifestation of overdose o Administer physostigmine (cholinesterase inhibitor) SECOND GENERATION – used for seasonal or allergic rhinitis do not block muscarinic receptors or alpha 1 receptors do not cross BBB MOA = block H1 receptor or stabilize mast cell (prevent release of histamine) Selective for H1 receptor therefore little or no sedative activity Piperidines o Loratadine (Claritin) o Desloratadine (clarinex) o Fexofenadine (Allegra) Piperazines o Cetirizine o Levocetirizine – isomer of cetirizine ***** brand name + D = has pseudoephedrine SECOND GENERATION ADRs The 2nd generations’ advantage over the first is that they are relatively specific for the H1 receptor and therefore have little or no sedative activity HOWEVER, significant DDIs (don’t memorize): Alkylamines Brompheniramine Chlorpheniramine Triprolidine – cause the least amount of sedation (may even cause CNS stimulation) Ethanolamonies Clemastine Diphenhydramine (Benadryl) – VERY sedating, anticholinergic Sympathomimetics, Antihistamines and ENT products o ANTIHISTAMINES EENT EFFICACY: More effective in preventing histamine-mediated effects than reversing these effects Most effective when taken 1-2 hours prior to anticipated exposure of offending allergen o ANTIHISTAMINES EENT KINETICS Well absorbed PO, large Vd, liver metabilism Zyrtec and Claritin Eye Drops Active ingredient is ketotifen o Not cetirizine or loratadine; it has antihistamine and mast cell stabilizing effects Indicated for itchy eyes due to pollen, ragweed, grass, animal hair and dander Cough and cold preparations in kids April 2009: FDA updated the Public Health Advisory recommending that OTC couch and cold products not be used in infants and children less than 2 years (specifically referring to antihistamines, decongestants and dextromethorphan) Topical antihistamines CAUTION IN THE ELDERLY – ANTICHOLINERGIC SEs Nonselective lipid soluble; cross BBB Also considered 2nd generation – used for seasonal or allergic rhinitis o Levocabastine o Aselastine o Olopatadine – mast cell stabilizer and antihistamine (blocks H1 receptor) Miscellaneous agents (EENT) Cromolyn – stabilizes mast cell membranes and thereby preventing degranulation and release of histamine Montelukast – used for seasonal allergic rhinitis in adults and children over 2 years old o Leukotrine receptor antagonist; inflammatory mediator Other agents for Rhinitis Intranasal steroids o Very efficacious, also good if pt also has asthma o Less systemic ADRs Ipratropium nasal spray Saline nasal preps Sympathomimetics, Antihistamines and ENT products Miscellaneous Otic preparations Otic antibiotics; PO approach; systemic Neomycin containing preparations o Neomycin, polymixin B and hydrocortisone Used for otitis externa Solution may be more irritating due to acid content Poor compliance due to frequency (tid; qid) Miscellaneous Otic antibiotics (fluoroquinolones) for otitis externa o Ciprofloxacin & hydrocortisone o Ciprofloxacin & dexamethasone o Ofloxacin o Carbamide peroxide (debrox) Used to emulsify ear wax Tilt head sideways and instill 1-10 drops in ear bid for 4 days Must keep drops in ears for several minutes by keeping head tilted and placing cotton in ear o Analgesics Used to treat acute pain associated with certain ear conditions (otitis media and externa) Antipyrine/benzocaine Miscellaneous Oral Preps & Sprays o Benzocaine o Local anesthetic o May be combined in other anesthetics in different products