HISTOLOGY
advertisement
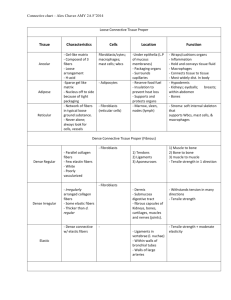
HISTOLOGY Prof. Dr. HUDA AL_KHATEEB 2011-2012 Lec.1 The Circulatory System Aim :study the histology of the circulatory system Objectives: 1. Study the layers and the sub-layers of the heart 2. Study the impulse conducting system structure and ultra-structure 3. Study the types of blood vessels 4. Study the classification of the arteries 5. Study the sorting of veins 6. Study the light and electron microscopical features of the capillaries 7. Classification of capillaries according to their ultra structures 8. Throw light on the lymphatic vessel 4 The circulatory system is categorized as: 1. blood vascular system: Consists of: 1. Heart 2. Vessels: A. arteries B. capillaries C. veins 2. Lymph vascular system: Consists of: 1. lymph vessels 2. organs Circulatory system can be divided into: 1. Macro-vasculature (includes vessels with more than 0.1mm in diameter). These vessels are seen grossly. 2. Micro-vasculature (includes arterioles, capillaries and postcapillary venules). These vessels are seen by microscope. Blood Vascular System The heart -it is a muscular, highly specialized portion of the vascular system. -it consists of 4 chambers: RT&LT atria RT&LT ventricles The heart wall consists of 3 layers 1. Endocardium (inner layer). 2. Myocardium (middle layer). 3. Epicardium (outer layer). The fibrous central region of the heart is called fibrous skeleton, which serves as base of the valves and site of origin and insertion of cardiac 5 muscle cells. Histologically, fibrous skeleton is composed of dense irregular connective tissue, with separated nodules of fibrocartilage. Endocardium -it lines all internal surfaces of the heart. -it is thicker in atria than ventricles (Figure 1 &2) -it has three layers: 1. The endothelium- it is the inner most layer. It is continues with that of blood vessels entering and leaving the heart. It is composed of simple squamous epithelium. 2. Subendothelial layer- consists of narrow zone of loose connective t. that is mainly composed of fine collagen, elastic and smooth muscle fibers. 3. subendocardial layer- which is composed of connective t. that contains: +B.V.s +nerves +branches of impulse-conducting system of the heart (Purkinje fibers) Myocardium 1. composed of cardiac m. fibers that run in different directions (complex-spiral) and usually inserted into the fibrous skeleton of the heart. 2. form the main mass of the heart wall. 3. It is the thickest layer in the heart wall. Its thickness varies in different parts of the heart being thinnest in the atria, thickest in the LT ventricle. 6 Epicardium (it is the visceral pericardium) -covered externally by a single layer of simple squamous epithelium (mesothelium), that is supported by very thin layer of connective t. containing elastic fibers (subepicardial layer). -subepicardial layer-composed of loose connective t. containing: 1. B.V.S. 2. N.s 3. adipose t. Cardiac valves: (1) atrio-ventricular valves (A-V valves):(tricuspid & mitral) -they are composed of core of dense fibrous connective t. (central core) that is lined on both sides by endothelium. The bases of the valves are attached to the fibrous skeleton. (2)Semi lunar valves (aortic and pulmonary valves): are similar in structure to the A-V valves, but they have thinner central core. Impulse-conducting system: 1. Sino-atrial node (SA node) 2. Atrio ventricular node (AV node) 3. Atrio-ventricular bundle (AV bundle);includes; A. Bundle of His B. Right and left bundle branches C. Purkinji fibers 7 All cells of impulse-conducting system are modified cardiac muscle cells (fuseform cells and smaller than atrial cardiac muscle fibers), except Purkinji fibers, which are larger. Purkinje fibers: -they are modified cardiac m. fibers. They conduct impulses faster than the ordinary heart m. fibers. -After traveling in subendocardium, they penetrate myocardium of ventricles. This arrangement is important because it allows the stimulus to get into the outermost layers of ventricular musculature. Histological features of Purkinji fibers: I. Light microscopical (L.M.) features: Purkinje fibers resemble ordinary cardiac m. in that: 1. they have central nuclei. 2. they have cross striation. However they differ from them in that: 1. they are generally larger and paler. 2. they have more sarcoplasm. 3. their nuclei are surrounded by clear perinuclear area. II. Electron microscopical (E.M.) features: Ultrastructurally Purkinje fibers have the following features: 1. they contain large amount of glycogen and mitochondria. 2. they contain less amount of myofibrils which tend to lie peripherally (this explain the presence of clear perinuclear area). 3. sarcoplasmic reticulum is not well developed as in cardiac m.s INNERVATION OF THE HEART Heart is innervated by: 1. Parasympathetic nerve (vagus) - ends near SA node. Its stimulation leads to reduction of the heart rate. 2. Sympathetic nerve - ends near SA and AV nodes. Its stimulation leads to increase of heart rate. 8 3. Free nerve ending - ends between cardiac muscle fibers. It is related to pain sensation. CLINICAL NOTES: -Partial obstruction of coronary artery or any of its branches leads to reduction of O2 supply to myocardium that leads to temporary pain(conducted by free nerve ending). This case is called Angina Pectoris. -Complete obstruction of coronary artery or any of its branches (by a thrombus ) leads to sever pain (conducted by free nerve ending). This case is called myocardial infarction. HISTOLOGY Prof. Dr. Huda Al-Khateeb 2011-2012 Lec.2 General structure of blood vessels (BV): Blood vessels (BV) have three basic types of tissues. These are: 1. Endothelium. 2. Smooth muscle cells 3. Connective tissue The amount and the arrangement of these three types of tissues, within BV wall, are influenced by: 1. Mechanical factor – represented primarily by blood pressure. 2. Metabolic factor – reflects the local needs of tissue. 9 VASCULAR ENDOTHELIUM It is a special type of simple squamous epithelium. It serves many functions, these are: 1. It forms a semipermeable barrier between plasma and interstitial fluid. 2. It converts angiotensin I to angiotensin II. The latter increase blood pressure. 3. It converts bredykinin, serotonin, prostaglandins and noradrenaline ------------etc. to biologically inert compounds. 4. It enhances lipolysis leading to formation of triglycerides and cholesterol. 5. It produces endothelin, which is a vasoconstrictive factor. 6. It produces nitric oxide, which is a relaxing agent. 7. It produces vascular endothelial growth factors (VEGFs). In embryo, VEGFs is responsible for the formation of vascular system, while in adults, they regulate capillary growth in normal and pathological conditions. 8. It has anti-thrombogenic action (preventing blood coagulation). Damage to endothelium will uncover connective tissue and induce platelates aggregation, thus cause thrombus and emboli formation. VASCULAR SMOOTH MUSCLE CELLS Found in all vessels, except capillaries and venules. They are arranged in helical layers in tunica media. Each muscle is enclosed by basal lamina and connective tissue (both are secreted by the smooth muscle). VASCULAR CONNECTIVE TISSUE Variable amount of connective tissue present in different BV. Collagen fibers type I found in tunica adventitia, type III in tunica media and type IV in the basement membrane. Elastic fibers are responsible for shrinkage of the expanded vascular wall. They are predominant in large arteries. Ground substance is composed of hetrogenous gel in extracellular spaces of the vessel wall. It affects the diffusion and permeability across the vessel wall. 10 Aging causes conformational changes in collagen and elastin with deposition of lipoproteins and calcium, in addition to atherosclerosis. LAYERS OF WALL OF BV Generally, each BV is composed of 3 layers; these are from inside to outside: 1-Tunica Intima (TI) – subdivided into: A- Endothelium- (simple sq. epith.) B- Subendothelium- loose con.t. C- Int. elastic lamina – composed of elastin that has gaps (for diffusion of substances to nourish cells deep in the vessel wall). It is found in arteries only. 2-tunica media (TM) – composed of: A- Circular smooth m. fibers B- Elastic fibers. C- Reticular fibers (collagen fibers type III) D- Fibroblast E- Ground substance (proteoglycan and glycoprotein) F- in arteries, TM has external elastic lamina that separate it from TA 3-tunica adventitia (TA) – consist of connective tissue (collagen type I and elastic fibers. The structure & relative thickness of each layer vary according to the type & size of the vessel. Classification of a.s. : 1-large-size a.-(elastic a.) 2-medium-size a. and small- size a. -(muscular a.) 3-arteriol In arteries, TM is usually the thickest layer, while in veins, TA is commonly the thickest layer. 11 large-size a. (elastic a.) (conducting a.) includes aorta & its largest branches. TI – relatively well developed -the int. elastic lamina is present but difficult to be diagnosed because It is usually mixed with the elastic lamina of TM TM – it is the thickest layer in this type of a.s -characterized by a distinct elastic laminae (40-70 in no., usually increase with age) arranged in a concentrical pattern. -interspaces between the elastic membranes are occupied by fibroblasts , amorphous ground substance, fine elastic net work and smooth m. cells. TA - Loose connective tissue Medium- & small- size a. (Muscular a.) (Distributing a.) Characterized by thick wall & narrow lumen, when compared with elastic a. TI - prominent thick int. elastic lamina TM -consists of about 40 layers of circularly arranged smooth muscle fibers. -between smooth muscle fibers, there are small amount of con.t. that contains elastic & reticular fibers & few fibro blasts. -ext. elastic lamina is Prominent & composed of many layers TA - loose connective tissue Arterioles generally less than 0.5 mm in diameter have relatively thick wall & narrow lumen (when compared with venule). TI *Int. elastic membrane present in big arterioles only and disappear in smaller arterioles. *has no subendothelial con.t. 12 TM *composed of (1-5) layers of circularly arranged smooth m. fibers among which scattered elastic fibers *the no. of smooth m. layers ↓ as diameter ↓. it becomes single layer at about 20μm diameter arteriole. *it has no external elastic lamina. TA - very thin Arterial capillary (pre-capillary) (met-arteriole) TI - composed of endothelium only TM - circularly oriented scattered smooth m. fibers that have branching processes. ATHEROSCLEROSIS: It is accumulation of cholesterol in the T.I. of arteries. Grossly, the artery contains fatty streaks and plaques on its internal surface. If these fatty thickenings become great, they occlude the vessel. Coronary arteries are most arteries predisposed to atherosclerosis, which sometimes leads to infarction (necrosis and tissue death) and other times it is overcome by arterial anastomosis. ANEURYSM: It is a pathological dilatation of an artery, which is due to embryonic defect, disease or lesion in its TM (that leads to its weakness in TM and dilatation in the artery). Rapture of aneurysm brings sever consequence and may cause death. 13 1. diameter of lumen 2. thickness of the wall 3. TM is mainly composed of 4. Internal and external elastic membranes 5. TI is 6. function 7. example Elastic artery Wider Thinner 40-70 elastic lamina Can't be easily diagnosed Muscular artery Narrower Thicker 40 layers of smooth m. fibers Very prominent and diagnosed easily Thinner Control the amount of blood flow to organs by contracting or relaxing its smooth m. Thicker Stabilize arterial blood pressure (during systole, elastic lamina stretch and reduce the increased blood pressure. During diastole, the elastic rebound increase the reduced blood pressure) Aorta and its large Coronary artery branches 14 HISTOLOGY Prof. Dr. Huda Al-khateeb 2011-2012 Lec. 3 Capillaries (cap.): - total length of human cap.s = 9600 km, which = 60000 mile -connects venous to arterial sides -(7-9) μm in diameter = diameter of a single RBC -form a network that varies in size & shape ex: in lung } liver } kidneys } have large mesh of cap. network glands } mucous membranes } skeletal muscles } gray matter of brain } tendon nerve smooth muscles serous membranes } } have spares cap. network } } Structure of cap.: L.M. 15 +transverse section of cap. contains (1-2) endothelial cells, whose nuclei bulge into the cap. Lumen. E.M. 1-endothelium -cytoplasm is thick opposite nucleus & thin elsewhere -organelles usu. lie in the perinuclear area -these are: +small Golgi complex +few mitochondria +free rrbosomes +RER +filaments → may be related to the contractility of endothelium 2-Basal lamina- which is a product of endothelial cells. 3-thin sheath of delicate collagen & elastic fibers. 4-pericytes- slender, elongated, highly branched cells, whose cytoplasm contain filaments (myosin, actin and tropomyosin), which are responsible for its contractile function. They are located between endothelial cells and their basal lamina. * After tissue injury, pericytes proliferate and differentiate to form new blood vessels and connective tissue cells, thus participating in tissue repair process. Classification of cap.s Cap. Are classified according to their ultrastructure into: 1-continuous cap. 2-fenestrated cap. 3-sinusoidal (or discontinuous) cap. continuous (type I) cap. *found in: muscle tissue lung CNS Skin Connective tissue Exocrine gland 16 *the endothelial cytoplasm contains no. of small vesicles (pinocytotic vesicles) of (50-70) nm in diameter. Functionally, it appears that they are involved in the transport of fluid & macromolecules across the cap. wall. *few or no pinocytotic vesicles are encountered in continuous cap.s of nervous system. this feature accounts for the existence of B. Brain Barrier. fenestrated (type ІІ) cap.s *found in: intestinal mucosa endocrine glands renal Glomerulus pancreas *peripheral cytoplasm of endothelium is perforated at intervals by “pores” ranging (30-50) nm. the pores are closed by thin diaphragm, except in cap. of renal glomeruli.(pores have no diaphragm) Sinusoidal cap.s (sinusoids): *the cap. lumen is greater than other types of cap.s (30-40) μm In diameter *the wall of sinusoid is composed of discontinuous layer of endothelial cells * cytoplasm of endothelial cells shows multiple fenestration without diaphragms. *macrophages are closely associated with the endothelial cells. both within & around the sinusoidal wall. *basal lamina is incomplete. *sinusoids are found in liver and haemopoietic organs (ex. Bone marrow & spleen). Venus cap.s (post-cap.s) -diameter up to 30μm. -wall consists of: 1-endothelium 2-thin con.t. coat contains pericytes (slender, elongated, highly branched cells found in cap.s & postcap.s surrounding endothelium). they are greater in no. in post cap. than that in cap.s. 17 classification of v.s 1- venules 2- small to medium size v.s 3- large size v.s Venules *the smallest venule (40μm in diameter) has -T.I. that possess endothelium with basal lamina -T.A.- outer thin sheath of collagenous fibers *in venules of 50μm diameter smooth m. fibers appear between endothelium & con.t. (i.e. T.M. appears). *in 200μm diameter venule- the circular muscle fibers form a continuous layer (T.M.)(1-3) cells thick. -T.A. is thicker & consists of longitudinally oriented collagenous fibers , scattered elastic fibers & fibroblasts . Small & medium size v.s -diameter ranges (1-9)mm -T.M. has no elastic membrane T.M. -thin *best developed in v.s of lower limb. T.A. -thickest layer -thick longitudinal collagenous bundles and frequently few smooth m. fibers which are arranged longitudinally along the vessels . 18 Large v.s -includes the sup. & inf. Vena cava & their main tributaries. T.I. -same as medium sized v. -it may be thicker. T.M. -poorly developed or absent T.A. -thickest composed of longitudinal coarse collagen fibers & smooth m.s venous valves - found in medium size v.s especially of lower limb are provided with valves that prevent the flow of b. away from the heart. -valves are folding of the T.I. BV of BV (vasa vasorum) -a.s & v.s of diameter over 1 mm are supplied by small , nutrient BV that is called vasa vasorum . -vasa vasorum usually inters T.A. & terminates in a dense cap. network which penetrate as far as the deepest layer of the T.M. -generally no cap.s are found in T.I. However , in some large v.s, cap.s penetrate as far as T.I. (probably because of low venous pressure & O2 tension) . Lymph vascular system Consists of : 1-lymphatic vessels their structure is usu. Similar to the structure of the corresponding size v.s 2-organs → lymph nodes 19