File
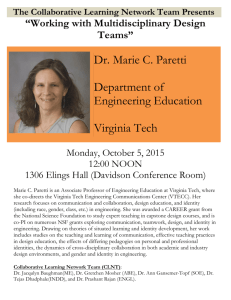
advertisement

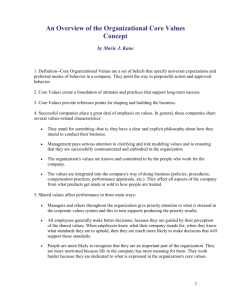
Clinical Bedside Orientation Workbook Directions: Please use the attached checklist and activity booklet as a guide for Clinical Orientation activities. It is also a tool for giving/receiving feedback between you, your clinical guides (aka ‘buddy nurses). It is also helps you start to develop your day-to-day organization and patient planning – a necessary practice element on 5A/B. By the end of your bedside orientation this booklet should be completed and a copy submitted to Marie McCoy, CNE for your file. If you have ANY questions along the way, PLEASE ask! Clinical Bedside Objectives – Day 1: On the initial Bedside Orientation day with Marie or Susan the New 5AB RN will: Give/receive verbal report using the Heart Centre Care Map Interpret ECG rhythm strips A basic understanding of the Drager® ECG monitoring system Planning patient care for the day Performing safety checks on patients Performing a physical assessment, as per “Cardiac Ward Assessment” protocol Administer medications as per CRNBC and PHC standards Document patient care on PHC flow sheets (i.e. Cardiac Sx Clinical pathways/ 24 hour Flow sheet). Communicate patient needs using a variety of communication tools and methods Operate and check commonly used equipment Locate regular used ward supplies Date: _________________________ New 5AB RN:_____________________ with Marie McCoy or Susan Roth, CNE Activity Giving/Receiving Report √ Comments CNE demonstrates receiving report in a.m. using the Heart Centre Care Map CNE reviews 5A/B specific ‘report cheat sheets’ and unit layout CNE review additional tools that could be used to give/receive report - Flow sheets, MAR, Chart, Unit white board New RN gives a break report to break buddy New RN to gives end of shift report CNE feedback to New RN on report giving Unit Socialization Orientates RN to the ward layout Verbally review ward routines During the shift, the CNE introduces the new hire to: CNL NP(s) (as available) Unit Clerk(s) Ward Aide(s) Other RNs working this shift Multi disciplinary team (as available): - Physiotherapist Dietician Pharmacist Occupational Therapist Pastoral Care - Social Worker Physicians (as available) 2 of 20 September/October 2012 Plan care for the day CNE leads discussion regarding plan for pt care, including: - a.m. care medication administration discharge planning and teaching - diagnostic tests or interventions, etc. CNE review ‘care planning’ document (to be completed on 1 patient per ‘buddy’ shift). New RN follows through with planned activities CNE provides on-going feedback (see comments) Safety Check(s) CNE demonstrates safety check and give rationale Performing Safety Check(s) Safety checks to include: - - ECG/cardiac monitoring alarms appropriate Bed in lowest position Railings down Suction equipment working & available (canister, tubing, yankauer) Oxygen equipment available (nipple, simple FM, meter) IV patent - Call bell within reach - 3 of 20 September/October 2012 Interpreting ECG Rhythms – Review Review tele protocol: CNE explains when to take strips - Look up protocol What is the difference between Class 1 & 2 tele? Other d/c criteria i.e. VAD pts or Cardiac Sx pts Frequency of electrode changes At start of shift - With each change in condition - Demonstrates where ‘strips ‘are documented New RN to analyze pt’s ECG strip and document appropriately New RN to explain any possible signs or symptoms related to the rhythm analyzed CNE and New RN to demonstrate appropriate care for rhythm CNE and New RN reviews 3-5 other pt’s ECG rhythms currently on ward Cardiac Monitoring System Review and Practice Printing/recording strips Personalizing alarm settings & protocol for Alarm ‘re-learning’ Tele suspension Transfer rooms Transfer tele packs Full disclosure/event disclosure Printing of above Calipers – how to use Equipment location and care/cleaning expectations Transport Monitors Where they are When they used How to use it – basic functions 4 of 20 September/October 2012 Cardiac Physical Assessment CNE reviews cardiac assessment as per protocol CNE demonstrates listening to heart sounds and includes the following information: - S1S2 audible (not responsible for extra heart sounds) Discusses trend sounds (are they different than the a.m., after epi wire removal) Extra/abnormal sounds can be reviewed with NP New RN listens to heart sounds CNE demonstrates listening to lung sounds Auscultation Tips - Don’t listen through gown Provide privacy CNE reviews all aspects of New RN’s physical assessment and documentation provides feedback See blue handout regarding breath sounds in orientation binder 5 of 20 September/October 2012 Medication Administration New RN to explain 7 rights of medication administration (Right medication, right patient, right time, right does, right route, right reason, right documentation). CNE review PHC Standards for Procedure for Processing Orders, MAR: Discontinuing a medication order procedure & MAR: Next-day Medication Administration Record Verification New hire to spend 1 hour with Unit Coordinator to review their role and reinforce above. New RN to administer all patient medications; under CNR supervision MAR to the bedside and using 2 patient identifiers with every med administration Medications remain in pharmacy packaging until administered at the bedside unless medication prep is required New RN to explain/teach reason for medications being given in regards to individual patient history/diagnosis New RN performs 3 safety checks New RN signs for medication in MAR New RN does NOT pre-pour medications (show examples of pre-pouring and reinforce ‘danger’ in this practice). New hire to review and practice Procedure for Processing Orders, MAR: Discontinuing a medication order procedure & MAR: Next-day Medication Administration Record Verification Procedure during Guided Clinical shifts. They are: _____________? 6 of 20 September/October 2012 Documentation Clinical Teacher shows documentation forms and where they are kept (i.e. 24 hour flow sheet, Clinical record, Cardiac sx pathway documentation tool, EKG record, MAR, ID progress notes) Clinical Teacher explains tips for good charting: - Using the DAR approach or “New” Cardiac sx assessment record Chart only what you need to Don’t double chart Chart as close to the time of the event as possible Keeping in mind who is reading the charting Chart only the care you provide Chart all the care you provide Write legibly CNE explains charting in ID notes (re: 5A vs. 5B ‘nroms’) New RN charts a.m. assessment and any further care provided during the day CNE provides direct feedback regarding charting Unit Communication CNE reviews different forms of communication and patient care planning to New RN (i.e. board rounds, Interdisciplinary rounds (Wednesdays-5B), documentation (as above), one to one (face to face, telephone etc.), Show call list location and who to call; review ‘who to call handout’ in orientation binder. New RN to observe above communication techniques throughout shift New RN to participate board rounds and in communication using SBAR format during guided bedside shifts 7 of 20 September/October 2012 Equipment Demonstration CNE shows storage location and demonstrate correct use of the following equipment (review related available protocols on-line) - - Glucometers, including Maintenance checks (show nightly ‘checks’ binder Hopper PCA pumps (has protocol) Least restrain equipment (has protocol) Pinel restraints (has protocol) - Trach equipment (has protocol) - Portable ‘dressing carts’ New RN to describe where to find various supplies and equipment New RN to return demonstrate correct use of equipment (described above). Section I: Clinical Bedside orientation day Homework! 1. Reflect on your classroom and bedside orientation. Send Marie (mdmccoy@providencehealth.bc.ca) or Susan (sroth@providencehealth.bc.ca) an E mail with the following evaluative information (within 1 week): The thing I enjoyed most about classroom orientation was… In class, I wish we had spent more time on…. In class, I wish we had leant about… The thing I enjoyed most about the clinical bedside orientation was… Two questions I still have are…(please try to think of questions or topics that have ‘occupied’ your thoughts since classroom or bedside orientation). 2. Complete the following ‘Reverse Case Study’ and submit (via E mail or ‘hard copy’) during your Orientation Check-In with Marie or Susan. Reverse Case Study Directions: The goal of the exercise is to understand how pieces of information relate and to anticipate the plan of care for your ‘imaginary’ patient. Using your nursing knowledge, formulate this case study including: Previous medical history, considering risk factors for the current situation What you would assess and expected findings Nursing and medical interventions expected Expected lab and diagnostic tests that may be ordered and their results List at least 3 nursing diagnoses and the expected outcomes after the interventions Remember, there are many ‘right’ answers. You decide what the medical history will be based on the medications and the current course. The other boxes will be completed based on what you decide. 8 of 20 September/October 2012 Home Medications: Metformin 500 mg po BID Metoprolol 25mg po BID Lasix 40 mg po daily ASA 81 mg po daily Atorvastatin 40 mg po daily Ramipril 5 mg po BID Pantoprazole 40mg po daily Allopurinol 300mg TID Digoxin 0.25mg po daily Clopidogrel 75mg po daily Current Course: Patient is a 73 yr old male who came to ER complaining of palpitations, lightheadedness, and chest pain beginning a few days ago. Also, increased tiredness and short of breath with minimal exertion. Previous Medical History Your Assessment Data Medical Diagnoses Nursing Diagnoses Expected lab and diagnostic tests with results Anticipated/actual collaborative and nursing interventions/orders Expected outcomes for Nursing Diagnoses (at least 5) 9 of 20 September/October 2012 Section II: On a minimum of 5 Guided Clinical Shifts – Complete the following table for ONE of your assigned patients (i.e. you should complete a minimum of 5 tables before you have completed your ‘buddy’ shifts). Pt’s (1) Admitting Diagnosis: Age: Sex: Known Cardiac Risk Factors: 5 key pieces of data I received from shift handover (report): Pt specific ‘head-to-toe’ assessment findings (comment on a minimum of 3 systems). 1) 2) 3) 4) 5) My TOP 3 goals for this pt on this shift: To accomplish these goals I will… 1) Goal 1: 2) Goal 2: 3) Goal 3: Other information I feel is important to help me prioritize and plan my care for this pt is: 10 of 20 September/October 2012 Pt’s (2) Admitting Diagnosis: Age: Sex: Known Cardiac Risk Factors: 5 key pieces of data I received from shift handover (report): Pt specific ‘head-to-toe’ assessment findings (comment on a minimum of 3 systems). 1) 2) 3) 4) 5) My TOP 3 goals for this pt on this shift: To accomplish these goals I will… 1) Goal 1: 2) Goal 2: 3) Goal 3: Other information I feel is important to help me prioritize and plan my care for this pt is: 11 of 20 September/October 2012 Pt’s (3) Admitting Diagnosis: Age: Sex: Known Cardiac Risk Factors: 5 key pieces of data I received from shift handover (report): Pt specific ‘head-to-toe’ assessment findings (comment on a minimum of 3 systems). 1) 2) 3) 4) 5) My TOP 3 goals for this pt on this shift: To accomplish these goals I will… 1) Goal 1: 2) Goal 2: 3) Goal 3: Other information I feel is important to help me prioritize and plan my care for this pt is: 12 of 20 September/October 2012 Pt’s (4) Admitting Diagnosis: Age: Sex: Known Cardiac Risk Factors: 5 key pieces of data I received from shift handover (report): Pt specific ‘head-to-toe’ assessment findings (comment on a minimum of 3 systems). 1) 2) 3) 4) 5) My TOP 3 goals for this pt on this shift: To accomplish these goals I will… 1) Goal 1: 2) Goal 2: 3) Goal 3: Other information I feel is important to help me prioritize and plan my care for this pt is: 13 of 20 September/October 2012 Pt’s (5) Admitting Diagnosis: Age: Sex: Known Cardiac Risk Factors: 5 key pieces of data I received from shift handover (report): Pt specific ‘head-to-toe’ assessment findings (comment on a minimum of 3 systems). 1) 2) 3) 4) 5) My TOP 3 goals for this pt on this shift: To accomplish these goals I will… 1) Goal 1: 2) Goal 2: 3) Goal 3: Other information I feel is important to help me prioritize and plan my care for this pt is: Section III: Clinical Guide Shift Feedback: It is your responsibility to give these 3 feedback forms to 3 different clinical guides. Please have them complete this form and 1) Make a copy (for you to keep and 2) Hand-in the originals during your orientation check-in or at the end of your bedside orientation. 14 of 20 September/October 2012 Written and verbal feedback is a vital component to building the confidence and skills of our new 5AB RN’s. Please take a few moments to document key areas of strength and areas for improvement for your new colleague; please be specific with your comments and provide examples (under each heading) to illustrate your comments where possible (point form is acceptable). This feedback will be reviewed with the new hire on their orientation check-in. Thank you for your hard work and continue support throughout the orientation process. Assessment: Example: Marie’s head-to-toe assessment was well organized and comprehensive, but she needs more practice with identifying adventitious lung sounds. Documentation: Example: Marie needs to work on concise documentation. One way she could improve would be to document only by exception. Also, Marie needs to remember to document the ‘Response’ of her ‘Actions.’ Medication Administration: Example: Marie is conscientious regarding her 7 Right of Med Administration. Always took the MAR to the beside; medications given in appropriate time frame. Clinical Thinking: Example: Marie’s clinical judgment and knowledge translation is appropriate for her experience level. For example, Marie was able to identify the ‘most acute’ pt in our assignment and prioritized his care accordingly. Time Management: Example: Marie was frequently ‘running behind’ throughout her day. One way she could improve her time management would be to ‘cluster’ her tasks and ensure she has everything she needs before commencing. Communication & Patient Teaching: Example: Marie tends to be long winded. Marie needs to be more direct in her communication style to ‘get her point across’ more efficiently. This will also help to improve her time management. ECG Interpretation: Example: Marie was to correctly interpret ¾ pt ECG rhythms, but some prompting was required. Marie needs to review her 2nd degree blocks. General Observations: Example: Marie is a compassionate and team oriented nurse – this is her greatest strength. She needs to improve her time management and patient teaching skills as she still feels uncomfortable with much of the discharge teaching material. I think she could benefit from an additional Clinical Transition shift. 15 of 20 September/October 2012 Written and verbal feedback is a vital component to building the confidence and skills of our new 5AB RN’s. Please take a few moments to document key areas of strength and areas for improvement for your new colleague; please be specific with your comments and provide examples (under each heading) to illustrate your comments where possible (point form is acceptable). This feedback will be reviewed with the new hire on their orientation check-in. Thank you for your hard work and continue support throughout the orientation process. Assessment: Example: Marie’s head-to-toe assessment was well organized and comprehensive, but she needs more practice with identifying adventitious lung sounds. Documentation: Example: Marie needs to work on concise documentation. One way she could improve would be to document only by exception. Also, Marie needs to remember to document the ‘Response’ of her ‘Actions.’ Medication Administration: Example: Marie is conscientious regarding her 7 Right of Med Administration. Always took the MAR to the beside; medications given in appropriate time frame. Clinical Thinking: Example: Marie’s clinical judgment and knowledge translation is appropriate for her experience level. For example, Marie was able to identify the ‘most acute’ pt in our assignment and prioritized his care accordingly. Time Management: Example: Marie was frequently ‘running behind’ throughout her day. One way she could improve her time management would be to ‘cluster’ her tasks and ensure she has everything she needs before commencing. Communication & Patient Teaching: Example: Marie tends to be long winded. Marie needs to be more direct in her communication style to ‘get her point across’ more efficiently. This will also help to improve her time management. ECG Interpretation: Example: Marie was to correctly interpret ¾ pt ECG rhythms, but some prompting was required. Marie needs to review her 2nd degree blocks. General Observations: Example: Marie is a compassionate and team oriented nurse – this is her greatest strength. She needs to improve her time management and patient teaching skills as she still feels uncomfortable with much of the discharge teaching material. I think she could benefit from an additional Clinical Transition shift. Clinical Guide: ___________________ New Hire: ______________________ Unit: ______ 16 of 20 September/October 2012 Written and verbal feedback is a vital component to building the confidence and skills of our new 5AB RN’s. Please take a few moments to document key areas of strength and areas for improvement for your new colleague; please be specific with your comments and provide examples (under each heading) to illustrate your comments where possible (point form is acceptable). This feedback will be reviewed with the new hire on their orientation check-in. Thank you for your hard work and continue support throughout the orientation process. Assessment: Example: Marie’s head-to-toe assessment was well organized and comprehensive, but she needs more practice with identifying adventitious lung sounds. Documentation: Example: Marie needs to work on concise documentation. One way she could improve would be to document only by exception. Also, Marie needs to remember to document the ‘Response’ of her ‘Actions.’ Medication Administration: Example: Marie is conscientious regarding her 7 Right of Med Administration. Always took the MAR to the beside; medications given in appropriate time frame. Clinical Thinking: Example: Marie’s clinical judgment and knowledge translation is appropriate for her experience level. For example, Marie was able to identify the ‘most acute’ pt in our assignment and prioritized his care accordingly. Time Management: Example: Marie was frequently ‘running behind’ throughout her day. One way she could improve her time management would be to ‘cluster’ her tasks and ensure she has everything she needs before commencing. Communication & Patient Teaching: Example: Marie tends to be long winded. Marie needs to be more direct in her communication style to ‘get her point across’ more efficiently. This will also help to improve her time management. ECG Interpretation: Example: Marie was to correctly interpret ¾ pt ECG rhythms, but some prompting was required. Marie needs to review her 2nd degree blocks. General Observations: Example: Marie is a compassionate and team oriented nurse – this is her greatest strength. She needs to improve her time management and patient teaching skills as she still feels uncomfortable with much of the discharge teaching material. I think she could benefit from an additional Clinical Transition shift. Clinical Guide: ___________________ New Hire: ______________________ Unit: ______ 17 of 20 September/October 2012 Section IV: See attached ‘5AB Learning Plan.’ It is now a registration requirement of CRNBC for EVERY nurse to complete an annual learning plan to help document and fulfill professional development goals. Please complete 2 “Learning Goals” and the associated documentation for your 3 Month check-in. This document will be reviewed and expanded with the CNE at each check-in session over the next year. Assessment: Example: Marie’s head-to-toe assessment was well organized and comprehensive, but she needs more practice with identifying adventitious lung sounds. Documentation: Example: Marie needs to work on concise documentation. One way she could improve would be to document only by exception. Also, Marie needs to remember to document the ‘Response’ of her ‘Actions.’ Medication Administration: Example: Marie is conscientious regarding her 7 Right of Med Administration. Always took the MAR to the beside; medications given in appropriate time frame. Clinical Thinking: Example: Marie’s clinical judgment and knowledge translation is appropriate for her experience level. For example, Marie was able to identify the ‘most acute’ pt in our assignment and prioritized his care accordingly. Time Management: Example: Marie was frequently ‘running behind’ throughout her day. One way she could improve her time management would be to ‘cluster’ her tasks and ensure she has everything she needs before commencing. Communication & Patient Teaching: Example: Marie tends to be long winded. Marie needs to be more direct in her communication style to ‘get her point across’ more efficiently. This will also help to improve her time management. ECG Interpretation: Example: Marie was to correctly interpret ¾ pt ECG rhythms, but some prompting was required. Marie needs to review her 2nd degree blocks. General Observations: Example: Marie is a compassionate and team oriented nurse – this is her greatest strength. She needs to improve her time management and patient teaching skills as she still feels uncomfortable with much of the discharge teaching material. I think she could benefit from an additional Clinical Transition shift. 18 of 20 September/October 2012 Learning Goal “What do I want to accomplish?” Activities/Strategies Strategy 1: “How will I accomplish my objectives?” Strategy 2: Strategy 3: Indicators/Evidence “How will I know I have accomplished my objectives?” “How will I measure that I met my goal?” Other Resources (could include people, literature, courses etc.) Target dates “When do I expect to accomplish this by?” Review with NE (review progress of goal achievement) 19 of 20 September/October 2012 Learning Goal “What do I want to accomplish?” Activities/Strategies Strategy 1: “How will I accomplish my objectives?” Strategy 2: Strategy 3: Indicators/Evidence “How will I know I have accomplished my objectives?” “How will I measure that I met my goal?” Other Resources (could include people, literature, courses etc.) Target dates “When do I expect to accomplish this by?” Review with NE (review progress of goal achievement) 20 of 20 September/October 2012