Clinical Protocols - Philadelphia University Athletics
advertisement

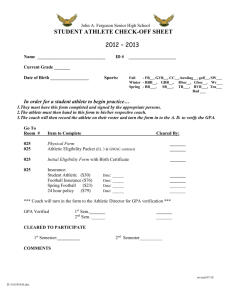
Athletic Training Clinical Policies and Procedures Updated June 2013 Athletic Training Policies and Procedures The mission of the Athletic Training staff is to help prevent athletic injuries from occurring by assisting in the conditioning of the athletes. In the event of injury the athletic training staff will evaluate injuries on the field or court, determine the extent of injury and plan for treating the injury. When necessary the athletic trainer will refer the athlete to the team physician or work through the athlete's primary care physician for continuation of treatment. The athletic trainer will work with the physician in rehabilitating the athlete's injury through to their full return to activity. Athletic Training Room Staff Philadelphia University has two National Athletic Training Association certified, Pennsylvania State licensed; athletic trainers on staff. The athletic training staff is responsible for the coordination of the medical needs for all varsity sports. This includes pre-participation physicals, evaluation and treatment of on-field injuries, injury rehabilitation, injury prevention education, and coordination of insurance coverage. The athletic training staff may also include graduate assistant athletic trainers, undergraduate student athletic trainers (Temple University and Immaculata University), and work study student assistants who are under the direct supervision of the head athletic trainer. The athletic training staff is certified in CPR and assist in providing medical coverage for athletic practices and games. The sports medicine staff also includes the medical doctors who are treating the athletes. Philadelphia University is affiliated with Drexel Sports Medicine and our staff is supervised by an orthopedic surgeon who helps coordinate the sports medicine care of our student-athletes. We also will coordinate care with the student-athlete's family doctor whenever necessary. Athletic Training Room The Philadelphia University Athletic Training Room is located in Harris Gym of the Athletic and Recreation Center. It is fully equipped as a therapy center with modalities such as hydrocollators, electrical stimulation, ultrasound, JOBST cryocompression therapy and whirlpools. There is an adjacent weight room and a full size gymnasium. Athletic Training Room Hours Athletic Training room hours and treatment times will be established and posted on the athletic training room door. These hours will be from 10 until the end of practice each day Monday - Friday during the school year, but may be adjusted as the seasons change and will reflect the needs of the individual sports in season. The athletic training room will be CLOSED on Saturdays and Sundays unless there are practices and games scheduled. Individual treatments will be scheduled on an as needed basis and student-athletes are expected to adhere to these scheduled times. No one is permitted to use the athletic training room facilities except under the direct supervision of a member of the sports medicine staff. Updated June 2013 Eligibility for Athletic Training Services Philadelphia University athletic training services are reserved for any sport covered under the Department of Athletics and its liability insurance policy. These sports include all 16 varsity sports and as well as cheerleading. In order to receive medical attention by the athletic training staff, an athlete must have their sports medicine paperwork up-to-date including their yearly physical for athletic eligibility. Pre-participation Physical Examinations 1. All student-athletes at Philadelphia University must complete a physical examination by the team physician or their own family physician prior to participation in any practice, workout, or event. Forms will be provided to the student if they elect to have their family physician do the screening. The university will not reimburse the student if they elect to go to their own physician. 2. The required freshman physical is acceptable for that year only. These physicals will be scheduled in April for returning fall/ winter sport athletes and in September for spring sport athletes. A screening will be scheduled in September for additional spring sport athletes. 3. The walk-on student-athlete must report to the sports medicine office for their physical examination forms. The student-athlete will then obtain a physical examination at his or her own expense. This can be scheduled through the University health services at a minimal cost. 4. All student-athletes will be expected to fill out a "Medical History" form and return it to the head athletic trainer prior to the beginning of their season. These forms will be mailed to the student-athletes during the summer and self-addressed stamped envelopes are provided for their return. Prompt completion of these forms is appreciated. Student-Athlete's Records Protected Health Information (PHI) is information about you, including that information about where you live, that can reasonably be used to identify you and that relates to your past, present or future physical or mental health or condition, the provision of health care to you or the payment for that care. We protect your privacy by: • Limiting who may see your PHI; • Limiting how we may use or disclose your PHI; • Informing you of our legal duties with respect to your PHI; • Explaining our privacy policies; • Adhering to the policies currently in effect. • How we may use and disclose your Protected Health Information (PHI)? In order to administer our sports medicine programs effectively, we will use and disclose PHI for certain activities, including notification of injuries to our athletic injury insurance carrier and your team coaching staff. Medical issues that are unrelated to athletic participation are not communicated without your consent. PHI is also compiled in a catalog for each team. This catalog is given to the head coach of each intercollegiate team and is used solely for the purpose of team Updated June 2013 travel safety. In the event of an injury to a student-athlete on a road trip, the coach would have the ability to share PHI with a medical provider and contact family members who are identified as emergency contacts. Athletic Injury Procedures 1. When injury care is requested, please have confidence in the staff and the method of care the athletic trainer chooses to use. 2. When a treatment regimen is suggested, the student-athlete is expected to cooperate in carrying it out. If a student-athlete fails to follow prescribed procedures this information will be forwarded to the coach. 3. Confidentiality concerning a student-athlete's injury or illness will be maintained. 4. Daily progress reports and weekly summaries may be sent, on request, to the head coach or to someone designated by him/her to receive such information. Such reports will include recommendations on when the athlete may resume activity. 5. The team physician is the FINAL AUTHORITY concerning when a student-athlete should be removed from participation for medical reasons, and when that student-athlete may return to full or partial participation. On occasion, a family physician may make the determination on whether an athlete may resume participation; your family physician must send a letter to our team physician and the Head Athletic Trainer to document this decision. The team physician may overrule your family physician’s decision. 6. Treatment for an injury will be scheduled by the staff or student assistant. All student athletes with injuries will be expected to report at the designated time. "No shows" will not be tolerated. Some rehabilitation will be set up as home programs; the athlete is expected to follow through with all prescribed therapeutic exercise programs. Failure to comply will slow the healing process and delay the athletes return to full activity. Coaches will be updated daily on the status of their athletes as well as any rehabilitation absences or noncompliance. 7. Treatments are to be continued until the medical staff decides they are no longer needed. DO NOT stop receiving treatments just because it "feels better". 8. Doctor appointments for an injury or illness must be made through a staff athletic trainer. If this procedure is not followed and the student-athlete seeks medical attention on their own, the student-athlete will be financially responsible for any and all cost. 9. Emergency treatment for an athletic injury will be channeled through a staff athletic trainer. If emergency room treatment is needed, the staff athletic trainer will notify the team physician and the local hospital. The student-athlete will then be transported to the hospital by a teammate or coach. If an ambulance is needed for transport to the hospital, arrangements will be made by the staff athletic trainer or coach. 10. On occasion injuries will occur on road trips. In the event that a staff athletic trainer cannot accompany a team on the road, the athletic trainer will communicate with coaches and the home athletic training staff on any treatments or injuries that may occur. The home team's certified athletic trainer will assume medical responsibility and make the final determination as to continued play and/or medical care. When possible the athlete will be treated so that they may return home for medical care. This will not be possible on occasion and medical assistance through the host school will be sought. Minors will not be Updated June 2013 treated in emergency rooms beyond immediate necessary treatment without a parent's or guardian's permission. 11. For cheerleading injury reporting, the head coach must notify the athletic training staff immediately of the injury. This may be via email or phone. By doing so, the athletic training staff will arrange a time with the student-athlete for injury evaluation and treatments. Failure to report the injury in a timely manner will result in a game violation. Intercollegiate Practice Policies 1. All athletes must report to the athletic training room in a timely manner prior to practices for any taping or treatments. The athletic training room is NOT an excuse for being late. 2. When a sport is out of season, they MUST conduct practices within the athletic training staff’s hours. If not, that team is practicing at their own risk. During off-season practice, teams are welcome to receive treatments and use water/ ice coolers, but water will not be supplied for them. 3. The Athletic Training Staff may not be present at all intercollegiate practices. In the event that they cannot be out at practice, they will supply water and ice via a work-study student who is certified in first aid and CPR/ AED. This student will be at practice 30-minutes prior to practice until 15 minutes after the coaches have left the field/ gym. In case of an injury, the work-study student will notify the athletic training staff immediately. 4. In the event of an emergency, all coaches must review the Philadelphia University Emergency Action Plan prior to the beginning of each season. They will also maintain CPR/ AED certification every 2 years. Proof of certification will be kept on file in the athletic training room. 5. The athletic training room will remain open until all practices are finished for the day. All post-practice treatments must be arranged with the athletic training staff BEFORE practice of that day, unless a new injury arises. 6. For cheerleading practices, an athletic trainer WILL NOT be on-site. In the event of an emergency, the cheerleading coaches must maintain first aid and CPR/ AED training. Furthermore, they must review the Philadelphia University Emergency Action Plan prior to the beginning of the season. When an injury occurs, the head coach must notify the athletic training staff immediately via email or phone to arrange a time for their athlete to be evaluated and treated. When reporting, the head coach or athlete must state the athletes name, injury, how the injury occurred, and a time when they are available to be treated the following weekday. a. During home games, the athletic trainer on-site will act as the covering athletic trainer for cheerleading. Intercollegiate Competition Policies 1. Philadelphia University must provide an Athletic Trainer for ALL home Varsity intercollegiate competitions or competitions in which Philadelphia University is deemed the “home” or “host” institution. This may involve the use of full time staff, graduate assitants, or per diem Athletic Trainers depending on availability, need, and assessment of other events taking place simultaneously. 2. As the “host” institution of a “home” athletic competition we are liable for treatment, care, and well-being of our own student athletes as well as the student athletes of the travUpdated June 2013 3. 4. 5. 6. 7. eling institution. It is not uncommon that the traveling institution will be unaccompanied by an ATC and therefore as the host institution we must be prepared to treat, assess, evaluate and student athletes from their team if injury occurs. It is expected that we will provide basic courtesy of water and ice to all student athletes of the traveling institution. Staff Athletic Trainers will arrive 2 hours prior to the start of home intercollegiate competitions for the purposes of setup and availability for any pre game treatments. For outdoor sports such as soccer, softball, baseball, etc the Athletic Trainer will aim to arrive at the field between 45 minutes and 1 hour prior to game time in order to assure field set up is complete and to assess the needs of the traveling team. It is the duty of the Athletic Trainer to stay until the conclusion of the competition they are covering regardless of any overtime periods, weather related delays, or delays of any other kind. Upon completion of the competition the Athletic Trainer should give the athletes approximately 15 minutes to report any injuries and get ice if they so wish. The Athletic Trainer will keep an AED with them during covering of all home athletic competitions in case of emergency. Away Events a. Philadephia University Staff Athletic Trainers are expected to provide coverage for the following away events unless athletic conflict prevents OR exception is granted by and agreed upon by (Head ATC, Athletic Director, Head Coach) i. Men’s Basketball ii. Women’s Basektball iii. CACC Cross Country Championships (Host) iv. Men’s and Women’s Soccer Post Season Play v. Volleyball Post Season Play vi. Men’s Soccer @ Wheeling Jesuit (occurs every other yr) vii. Baseball Post Season Play viii. Softball Post Season Play ix. Women’s Lacrosse Post Season Play x. Rowing- Dad Vail Regatta and NCAA competition Medical Expenses and Insurance 1. Insurance information is mandatory from the student-athlete or their parents. This information must be submitted to the head athletic trainer before the student-athlete’s scholarship will be validated. All information requested is necessary to complete our athletic insurance forms. 2. Family insurance is the primary source of payment for all medical expenses. Philadelphia University carries a secondary athletic insurance policy, at no charge, on every varsity athlete. If the family’s insurance coverage terminates during an academic term, the coverage of our athletic insurance company will become primary. If you do not have primary medical insurance the University will automatically enroll you in the Student Injury and Sickness Insurance Plan on the first Friday after classes begin in the fall. The charge for this insurance will be applied to your bill. Families are encouraged to carry a primary insurance; the secondary policy will only cover charges that are considered 'usual and customary'. Typically there are balances that will become the family's responsibility if primary insurance does not cover the excess. Updated June 2013 3. Initially, all medical bills are submitted to the athlete's primary insurance company. If a balance remains after primary insurance has reviewed the claim, then the balance is submitted (along with the primary insurance company's explanation of benefits form) to the secondary carrier. Any balance after this is the student-athlete or his/her family's responsibility. 4. The university maintains a $250.00 deductible on their secondary policy. If the primary insurance pays a minimum of $250.00 on any claim, this deductible is met. If the primary does not pay all or part of this $250.00 then the university will accept responsibility for up to the $250.00 deductible. This deductible will be paid or reimbursed after all insurance claims and payments have been completed. As you can see several steps may be necessary for complete payment of some claims. The head athletic trainer is the University’s representative in coordinating the payment of medical claims. Cooperation between the student-athlete's family, insurance company, and the athletic trainer is necessary for complete payment of athletic injury claims. 5. Student-athletes with HMO coverage must use their plan's covered services whenever possible. A referral is necessary to see the school orthopedist. In most cases a visit to your primary care physician must precede an orthopedic referral. X-rays or other testing that is prescribed must be referred to the student-athlete's HMO primary physician. The Philadelphia University secondary insurance can be used for some items that HMOs may not cover, but denials from the HMO company itself must be received before claims can be submitted to the secondary carrier. 6. The secondary athletic insurance policy only applies to injuries incurred during supervised games, practices, and/or conditioning sessions that are scheduled by the team's coaching staff. This policy doesn't cover: a. Injuries that occur during intramural competitions, 'pick-up' games, or non-sport accidents. b. Pre-existing conditions, even those that have occurred since your university career has started if it was not a school related athletic injury. c. Dental injuries are only covered if there is damage to a healthy, sound tooth or teeth. Our dental coverage has a $250.00 per tooth maximum benefit. 7. The athletic training department maintains a supply of dispensable medical goods (e.g. tape, Band-Aids, pads, ace wraps, etc...) these are for the prevention and treatment of athletic injuries throughout the entire academic year. Braces that are prescribed by physicians are ordered through a third party provider and the bills are submitted through your insurance. Medical facilities Health Services: Philadelphia University has a Student Health Center located on the lower level of Scholler Hall. It is staffed by nurse practitioners. Walk In Hours are Monday-Friday from 9:30am to 12:30. Appointments are available until 4:30. Medical care and some preventative services are available. Students are responsible for the cost of prescriptions, medical tests, and specialty care. Updated June 2013 Hospitals: Philadelphia University is close to Roxborough Hospital and Temple University Hospital. Philadelphia University security will transport any student to Roxborough Hospital, at no charge, for emergency care. Occupational Safety and Health Administration (OSHA) 1. Occupational Safety and Health Administration has mandated health standards and guidelines under which the athletic training rooms must comply. Rules and regulations must be followed by the staff and student trainers. Your cooperation in such matters will be greatly appreciated. 2. There are no known cases of HIV or AIDS being transmitted through athletics at this time. However, report all open wounds, scratches, abrasions, etc. to the head athletic trainer or student assistants immediately for first aid care. 3. The NCAA has specific rules in all sports governing the treatment of open wounds during athletic events; the athletic training staff must treat all wounds in accordance with these rules. This may include removal from the game until bleeding has been controlled and the wound dressed and the uniform cleaned properly or replaced. Athletic Training Room Rules 1. All injuries should be reported immediately. It is very difficult to care for an injury without knowledge of its existence. 2. Everyone must sign-in prior to any treatment. 3. Everyone must have a pre-participation sport screening physical prior to competing/practicing in an intercollegiate sport. There are no exceptions to this rule. 4. Student-athletes will be treated and/or taped in the order in which they come into the athletic training room. During busy periods athletes should allow sufficient time for their treatment based upon all of the teams being treated during that season. Team coaches don't accept daily treatments as excuse for lateness to practices or games. 5. Acute injuries will be treated based upon their severity according to the rules of medical triage. 6. No one is permitted in the athletic training room except (a) while receiving injury care, or (b) by request of a member of the sports medicine staff. If a trainer asks a student athlete to wait outside the athletic training room, the student-athlete is expected to cooperate since crowded conditions simply slow down the work process. 7. No training items (tape, wraps, scissors, etc.) or rehabilitation equipment should be taken from the athletic training room without the consent of a member of the sports medicine staff. 8. No "horseplay", profanity, racial comments, or other forms of disruptive behavior will be allowed in the athletic training room. 9. No nudity or dressing is allowed; the Philadelphia University training rooms are co-ed, appropriate clothing must be worn at all times. No spikes or cleated shoes are allowed inside the athletic training room. 10. The telephone and computers in the athletic training room and offices are for STAFF USE ONLY. Updated June 2013 Philadelphia University Sports Medicine Emergency Action Plan Introduction Emergency situations may arise at anytime during athletic events. Expedient action must be taken in order to provide the best possible care to the sport participant of emergency and/or life threatening conditions. The development and implementation of an emergency plan will help ensure that the best care will be provided. As emergencies may occur at anytime and during any activity, the athletic association must be prepared. Athletic organizations have a duty to develop an emergency plan that may be implemented immediately when necessary and to provide appropriate standards of emergency care to all sports participants. As athletic injuries may occur at any time and during any activity, the sports medicine team must be prepared. This preparation involves formulation of an emergency plan, proper coverage of events, maintenance of appropriate emergency equipment and supplies, utilization of appropriate emergency medical personnel, and continuing education in the area of emergency medicine and planning. Hopefully, through careful pre-participation physical screenings, adequate medical coverage, safe practice and training techniques and other safety avenues, some potential emergencies may be averted. However, accidents and injuries are inherent with sports participation, and proper preparation on the part of the sports medicine team should enable each emergency situation to be managed appropriately. Components of the Emergency Plan These are the basic components of this plan: 1. Emergency Personnel 2. Emergency Communication 3. Emergency Equipment 4. Roles of First Responder 5. Emergency Action Plan Checklist for Non-medical Emergency Emergency Plan Personnel With athletic association practice and competition, the first responder to an emergency situation is typically a member of the sports medicine staff, most likely a certified athletic trainer. The type and degree of sports medicine coverage for an athletic event may vary widely, based on such factors as the sport or activity, the setting, and the type of training or competition. The first responder in some instances may be a coach or other institutional personnel. Certification in cardiopulmonary resuscitation (CPR), first aid, prevention of disease transmission, and emergency plan review is required for all athletics personnel associated with practices, competitions, skills instruction, and strength and conditioning. The development of an emergency plan cannot be complete without the formation of an emergency team. The emergency team may consist of a number of healthcare providers including physicians, emergency medical technicians, certified athletic trainers; student athletic trainers; coaches; managers; and, possibly, bystanders. Roles of these individuals within the emergency team may vary depending on various factors such as the number of members of the team, the athletic venue itself, or the preference of the head athletic trainer. There are four basic roles within the emergency team. The first and most important role is establishing safety of the scene and immediate care of the athlete. Acute care in an emergency situation should be provided by the most qualified individual on the scene. Individuals with lower credentials should yield to those with more Updated June 2013 appropriate training. The second role, EMS activation, may be necessary in situations where emergency transportation is not already present at the sporting event. This should be done as soon as the situation is deemed an emergency or a lifethreatening event. Time is the most critical factor under emergency conditions. Activating the EMS system may be done by anyone on the team. However, the person chosen for this duty should be someone who is calm under pressure and who communicates well over the telephone. This person should also be familiar with the location and address of the sporting event. The third role, equipment retrieval may be done by anyone on the emergency team who is familiar with the types and location of the specific equipment needed. Student athletic trainers, managers, and coaches are good choices for this role. The fourth role of the emergency team is that of directing EMS to the scene. One member of the team should be responsible for meeting emergency medical personnel as they arrive at the site of the emergency. Depending on ease of access, this person should have keys to any locked gates or doors that may slow the arrival of medical personnel. A student athletic trainer, manager, or coach may be appropriate for this role. Roles within the Emergency Team 1. Establish scene safety and immediate care of the athlete 2. Activation of the Emergency Medical System 3. Emergency equipment retrieval 4. Direction of EMS to scene Activating the EMS System Making the Call: · notify campus police at x2999 · 9-911 (through campus phone) · telephone numbers for local police, fire department, and ambulance service Providing Information: · name, address, telephone number of caller · nature of emergency, whether medical or non-medical * · number of athletes · condition of athlete(s) · first aid treatment initiated by first responder · specific directions as needed to locate the emergency scene ("come to south entrance of coliseum") · other information as requested by dispatcher * if non-medical, refer to the specific checklist of the emergency action plan When forming the emergency team, it is important to adapt the team to each situation or sport. It may also be advantageous to have more than one individual assigned to each role. This allows the emergency team to function even though certain members may not always be present. Emergency Communication Communication is the key to quick emergency response. Athletic trainers and emergency medical personnel must work together to provide the best emergency response capability and should have contact information such as telephone tree established as a part of pre-planning for emergency situations. Communication prior to the event is a good way to establish boundaries and to build rapport between both groups of professionals. If emergency medical transportation is not available on site during a particular Updated June 2013 sporting event then direct communication with the emergency medical system at the time of injury or illness is necessary. Access to a working telephone or other telecommunications device, whether fixed or mobile, should be assured. The communications system should be checked prior to each practice or competition to ensure proper working order. A back-up communication plan should be in effect should there be failure of the primary communication system. The most common method of communication is a public telephone. However, a cellular phone is preferred if available. At any athletic venue, whether home or away, it is important to know the location of a workable telephone. Pre-arranged access to the phone should be established if it is not easily accessible. Emergency Equipment All necessary emergency equipment should be at the site and quickly accessible. Personnel should be familiar with the function and operation of each type of emergency equipment. Equipment should be in good operating condition, and personnel must be trained in advance to use it properly. Emergency equipment should be checked on a regular basis and use rehearsed by emergency personnel. The emergency equipment available should be appropriate for the level of training for the emergency medical providers. Creating an equipment inspection log book for continued inspection is strongly recommended. It is recommended that a few members of the emergency team be trained and responsible for the care of the equipment. It is important to know the proper way to care for and store the equipment as well. Equipment should be stored in a clean and environmentally controlled area. It should be readily available when emergency situations arise. Medical Emergency Transportation We are not required to have an ambulance at any of our sporting events by NCAA rules. In the event of an emergency, the 911 system (9-911 on campus) will still be utilized for activating emergency transport. In the event that an ambulance will be used, there should be a designated location with rapid access to the site and a cleared route for entering/exiting the venue. In the medical emergency evaluation, the primary survey assists the emergency care provider in identifying emergencies requiring critical intervention and in determining transport decisions. In an emergency situation, the athlete should be transported by ambulance, where the necessary staff and equipment is available to deliver appropriate care. Emergency care providers should refrain from transporting unstable athletes in inappropriate vehicles. Care must be taken to ensure that the activity areas are supervised should the emergency care provider leave the site in transporting the athlete. Any emergency situations where there is impairment in level of consciousness (LOC), airway, breathing, or circulation (ABC) or there is neurovascular compromise should be considered a “load and go” situation and emphasis placed on rapid evaluation, treatment and transportation. Updated June 2013 Conclusion The importance of being properly prepared when athletic emergencies arise cannot be stressed enough. An athlete’s survival may hinge on how well trained and prepared athletic healthcare providers are. It is prudent to invest athletic department “ownership" in the emergency plan by involving the athletic administration and sport coaches as well as sports medicine personnel. The emergency plan should be reviewed at least once a year with all athletic personnel, along with CPR and first aid refresher training. Through development and implementation of the emergency plan, the athletic association helps ensure that the athlete will have the best care provided when an emergency situation does arise. Updated June 2013 Philadelphia University Concussion Protocol What is a Concussion? Mayo Clinic defines a concussion as “a traumatic brain injury that alters the way your brain functions. Effects are usually temporary, but can include problems with headache, concentration, memory, judgment, balance and coordination.” There are a wide variety of signs, symptoms, and behaviors consistent with a concussion. Common signs, symptoms, and behaviors are listed in the table below. It should be noted, an athlete with a concussion does not have to experience loss of consciousness (LOC). If an athlete has had a concussion previously, then they are at increased risk to have another concussion. The more concussions a student athlete has had, the longer it may take for that athlete’s brain to recover; in addition, the effects of repetitive concussions may be cumulative. Possible complications and consequences of a concussion include but are not limited to: post-concussion syndrome, second-impact syndrome, and perhaps neuropathologic changes such as chronic traumatic encephalopathy from repetitive head injuries. Possible consequences of any head injury include death or permanent disability. If an athlete is unsure if they have a concussion but “don’t feel right”, then they should proceed as if they have a concussion. As a general rule, when in doubt, get it checked out. Common Signs and Symptoms of a Concussion Headache Dizziness Nausea Balance Difficulties Light Sensitivity Fatigued Blurred Vision Easily Distracted Feeling “In a Fog” Unusually Emotional Irritability Loss of Consciousness Loss of Orientation Memory Problems Nervousness Personality Changes Ringing in the Ears Sadness Seeing Stars Sensitivity to Noise Sleep Disturbances Vacant Stares Vomiting Confusion Concussion Testing All student-athletes will undergo baseline concussion assessments through the sports medicine department prior to ANY athletic participation. This will consist of a thorough concussion history, neurocognitive (ImPACT) testing, and postural-stability testing. These tests will also be used in our concussion evaluation techniques. Updated June 2013 Concussion Reporting All athletes will sign a statement acknowledging the risks of concussion and accepting the responsibility of reporting ALL injuries and illnesses to the sports medicine staff. If any athlete experiences a blow to the head and experiences ANY concussion symptoms, they will be held out from participation for the remainder of the day. At the time of injury, a sports medicine professional will evaluate the athlete for acute signs and symptoms of a concussion. The attending Certified Athletic Trainer (ATC) will utilize a Sport Concussion Assessment Tool to assess the athlete’s cognitive and physical symptoms. If a student athlete demonstrates any symptoms of a concussion, they will not be allowed to participate in athletic activities until they have been cleared to begin the Return to Play progression. Following the initial concussion assessment, the student athlete is to report to the athletic training room within 24 hours of the injury to undergo a post-injury ImPACT test. They will also report signs and symptoms daily to the ATC until they have been symptom-free for 24 hours. Once they have been asymptomatic for 24 hours and have been cleared by Drexel Sports Medicine, they can begin the Return to Play progression. Return to Play Progression Rehabilitation Stage Level 1 – No Activity Level 2 – Light Aerobics Level 3 – Moderate Aerobics Level 4 – Sport-Specific Activity Level 5 – Non-Contact Level 6 – Full-Contact Normal Game Play Functional Exercise Physical and Cognitive Rest Stationary Bike (10-20 minutes) Consistent Running (30 minutes) Sprinting, Light Resistance Training SAQ drills, Progression to more complex drills Normal Training Activity Return to Play Progression (RTP) will not begin until athlete is asymptomatic for a full 24 hours and has been cleared by Drexel Sports Medicine to begin activity. If ANY symptoms return during Levels 1-6, athlete must stop all activity and wait until symptom-free for full 24 hours. Once they are asymptomatic again, they will begin from Level 1 of RTP progression. Updated June 2013 Heat Policy (for the fall camps) Head athletic trainer will monitor the temperature and the humidity several times daily, after which he/she will advise all of the coaches on what type of changes in their practices (modified workout, walk through, etc.) if any they should make or if the practice should be cancelled. Prevention is the key to any heat illness make sure athletes are acclimatized to the environment. Below is the National Oceanic and Atmospheric Association Heat Index which will be used to make practice/competition decisions: Caution Zone: Most long-term residents of will be acclimated to the “Caution” zone temperature/humidity range above. Fluids should be encouraged, and the “Heat Stress Prevention: General Tips” on the following pages should be followed. Extreme Caution Zone: Fluids, shaded breaks, and decreased activity are required when the temperature/humidity readings reach this level. Watch for signs/symptoms of heat exhaustion and heat stroke. Practices for athletic teams and bands should be moved off high heat surfaces (cinders, sand, concrete, asphalt, etc.) to grassy areas. Updated June 2013 Danger Zone: Most people working in this temperature/humidity range for a prolonged period will experience heat exhaustion and some may have heat stroke. Activities in this range must be severely curtailed, and cooling stations or indoor breaks must be used regularly. Fluids should be taken at a rate of about one quart per person per hour. Practices for marching bands and athletic teams should be moved indoors or scheduled for a cooler part of the day. Parades and athletic competitions that must be completed in this heat index range must be supported by the following: • Designated persons must provide fluids to all participants at a rate of one quart per person per hour. • Responsible persons must be available to regularly assess all participants for signs & symptoms of heat exhaustion and heat stroke. Extreme Danger Zone: Heat exhaustion is probable and heat stroke is likely in this extreme heat index range. Outdoor practices, athletic events, parade participation and most other outdoor activities should be cancelled. Outdoor physical education classes should be kept indoors. Employees should limit outdoor exposure in this heat/humidity range. Breaks for cooling must be provided every hour, along with hydration of at least one quart per hour. Supervisors should attempt to reschedule outdoor labor projects to cooler times of morning or evening if possible. No worker should be left unattended performing heavy labor in this heat index range. Updated June 2013 Fluid Replacement Guidelines and Exertional Heat Illnesses The following policy on fluid replacement, rehydration, and exertional heat illnesses has been developed in accordance with the NATA Fluid Replacement Position Statement, the NATA Exertional Heat Illnesses Position Statement, and Philadelphia University Department of Sports Medicine’s Mission Statement to provide quality healthcare services and assure the well-being of each student-athlete at Philadelphia University. RATIONALE OF FLUID REPLACEMENT: Student-athletes who are exposed to prolonged practices and competitions in an excessively hot and humid environment may be deprived of essential fluids, carbohydrates, and electrolytes that an ultimately lead to dehydration and potential heat illness. It has been demonstrated that dehydration of just 1-2% of body weight (1.5-3 pounds for a 150pound athlete) can alter physiological function and negatively influence an athlete’s performance. Athletes who are not properly hydrated prior to the start of practice or competition can begin to notice the signs of dehydration in just one hour or sooner of exercise. Dehydration has been identified as an increased risk factor for athletes developing heat-related illness such as heat cramps, heat exhaustion, and the potentially life-threatening heat stroke. SIGNS AND SYMPTOMS OF DEHYDRATION: Staff athletic trainers, graduate assistant athletic trainers, and athletic training students all need to be aware of the signs and symptoms of dehydration to properly recognize and intervene on behalf of the student-athlete. Signs and Symptoms are: 1. Thirst 7. Nausea 2. Irritability 8. Cramps 3. General discomfort 9. Chills 4. Headache 10. Vomiting 5. Weakness 11. Head or neck heat sensations 6. Dizziness 12. Decreased performance Updated June 2013 REHYDRATION GUIDELINES: The Sports Medicine Staff at Philadelphia University has developed the following rehydration guidelines based on national accepted criteria. The Sports Medicine Department Staff will assist in promoting the consumption of beverages. All beverages will be provided onsite when requested or as deemed necessary. Prior to Exercise: All athletes should be encouraged to drink 17 to 20 fluid ounces of water or sports beverage (with 6-8% charbohydrates) 2-3 hours before exercise. Ten to twenty minutes before the beginning of practice or competition, athletes should be encouraged to drink an additional 7-10 fluid ounces of water or sports beverage. During Exercise: Encourage athletes to drink early and often – by the time an athlete is thirsty they are already dehydrated. Drink 7-10 fluid ounces or sports drink every 10-20 minutes. It is important to stress to the athletes to drink prior to becoming thirsty. An athlete who is thirsty may already be in the early stages of dehydration. After Exercise: Encourage athletes to replace any fluid loss due to sweating within 2 hours from the end of exercise. This rehydration should include water, carbohydrates, and electrolytes to allow the immediate return of physiologic function. Encourage them to drink 20-24 fluid ounces for every pound of weight lost. **Sport beverages should ideally contain a carbohydrate level of no more than 8%. A higher carbohydrate level can retard fluid absorption and cause stomach problems. **Fruit juices, carbohydrate gels, and carbonated beverages should not be recommended as the sole rehydration beverage of choice. Beverages containing caffeine, alcohol, or carbonation should be avoided and discouraged due to their diuretic effects and decreased fluid retention. WEIGHT LOSS/GAIN GUIDELINES: It is recommended that all athletes exercising in hot and humid environments as well as those sports such as wrestling with closely regulated weight classes be weighed in prior to and after practice or competition. By weighing in, a determination can be made of the percentage body weight lost due to sweating and the amount of rehydration that must occur prior to the next prac- Updated June 2013 tice session. Furthermore, athletes should be weighed preferably in the nude, in clean/dry undergarments, or wearing the same amount of clothing pre-and post-practice. The percentage of weight lost between practice sessions will be used as one factor to determine if an athlete can safely continue to practice. Athletes should ideally have their pre-exercise body weight remain relatively consistent. A 2% body weight difference should be noted by the athletic trainer and that athlete should be closely monitored for any signs or symptoms of dehydration. An athlete with greater than 2% body weight loss should not be allowed to return to practice until proper fluid replacement has taken place. INTRAVENOUS (IV) FLUID REPLACEMENT: In certain instances an athlete may receive intravenous fluid replacement therapy to combat dehydration or associated heat illnesses. This form of treatment will be conducted at the discretion of the Team Physician. In the absence of the Team Physician, if the attending certified athletic trainer determines that an athlete may be suffering from dehydration or associated heat illness, he/she will make every effort to contact the Team Physician and/or arrange for treatment to be administered through the closest hospital emergency room. DEFINITION OF HEAT ILLNESS: Heat illness if closely associated with physical activity and its occurrence increases with a rise in temperature and relative humidity. It is usually classified in three categories: heat cramps, heat exhaustion, and heat stroke. Although most often occurring in hot, humid weather, heat illness can also occur with the absence of both heat and/or humidity. Exercise-Associated Muscle (Heat) Cramps: Occurs during or after intense exercise as an acute, painful, and involuntary muscle contraction Causes may include dehydration, electrolyte imbalances, neuromuscular fatigue, or a combination of factors. Signs and Symptoms: dehydration, thirst, sweating, transient muscle cramps, fatigue. Exercise (Heat) Exhaustion: Occurs most frequently in hot, humid conditions and causes an inability to continue exercise. May be caused by dehydration, heavy sweating, sodium loss, and energy depletion. Updated June 2013 Signs and Symptoms: pallor, persistent muscle cramps, urge to defecate, weakness, fainting, nausea, decreased urine-output, cool and clammy skin, anorexia, diarrhea, body temp between 97-104°F. Exertional Heat Stroke: Occurs when core temperature is elevated (usually greater than 104°F) with associated signs of organ system failure due to hyperthermia and physical activity. Caused by an overwhelmed temperature regulation system due to excessive endogenous heat production or inhibited heat loss due to environmental conditions. Signs and Symptoms: tachycardia, hypotension, sweating (although skin may be wet or dry), hyperventilation, altered mental status, vomiting, diarrhea, seizures, coma, CNS changes Life-threatening condition that can be fatal unless promptly recognized and treated. PREVENTION OF HEAT ILLNESS GUIDELINES: All pre-participation examinations will identify student-athletes who may be predisposed to heat illness or have a history of heat illness. The Sports Medicine Department Staff will be onsite at most practices and competitions to assist in providing hydration and access to further cooling supplies. Along with athletic training students, the staff will be aware of the signs and symptoms of heat illness to properly recognize and intervene on behalf of the student-athlete. The certified athletic trainer will also help educate athletes and coaches regarding the necessary time needed to have student-athletes adapt to their environment. Acclimatization should be a gradual progression. Well-acclimatized athletes should be able to train 1 to 2 hours under the same heat conditions that will be present for their event. In addition, the certified athletic trainer should know how to use a wet-bulb globe temperature (WBGT) and/or a sling psychrometer, decipher the corresponding temperature graphs for these instruments, and base the level of physical activity upon the gathered information. This will be used as one of the factors in determining any risk of heat illness associated with relevant environmental conditions. TREATMENT OF HEAT ILLNESS: The Sports Medicine Department will treat heat illness by recognizing its signs and symptoms, understanding the causes of heat illness, and taking the necessary measures to ensure an efficient and safe recovery for the student-athlete. Exercise-Associated Muscle (Heat) Cramps: Updated June 2013 The student-athlete should stop activity, replace lost fluids (containing sodium), and begin mild stretching and massage of the muscle spasm. Instruct the student-athlete to lie down, as this may allow blood flow to be distributed more rapidly to cramping leg muscles. Exercise (Heat) Exhaustion: Assess cognitive function and vital signs, taking body-core temperature if possible. Transport the athletes to a cool and/or shaded environment, remove excess clothing, start fluid replacement, and cool the student-athlete with fans, ice towels, or ice bags (placed in armpits, neck, and groin). The student-athlete should be referred to the team physician and/or the emergency room of the closest hospital if in the judgment of the attending certified athletic trainer symptoms warrant further immediate attention. Exertional Heat Stroke: Activate the emergency medical system. Assess cognitive function and vital signs, measuring rectal temperature if feasible to differentiate between heat exhaustion and heat stroke (heat stroke is 104°F or higher). Lower the body-core temperature as quickly as possible by removing excess clothing and immersing the body into a tub of cool water (35 - 59°F) while checking temperature every 5 to 10 minutes. Remove athlete from water if temperature reaches 101 to 102°F to prevent overcooling. Continue using cooling methods mentioned for heat exhaustion while transporting to decrease body-core temperature. Maintain and monitor airway for breathing and circulation. RECOVERY OF HEAT ILLNESS: Athletes who experience a heat stroke may have impaired thermoregulation, persistent CNS dysfunction, and hepatic or renal insufficiency following recovery. Decreased heat tolerance has been shown to affect 15% to 20% of athletes experiencing a heat stroke-related collapse. Following recovery, the student-athlete’s activity should be restricted with a gradual return regulated by the Team Physician. Updated June 2013 Lightening Policy Philadelphia University Athletics will use the following methods to monitor lighting in accordance to the NATA recommendations regarding lightning safety: I. Lightning Detector: In the case of inclement weather, the attending athletic trainer is to turn on the lightning detector application on their mobile device. Once it goes off detecting lightning within 3-8 miles, the athletic trainer will notify the Head Coach and Officials immediately to suspend play. If lightning occurs during a practice, one individual on the coaching staff is required to have lightning detection activated on their mobile phone. Flash-to-Bang Method: After a flash of lightning, count the seconds until the bang of thunder. Divide this number by 5. The product is an estimate of how many miles away the lightning is. (5 sec = 1 mile) II. Chain of Command: In the event of a lightning storm, a member of the sports medicine staff will monitor the local weather with the utilization of the flash-to-bang method for determining proximity of lightning strikes and to suspend activity in the event of imminent lightning. In the event that a member of the sports medicine staff is not present during the storm, another qualified individual (i.e. member of Athletic Administration, Head Coach, and Officials) will suspend activity. III. Suspending Activity: Once lighting enters the 30 mile radius of practice/competition, we will begin preparations to protect the student-athletes and spectators. Once lighting enters a 3-8 mile radius of practice/competition, all outside activities must stop and student-athletes and spectators will be moved to safe structures. 30 minute time frame begins at the last sight/sound of lightning/thunder and/or last flash within 3-8 miles on the lightning detector. IV. Competition/Practice: Prior to competition or practice, a member of the athletic training staff will meet with the officials/coaches and offer to monitor imminent danger from lightning. 1. Once it is determined there is danger of a lightning strike, the athletic trainer or athletic administrator will notify the head coach and official. 2. The official/coach will subsequently summon athletes, coaches, and spectators off the playing field via a horn or whistle. 3. During competitions, a message will be read over the public address system warning individuals of the danger and guiding them to the nearest safe structure. V. Safe Structure: Immediately following suspension of play, all athletes, coaches, officials, and support personnel are to evacuate to an enclosed grounded structure.(example: locker room, lower level of center of parking deck or stairwell, grounded press box). If unable to reach shelter immediately, seek a flat area, (not an open area where you will be the highest object) or a ditch Updated June 2013 without water, and crouch down wrapping your arms around your knees, lower your head, and wait for the storm to pass. Due to conduction of electricity wearing metal spikes, athletes should remove shoes, and should not hold metal equipment (golf clubs, bats, etc.) A suitable shelter is any building normally occupied or frequently used by people (a building with pluming or electrical wiring that acts to electrically ground the structure.) Avoid using shower facilities and land-line telephones (in the case of an emergency use a cell phone) during thunderstorms. Automobiles, golf carts, dugouts, and open structures do not provide adequate protection from lightning. If there is no other shelter, you may seek refuge in a hardtop vehicle with windows rolled up. While inside of the vehicle do not touch any of the metal frame of that vehicle it is what dissipates the electrical charge, not the rubber tires. Sport Specific Evacuation Locations o Ravenhill Field: Ravenhill Dining Hall o Softball Field: Tuttleman Center o Tennis Courts: Gallagher Athletic, Recreation, and Convocation Center o Alumni Field: Gallagher Athletic, Recreation, and Convocation Center o Away contest: Athletic trainer or head coach should find out procedure from host athletic trainer and report back to the athletes and coaching staff. VI. Resuming Activity: As stated above, lightning strikes will be determined with the utilization of the flash-to-bang method. Decision to return to play will be determined by a member of the sports medicine staff, athletic administrator, both home and away head coaches, and officials. Play may resume after 30 minutes have passed since the last lighting strike inside the 3-8 mile warning ring. **Note: Individuals who have been struck by lightning do not carry an electrical charge; therefore CPR is safe for the responder. In the event that a person has been struck by lightning, follow the site emergency action plan. Updated June 2013