Hypospadias
DEFINITION
a congenital anomaly characterized by a ventrally placed urethral meatus in a
more proximal position on the midline than its normal position in the glanular
part of the penis
INCIDENCE
1 in every 200 to 300 male births (G + S)
Evidence of increasing incidence
Older maternal age
Low birth weight
improved fertility in men treated for cryptorchidism and hypospadias in the
postwar decades
The majority of cases occur sporadically (90%)
About 5-10% have a family history:
Fathers have Hypospadias in 7-10% of patients.
Brothers have Hypospadias in 10-20% of patients.
In some families multiple members are affected.
Whites > Blacks.
More common in Italians and Jews
ANATOMY
Local abnormalities include:
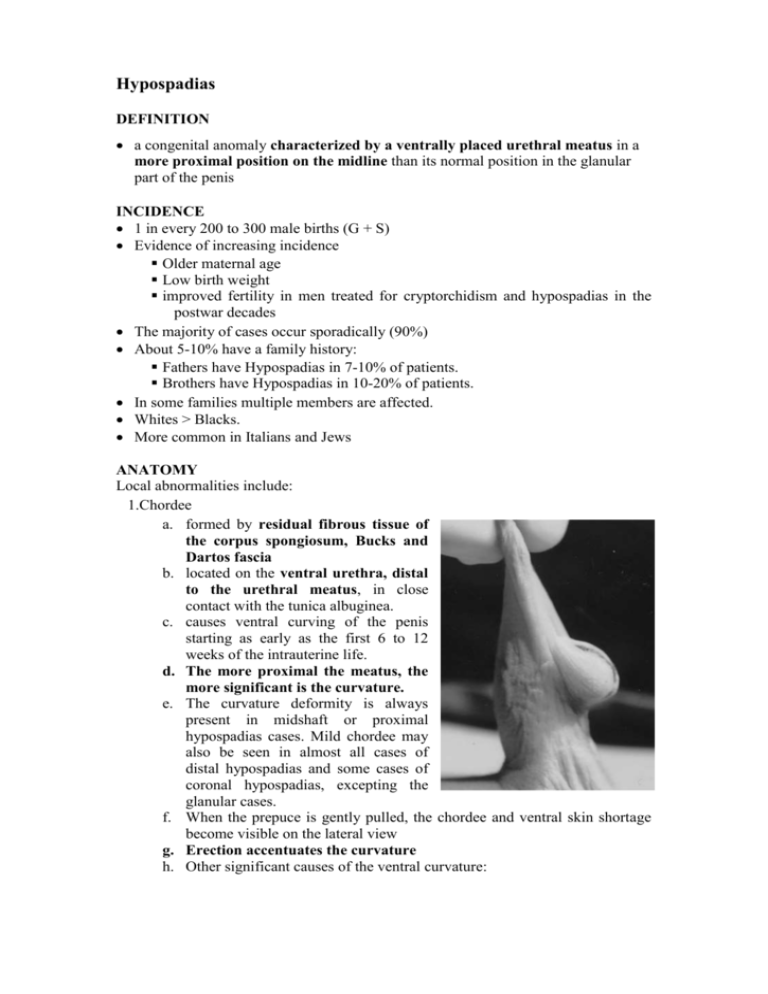
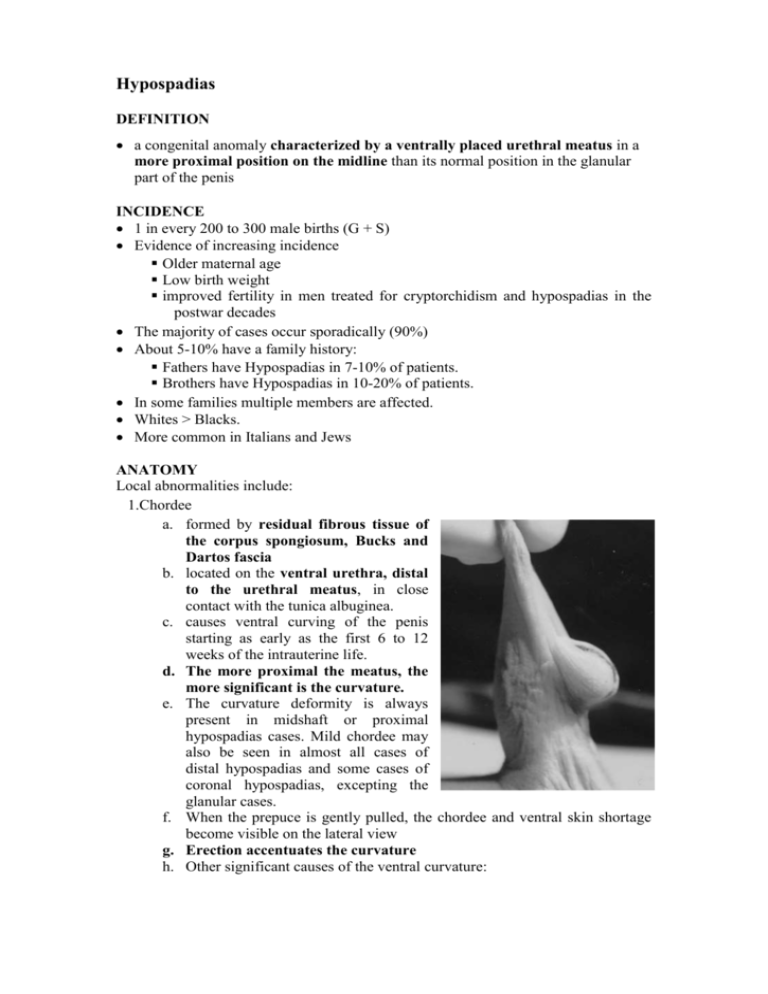
1.Chordee
a. formed by residual fibrous tissue of
the corpus spongiosum, Bucks and
Dartos fascia
b. located on the ventral urethra, distal
to the urethral meatus, in close
contact with the tunica albuginea.
c. causes ventral curving of the penis
starting as early as the first 6 to 12
weeks of the intrauterine life.
d. The more proximal the meatus, the
more significant is the curvature.
e. The curvature deformity is always
present in midshaft or proximal
hypospadias cases. Mild chordee may
also be seen in almost all cases of
distal hypospadias and some cases of
coronal hypospadias, excepting the
glanular cases.
f. When the prepuce is gently pulled, the chordee and ventral skin shortage
become visible on the lateral view
g. Erection accentuates the curvature
h. Other significant causes of the ventral curvature:
i. asymmetric distribution of the skin around the penis can originate
some degree of curvature both in distal and in proximal hypospadias.
In severe cases, there may be a penoscrotal web
ii. asymmetry of the tunica albuginea, which accounts for the permanence
of the curvature despite the excision of the entire fibrous chordee
iii. growth differential between the corpora cavernosa and the corpus
spongiosum.
2.Prepuce
a. In proximal hypospadias, the prepuce is asymmetric, accumulating on the
dorsum of the penis and being deficient on the ventral segment.
b. Gives glans a dorsal hooded appearance.
c. Width of the ventral deficiency of prepuce = width of dysgenetic band
causing the chordee
d. The prepuce may be normal in distal hypospadias in up to 7% of cases.
Axial kicking of the shaft of the penis occurs in 14% of patients, and is not
dependent on the degree of hypospadias.
3.Urethral meatus stenosis
a. less frequent in proximal hypospadias(15%)
4.Scrotal abnormalities
a. Proximal hypospadias are usually associated with scrotal malformations,
such as penoscrotal synaechia, hypoplasia, bifid scrotum and high scrotum
implantation.
5.Other associations
a. Undescended testes (10%) – female karyotype until proven otherwise if
shows combination of undescended testes and hypospadias
b. Inguinal hernia (10%)
c. Upper urinary tract anomalies (1-3%) – higher risk with proximal
hypospadias
AETIOLOGY
a deficiency of androgens during embryogenesis.
CLASSIFICATION
1. Browne, 1936 Classification according to original site of meatus.
2. Barcat, 1973Classified hypospadias according to the new position of the urethral
orifice acquired intraoperatively after the surgical removal of chordee This is the
preferred classification (Duckett).
i. Distal (80%)
a)
Glandular
b)
Coronal
c)
Distal penile
d)
Mid penile
ii. Proximal (20%)
a)
Proximal Penis
b)
Penoscrotal
c)
Scrotal
d)
Perineal
ASSESSMENT
Whenever possible, the child should be seen as a newborn.
On examination, note:
i. meatal position,
ii. adequacy of the meatus (if the meatus is too tight a neonatal meatotomy may
be required),
iii. cryptorchidism
iv. ambiguous genitalia
v.other congenital anomalies.
Whether or not to do an IVP is controversial. Serafin + Georgiade recommend
doing IVP if:
1. Hypospadias more proximal,
2. Hypospadias (of any degree) associated with cryptorchidism,
3. Hypospadias (of any degree) associated with any other organ system
anomalies.
If the patient has glandular or coronal Hypospadias and is otherwise normal, the
yield from IVP is too low to warrant the procedure.
In cases of ambiguous genitalia, tests include sexual chromatin investigation,
karyotype, stimulation test using chorionic gonadotrophin, pelvic sonographic
screening and retrograde and urinary urethrocystography, and eventually biopsy of
the gonad.
HISTORY OF HYPOSPADIAS REPAIRS
Original operations were staged, first stage being correction of chordee and second,
construction of a neourethra
i. Stented SSG urethroplasty
o Devised by Novè-Joserand. This technique consisted of a split-thickness
graft to fill a channel in the penis. The split-thickness graft required stenting
for many months because of the inherent contracture. Stenoses and strictures
occurred with this technique, and it was abandoned.
o Later popularized by McIndoe, who recommended that the stent be left in
place for 6 to 12 months to overcome the tendency for contracture. This
technique has many complications and is no longer used.
ii. Sutured ventral tube urethroplasty
o Thiersche and Duplay performed a two-stage repair in which they first
resected the tissue causing chordee and straightened the penis. The penile
skin was closed, and months later the urethra was constructed by making
longitudinal incisions down the ventral surface of the penis to form a urethra
tube undermining the lateral skin flaps and covering the buried tube of skin.
The deficiency of this operation was that it never adequately extended the
urethra to the tip of the glans. In many cases, adequate tissue for
construction of the urethra and coverage of a new urethral tube was not
present.
o The technique, however, was successfully reintroduced and popularized by
Blair and Byars. This operation was probably the most common type of
hypospadias repair reported in the literature until one-stage repairs became
popular. Browne modified the technique by not making the ventral strip of
skin into a tube, but simply leaving it as a strip of skin covered by the lateral
skin flaps of the ventral surface of the penis. This ventral strip of skin then
tubed itself with normal circumferential growth, and the urethra was formed.
This simple technique gained popularity for hypospadias repair, but the
complication rate was so high that the operation has been largely abandoned
by most hypospadias surgeons. All of these operations ended with a
subglandular meatus.
iii. Closed ventral tube urethroplasty sutured to a scrotal bed
o introduced by Cecil during the mid 1940s, addressed the fact that adequate
shaft skin was difficult to obtain in all cases.
o after the chordee was released and the penis straightened, the urethra was
constructed at a second stage, 6 months later, of tubed ventral penile skin by
making parallel longitudinal incisions.
o Rather than attempt coverage of the urethra with flaps of penile skin, an
incision was made into the scrotum, and the penis was sutured into the
scrotal bed. The penis was left in this position for 6 to 8 weeks with the new
urethra covered.
o At a third stage, the scrotum was released from the penis, leaving normal
vascularized scrotal skin present on the ventral surface of the penis. This
technique is still useful for certain complicated hypospadias cripples;
however, it has largely been abandoned as a primary form of hypospadias
repair.
o Cannot be recommended because of the undesirable aesthetic appearance of
the scrotal skin on the penis and because it is a three-stage operation with a
high complication rate.
In 1961, C. E. Horton and C. J. Devine, Jr., developed single-stage modern surgical
techniques, namely, local skin flaps and free skin grafts, for urethra reconstruction
in hypospadias repair, which may be applied to almost any case with different
localizations of the meatus. Later, two new methods, advancement of the urethra
and preputial island flap techniques, were added to the surgical algorithm.
AIMS OF SURGICAL REPAIR
One stage procedures are now regarded as being superior to multi-staged repairs.
Aims:
1. A normally sited meatus at the tip of the glans.
2. A complete release of chordee with straightening of the penis.
3. A normal urinary stream without spraying.
4. Absence of excessive scar tissue or redundant skin.
5. The ability to produce a normal erection.
In all but the most distal forms of hypospadias, the dysgenetic band of fibrous
tissue must be removed to correct the chordee.
NEVER circumcise a child with hypospadias. The extra skin of the hood of
the prepuce dorsally will generally be used for the construction of the new
urethra or resurfacing of the ventral skin defect.
TIMING OF SURGICAL REPAIR
Definitely < 12 years and most say that surgery should be complete before the
child starts school.
According to Devine (in Mustarde), reconstruction should be complete before the
child has any memory of it, yet it should be delayed until the child can cooperate
and understand what is said to him. He therefore recommends that surgery should
be done around the time of the child’s 2nd birthday.
At PHM, between 6 – 12 months
1. post operative care tends to be less complicated
2. size of the penis is almost equivalent to that of a 3 year old child
3.
trophic conditions of the skin allow a high degree of safety during operation.
4. Children at that age suffer much less emotionally during the postoperative
period than do older children and, as a consequence, parents’ anxiety is also
alleviated
5. During that period children are still in diapers and have not been exposed to
other people’s observation.
6. more important, in case of complications that require reintervention further
correction can be carried out sometime before the second year. At about this
time the genital awareness begins and the child becomes more prone to
psychological problems.
Penis grows more in proportion to baby for 1st six months, if remains small at 6
months, testosterone enanthate 25-50 mg intramuscularly once a month for 3
months has been shown to increase penis size.
OPERATIVE PRINCIPLES
1. Orthoplasty
Complete correction of chordee mandatory
i. Some advocate total resection of fibrotic corpus spongiosum
ii. Others raise the chordee as a flap to create the neourethra and in doing so
corrects the chordee
iii. Dissection along the septum between the corpus cavernosa may be
required
iv. Nesbit type dorsal plication of tunica albuginea
Artificial erection test to confirm complete correction
i. Tourniquet around base of penis, inject saline into both corpora
cavernosa
ii. Local injection using prostaglandin E1 said to give a more physiologic
response (ie tendency to overcorrect with saline)
2. Urethroplasty
Depends on the level of the meatus following chordee release
i. True Glanular hypospadia (no chordee)
o Magpi technique
o Dividing septum between glanular pit and meatus
ii. Distal penile with no chordee
o Flip Flap
iii. Distal penile with chordee
o Mustarde
iv. Mid/Proximal/Penoscrotal
o Vascularised preputial flap based on dorsal artery of prepuce (tubed or
onlay) – vertical, transverse, bileaflet island or penopreputial rotation
flap)
o Full thickness graft (Horton-Devine)
Preputial skin
Bladder mucosa – prone to complications
Buccal mucosa – prone to stenosis at meatus
Postauricular skin - least hairless skin
v. Perineal hypospadia
o 2 staged procedure
Midline scrotal skin for proximal urethra
Ventral tube or FTG urethroplasty
3. Meatoplasty
Avoid tension
neomeatus should be oval and not round.
Horton V flap to reduce tendency to circumferential scar stricture
4. Glansplasty
Important for aesthetics
Tip is usually rotated ventrally (tip tilt)
Undermine the
ventral half of the glans to correct tip tilt and also this
mobilises the glans to allow creation of urethra within the glans
Excessive undermining will lead to the soft glans syndrome (unerected glans
despite penile shaft erection)
5. Ventral skin coverage
Byers flaps of preputial skin
Preputial rotation flap is penile torque needs to be corrected
SURGICAL METHODS
CHORDEE
The creation of an artificial erection should be done at the beginning of all
operations for hypospadias so as to document the degree of chordee.
This is done by the application of a tourniquet to the base of the penis followed by
the injection of saline into both corpora cavernosa via a small needle.
Often it is found that in a penis thought to be free of chordee when flaccid, the
artificial production of an erection demonstrates that chordee is in fact present.
Chordee can occur without hypospadias, ie even when the urethral meatus is in the
normal position.
Classification (Devine and Horton):
TYPE I
The urethra lies subcutaneously not surrounded by the normal layers of corpus
spongiosum, Buck’s fascia or dartos fascia. This may be associated with a mild
degree of hypospadias (uncommon).
TYPE II
The urethra is enclosed by the corpus spongiosum and the chordee is due to the
fibrous tissue that lies deep and lateral to the urethra.
TYPE III
The urethra is enclosed normally by the corpus spongiosum and Buck’s fascia and the
chordee is due to abnormal inelastic dartos fascia.
TYPE IV
Intrinsic fibrous abnormality on the ventral aspect of the corpora cavernosa -very
uncommon.
TYPE V
Congenital short urethra - very uncommon.
Surgical treatment of chordee without hypospadias
1. Excision of dysgenetic fibrous tissue.
2. Longitudinal incision in the tunica albuginea ventrally.
3. Transverse ventral incision and insertion of a dermal graft.
4. Excision of ellipse(s) of tunica albuginea from dorsally and placation sutures
Surgical Methods
Glanular Hypospadia: MAGPI
dorsal Meatal Advancement and Glansplasty (MAGPI) procedure indicated for
glanular hypospadia.
Skin flaps used to reinforce the inferior distal surface.
It cannot produce an adequate repair in subglandular cases.
Method
o After demonstrating that the penis is straight with an artificial erection, a
circumcising incision is made.
o Skin hooks are placed into the lateral edges of the glandular urethral groove
and retracted laterally.
o This move raises a transverse band of mucosa that is then incised
longitudinally in the midline.
o This incision in the dorsal glandular wall of the urethra is then closed
transversely with 6-0 chromic catgut. A skin hook is placed in the skin at the
margin of the corona in the ventral midline. With distal traction, the edges of
the glans are pulled forward and approximated in the midline with
subcuticular interrupted 5-0 PDS sutures.
o The glans epithelium is closed with interrupted 6-0 chromic catgut. Redundant
dorsal prepucial skin can be tailored for skin closure and reapproximated with
interrupted 5-0 catgut.
o Urinary diversion is not required. This procedure is routinely done in an
outpatient setting.
Horton Flip-Flap: Coronal/Distal hypospadias without Chordee
For distal cases ending at the coronal sulcus, extensive mobilization of the urethra
with advancement to the tip of the glans is recommended.
For hypospadias cases in which the urethra is subglandular, a “flip-flap” operation
is utilized.
If the meatus is adequate and there is no chordee, two parallel incisions outlining
the urethral plate continue from the meatus to the neomeatus so that the flip flap
can be sutured to this glans strip, thereby constructing the distal urethra.
Coronal/Distal hypospadias with Chordee
When chordee is present, transection of the urethral plate and excision of the
underlying dysgenetic tissue are suggested.
In such cases, a V-shaped midline glans flap is elevated. Lateral glans wings are
closed over the new urethra, and prepucial skin is shifted from the dorsal surface to
the ventral surface, covering the penile shaft. If the meatus is small, a meatotomy is
performed and the midline V-shaped glans flap advanced into the meatus.
After tissue causing chordee is resected, the flip flap is sutured to the midline glans
flap to construct the urethra. The lateral glandular wings are used to cover the
distal urethra. The prepuce is split and shifted ventrally for resurfacing. These
techniques are sufficient for about 90% of all hypospadias cases. In more proximal
cases, in which the midline glans flap does not reach the native urethra without
causing curvature, a new interposed urethra must be constructed to bridge the gap
and meet the glans flap.
TIP (Tubularised Incised Plate) – Snodgrass BJU International 2005
Essentially all patients with midshaft and more distal hypospadias can undergo TIP
of the urethral plate
repair consists essentially of a Duplay- type tubularized repair with the added
feature of a full-thickness midline incision extending the full length of the urethral
plate.
This key point in the operation widens the plate and allows it to be tubularized with
no additional skin flaps
Concerns are with regards as to whether this leads to meatal stenosis.
Experimental studies in animal models show rapid epithelialization of the defect
created by a urethral incision but it remains unclear whether experimental findings
in a normal, well-vascularized and spongiosum-supported urethra can be reliably
extrapolated to the thin atrophic urethral plate tissue commonly encountered in
hypospadias.
Step 1. A 5–0 polypropylene suture is place into the
glans for traction and to later secure the urethral stent.
The initial skin incision depends upon whether the
family prefers circumcision or foreskin reconstruction,
as either can be performed. When circumcision is the
desired result care is taken to preserve sufficient inner
prepuce so that a so-called 'mucosal collar' can be
approximated in the ventral midline after glansplasty.
Then the penis is degloved to near the penoscrotal
junction. If the foreskin is to be reconstructed the skin
incision extends from the corners of the dorsal preputial
hood to 2 mm proximal to the meatus. Ventral shaft
skin is released until normal dartos tissues are
encountered.
An artificial erection confirms the absence of ventral
curvature, but if there is significant bending a midline
dorsal plication is done using a single 6–0
polydioxanone suture placed in the tunica albuginea of
the corpora cavernosa directly opposite the point of
maximum curvature.
Step 2. Next, longitudinal incisions are made along the visible junction of the glans
wings to the urethral plate. Proposed lines for incision are first infiltrated with
1 : 100 000 noradrenaline or a tourniquet is used around the base of the penis for
haemostasis. After making the skin incision with the 69 Beaver scalpel, I prefer to
complete the dissection and glans wings mobilization using tenotomy scissors, taking
care both to preserve vascularity to the urethral plate and sufficient thickness for the
wings to be securely approximated.
Step 3a: The key step in the procedure is midline incision of the urethral plate. This
manoeuvre is facilitated by counter-traction maintained by the surgeon and assistant
along opposite margins of the plate. Using tenotomy scissors, the relaxing incision is
made from within the meatus to the tip of the urethral plate. It should not be carried
further distally into the glans. The depth of incision depends upon whether the plate
is grooved or relatively flat, but in all cases extends down to near the corpora
cavernosa.
Figure 3c: A 6 F Silastic stent is passed into the bladder and secured to the glans
traction suture. Then the urethral plate is tubularized beginning at the neomeatus,
using 7–0 polyglactin suture. The first suture is placed through the epithelium at a
point just distal to the midglans so that the meatus has an oval, not rounded,
configuration. Tubularization is completed with a running two-layer subepithelial
closure, turning all epithelium into the neourethral lumen.
Step 3b: I recommend initially maintaining the urethral plate in all proximal
hypospadias repairs, as even apparently severe ventral curvature sometimes can be
straightened without transecting the plate. The skin incision should be made
immediately next to the plate to minimize the risk of incorporating hair follicles into
the neourethra.
Similarly, the foreskin also can be preserved at the beginning of surgery as curvature
is assessed, although in many patients it will be necessary to completely deglove the
penis and ultimately circumcise it. My experience with foreskin reconstruction in
boys with proximal defects is limited, and a desire to avoid circumcision should not
outweigh the need to correct significant ventral curvature that might later impair
sexual function.
After degloving, the corpus spongiosum alongside the urethral plate is dissected off
the underlying corpora cavernosa. This tissue later will be approximated over the
neourethra as a barrier layer against fistula, and its mobilization sometimes also
lessens the extent of ventral penile bending. Then an artificial erection is created;
persistent mild curvature is corrected by midline dorsal plication, as described above.
More severe bending next leads to dissection under the entire urethral plate, and if it
still persists, to transection of the plate and, in my hands, a staged urethroplasty.
Step 4: dartos pedicle flap is dissected from the preputial hood and dorsal shaft skin
in patients undergoing circumcision, then button-holed and transposed ventrally to
cover the entire neourethra.
Glansplasty is a key determinant of the final cosmetic outcome. Over the years my
technique has developed, and currently begins with a 7–0 polyglactin suture through
the epithelium at the desired point for the ventral lip of the meatus. A second 7–0
suture is placed subepithelially in this same location to further buttress the neomeatus
and hopefully prevent partial dehiscence that would result in a larger than normal
meatus. No attempt is made to secure the glans to the underlying neourethra. The
remainder of glans approximation is then done using interrupted 6–0 polyglactin
subepithelial sutures proximally to the corona. It is not necessary to place sutures
through the epithelium of the glans, and I have seen a few patients develop suture
tracks when a second layer was created.
Dripping stent is left in place inside the nappy – usually removed after 1 week.
most common complication from TIP urethroplasty is fistulae.
prevented by
1. turning all epithelium into the neourethra
o 2 layered subepithelial suture closure
2. using sufficient barrier layers
o recommend using corpora spongiosum as an additional layer for
proximal hypospadias and a dartos flap harvested from the dorsum.
3. avoiding meatal stenosis
o most important factor is not to tubularise the urethra too far distally
o neomeatus should be oval, not round
o Other key manoeuvres include incising the plate deeply to near the
corpora cavernosa, so the neourethra will have an adequate diameter,
and resisting the temptation to extend the relaxing incision into the
glans, as this will also lead to tubularizing the plate too far distally.
Proximal hypospadias
Duckett preputial island flap (tubed)
In certain cases, an arterialized flap for urethroplasty works with great success
The procedure described here is used for proximal hypospadias when the prepuce
is large and the rotation of an island flap of prepuce does not cause torsion.
Initially, chordee is corrected, and penile straightness is confirmed on artificial
erection. Attention is then turned to the redundant dorsal prepucial skin in order to
develop a flap for the neourethra. The prepuce is freed from the penile shaft, and
the length and breadth of the tube for the neourethra are marked on the inner
surface of the prepuce. Careful dissection is then performed to develop a vascular
pedicle for this island flap. The vascular pedicle is dissected free from the dorsal
penile skin until the flap can be easily rotated to the underside of the penis. The
neourethra can then be tubed around an appropriately sized stent with a
subcuticular PDS suture. A tunnel can be created in the glans for the distal
neourethra, or the glans can be split. The proximal elliptical anastomosis is
completed first. The chances of meatal stenosis can be minimized by excising a
core of glans tissue from the tunnel or by use of a V-flap in the meatus. When the
urethroplasty has been completed, residual dorsal penile skin is brought ventrally
for skin coverage. A stent is left in the urethra for 5 days, and urine is drained via
a percutaneous suprapubic catheter until the voiding trial 10 days later.
Bracka’s 2 stage repair(BJPS 1995)
Stage 1: release of chordee, clefting of glans and lining with FTSG from prepuce
Stage 2 (6 months apart) : closure of neourethra and waterproofing flap using
subcutaneous aspect of preputial hood.
Perineal, Scrotal, and Proximal Shaft Hypospadias
Tube Graft Hypospadias Repair (Horton-Devine Technique)
Both techniques give approximately the same success rate. Flap dissection may cause
devascularization of the dorsal penile skin or result in tortuosity of the urethra and
thus cause flap disturbance. For more proximal cases, the flap may not have enough
length. The proximal flap is more difficult to construct and requires more operating
time; it may also be more prone to form diverticula.
The full-thickness graft urethroplasty allows greater freedom in resurfacing the penile
shaft. Hairless groin skin, buccal mucosa, and bladder mucosa are other potential graft
donor sites available to form the neourethra.
Hypospadias Cripples
There are many patients who have had prior unsuccessful hypospadias repairs.
Typically, they have insufficient penile skin remaining so that preputial grafts or
flaps are not an option.
Management:
1. free tubed graft techniques, with the graft material provided by using extragenital skin, bladder mucosa, or buccal mucosa.
2. Cover with local flap or scrotum
3. Prelaminated free radial forearm flap
1st stage – insert tubed SSG into forearm tunnel
2nd stage – raise free flap and inset
Buccal mucosa is reported to have certain advantages in that it is hairless, leaves
no donor site defect, and may have enhanced graft take because of the thin lamina
propria dense capillary network.
COMPLICATIONS OF HYPOSPADIA REPAIR
Attempt to reduce with a careful preoperative evaluation, precise surgical
technique, meticulous and careful handling of tissues and appropriate postoperatice
care
2 groups : early and late
Difficulty in assessing effectiveness of hypospadia operations is that techniques
continue to evolve but complications occur late (ie when the children undergo
puberty)
EARLY
i. Bladder spasm – reflex urinary retention (morphine, oral anticholinergics, hot
baths, repositioning the catheter)
ii. Infection (antibiotics before and after the operation)
iii. Wound dehiscence (treat conservatively and repair later, can use taping methods
to hold the wound edges in close approximation)
iv. Necrosis
v. Haematoma (evacuated if feopardizes the graft or skin flaps otherwise manage
conservatively if small)
LATE
i. Fistula (10-20%)
a. Higher with proximal hypospadia
b. prevented by turning epithelium into the neourethra, using sufficient barrier
layers, and avoiding meatal stenosis
c. Snodgrass reduces this risk by mobilising corpus spongiosum and closing over
the neourethra, then adding a dorsal dartos pedicle flap on top of this.
d. Treatment
i. Early – wait until wounds heal then repair
ii. Chronic (<2mm) – treat stricture, excise fistula, wide undermining and
defect closure. Avoind overlapping suture lines
iii. Large (>2mm) – turnover flaps, reinforce with local flaps
iv. Unable to close – treat strictures, tube graft repair, local flaps or bury
in scrotum
ii. Diverticulum
a. Neourethra too patulous
iii. Strictures
a. Avoid circumferential scars
b. Possible benefit from dilation
c. Repair by open and patch flap/graft
iv. Meatal stenosis - up to 40% with severe hypospadias can have some degree of
voiding problems
v. Hair growth in the urethra – stones
vi. Tortuosity of the new urethra causing an irregular urine flow
vii. Retrusive meatus
viii. Chordee (ventral bend) – poor correction
ix. Soft glans syndrome
x. Sexual problems affecting erection, ejaculation and sexual sensation have now
been reported in more than 20% of men