Quiz 3
advertisement

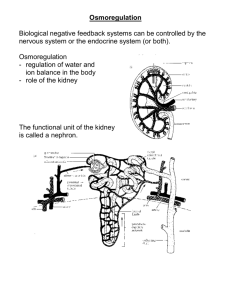
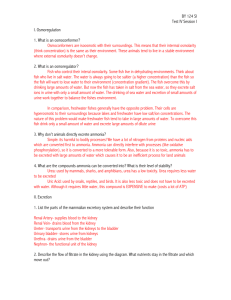
Posterior Pitutary Quiz # 3 Material Antidiuretic Hormone Vassopressin ADH is critical to maintaining the volume and osmolality of the extracellular fluid, by controlling the final volume and osmolality of the urine Uterotonic activity Vasoconstrictive activity Antidiuretlc activity Changes in the plasma volume or osmolality from the ideal constant of 285 mOsm, controls the release of ADH. Stimulation of osmoreceptors (Osmo-sodium receptors) in the hypothalamous and pressure (baroreceptors) in the venous and arterial beds and heart result in the release of ADH OSMORECEPTORS The osmoreceptors respond to changes in extracellular sodium concentrations. When the osmolarity becomes low, osmosis of water into the osmoreceptors causes them to swell, thus decreasing the rate of impulse discharge. Conversely, increased osmolarity in the extracellular fluid pulls water out of the osmoreceptors, causing them to shrink and therby increasing the rate of impluse discharge. The release of ADH, following osmoreceptor impulse stimulation increases the permeability of the collecting ducts of the kidney and thus an increased conservation of water. This results in a loss of sodium(excretion) causing a dilution of the extracellular sodium and a drop in the osmolarity. Conversely, when the extracellular fluid becomes too dilute (hypo-osmotic), less ADH is formed and excess water is lossed, with sodium being conserved and the osmolarity increases. The Ultimate Effects of ADH 1. To conserve water 2. To control sodium concentrations 3. To eliminate water Diabetes Insipidus Diabetes Insipidus is a polyuric syndrome that results from a lack of ADH (pituitary) OR from a lack of ADH effect (nephrogenic), sufficient to effect appropriate concentration of urine for the conservation of water. Pituitary Diabetes Insipidus Trauma to the pituitary A pituitary tumor (primary or metastatic) Infiltrations/inflammations of the pituitary Idiopathic in 30 to 40% of case there is no identifiable causes. Most commonly Pituitary diabetes inspidus is the result of atrophy or destruction of the hypothalamic center responsible for the production of ADH A second mechanism responsible is a selective failure of the osmoreceptors to stimulate ADH release. This form is often classed as “essential hypernatremia”, as high sodium concentrations do not stimulate ADH release. Nephrogenic Diabetes Insipidus Nephrogenic Diabetes Insipidus should be used to describe the state in which renal tubular unresponsiveness to ADH is responsible for the polyuria and hyposthenuria. May be either familial of acquired: Familial occurs prirmarily inmalesand exogenous ADH produces no effect. The defect is believed to be in the ADH receptor- adenylate cyclase system . Acquired is most often secondary to drug therapy: antibiotics methoxyflurane Li (15 to 3O%) systemic disease ( sarcoidosis, etc.) Clinical Manifestations Of Diabetes Insipidus Polyuria is the foremost feature ( 3 to 15 L of urine per day) Thirst may be near continuous, often with a preference for cold water Nocturia is almost always present The onset of pituitary diabetes insipidus is most often abrupt, with a peak urine flow reached in 1- 2 days. Thus polyuria developing over weeks to months suggests a disorder other than diabetes insipidus. Aside from the inconvenience of poluria and polydipisia, patients with diabetes insipidus usually suffer no ill efects UNLESS they are deprived of water When water is withheld, circulatory collapse or hypertonic encephalopathy can occur within hours. Hypertonic Encephalopathy May be caused by NaCl or glucose concentrations which produce a serum osmolality > 350 mOsm/L. These solutes cross cell membranes poorly and as a result, water is pulled out of the CNS cell in the presence of high extracellular solute concentrations, producing cell shrinkage and CNS dysfunction. This can range from lethargy to coma. In children with hypernatremia (>160 mEqIL for 24hrs), the mortality rate is greater than 40%, with about 66% of the survivors having some degree of permanent neurological damage. Laboratory Findings of Diabetes Insipidus Urine specific gravity of 1.005 or less Urine osmolarity of less than 200 mOsm/L Serum osmolarity usually normal (285 to 290 mOsmIL) Serum sodium may be Increased (> 148 to 152 mEq/ml) The Polyuric Syndromes Diagnosis Pituitary diabetes insipidus Absence or diminished production of ADH History of head trauma, tumor Sudden onset of polyuria Nocturia Random plasma osmolarity >290 mOsmIL Nephrogenic diabetes insipidus Renal unresponsiveness to ADH Present since birth Slower onset of poluria Family history of diabetes insipidus History of exposure to ADH antagonists Diabetes mellitus Poluria,Polydipisia,Polyphagia Hyperglycemia, Glycosuria Primary Polydipisia The ingestion of unusually large volumes of water Polyuria is an appropriate physiological response Nocturia usually absent Random plasma osmolarity usually normal Diagnosis of Pituitary Insipidus The basis of all tests for pituitary diabetes insipidus is the ability of the kidney to excrete a hypertonic urine after an osmotic stimulus. Water deprivation studies depend on endogenous ADH release in response to dehydration. However, these tests have the potential for serious harm to the patient and are most often done in a hospital . Diagnosis of Pituitary Diabetes Insipidus Exogenous ADH Normal subjects: Urine osmolarity 2-4x > serum osmolarity 9% increase in urine osmolarity) post-ADH Complete pituitary diabetes insipidus: Urine osmolarity < serum osmolarity 50% increase in urine osmolarity) post-ADH Partial Pituitary diabetes insipidus: Urine osmolarity = or > serum osmolarity about a 10 to 15% increase in urine osmlarity) post-ADH Direct ADH assay of the serum is probably the best in terms of simplicity and reproducibility (NEJM 305:1539-1546, 1981)