N222 Lecture 6
advertisement
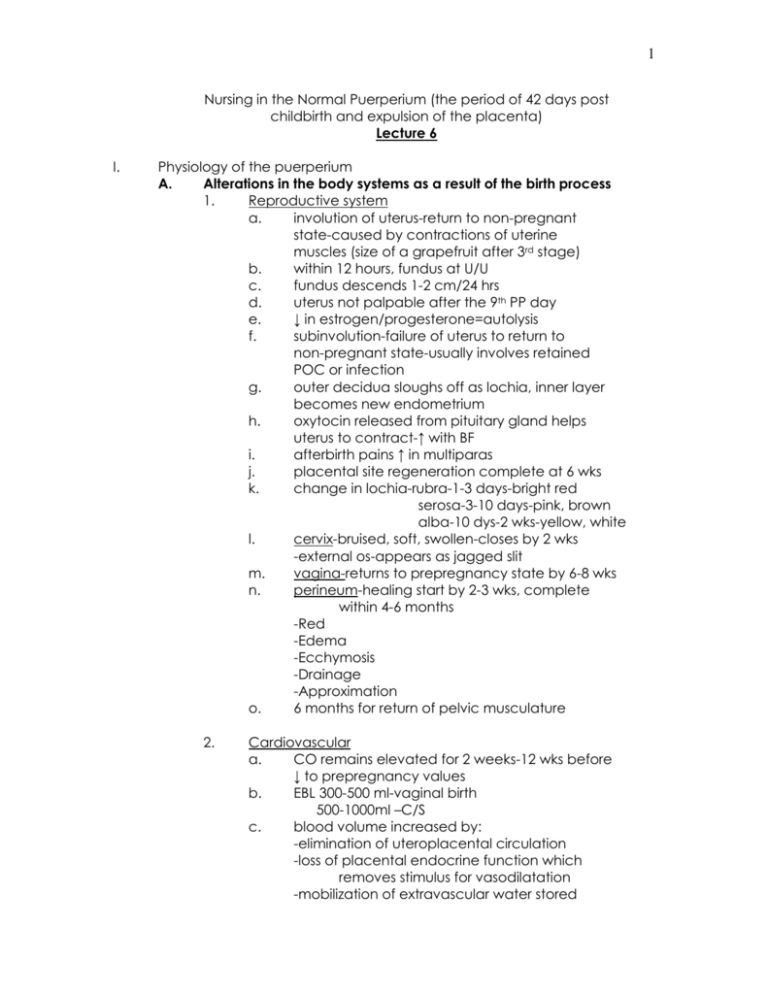
1 Nursing in the Normal Puerperium (the period of 42 days post childbirth and expulsion of the placenta) Lecture 6 I. Physiology of the puerperium A. Alterations in the body systems as a result of the birth process 1. Reproductive system a. involution of uterus-return to non-pregnant state-caused by contractions of uterine muscles (size of a grapefruit after 3rd stage) b. within 12 hours, fundus at U/U c. fundus descends 1-2 cm/24 hrs d. uterus not palpable after the 9th PP day e. ↓ in estrogen/progesterone=autolysis f. subinvolution-failure of uterus to return to non-pregnant state-usually involves retained POC or infection g. outer decidua sloughs off as lochia, inner layer becomes new endometrium h. oxytocin released from pituitary gland helps uterus to contract-↑ with BF i. afterbirth pains ↑ in multiparas j. placental site regeneration complete at 6 wks k. change in lochia-rubra-1-3 days-bright red serosa-3-10 days-pink, brown alba-10 dys-2 wks-yellow, white l. cervix-bruised, soft, swollen-closes by 2 wks -external os-appears as jagged slit m. vagina-returns to prepregnancy state by 6-8 wks n. perineum-healing start by 2-3 wks, complete within 4-6 months -Red -Edema -Ecchymosis -Drainage -Approximation o. 6 months for return of pelvic musculature 2. Cardiovascular a. CO remains elevated for 2 weeks-12 wks before ↓ to prepregnancy values b. EBL 300-500 ml-vaginal birth 500-1000ml –C/S c. blood volume increased by: -elimination of uteroplacental circulation -loss of placental endocrine function which removes stimulus for vasodilatation -mobilization of extravascular water stored 2 d. e. f. g. Vital signs: -Temp-↑ to 380 C/1004 F R/T dehydration -Pulse-↑ 1st hr-return to pre-preg. 8-10 wks -Resp-↓ by 8-10 wks -BP-may have orthostatic hypotension Hgb/Hct: -1st 72 hrs-↑ loss of plasma volume compared to RBC’s -↑ in H & H by day 7 WBC’s may ↑ to 25-30,000/mm3 Coag factors-hypercoagulable state may lead to possible thromboembolism 3. Gastrointestinal a. ↑ appetite b. no BM for 2-4 days post delivery -encourage ambulation -hydration -fiber -medications, i.e.: stool softeners c. tx hemorrhoids-ice packs, tucks, crm -no pr meds if 3rd-4th degree laceration d. Kegel exercises to strengthen pelvic floor 4. Renal a. returns to normal function 1 month after birth -bladder tone returned by 5-7 days b. diuresis-from fluid retention, pitocin, etc c. excessive vaginal bleeding may be noted if bladder is allowed to get distended with urine 5. Musculoskeletal a. joints stabilize 6-8 weeks post birth b. may have permanent increase in shoe size c. may have separation of symphysis pubis or rectus abdominis 6. Integumentary a. chloasma (mask of pregnancy) usually fades by end of pregnancy b. hyperpigmentation of areolae and linea nigra may continue c. may note perfuse diaphoresis post delivery 7. Endocrine a. Expulsion of placenta=↓ in estrogen, cortisol progesterone, and hPL (hCS) [human placental lactogen/human chorionic 3 b. 8. somatomammotropin] -reverse diabetogenic effect-lower BS level if BF-↑ prolactin levels for 6 weeks if bottle-fed-↓ -usually means later ovulation in lactating women Psychosocial a. parent’s acceptance of infant’s needs and abilities b. need to learn cues, understand emotional states c. bonding-proximity, touch, voice, interaction d. identify infant as an individual yet part of the whole family e. mutuality-infant’s behaviors stimulate mom’s f. may feel attracted to alert, responsive infant and repelled by irritable, disinterested infant g. attachment occurs more readily with the infant whose temperament, social capabilities, appearance, and sex fit parent’s expectations h. need to assess mother-infant communication i. behaviors -entrainment-moving in time with adult speech -biorhythmicity-soothed by mom’s heartbeat -reciprocity-responds to cues -synchrony-mutually rewarding -engrossment-interest in baby by father j. maternal adjustments -taking in-first 24 hrs-focus on self and basic need Dependent, passive -taking hold-last 10 days to several weeks-focus on care of baby and competent mothering-dependent -letting go-focus on forward movement of the family unit k. PP blues- 70% of women-mood swings, anger, depression, letdown, fatigue, insomnia, H/A’s, weepiness (resolves in 10-14 days) l. PP depression-7-30%-more severe syndrome -depression, feeling of failure overwhelming guilt, loneliness 4 II. Nursing Process A. Data collection/Assessment 1. Vital signs 2. Fundus a. ck fundal location, tone, lochia b. have pt empty bladder before exam 3. Bladder a. assess for distention b. measure first voids until 500 ml (voided out) c. catheterize if needed 4. Perineum a. if repair done, assess site for intactness, edema, hematomas, redness, or drainage (REEDA) b. assess for presence of hemorrhoids 5. Breasts a. note if breast are filling-palpate b. note any redness, soreness, cracking of nipples B. Nursing Diagnoses 1. Risk for fluid volume deficit 2. Alteration in urinary elimination 3. Pain 4. Fatigue 5. Ineffective breast feeding 6. Situational low self-esteem 7. Anxiety due to lack of knowledge base 8. etc. C. Interventions 1. Safety a. infant ID bands b. orientation to unit c. staff picture ID’s d. move infant in crib 2. Standard precautions a. wash hands before handling baby b. change linens c. proper hygiene d. use of squeeze bottle for peri care e. wiping front to back f. teach pt about fundal massage g. use of peppermint or running water to aid in 5 h. i. j. k. l. m. n. o. p. q. III. IV. voiding to prevent urinary retention use of ice packs for the first 12 hours post repair of peri then instruct on use of sitz bath squeeze buttocks together when sitting or rising from a chair to help keep repair intact wear good supportive bra use lanolin crm to prevent cracking of nipples warm packs before breast feeding, cool packs post walk as soon as possible-helps with gas pains take pain meds prn encourage rubella vaccine if non-immune pt should prevent getting pregnant for at least 4 weeks post vaccination Tdap-Pertussisrhogam given to Rh – moms who had Rh+ babies Early Discharge A. Candidates and criteria 1. Newborns’ and Mothers’ Health Protection Act of 1996 a. 48 hours minimum post vaginal delivery b. 96 hours minimum post C/S c. pt and doctor may agree on earlier D/C 2. Maternal criteria for early D/C a. VSS b. voiding c. Hgb >10 d. no bleeding e. instructions on self-care 3. Infant criteria for early D/C a. term infant b. VSS c. normal physical assessment d. at least 2 successful feedings e. at least 1 void and 1 defecation f. no jaundice g. circ site ok h. newborn blood/hearing screenings done i. follow-up in 1 week j. maternal/infant teaching cklist completed Care of the Cesarean Birth Patient A. Assessment/Interventions 1. VS every 15 min X 1hour, 30 min X 1 hour, then per hospital protocol 2. monitor I & O’s-need UO at least 30 ml/hr 6 3. 4. 5. 6. 7. 8. V. assess abdominal dressing for drainage assess need for pain medication assess fundal location, tone, and lochia (still have 3 distinct lochia stages) ambulate asap assess for passage of gas-advance diet as tolerated C & DB-may use inspirometer B. Nursing diagnoses 1. Fluid volume deficit 2. Pain 3. Risk for infection 4. Risk for injury 5. Anxiety R/T surgery, fetal well-being 6. Situational low self-esteem C. Possible post-op complications 1. CV-hemorrhage, shock, dvt 2. Pulm-embolus, pnemothorax 3. GI-paralytic ileus 4. GU-renal failure, hematuria, UTI, oliguria 5. Reprod-endometritis, emboli 6. Skin-wound infection, dehiscence Care of the Lactating Woman A. Physiology of Lactation 1. Female breast has 15-20 lobes containing alveoli (the milk producing cells) 2. alveoli→ductules→lactiferous ducts→nipple 3. ↓ estrogen & progesterone post delivery=↑ prolactin levels which remain above baseline thru duration of lactation (highest level is at day 10) 4. Prolactin: -highest level at day 10 -is produced in response to infant’s sucking -promotes milk production by stimulating alveolar cells B. Other hormone changes/reflexes 1. Oxytocin responsible for let-down reflex nipple stimulation→pituitary produces oxytocin→ makes cells around the alveoli contract→sends milk to nipple 2. Nipple erection reflex infant cries or rubs against the breast→nipple becomes erect→propulsion of milk 7 VI. C. Supply/demand 1. First milk called colostrum a. rich in immunoglobins b. higher concentration of protein and minerals to mature milk but less fat c. promotes growth of Lactobacillus bifides in GI 2. If infant is well nourished, will see 6-8 wet diapers and 3 stools in 24 hours at day 5 of breastfeeding 3. Incomplete emptying can lead to ↓ milk supply 4. watch for infant growth spurts -10 days -3 weeks -6 weeks -3 months -4.5-6 months D. Maternal nutrition/considerations 1. add addition 200-500 calories/dy while breastfeeding 2. drink 2-3 liters of fluid daily 3. continue on PN Vitamins and iron as directed 4. watch for engorgement/plugged milk ducts/ sore nipple/monilial (yeast) infections/mastitis Care of the Woman/Neonate Formula-fed A. Formula types 1. commercial formulas primarily cow-milk based but soy and other specialty formulas available 2. may be in powdered, concentrated, or ready to eat B. Common problems 1. positioning-need to make sure milk covers nipple area 2. warming-never microwave bottle 3. propping-don’t leave infant unattended while feeding C. Nutritional requirements 1. first day-only give 7.5-15 ml formula at one time -their eyes are bigger than their stomachs 2. usually feed every 2-4 hours 3. some infants swallow air as they feed-burp them! 4. by 1 week of age, babies will be drinking 700-900 ml in 24 hours *bottle fed because-returning to work, +HIV, mastectomies, adopted infant, maternal medications 8 VII. Contraception Education A. Considerations for Choosing a Method 1. resumption of sexual activities should wait 2-3 weeks to decrease risk from infection 2. best to use condoms/foam at this time 3. when discussing contraception with your doctor, -action -safety -effectiveness -convenience -availability -expense -personal preference B. Methods (failure rates listed within 1st year of use) 1. Coitus interruptus (withdrawal) -action-prevents fertilization -safety-no protection from STI’s -convenience/availability-good -expense-N/A 2. Fertility awareness methods -periodic abstinence-no sex 4 days before and 4 days after ovulation -rhythm-based on 3-4 cycles-use shortest and longest -BBT-sl. ↓ temp before ovulation (0.050C) then ↑ 0.3-0.60C -cervical mucus-ck for changes-amt. and consistency -symptothermal-combo of BBT and cervical mucus -ovulation kits-detect surge in LH that occurs approx. 12-24 hours before ovulation 3. Barrier methods a. spermicides -action-physical/chemical barrier to sperm -safety-may provide some protection from STI’s -convenience-needs to placed before act -availability-good if thought of in advance -expense-cheap b. condoms -action-physical barrier to sperm -safety-protect against STI’s/HIV if used properly -effectiveness-can ↓ failure rate with use of spermicides -vaginal sheath/condom c. diaphragm -action-mechanical barrier to sperm -safety-see condoms, small amt of cases with 9 TSS-toxic shock syndrome -effectiveness-needs to be fitted to woman’s anatomy, needs to be used with spermicide -convenience-may be placed 6 hours before intercourse but must be left in for 6 hours post act, additional spermicide each time -availability-MD appt -expense-affordable d. 4. cervical cap/sponges -cervical cap needs fitting -must ck position of cap before intercourse -failure rate in parous women-40% -sponge-moisten with water before insertion -have spermicide -risk of TSS if not removed after 24 hours Hormones a. over 30 different formulations b. may have estrogen/progestin or only prog. c. may be oral, subdermal implantation, IM, vaginal d. prevent pregnancy by stopping ovulation or prevention of implantation e. do not protect against STI’s f. not recommended for some women -h/o thromboembolic -smoker -h/o estrogen dependent tumors -h/o CAD -h/o impaired liver -over the age of 35 -HTN g. mini pill (progestin-only) -problems with irregular menses h. injectable progestin-Depo Provera -injected q 11-13 weeks-may need appt. -↑ risk of venous thrombosis i. implanted progestin-Nexplanon -good for 3 years -implanted in arm -no STI protection j. Emergency contraception Plan B One Step-OTC any age -levonorgestrel -needs to used within 72 hours -prevents ovulation/implantation -90% effective 10 -(Plan B-two pills-being D/C’d) Ella-non-hormonal -needs to used within 120 hours -needs Rx -90% effective IUD insertion -98% effective if inserted within 5 days 5. Intrauterine Devices a. usually T-shaped b. loaded with either copper or levonorgestrel c. may be used for 5 yr (hormone)-10 yrs (copper) d. prevents fertilization e. Mirena (hormone IUD)-helps to diminish menses f. Copper “T”-good choice for women over 35, smokers, h/o CAD, HTN g. not recommended for women with: -h/o PID -suspected pregnancy -h/o distorted uterine cavity -h/o multiple partners 6. Sterilization a. females - bilateral tubal ligation -surgical procedure -expense usually higher than vasectomy -electrocoagulation, ligation, banded, crushed, or plugged -no protection against STI’s -should be considered permanent -informed consent needed at least 72 hours before procedure -eSSURE -done in clinic or OR -uses water to visualize fallopian tube meatus -coil placed and tissue collects on coil creating a blockage -HSG performed at 3 months to establish closure -back-up BC method used during this period b. males-vasectomies -done in clinics under local anesthetic -vas deferens are ligated/cauterized -takes multiple ejaculations to clear remaining sperm from vas deferens 11 BIRTH CONTROL COMPARISONS FAILURE RATES MECHANISM OF ACTION STD USER method of birth control perfect actual prevents prevents postpone protection continuation use fertilization implantation sex use rates No Method 85 85 Spermicides 18 29 ++++ + 42 Male Condoms 2 15 ++++ ++ 53 Female Condoms 5 21 ++++ ++ 49 Diaphragm 6 16 ++++ + 57 Cervical FemCap 4 w/o prior pregnancy 14 ++++ + 57 Sponge 9 w/o prior pregnancy 16 ++++ + 57 Sponge 20 w/ prior pregnancy 32 ++++ + 46 Ovulation Method 3 22 +++ + 51 Sympto-Thermal 2.5 16 +++ + 51 Standard Days Method 5 12 +++ + Calendar Method 5 13-20 +++ + Lactation (LAM) 0.5 6 ++++ Withdrawal 4 27 ++++ Oral Contraceptives 0.3 8 +++ + 68 Ortho Evra Patch 0.3 8 +++ + 68 Nuva Ring 0.3 8 +++ + 68 Shot (DepoProvera) 0.3 3 +++ + 56 Shot (Lunelle) 0.05 3 +++ + 59 IUD (ParaGard Copper) 0.8 0.6 ++ ++ 80 IUD (Mirena) 0.1 0.1 ++ ++ 80 Abstinence 0 0 ++++ 51 + ++++ 43 ++++ For added protection against pregnancy, you can use more than one method of contraception at a time. For example, many clinicians recommend that when using condoms, spermicides be used as well. If a woman is allergic to spermicides she can use a natural method and a condom and for extra protection. Any of these combinations will reduce the predicted failure rate 01/16