CUTANEOUS FUNGI:
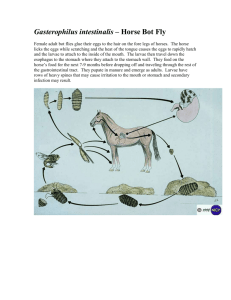
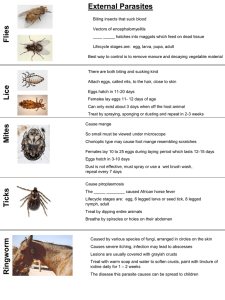
advertisement

FUNGI: cell wall: chitin cell membrane: sterols (ie. ergosterol) favored by heat and humidity YEASTS MOLDS single cells (oval or round) long filaments or hyphae (septate or nonseptate) asexual budding asexual spores (conidia) pseudohyphae (clusters of buds) mycelia (segments of hyphae) humans environment (ie. soil) grows on 37C (blood agar, humans) grows on 25 (Sabouraud’s agar) CUTANEOUS FUNGI: ORGANISM Superficial fungal infections (dead skin): PATHOGENESIS / CLINICAL FEATURES cause pigment changes on surface of skin lesions contain budding yeast cells and hyphae Pityriasis (Tinea) versicolor (multi-colored) Malassezia furfur Tinea nigra (black-colored) Cladosporium (Exophiala) werneckii hypopigmented patches on the skin, especially on tanned skin in the summer ( with hot, humid weather); scaling, itching dark brown to black painless patches on palms and soles found in soil and transmitted during injury (southern states) Dermatophytes: no yeast form affect superficial keratinized structures (scaly skin, hair loss, and brittle nails) through action of keratinase pruritic papules, vesicles Microsporum (spiky, spindle-shaped, thick-walled, single) Trichophyton (cylindral, smooth, thinwalled, single) Epidermophyton (club-shaped, smooth moderately thick-walled, clusters of 2-3) direct contact fomites animals: Microsporum also spread from dogs, cats ”Dermatophytid” reactions: hypersensitivity to fungal antigens no organisms found in granulomas tinea capitis: scaly calp, hair loss (T. tonsurans, T. rubrum) tinea corporis: ringworm of glabrous/smooth skin red, raised tinea cruris (jock itch): red itchy patches on groin, scrotum tinea pedis (athlete’s foot): toescracking, peeling of skin tinea unguium (“onchomycosis”): thickened, discolored, brittle nails tinea barbae: patches along beard distribution DIAGNOSIS / TREATMENT skin scrapings w/ KOH prep selenium dandruff shampoo topical imidazole topical miconazole for Tinea versicolor keratolytic agent: salicylic acid for Tinea nigra skin scrapings w/ 10% KOH on glass slide shows hyphae macronidia or microconidia ecothrix: hyphae around hair shaft endothrix: hyphae w/in hair shaft Wood’s light: fluorescence when tinea capitis lesions caused by Microsporum placed in UV light topical imidazole oral griseolfulvin (hair, nails) Subcutaneous Mycoses: Sporotrichosis: Sporotrix schenckii dimorphic fungi in soil, plants (rose thorns, splinters) enters via trauma grow in soil, vegetation infect during trauma subcutaneous nodule: local pustule or ulcer that spreads along lymphatics more necrotic nodules along linear, lymphatic distribution Chromoblastomycosis (Phialophora, Cladosporium) soil fungi in tropics: bare feet and legs Mycetoma (Petriellidium, Madurella) wounds on feet, hands, or back slowly progessive granulomatous infection through skin trauma cauliflower warts w/ crusting abscess along lymphatics: initially, one violet-colored wartlike lesion more nodules over months/years abscesses, with pus discharged through sinuses (pus has compact colored granules similar to Actinomyces, Nocardia lesions cigar-shaped budding yeasts branching hyphae w/ oval conidia at tips “daisy petals” oral KI itraconazole or amphotericin B copper-colored sclerotic bodies: dark brown, funus in WBC’s, M local excision/ itraconazole sulfonamides: actinomycotic form no treatment for fungal form SYSTEMIC FUNGI: within lungs differentiate into yeasts itraconazole for lung disease Coccidiodes immitis dimorphic (mold, spherule w/ endospores) soil of arid regions: southwestern USA, Latin America (Arizona, New Mexico, southern CA) Filipinos 2nd most common opportunistic infection in AIDS patients Histoplasma capsulatum (nonencapsulated) dimorphic (mold, yeast) faculatative intracellular parasite soil w/ bird droppings (ie. Starlings, bats) Ohio, Mississippi River Valleys mostly asymptomatic or mild pneumonia not contagious from person to person amphotericin B for severe , disseminated disease in soil, it forms hyphae with alternating arthrospores and tissue: spherules w/ doubly refractive walls filled w/ endospores empty cells inhalation of arthrospores by humans dissemination in IC: meningitis; bone and skin granulomas erythema nodosum (red tender nodules on extensor surfaces) and arthralgia “valley fever” (San Joaquin Valley, CA.) or “desert rheumatism” (Arizona) 2 types of asexual spores: tuberculate macroconidia (thick walled w/ fingerlike projections lab ID) and inhaled, infectious microconidia (smaller, thin, smooth-walled spores) calcification of small granulomatous foci in lungs/ spleen AIDS pts: liver, spleen, and lymph nodes: hepatosplenomegaly skin tests (spherulin or cocciodin) DTH rxn IgM/ IgG precipitin test tissue: oval budding yeast cells found in M skin tests (histoplasmin) DTH rxn complement fixation chest X-ray (TB) Blastomyces dermatitidis dimorphic (mold, yeast) moist soil rich in organic material North America (east of Mississippi) and Central America worldwide Paracoccidiodes brasiliensis endemic to rural Latin America inhaled ovid conidia also infects other animals (dogs) rarest systemic fungal infection but also most severe and rarely asymptomatic ulcerated granulomas of skin, bone w/ weight loss, night sweats inhaled spores tissue: thin-walled round yeast cells w/ single broad-based buds and doubly refractive walls tissue: thick-walled with multiple buds OPPORTUNISTIC FUNGI: diabetes, lymphomas, broad spectrum antibiotics, immunosuppression (chemotherapy, AIDS pts) Candida albicans oral thrush (creamy white patches) oval yeast w/ single bud; blastoconidium diaper rash (skin folds: between fingers, groin) budding yeast cells and pseudohyphae vaginitis: vaginal itching and discharge ( risk during menses and pregnancy, oral contraceptives, antibiotics, DM, pH) normal flora of mucous membranes of upper IC: esophagitis (substernal chest pain and dysphagia) respiratory, GI, and female genital tracts dissemination (retinal exam shows multiple white fluffy candidal normal flora, but never in blood patches) sign of neutropenia Cryptococcus neoformans oval budding yeast (no mold form) pigeon droppings eucalyptus tree Aspergillus fumigatus aspergilloma mold only: septate hyphae V-shaped airborne conidia (inhaled, ingested, cut skin) A. flavus on rice/grains mycotoxins (ie. aflatoxin) toxic or carcinogenic to liver hepatocellular carcinoma Mucormycosis (Mycor, Rhizopus) saprophytic molds only: nonseptate hyphae (root branches) w/ broad irregular walls and right-angle branches inhaled through lungs mostly asymptomatic meningitis pneumonia; bone and skin granulomas 4th cause of death in AIDS pts dissemination: skin, CNS, heart, lung, nasa-orbital area, cornea AIDS: hemoptysis and granulomas (lung cavitations) allergic bronchopulmonary aspergillosis: type I hypersensitivity reaction (IgE) resembling asthma rhinocerebral mucormycosis: associated with diabetes infection of nasal mucosa w/ invasion of sinuses and orbit molds proliferate in walls of blood vessels (telangiectasia) C. albicans: germ tube test at 37 C X 3hrs. and chlamydospores oral thrush: ”swish and swallow” nystatin vaginitis: imidazole suppositories amphotericin B (dissem. disease) skin test w/ Candida: indicator of competent cellular immunity India ink: halo around organism CSF: Ab to capsular antigen flucytosine or amphotericin B flat, velvety, bluish-green colony fungus ball on chest X-ray surgical removal, amphotericin B endospores enclosed w/in a sporangium surgical resection amphotericin B PROTOZOANS: eukaryotes with endoplasm, ectoplasm, and a cytosome definitive host: harbors sexually reproducing stage intermediate host: harbors asexually reproducing stage Intestinal and Urogenital: Entamoeba histolytica invasion of intestinal epithelium and secrete enzymes localized trophozoites w/ RBC in motile amoeba (trophozoite) cytoplasm active disease necrosis “teardrop” ulcer erode and destroy intestines cysts or trophozoites w/o ingestion of nonmotile cyst (4 nuclei) amoebic dysentery: bloody, mucus-containing diarrhea w/ internalized RBC carrier state lower abdominal discomfort, flatulence, tenesmus, weight loss differentiates into trophozoites in the ileum diloxanide furoate to kill cysts 1 cyst=8 trophozoites colonize colon, cecum amoebic abscess of liver: RUQ pain, weight loss, fever, tender, (luminal amebicide) enlarged liver can penetrate diaphragm and cause lung disease trophozoites (single nucleus) in diarrheal stool metronidazole (Flagyl): luminal E. coli: 8 nuclei E. hartmani: 4 nuclei also, but smaller cysts in formed stool and systemic amebicide E. dispar: nonpathogenetic 1-2% of U.S. population (homosexual males) Giardia lamblia cysts differentiate to trophozoites in duodenum filter water: chlorination does not ingestion of cysts (4 nuclei) kill; must boil and filter no invasion: attachment to duodenal wall (surface of villi) 1 cyst = 2 trophozoites (pear-shaped w/ 4 string test: swallowing string into inflammation of mucosa malabsorption of protein, fat duodenum trophozoites adhering pairs of external flagella w/ 2 anterior nuclei) nonbloody, foul-smelling diarrhea w/ nausea, anorexia, camping, day-care centers, homosexuals metronidazole (Flagyl) flatulence, and abdominal cramps for weeks to months; no fever Cryptosporidium parvum mild diarrhea attach to jejunum (no invasion) acid-fast stain (modified Kinyoun oocysts release sporozoites, which form acid-fast stain) oocysts in feces infants and AIDS patients: chronic, watery, nonbloody trophozoites oocysts passed out in feces diarrhea w/ large fluid loss (up to 3-17 liters of stool per day) no effective drugs; purify water ingested oocysts (4 motile sporozoites) life-threatening; may also have fever, dehydration, weight loss try azithromycin Cyclospora cayatanensis 1996 outbreak from contaminated raspberries fluoresce blue under UV light (Cyanobacterium-like body CLB) disease similar to Cryptosporidium (up to 6 weeks) Isospora belli severe diarrhea in immunocompromised (AIDS) patients trimethoprim + sulfamethoxazole (invasion of small intestine mucosa destruction of brush border) (Bactrim) elliptical oocysts w/ 8 sporozoites Microsporidia severe, persistent, watery diarrhea in AIDS patients albendazole obligate intracellular replication spores (spiral polar filaments) Balantidium diarrhea large ciliated trophozoites or large only ciliated protozoan cysts w/ V-shaped nucleus in stool main reservoir are domestic animals like pigs Trichomonas vaginalis watery, foul-smelling, greenish vaginal discharge w/ itching pear-shaped motile trophozoites on wet mount of vaginal secretions pear-shaped w/ central nucleus and 4 and burning sensation anterior flagella and undulating membrane 10% of men have urethritis (most are asymptomatic) sexual contact (no cysts, only trophozoite) metronidazole for both partners very common cause of vaginitis may affect pregnancy Naegleria fowleri cysts (resistant to chlorine) and trophozoites Acanthamoeba cysts (resistant to chlorine) and trophozoites Blood and Tissue Protozoa: Malaria: Plasmodium falciparum (common) Plasmodium malariae (4%) Plasmodium vivax (common) Plasmodium ovale (very rare) vector: female Anopheles mosquito tropical, subtropical areas 300-500 million clinical cases/ year 1.5-2.7 million deaths (mostly children) blacks w/ sickle cell more immune than whites P. vivax, P. ovale, P. falciparum 48 hr. cycle P. malariae 72 hr. cycle schizogony: nuclear division w/o cell division merozoites bud off from schizonts P. vivax, P. ovale: hypnozoites latent in liver reactivation Toxoplasma gondii cat feces w/ cysts eat undercooked pork sexual reproduction in cats transplacental transmission (TORCH) infect any nucleated cell most common CNS infection in AIDS patients Pneumocystis carinii (classified as fungus) mortality > 80% if untreated, 50% if treated 1st disease diagnosed in >50% of AIDS pts. most people have been exposed meningoencephalitis: just like bacterial meningitis nausea/vomiting, fever, headache, stiff neck 95% die within 1 wk chronic, granulomatous, brain infection in AIDS patients keratitis: inflammation of cornea in contact lens wearers PMN, protein, glucose amphotericin: poor results PMN, protein, glucose amphotericin: poor results asexual cycle/schizogony (in humans): sporozoites enter humans during blood meal by mosquito enter hepatocytes within 30 minutes differentiate into schizonts rupture and release merozoites into blood infect RBC’s differentiate into ringshaped trophozoites schizonts (16-32 nuclei) merozoites sexual cycle/sporogony (in mosquitoes): some merozoites develop into male and female gametocytes (one female macrogamete or 8 sperm-like microgametes) diploid zygote sporozoites salivary glands thick and thin Giemsa stain of blood smears: presence and ID signet-ring trophozoites w/in infected RBC’s P. falciparum: crescent-shaped gametocytes others: spherical chloroquine: acute malaria kills merozoites (in RBC’s) primaquine: prevent relapses in P. vivax, P. ovale by killing hypnozoites mefloquine or (quinine + Fansidar: sulfadoxine, pyrimethamine) for chloroquineresistant strains of P. falciparum chemoprophylaxis w/ chloroquine, pyrimethamine bednets avoid stagnant water abrupt onset of fever/chills, headache, myalgia, arthralgia two weeks after mosquito bite periodic cycle of chills, fevers, and sweats (coincides w/ cycle between destruction of RBC’s) fever spikes (up to 41 C) w/ splenomegaly, nausea/vomiting, abdominal pain, and drenching sweat accompanying fever brain/kidney involvement if P. falciparum untreated hemolysis hemoglobiuria (dark urine = “blackwater fever”) “sticky knobs” adhere and plug up capillaries brain necrosis cell-mediated immunity symptoms may resemble mononucleosis (heterophil-negative) infection during pregnancy (new infection) abortion, stillbirth, neonatal disease w/ encephalitis, chorioretinitis (blindness), hepatosplenomegaly, fever, intracranial calcifications IC: fatal encephalitis (reactivation of dormant cysts) airborne inhalation (no person to person though) sudden onset of fever, nonproductive cough, dyspnea, tachypnea cysts in alveoli: inflammation frothy exudate blocking gas exchange no invasion of lung tissue IF assay for IgM antibodies crescent-shaped trophozoites in Giemsa stain preps sulfadiazine + pyrimethamine pregnant should avoid emptying litter boxes Giemsa stain of lung smear: trophozoites, intracystic bodies (opposed comma-like particles) bilateral rales and ronchi TMP-SMZ or pentamidine Trypanosoma cruzi (Chagas’ disease) South and Central America infected reduviid bug bites and defecates trypomastigotes contained in feces enter host bloodstream local replication in M and infiltration chagoma nonflagellated, round amastigotes w/in host cells (myocardial, glial, reticuloendothelial) Trypanosoma gambiense (Western Africa) humans only (slower: kills in months-years) Trypanosoma rhodesiense (Eastern Africa) zoonotic (more severe: kills in weeks-months) African Sleeping Sickness painful bite of Tsetse fly antigenic variation on surface glycoproteins VSG: > 100 genes, but 1 expressed at a time due to gene rearrangement chagoma (Romana sign) near bite site: facial edema (periorbital, perioral) + nodule myocarditis/cardiomyopathy arrhythmia death megasyndrome: megacolon, enlarged heart, enlarged esophagus meningoencephalitis in AIDS patients Leischmaniasis: Leishmania donovani visceral leishmaniasis attachment to M mediated by 2 molecules on parasite: 1) gp 63 (glycoprotein) 2) LPG (lipophosphoglycan) and several molecules on M C3 receptor, LFA1, p150,95 visceral leishmaniasis (Kala-azar): double peak (diurnal) fever, hepato-splenomegaly, pancytopenia, immunosuppression, IgG affect organs of reticuloendothelial system (liver, spleen, BM) hyperpigmentation of light-skinned patients Leishmania tropica (Old World)cutaneous Leishmania mexicana (New World)cutaneous Leishmania braziliensis mucocutaneous painless bite of sandfly ingestion of amastigotes in M of host amastigotes able to live at pH=4 (cytoplasm) differentiate to promastigotes migrate to pharynx of sandfly infect on next bite reside in phagolysosome of M reservoir: forest rodents trypomastigotes multiple and differentiate into epimastigotes in insect gut become trypomastigotes passed in insect feces metacyclic trypomastigotes ingested in blood meal by tsetse fly procyclic stage: multiplication in insect midgut migrates to salivary glands transforms to epimastigotes multiply more and forms metacyclic trypomastigotes carried by fly bite host enter bloodstream and become blood-form trypomastigotes hard, red painful skin ulcer: heals within 2 weeks lymphadenopathy and intermittent weekly fever; dizziness demyelinating encephalitis: daytime drowsiness, dysarthria, muscle tremors, apathy coma and death (usu. from pneumonia) cutaneous: initially, red papule at bite site enlarge satellite nodules that coalsce & ulcerate Oriental sore, Chiclero’s ulcer in CMI large areas of skin affected (leprosy) mucocutaneous: papule at bite site metastatic lesions at mucocutaneous junction of nose-mouth destroy nasal cartilage death 2 to infection, starvation, aspiration pneumonia blood smear trypomastigotes xenodiagnosis: reduviid bug bites host look for epimastigotes in gut nifurtimox or benznidazole: kill trypomastigotes in blood; less effective against amastigotes in tissue no effective therapy for chronic disease blood smear trypomastigotes aspirate of chancre or enlarged LN parasites suramin: curative if given before onset of encephalitis (does not cross BBB no CNS penetration) melarsoprol: extremely toxic but used if CNS involvement pentamidine: alternative drug presence of amastigotes in skin lesion or BM, spleen, LN biopsy skin test (using leischmanin: crude homogenate of promastigotes) sodium stibogluconate HELMINTHS (WORMS): Cestodes: Tapeworms Taenia solium (pork tapeworm) ingestion of raw, cured, undercooked pork containing larvae (cysticerci) cysticercus: pea-sized fluid-filled bladder scolex has 4 suckers and circle of hooks attach to gut wall worldwide, but endemic in Mexico, Latin America, Spain, Portugal, Africa, SE Asia Taenia saginata (beef tapeworm) ingestion of raw or undercooked beef containing larvae (cysticerci) scolex had 4 suckers and NO hooklets worldwide, but endemic in Africa, S. America, Europe Diphyllobothrum latum (fish tapeworm) ingestion of undercooked fish containing larvae (plerocercoid or sparganum larvae) no suckers; 2 elongated suckling grooves Scandinavia, Japan, northern Russia, Canada Echinococcus granulosus (dog tapeworm) ingestion of eggs by humans dog=definitive host sheep=intermediate host human=dead end intermediate hosts sheep-raising areas: CA, AZ, NM, Alaska, Canada, S. America, Africa, Mediterranean scolex w/ hooks, but only 3 proglottids (one of smallest tapeworm) Hymenolepis nana (dwarf tapeworm: smallest) most frequently found tapeworm in U.S. Trematodes: Flukes pig ingests egg-infested human feces eggs develop into larvae that disseminate through intestine into muscle of animal and develop into cysticercus uncooked pork with larvae eaten by humans cysticercus attach to gut wall: anorexia, mild diarrhea larvae take 3 months to grow to adult size (5 m) ingestion of eggs cysticercosis: eggs hatch into larvae in gut and penetrate into tissue and encyst usually asymptomatic until larvae dies in 4-5 years inflammatory response: anaphylactic shock, retinitis/uveitis, seizures, meningitis, death cattle ingest gravid proglottids detached daily and passed in human feces embryos (oncospheres) emerge from egg and burrow into cow’s intestine larvae in muscle of cattle larvae take 3 months to grow to adult size (10 m) most are asymptomatic: anorexia and mild diarrhea do not cause cysticercosis in humans larvae attach to gut wall and become adult worms gravid proglottids release fertilized eggs and passed in stool fresh water eggs eaten by crustaceandifferentiate to larvae eaten by fish most are asymptomatic: abdominal discomfort and diarrhea absorb vitamin B12: megaloblastic anemia 1000’s of worms in dog’s intestineseggs passed out in feces and contaminate environment and ingested by sheep (or humans) oncosphere embryos emerge migrate to liver (or lungs, bones, brain) large fluid-filled hyatid cysts cyst rupture anaphyaxis liver cyst hepatic dysfunction lung cyst bloody sputum brain cyst headache, focal neurologic signs no intermediate hosts: humans ingest eggs reinfect humans abdominal discomfort and nausea/vomiting gravid proglottids w/ 5-10 primary uterine branches in stools (T. saginata has 15-20 branches) calcified cysticerci on CT scan larvae floating in vitreous niclosamide praziquantel for cysticercosis ( Ca++ permeability paralyze worm; Ab-mediated WBC killing) gravid proglottids w/ 15-20 primary uterine branches in stools niclosamide for intestinal worms (uncouples oxidative phosphorylation immobilizationexpulsion) oval (other tapeworms are round) eggs w/ lidlike opening (operculum) longest tapeworm (up to 13 m) niclosamide brood capsules containing multiple protoscoleces CT scan and tissue biopsy surgical removal of cysts hypertonic saline kill organism albendazole niclosamide 8-10 polar filaments between hooks praziquantel Schistosomiasis (blood flukes): S. mansoni (African, Middle East, S. America), S. japonicum (Orients, water buffalo, pigs) affect GI system (live in mesenteric veins) in definitive venos site, female lays fertilized eggs penetrate vascular endothelium enter gut or bladder lumen eggs excreted in stools or urine hatch in fresh water ciliated larvae penetrate snailsdevelop & multiplemany cercariae S. haematobium (Africa, Middle East) affects urinary tract (adults live in urinary bladder) most pathologic findings from presence of eggs in liver, spleen, or wall of the gut or bladder acute phase: itching, dermatitis, fever/chills, diarrhea, lymphadenopathy, hepatosplenomegaly, eosinophilia free-swimming, fork-tailed cercariae penetrate the skin “Swimmer’s Itch” adults exist as separate sexes but live attached to each other: female resides in a groove in the male, “the schist”, where he continously fertilizes her egg Clonorchi sinensis (Oriental liver fluke) ingestion of undercooked fish w/ cercaria snail is intermediate host (ingests eggs) Paragonimus westermani (lung fluke) ingestion of raw crab meat w/ larvae penetrate GI wall migrate thru diaphragm Fasciola hepatica (sheep liver fluke) sheep and other domestic animals in Latin America, Africa, Europe, and China eating watercress (or other aquatic plants) contaminated by larvae Fasciolopsis buski (intestinal parasite of hymans and pigs) endemic to Asia, India Heterophyes heterophyes eating raw fish (Africa, Asia) w/ cysts Nematodes (Intestinal): Roundworms S. mansoni, S. japonicum: GI hemorrhage, hepatosplenomegaly (eggs in liver granulomas fibrosis, hepatomegaly, portal hypertension splenomegaly), death from exsanguination from ruptured esophageal varices S. haematobium: hematuria; superimposed bacterial UTI’s; granulomas, fibrosis of bladder carcinoma of the bladder excystation in duodenumenter biliary ducts bile duct fibrosis/ hyperplasiabile duct carcinoma (cholangiocarcinoma) upper abdominal pain, anorexia, hepatomegaly, eosinophilia enters the lung parenchyma hermaphroditic adults produce eggs that enter bronchioles chronic cough w/ bloody sputum TB-like: pleuritic chest pain, dyspnea, recurrent bact. pneumonia larva excyst in duodenum penetrate gut wall reach liver RUQ pain, fever, hepatomegaly obstructive jaundice halzoun: painful phayngitis from adult flukes on posterior wall flukes acquired from eating raw sheep liver eating aquatic vegetation carrying cysts pathology due to damage of intestinal mucosa by adult fluke most asymptomatic; may have ulceration, abscesses, hemorrhage inflammation of intestinal epithelium: abdominal pain, nonbloody diarrhea molecular mimicry: incorporating host antigens onto surface fool host’s immune system S. mansoni: prominent lateral spine S. japonicum: small lateral spine S. haematobium: terminal spine praziquantel: initial exacerbation of symptoms (death evokes vigorous immune response) typical small, brownish, operculated eggs in stool praziquantel typical operculated eggs in sputum or feces praziquantel praziquantel surgically remove adult flukes in pharynx and larynx typical eggs found in feces praziquantel typical eggs found in feces praziquantel Enterobius vermicularis (pinworm) ingestion or inhalation of worm eggs most common helminth in U.S. (mostly affects children < 12) Trichuris trichiura (whipworm) ingestion of eggs in soil contaminated w/ feces slow life cycle (incubate 3-6 wks in soil) Ascaris lumbricoides (largest intestinal: >25cm) ingestion of eggs in soil contaminated w/ feces very common (esp. in tropics, and southern states in the U.S.) major damage occurs during migration rather than presence of adult worms in the intestine Ancylostoma duodenale (Old World) Necator americanus (New World hookworm) filariform larva in moist soil penetrate skin worlwide distribution, esp. tropical areas endemic in southern states major damage occurs during migration rather than presence of adult worms in the intestine Strongyloides stercoralis (small roundworm) 2 distinct life cycles: 1) w/in human body 2) free-living in soil penetration of skin by infectious (filariform) larvaemigration up trachea and swallowed major damage occurs during migration rather than presence of adult worms in the intestine Trichinella spiralis eating undercooked pork (U.S.: home-made sausages) w/ larvae encysted in striated muscle Nematodes (Tissue): Roundworms lifecycle confined to humans: eggs hatch in small intestine, where larvae differentiate to adults and migrate to colon and mate female migrates to anus at night and releases 1000’s of eggs majority: asymptomatic, some perianal pruritus eggs hatch in GI migrate to cecum and ascending large intestinemature adult produces 1000’s of eggs/day for 6-8 yrs abdominal pain and diarrhea larvae migrate through gut wall into bloodstream into the lungs up bronchi and trachea and swallowed become adults in SI live in lumen, does not attach to wall 1000’s of eggs/ day ascariasis: pneumonia w/ fever, cough, and eosinophilia adult worms can cause abdominal pain and obstruction larvae carried by blood to lungsmigrate into alveoli and up bronchi and trachea swallowed become adults in SI attach to wall (cutting plates: Necator or teeth: Ancylostoma) eggs develop 1st into noninfectious, feeding (rhabditiform) larvae then into 3rd stage, infectious, nonfeeding (filariform) larvae ”Ground itch”: pruritic papule or vesicle at entry site loss of blood microcytic anemia (weakness and pallor) larvae molt into adults in small intestine eggs hatch in mucosa rhabditiform larvae passed in feces entire life cycle in soil or filarial larvae, which penetrates intestinal wall directly w/o leaving host and migrate to lungs (autoinfection) pneuminitis w/ coughing and wheezing if high worm burden female worms: inflammation of mucosa hyperinfection ( damage) in immunocompromised: bloody, watery diarrhea and sepsis from infiltration of enteric bacteria gastroenteritis a few days after eating undercooked pork 1-2 weeks later: fever, muscle pain, periorbital edema, eosinophilia CNS, cardiac symptoms frequent ”Scotch tape” of perianal skin eggs not found in stools mebendazole or pyrantel pamoate (only kill adult worms, not eggs) may require retreatment typical eggs (barrel-shaped w/ plugs at each end) in stool mebendazole transient pulmonary infiltrates and eosinophilia (Loeffler’s syndrome) oval eggs with irregular surface in stools; occasionally, adult worms mebendazole or pyrantel pamoate transient pulmonary infiltrates and eosinophilia (Loeffler’s syndrome) eggs in stool occult blood in stool frequent mebendazole or pyrantel pamoate larvae in stool striking eosinophilia (seen in all migratory nematode infections) thiabendazole or mebendazole larvae w/in striated muscle steroids plus mebendazole (not very effective) Wuchereria bancrofti (Pacific Islands, Africa) Brugia malayi (Malay Peninsula, SE Asia) female mosquito (Anopheles, Culex) bites and deposits infective larva (L3) that penetrates skin and enters lymph node Onchocerca volvulus female blackfly Simulium deposits infective larvae while biting subcutaneous tissue Loa loa bite of deer fly Chrysops deposits infective larva on skin wander in body become adults Dracunculus tiny crustaceans w/ infective larvae swallowed in drinking water Nematode Larvae Diseases: Toxocara canis major cause of visceral larva migrans definitive host is dog; humans: dead-end hosts young children (more likely to ingest soil) Ancylostoma caninum (dog hookworm) Ancylostoma braziliense (cat hookworm) children, construction workers exposed to infected soil (mainly southern U.S.) Anisakis ingested in raw seafood (sushi, sashimi) After 1 year: mature to adults that produce microfilaria (L1) circulate in blood (mainly at night) ingested by mosquito microfilaria produce infective larva (L3) transferred w/ next bite early: asymptomatic late: fever, lymphangitis, cellulitis obstruction of lymphatics edema of legs and genitalia (elephantiasis) differentiate into adults, usually within dermal nodules ”river blindness” (infection rate > 80% in endemic areas) disease: cellular immune response to death of microfilariae females release microfilariae that enter blood (daytime)taken up by fly during bloodmealdifferentiate to infective larvae…. thick blood smears from patient at night reveal microfilariae Calabar swellings: hypersensitivity rxn causing transient (2-3 days), localized, erythematous, subcutaneous edema adult worm crawling across the conjuctiva (harmless) larvae released in small intestine and migrate to body adults adult females cause skin to ulcerate and release motile larvae burning, itching inflamed papule w/ ulceration diethylcarbamazine (microfilariae only) surgical excision of worms in eyes head of worm in the skin ulcer: worm looped out under the skin and slowly pulled out over course of days adult female in dog intestine produces eggs that are passed in feces into the soil human ingest soil w/ eggs larvae in SI migration to many organs (liver, brain, and eyes) granulomas form around dead larva (delayed hypersensitivy) blindness due to retinal involvement; fever, hepatomegaly larvae penetrate skin and migrate through subcutaneous tissue causing an inflammatory response prurutic lesions (“creeping eruption”) similar eruptions w/ Strongyloides and Necator eosinophilia (larval migration) hypergammaglobulinemia can penetrate submucosa of stomach or intestine gastroenteritis, eosinophilia, and occult blood in stool no effective drugs diethylcarbamazine (against microfilaria only paralyze) ivermectin (microfilaria only GABAmuscle paralysis) suramin (kills adults, but toxic) visualization of microfilariae in a blood smear diethylcarbamazine oral or topical thiabendazole