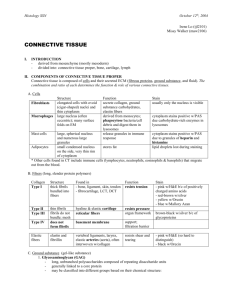
Connective Tissue
advertisement
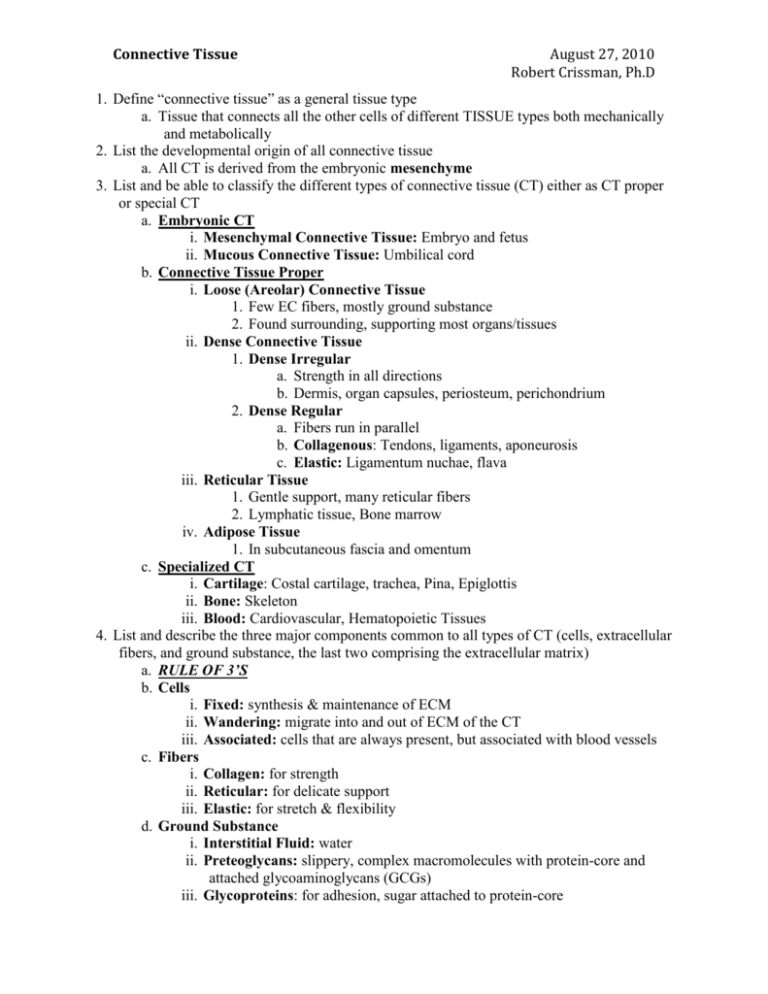
Connective Tissue August 27, 2010 Robert Crissman, Ph.D 1. Define “connective tissue” as a general tissue type a. Tissue that connects all the other cells of different TISSUE types both mechanically and metabolically 2. List the developmental origin of all connective tissue a. All CT is derived from the embryonic mesenchyme 3. List and be able to classify the different types of connective tissue (CT) either as CT proper or special CT a. Embryonic CT i. Mesenchymal Connective Tissue: Embryo and fetus ii. Mucous Connective Tissue: Umbilical cord b. Connective Tissue Proper i. Loose (Areolar) Connective Tissue 1. Few EC fibers, mostly ground substance 2. Found surrounding, supporting most organs/tissues ii. Dense Connective Tissue 1. Dense Irregular a. Strength in all directions b. Dermis, organ capsules, periosteum, perichondrium 2. Dense Regular a. Fibers run in parallel b. Collagenous: Tendons, ligaments, aponeurosis c. Elastic: Ligamentum nuchae, flava iii. Reticular Tissue 1. Gentle support, many reticular fibers 2. Lymphatic tissue, Bone marrow iv. Adipose Tissue 1. In subcutaneous fascia and omentum c. Specialized CT i. Cartilage: Costal cartilage, trachea, Pina, Epiglottis ii. Bone: Skeleton iii. Blood: Cardiovascular, Hematopoietic Tissues 4. List and describe the three major components common to all types of CT (cells, extracellular fibers, and ground substance, the last two comprising the extracellular matrix) a. RULE OF 3’S b. Cells i. Fixed: synthesis & maintenance of ECM ii. Wandering: migrate into and out of ECM of the CT iii. Associated: cells that are always present, but associated with blood vessels c. Fibers i. Collagen: for strength ii. Reticular: for delicate support iii. Elastic: for stretch & flexibility d. Ground Substance i. Interstitial Fluid: water ii. Preteoglycans: slippery, complex macromolecules with protein-core and attached glycoaminoglycans (GCGs) iii. Glycoproteins: for adhesion, sugar attached to protein-core Connective Tissue August 27, 2010 Robert Crissman, Ph.D 5. List all common locations in the body of each type of CT a. This is found in the answer to Objective 3 6. List and describe the three types of fibers in CT. Classify them according to size, morphology, chemical composition, and function a. Collagen: for Strength i. Most abundant protein in the body ii. Inelastic, yet flexible iii. Fasicles: Bundles of fibers found in CT Proper iv. Collagen Fiber 1. Straight, unbranched fibrous protein 2. 64 nm periodicity 3. Made of collagen fibrils v. Collagen Fibril 1. Singular unit of FIBER 2. Same Periodicity 3. Made of up Tropocollagen Molecules vi. Tropocollagen Molecules 1. Consist of 3 Consist of 3 polypeptide chains a. Each ~1000 a.a. b. Rich in Glycine, Proline, Hydroxyproline, and Hydroxylysine c. 3 chains held together by h-bonding b/t hydroxyproline d. These molecules line up end-to-end and side-by-side to form fibril e. Quarter Stagger Theory: describes alignment of tropocollagen and accounts for periodicity f. Covalent bonding b/t hydroxylysine in adjacent tropocollagen molecules holds together collagen fibril vii. Types of Collagen 1. Type I: Strength; Skin, Tendons, Organ capsules, Bone, Dentin 2. Type II: Resist Pressure; Hyaline & Elastic cartilage 3. Type III: Delicate Support; Lymph system, spleen, liver, Lungs, CV 4. Type IV: Attachment Filtration; Basal Lamina b. Reticular Fibers i. Small, branched, and squiggly; intersect at Right Angles ii. Composed of Collagen Type III fibrils covered with a Sugar Coat iii. Reticular cells wrap each fiber iv. Found in regions with many wandering cells v. Function to provide “delicate support” c. Elastic Fibers i. Y-branched, fuse at acute angles, not squiggly *diagnostic character* ii. Consist of 2 Components 1. Amorphous Component: made of elastin, rich in Glycine, but also contains desmosine & isodesmosine 2. Microfibril Component: different glycoprotein iii. Function to add elasticity to tissue (up to 150% stretch memory) iv. Found in areas with a much stretching: vessels, aorta, skin, lungs, uterus Connective Tissue August 27, 2010 Robert Crissman, Ph.D 7. Describe how the precursors of different fibers are secreted by the cell and aggregate to form fibers outside of the cell. Be able to characterize disease related to improper fiber formation a. Secretion and Aggregation i. Collagen 1. Multiple steps 2. Transcription in nucleus 3. Translation in rER 4. Hydroxylation of proline & lysine in rER 5. Formation of procollagen 6. Secretion via Golgi 7. Cleavage of procollagen into tropocollagen by Procollagen peptidase on the cell’s exterior 8. Self-assembly of tropocollagen into fibril in ECM 9. Covalent linking of hyrodxylysine by Lysyl Oxidase to form insoluable fibril 10. Constant turnover due to breakdown of collagen by collagenase ii. Reticular Fibers: same as collagen iii. Elastic fibers 1. Proelastin tropoelastin outside of cell 2. Covalent bond formation by Lysyl oxidase to form elastin in a mesh of microfibrils 3. Elastic fiber system composed of 3 types of elastic fibers a. Oxytalan fibers: microfibrillar component b. Eulanin fibers: microfibrils and amorphous elastin c. Elastic fibers: as previously described 4. Continuous turnover due to breakdown of elastic fiber by elastase b. Related Disease States i. Collagen-related 1. Scurvy: a. Lack of Vitamin C (necessary co-factor in hydroxylation of proline b. Results in weak collagen, no wound-healing, etc 2. Ehlers-Danlos, Type VII a. Change in procollagen peptidase b. Hyperflexibilty, soft skin, dislocations c. Indicated by increased [Gly] in urine ii. Reticular fiber-related 1. Ehler-Danlos, Type IV a. Deficiency of Type III collagen b. Aneurysms, Intestinal rupture iii. Elastic fiber-related 1. Marfan’s a. Poor microfibrillar (fibrillin) component formation b. Tendency of aorta and blood vessels to rupture 2. Emphysema a. Lung dysfunction caused by breakdown of elastic fibers Connective Tissue August 27, 2010 Robert Crissman, Ph.D 8. List and describe the components of the amorphous ground substance (water, proteoglycans, and glycoproteins). Relate their structure to their function. a. Proteoglycans i. Protein core with sulfated glycsoaminoglycans attached to form a porous, hydrated gel. ii. Can be non-sulfated or sulfated 1. Non-Sulfated: Hyaluronic Acid a. Large macromolecule, highly coiled b. Carries a net negative charge which attracts Na and Ca, and subsequently water c. Slippery, lubricating d. Resists Compression e. Acts as physical barrier to prevent migration of bacteria, except pathogenic species use hyaluronidase to cleave it and migrate f. Acts to inhibit cellular adhesion and facilite cell migration, esp during development and wound healing 2. Sulfated GAGs a. Keratin sulfate: cartilage b. Heparin Sulfate: basement membrane c. Chondroitin-6- and Chondroitin-4-: skin, bone, cartilage d. Dermatin sulfate: dermis iii. Can be free or transmembrane 1. Free Proteoglycan: present within ground substance of loose CT a. Aggrecan: free in areolar CT matrix b. Aggrecan Aggregate: hyaluronic acid with 100s of aggrecan i. very gel-like c. Perlacan: found in basal lamina, contains much heparin 2. Transmembrane: Proteoglycans which span cell membrane a. Syndecan: rich in heparin and chondroitin; one end in cytoplasm, one in ECM b. Fibroglycan: Binds 3 types of collagen and fibronectin b. Glycoproteins i. Smaller molecules, protein core with branched sugars attached ii. Typically act as adhesion molecules to hold cells to EMC iii. Fibronectin: found in basal lamina, binds heparin and Type IV Collagen iv. Laminin: Lacated in BM; binds heparin and Type IV v. Entactin: Located in BM; binds laminin and Type IV vi. Tenascin: Located in BM; binds syndecan and fibronectin c. Interstitial Fluid i. Water found in interstitial space ii. Important for material transport iii. Bound by proteoglycans (hyaluronic acid) 9. Describe how the components of the extracellular matrix enable it to act as a medium for transfer of nutrients and wastes between the blood stream and any other cells or tissues. a. Much of the water in the interstitial fluid flows out of capillaries, along parenchyma and back into either the lymphatic system or other capillaries. This movement brings along nutrients. Connective Tissue August 27, 2010 Robert Crissman, Ph.D 10. Describe the process of edema and relate this to its various causes a. Edema: abnormal buildup of interstitial fluid in extracellular matrix b. Pitting vs Myxedema: Myxedema does not pit, caused by hypthyroidism (increased [GAG]) c. Causes: i. Blocked Lymphatics: sugery, elephantiasis ii. Blocked Venous Return: compromised veins iii. Liver disease: insufficient albumin iv. Increased vascular permeability: histamine (mast cells), anaphylaxis v. Hypertension: increased hydrostatic pressure at arterial end of capillary vi. Starvation: decreased albumin = decreased veinule osmotic pressure 11. Describe and understand the components of the basement membrane and relate its structure to its function. a. Basement membrane: i. Visible with light microscopy, located in extracellular space ii. Functions to connect NERVE, MUSCLE, EPITHELIAL, & ADIPOSE tissue to connective tissue (i.e. no BM around CT, except for adipose tissue) iii. Three layers (from closest to plasma membrane, out) 1. Lamina lucida: contains integrins, laminins, entactin 2. Lamina densa: contains Type IV collagen, perlancan (heparin sulfate), fibronectin, carries (-) charge 3. Lamina reticularis: reticular fibers (Type III) and type IV/VII and anchoring fibers iv. Basal lamina: Lamina lucida and Lamina densa v. Function: anchor cells to connective tissue, act as macromolecular sieve 12. List and describe the morphology and function of each cell type normally found in the connective tissue. Classify them as “fixed,” “wandering,” or “associated.” a. Fixed Cells: cells that produce and maintain ECM of a particular CT type i. Fibrocyte 1. Most common fixed cell 2. Can’t see cytoplasm, vesicular nucleus with nucleolus 3. Secretory cell 4. –blast: Immature, divisible, production of fibers 5. –cyte: not able to divide, upholds matrix ii. Mesenchymal Cell 1. Embryonic, pluripotential 2. Looks like fibrocyte (only difference is location) iii. Reticular Cell 1. Found in reticular tissue 2. Processes wrap around reticular fibers 3. Form cell-lined fiber network iv. Adipose cells 1. White Adipocytes a. Large, spherical b. Unilocular: single, large lipid droplet c. Empty due to lipid extraction during processing, Connective Tissue August 27, 2010 Robert Crissman, Ph.D d. “Signet Ring” appearance e. Location: Loose CT, subcut. Fascia f. Function: Lipid storage i. Lipid leaves blood and broken down by Lipoprotein Lipase into free fatty acid and glycerol ii. Fatty acid taken up by adipocyte and complexed with glycerol into neutral lipid (triglyerides) iii. Lipid released from adipocyte by Hormone Sensitive Lipase, which breaks up triglyceride back to free fatty acid which complexes with albumin in blood g. Produce Leptin: which acts to decrease appetite and increase energy consumption. h. Acted on by insulin to form triglycerides from glucose, increase glucose uptake, and produce Lipoprotein Lipase i. Norepi/Epi act in opposition to insulin: fight or flight, increase Hormone sensitive lipase 2. Brown Adipocytes a. Found in hibernating animals and newborn humans near aorta, axilla, mediastinum, scapulae b. Multilocular: many lipid droplets c. Function: heat generation i. Fatty acid accumulation acts to uncouple oxidation process ii. Thermogenin: Mitochondrial membrane protein permitting flow of H+ to make heat instead of generate ATP 3. Others a. Chondrocyte: Cartilage b. Osteocyte: Bone c. Blood cells: “Fixed” cell of blood b. Wandering Cells: transient cells which migrate into and out of connective tissue i. Macrophage: Big eaters 1. Phagocytic 2. Part of Mononuclear Macrophage System a. Monocyte Macrophage once in CT 3. Only identifiable by using vital dye 4. Oval, indented nucleus with vesicular chromatin pattern 5. Lots of lysosomes 6. Functions: Phagocytic, Antigen-presenting ii. Mast Cells 1. Granular, oval cells associated with small blood vessels 2. Clear nucleus, obscured by granules 3. Granules include: Heparin, Histamine (Vasodilator, Increase Vascular permeability, Bronchiole constriction), Eosinophilic Chemotaxic factor, Neutrophilic Chemotaxic factor, Leukotrienes 4. Function: Store mediators of inflammation, Connective Tissue August 27, 2010 Robert Crissman, Ph.D 5. Bind IgE and interact with antigens. Upon first antigenic exposure, form IgE’s. Upon second antigenic exposure, antigen binds to IgE and causes cascade which releases granular contents 6. Potential to cause anaphylactic shock 7. Located along capillaries of mucosa, respiratory, digestive and urinary tracts 8. Paracine secretion iii. Plasma 1. Eccentrically located nucleus, cartwheel chromatin, lots of rER** diagnostic 2. Normally found only in CT (i.e. not in blood) 3. Derived by B-lymphocytes 4. Function: produce antibodies c. Associated Cells: Cells found in blood vessels which are always surrounded by CT i. Endothelial Cells: Lining of blood vessel ii. Smooth Muscle Cells: surround endothelium and control size iii. Pericytes: MPSCs for vessel repair/growth 13. Describe and discuss how the mount and type of the individual components determine the structural and functional characteristics of the individual types of connective tissues a. Different types of connective tissue have cells/fibers/ground substance in varying proportions to serve specific function. Structure determines function. 14. List the general functions of connective tissues. a. Mechanical support: “mother natures packing material” b. Mechanical protection c. Energy storage/temp control d. Material transport e. Protection from infection f. Repair after injury 15. Understand that adipose tissue is a special type of connective tissue. Identify the major cell type found in the two different types of adipose tissue and its function with its specific morphology. Be able to locate the 2 different types of adipose tissue in the body. a. See above objective 16. Describe and identify the characteristic morphology and function of the specific types of CT (areolar CT, mucous CT, mesenchyme, dense irreguluar, dense regular, elastic, reticular, and adipose). a. See above objective 17. Know the meaning of the following terms and how they are related to connective tissues a. Review list on page 252 of packet