Appendix 12: Occupational Health Assessment Questionnaire
advertisement

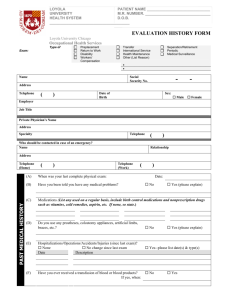
RESEARCH PASSPORT Occupational Health Assessment Questionnaire [This template taken from Research in the NHS – HR Good Practice Resource Pack is the minimum standard expected. Current version of Pack available at: www.nihr.ac.uk/systems/Pages/systems_research_passports.aspx] Occupational Health Assessment Questionnaire This form contains confidential medical information and must not be copied or forwarded to anyone outside the occupational health service of the researcher’s substantive employer/place of study. Only with the researcher’s consent may any confidential information about the researcher be discussed with the occupational health service of NHS organisations where the researcher wishes to conduct research. The purpose of this health assessment is to ensure, so far as is possible, that you are fit for the research activities you will be undertaking in order to protect your own and others’ health and safety. Questions are asked about your past and present health, medical treatment and any impairment which may have implications for health and safety. Please see guidance notes for infectious diseases and vaccinations attached to this form Please note a response to your Health questionnaire will be issued within 14 days. If you have any difficulties completing this form or wish to discuss any issues in a confidential setting please contact the occupational health department on Tel: 0191 208 7344 for advice. 1. PERSONAL DETAILS Surname: Prof Forename(s): Miss Work Address/Place of Study: Cost Centre No. Tel: Mobile: Dr Ms Mr Mrs Other Email: Date of birth: Gender: Male Position applied for Proposed start date Have you attended an Occupational Health Department for screening, or completed a Health Questionnaire previously? Female Yes No If yes, where, when and why? NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 1 of 11 2. DESCRIPTION OF RESEARCH ACTIVITIES: (This will enable our occupational health advisers to assess the health risk involved with your research) Name of Research project Please give details of the project and nature of the work involved 2.2. During your research activity will you be involved in direct contact with patients/service users? This includes face to face interviewers, trial coordinators and with contact with patients. If yes describe nature of patient contact below. Yes No If NO complete Section 3 and Declaration only. If YES please complete the full questionnaire 2.3. Will you be undertaking exposure-prone procedures (EPP)? Exposure-prone procedures (EPPs) are those invasive procedures where there is a risk that injury to the worker may result in the exposure of the patient’s open tissues to the blood of the worker. These include procedures where the worker’s gloved hands may be in contact with sharp instruments, needle tips or sharp tissues (e.g. spicules of bone or teeth) inside a patient’s open body cavity, wound or confined anatomical space where the hands or fingertips may not be completely visible at all times. Yes No If YES complete Section 4. If NO Section 4 may be omitted. Further information NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 2 of 11 3. BLOOD BORNE VIRUS RISK 3.1 Will you be at risk of exposure to blood-borne viruses? Yes No This includes work with human blood, tissue or cells. If so give details of the nature of the work involved. 3.2 Hepatitis B immunisation. Give dates of when you completed initial immunisation and your last booster. Please indicate if you had a blood test to confirm the effectiveness of the immunisation. Initial: 2nd: 3rd: Booster: PVS blood test* Do you have documented evidence of the blood test *Documented evidence of this is required. Please attach scanned copies to this result. Yes No 4. EXPOSURE PRONE PROCEDURES ASSESSMENT (IF REQUIRED) Have you had: Yes No Date Result/.Comments /Validation (For OH Use) Hepatitis B antigen (HBsAg) *if positive positive//negative Hepatitis B e antigen (HBeAg) positive//negative *if negative Hepatitis is B viral load (BV DNA) Hepatitis C antibody copies/ml positive/negative HIV Antibody positive//negative NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 3 of 11 5. VACCINATION HISTORY Please give details of vaccinations and tests you have had. Have you had: Yes No Date Result/.Comments /Validation (For OH Use) 1. BCG vaccination Scar size: mm 2. Do you have a scar? 3. Rubella (German measles) immunisation Documented evidence of at least 2 MMR vaccinations required. Please attach scanned copies to this form 4. Rubella antibody test Documented evidence of test result required. Please attach scanned copies to this form. 5. Measles immunisation Either as part of MMR or as a single measles immunisation Documented evidence of test result required. Please attach scanned copies to this form. Immune : Yes No Immune : Yes No 6. Tetanus immunisation Give date of last booster 7. Diphtheria immunisation 8. Varicella (Chickenpox ) immunisation Immune : Yes 9. Varicella (VZV) antibody test No 6. CHILDHOOD INFECTIOUS DISEASES HISTORY Please give details of childhood infectious diseases you have had. Where possible give dates. Have you had: Yes No Date Comments /Validation (For OH Use) Measles Mumps Chicken pox German measles (rubella) Whooping cough NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 4 of 11 7. TUBERCULOSIS ASSESSMENT Have you lived for a significant length of time in a high tuberculosis risk area (Africa, Indian subcontinent or the far east) Yes No Dates Have you had a TB immunity/screening test (Heaf, Mantoux or interferon – gamma test). Yes No Date Have you ever had a chest x-ray? If yes please state why Where and when was the chest x -ray done? If yes please provide scanned documented result Yes No Was it normal? Yes No Have you had a cough for more than 3 weeks in the past year? Yes No Have you had any unexplained loss of weight or fever (high temperature) in the past year? Yes No Have you or anyone in your family had Tuberculosis (T.B.)? If YES who and when? Yes No Are you being followed up for contact with infectious Tuberculosis? Yes No 8. DECLARATION OF HEALTH 1. Do you currently have any health problems, including psychological problems, or are you awaiting surgery? Yes No 2. Are you presently receiving any prescribed medication, treatment or therapy except contraception? Yes No 4. Do you have any health or psychological condition that may affect your ability to perform the proposed research activity? Yes No 5. Do you have any health condition caused or made worse by work? Yes No Yes No Yes No 3. How many days off sick have you had over the past two years? 6. Do you have any disability or other health condition not mentioned above that may require additional help or support to perform the research activity? 7. Have you been working abroad in the last 12 months? NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 5 of 11 If you have answered ‘yes’ to any of the above, please give details including dates and how it affects you now. Continue on a separate sheet if necessary. Question Further details 1. 2. 3. 4. 5. 6. 7. 9. DECLARATION The information in this form is true and complete. I agree that any deliberate omission, falsification or misrepresentation in the form may be grounds for rejecting this application and/or subsequent disciplinary action. I consent to relevant health information about me being shared between the occupational health service of my employer/place of study and the occupational health service of any NHS organisations where I wish to undertake research activities. I hereby agree to inform the occupational health service of my employer/place of study and of any NHS organisations where I will be conducting research activities of any changes in my health circumstances that may affect my ability to perform the research activity. I understand my responsibility to notify the occupational health service of my employer/place of study and of any NHS organisations where I will be conducting research activities if I think I have had significant exposure to, or am carrying, a serious communicable condition such as Hepatitis B, Hepatitis C or HIV and to follow advice from a consultant in occupational health or another suitably qualified colleague about treatments and/or modifications to my practice. I understand the importance of routine infection-control procedures, including the importance of hand hygiene, appropriate use of protective clothing and compliance with local policies in the NHS organisations where I wish to undertake research activities. Signed: NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Date: Occupational Health & Safety Services Page 6 of 11 FOR OCCUPATIONAL HEALTH SERVICE USE INITIAL DECISION FIT ON QUESTIONNAIRE FURTHER INFORMATION REQUIRED CLINIC ASSESSMENT REQUIRED SEE ON COMMENCEMENT DATE COMMENT/ ACTION NHS TRUST/HR INFORMED HR/ MANAGER INFORMED APPOINTMENT ARRANGED HUMAN RESOURCES INFORMED APPOINTMENT ARRANGED Date_______________ __________________ Date_______________ Date_______________ Date_______________ Date_______________ Notes ____________________________________________________________________________________________ _________________________________________________________________________________________________ CLINIC TESTS SPECIFY RESULTS FINAL DECISION RECOMMNEDATIONS /COMMENT FIT TO UNDERTAKE RESEARCH FIT FOR PATIENT CONTACT FIT FOR EPP FIT WITH RESTRICTIONS UNFIT OH Physician / Adviser’s signature _____________________________ Date _________________________ NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 7 of 11 CERTIFICATE OF FITNESS FOR RESEARCH PASSPORT Name: Position: Date of Screening Research Protocol : Chief Investigator : School/Service/Institute : Project Start Date Following review of the pre placement health screening questionnaire the above person is considered to be : ( tick appropriate) Fit to undertake research project work within HEI Fit for patient contact Fit with restrictions( specify): Unfit Fit for Exposure Prone Procedures Unfit for EPP Occupational Health Newcastle University Name OH Physician/ Practitioner / Advisor Title Signature Date Forward to Newcastle Trust for MRSA screening NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 8 of 11 Guidance Note Infectious Diseases Screening for Research Passport Rubella (German Measles) Rubella infection during pregnancy poses a significant threat to the developing baby. All health care workers (which includes researchers) with direct patient contact who are not immune to rubella must be immunised using the MMR (measles, mumps, rubella) vaccine unless documented evidence of two doses of MMR vaccine rubella immunity is available. A past history of the illness or of vaccination alone is not sufficient evidence of immunity. The candidate must produce documentary proof of two doses of MMR vaccine or rubella immunity demonstrated by blood test. If this is not possible give a course of MMR vaccine. There is no need to carry out a further blood test. Varicella (Chicken Pox) The Chief Medical Officer has recommended that health care workers (which includes researchers) with direct patient contact who are not immune to chicken pox should be immunised using the chicken pox vaccine. This is recommended to protect susceptible workers and also to protect vulnerable patients from acquiring chickenpox from an infected member of staff. Those candidates who are UK born with a good history of chickenpox or shingles can be considered immune to varicella. Those who do not have such a history or were born outside of the UK should be checked for antibodies to varicella and informed of the result; in the vast majority of cases, they will be found to be immune. Those found to be susceptible should be offered immunisation against varicella, provided immunisation is not contra-indicated in that individual: The following staff are required to be immune to varicella staff routinely working with immunocompromised patients staff in the adult and paediatric infection diseases units and staff routinely working with neonates Contra-indications to the vaccine include pregnancy, immunosuppression due to disease or treatment, and previous hypersensitivity reactions to the vaccine. People immunised with this vaccine may develop a varicella-like rash following the first or second dose. All such rashes must be reported to Occupational Health. If the rash is generalised, then the staff member should be excluded from work until all lesions are crusted over and no new lesions are appearing. Localised rashes may be kept covered and the staff member allowed to continue working, but if the staff member works with immunocompromised patients, or paediatric patients his/her status should be reviewed by Occupational Health and infection control on an individual basis. NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 9 of 11 Tuberculosis Persons carrying out research in the NHS who have direct contact with patients or work with clinical specimens should not start work until they have completed a TB screen or health check, or until documentary evidence is provided of such screening having taken place within the preceding 12 months. If the candidate has had a health screen for tuberculosis within the last twelve months ask them to provide documentary evidence. If they have received BCG vaccine check for the presence of a BCG scar or obtain documentary evidence of successful BCG to confirm this. If they have not had BCG vaccine for tuberculosis or a BCG scar is not evident and documentary evidence is not available, carry out an interferon-gamma test for latent TB. This test does not indicate TB immunity and is not affected by previous BCG vaccination. A positive result indicates the possibility of latent tuberculosis. Staff should be advised that they may have encountered tuberculosis in the past and that they do not need a BCG vaccination. They should be advised to report suspicious symptoms should they arise in the future. However, staff coming to work in the UK from countries with a high incidence of tuberculosis should be referred to the chest clinic for clinical examination and chest X-ray, even if they are asymptomatic. If the candidate has not had BCG or a BCG scar is not evident a risk assessment for TB exposure should be carried out. High risk areas include: Work in neonatal and maternity units Work in mortuaries Work in respiratory medicine Work with people from high risk areas Work with clinical specimens which may pose a risk such as sputum specimens. Work with immunocompromised patients. Candidates in these areas should be assessed for TB immunity. Evidence of immunity includes: documented evidence of previous BCG immunisation a history of immunisation plus BCG scar a history of immunisation without a BCG scar but with a documented positive Heaf test of grade 2 or more (or a positive Mantoux test with 6-15mm of induration) within the last five years No further action is required if the above criteria are satisfied. Otherwise a Mantoux test should be performed and a BCG vaccination offered when the test result shows induration of less than 5mm. If BCG is given, there is no need to inspect the site of vaccination at a later date for the presence of a scar, and repeat Mantoux testing and repeat BCG immunisations are unnecessary. It should be remembered that the period between immunisations and scar development, the staff member will not be fully protected against tuberculosis. The activities of the staff member during this period should be reviewed by Occupational Health and the infection control team to assess the potential risk to the staff member and to patients. NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 10 of 11 If a member of staff refuses to have a BCG or cannot be immunised for other reasons, this fact should be recorded and the risks explained to him/her. Asymptomatic staff who have Mantoux test results with an area of induration of 6mm or more should not be automatically referred for a chest x-ray, with one exception Such staff should be advised that they may have encountered tuberculosis in the past and that they do not need a BCG vaccination. They should be advised to report suspicious symptoms should they arise in the future. However, staff coming to work in the UK from countries with a high incidence of tuberculosis should be referred to the chest clinic for clinical examination and chest X-ray, even if they are asymptomatic, if their Mantoux test result shows an area of indurations of 15mm ore more. Tetanus / Measles / Diphtheria The candidate should confirm immunisation status for these conditions. There is no specific requirement for these with regard to the provision of an NHS passport but MMR vaccine is recommended for those who have not had measles or been vaccinated against measles. Candidates born prior to 1970 and those with a definite history of measles can be considered immune to measles. Others should be offered immunity screening or two doses of MMR vaccine. Hepatitis B Candidates working with human blood, tissue or cell cultures should be immunised against Hepatitis B. *’Direct contact’ means face-to-face contact with patients/service users NTWCLRN-P003_RPPolicy_Version 0.4_04AUG2009 /ohupdatedJAN2012 Newcastle University Occupational Health & Safety Services Page 11 of 11