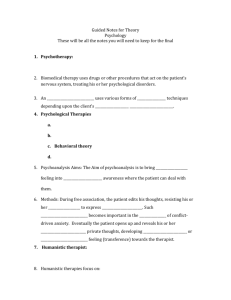
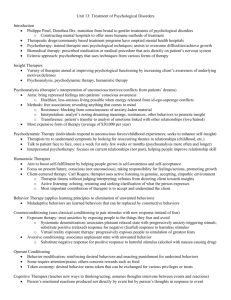
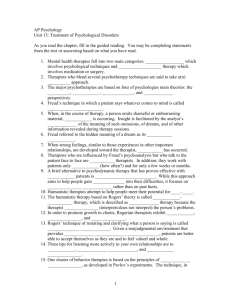
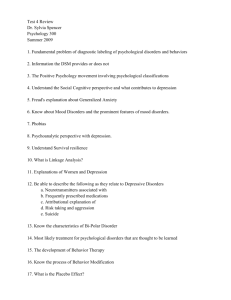
Unit Summary
advertisement

PLEASE NOTE: The Instructor’s Resources files lose their formatting in the conversion from Quark XPress® to Microsoft Word®. The final formatted files are also available in Adobe PDF® for your convenience. Treatment of Psychological Disorders OUTLINE OF RESOURCES I. Introducing Treatment of Psychological Disorders Introductory Exercise: Fact or Falsehood? (p. 3) Lecture/Discussion Topic: The Availability and Adequacy of Treatment (p. 4) Classroom Exercises: Therapist Role-Playing (p. 3) Attitudes Toward Seeking Professional Psychological Help (p. 3) Videos: Psychology: The Human Experience, Module 40: Problems in Living* Digital Media Archive: Psychology, 1st ed., Video Clips 35 and 36: Treatment of Drug Addiction and Early Treatment of Mental Disorders* Psychology Video Tool Kit: Early Treatment of Mental Disorders* Outpatient Commitment: Forcing Persons Into Mental Health Treatment* II. The Psychological Therapies Feature Film: Ordinary People and Psychotherapy (p. 4) A. Psychoanalysis Lecture/Discussion Topic: Good Candidates for Psychoanalysis (p. 5) B. Humanistic Therapies Lecture/Discussion Topic: Computer-Assisted Psychotherapy (p. 5) Classroom Exercises: Understanding Empathy (p. 7) Role-Playing to Demonstrate Client-Centered Therapy (p. 7) The Self-Concealment Scale (p. 8) The Imposter Phenomenon (p. 8) Student Project: Dibs and Play Therapy (p. 8) PsychSim 5: Computer Therapist (p. 5) C. Behavior Therapies Lecture/Discussion Topics: Virtual Iraq (p. 10) Exposure Therapy—Improving Its Effectiveness (p. 11) Therapy and Totalitarian Control (p. 11) Classroom Exercises: Using Systematic Desensitization to Treat Eraser Phobia (p. 9) Modeling (p. 11) Assessing Assertiveness (p. 12) Student Projects: Practicing Systematic Desensitization (p. 10) Modifying an Existing Behavior (p. 12) ActivePsych: Digital Media Archive, 2nd ed.: Therapy in the Real World: The Use of Real-Life Exposure to Treat Phobias* *Video, ActivePsych, and Psychology Video Tool Kit titles followed by an asterisk are not repeated within the core resource unit. They are listed, with running times, in the Preface of these resources and described in detail in their Faculty Guides, which are available at www.worthpublishers.com/mediaroom. Videos: The Mind, 2nd ed., Module 30: Treating Drug Addiction: A Behavioral Approach* Scientific American Frontiers, 2nd ed., Segment 31: Virtual Fear* Feature Film: Harry Potter and the Prisoner of Azkaban (p. 9) D. Cognitive Therapies Lecture/Discussion Topics: Strategies to Correct One’s Thinking (p. 13) Overcoming the Fear of Public Speaking (p. 14) Classroom Exercise: Frequency of Self-Reinforcement Questionnaire (p. 14) Student Project: Mood-Memory Repair (p. 15) Psychology Video Tool Kit: Treating OCD: Exposure and Response Prevention* E. Group and Family Therapies Psychology Video Tool Kit: City of Gheel: Community Mental Health at Its Best* III. Evaluating Psychotherapies A. Is Psychotherapy Effective? Lecture/Discussion Topics: The Consumer Reports Study (p. 16) Fringe Medicine (p. 17) Regression Toward the Mean (p. 17) Thinking Errors and Clinical Judgment (p. 19) Therapy and the Nature of the Problem (p. 19) Classroon Exercise: Regression Toward the Mean and Aspiration Level (p. 18) Video: The Mind, 2nd ed., Module 3: The Placebo Effect: Mind-Body Relationship* PsychSim 5: Mystery Therapist (p. 16) B. The Relative Effectiveness of Different Therapies Lecture/Discussion Topics: Writing About Emotional Experiences as Therapy (p. 20) Psychological Treatments Versus Psychotherapy (p. 21) Video: Psychology: The Human Experience, Module 41: Empirically Validated Therapies* C. Evaluating Alternative Therapies Lecture/Discussion Topics: Pets in Therapy (p. 21) Trepanation (p. 22) Autobiographies (p. 22) Psychology Video Tool Kit: Dealing With Panic* D. Commonalities Among Psychotherapies Lecture/Discussion Topic: Evaluating Self-Help Resources (p. 23) E. Culture and Values in Psychotherapy Lecture/Discussion Topic: Mental Health Values of Professional Therapists (p. 24) Student Project: Applying the Major Therapies (p. 25) (Useful as a conclusion to section III) Psychology Video Tool Kit: Mentally Ill Chemical Abusers: A Community Problem* When Treatment Leads to Execution: Mental Health and the Law* IV. The Biomedical Therapies A. Drug Therapies Lecture/Discussion Topics: SSRI Antidepressants (p. 25) Cosmetic Psychopharmacology (p. 25) A Pill for Stage Fright (Anxiety) (p. 26) ActivePsych: Digital Media Archive, 2nd ed.: The Therapeutic Effect of Antipsychotic Drugs* Schizophrenia: New Definitions, New Therapies * Undesired Effects of Conventional Antipsychotic Drugs* Videos: The Mind, 2nd ed., Module 33: Mood Disorders: Medication and Talk Therapy* The Brain, 2nd ed., Module 28: Schizophrenia: Pharmacological Treatment* Digital Media Archive: Psychology, 1st ed., Video Clip 34: Schizophrenia* B. Brain Stimulation Lecture/Discussion Topic: Electroconvulsive Therapy (p. 27) Videos: The Mind, 2nd ed., Module 34: Treating Depression: Electroconvulsive Therapy (ECT)* Digital Media Archive: Psychology, 1st ed., Video Clip 37: Electroconvulsive Therapy* C. Psychosurgery Lecture/Discussion Topic: Cingulotomy (p. 27) D. Therapeutic Life-Style Change Lecture/Discussion Topic: Therapeutic Life-Style Change (p. 28) V. Preventing Psychological Disorders Lecture/Discussion Topics: Positive Psychotherapy (p. 29) From a Disease Focus to a Wellness Model (p. 29) Principles of Effective Prevention Programs (p. 30) Classroom Exercise: The Personal Growth Initiative Scale (PGIS) (p. 30) UNIT OUTLINE I. Introducing Treatment of Psychological Disorders (pp. 605–606) Introductory Exercise: Fact or Falsehood? The correct answers to Handout 13–1, as shown below, can be confirmed on the listed text pages. 1 2 3 4 5 F (p. 606) 6. F (pp. 625–626) F (p. 610) 7. F (p. 626) F (p. 613) 8. T (p. 628) F (pp. 620–621) 9. T (p. 632) T (p. 625) 10. F (p. 633) Classroom Exercise: Therapist Role-Playing Timothy Osberg suggests a role-playing activity to introduce the topic of therapy. He uses it primarily to demonstrate how our underlying theories about psycho-logical disorders guide the therapeutic methods we use. Although Osberg designed the exercise primarily for abnormal and clinical psychology courses, it also seems appropriate for introductory psychology students, particularly if they have just studied Unit 12 on psychological disorders. As an introduction to Unit 13, read the following to your students: As a preface to our discussion of the various theoretical approaches to psychotherapy, I have a brief exercise wherein I’d like each of you to assume the role of therapist. Please sit back and imagine that a good friend of yours has approached you about a problem he or she has developed recently. This friend describes several symptoms, including increased feelings of depression, crying spells, loss of interest in usual activities, and changes in sleep and eating patterns. Let’s assume you have asked enough questions to allow you to conclude that this per-son is clinically depressed. Your task is to assume the role of therapist and develop some possible interventions. Spend a few minutes reflecting and I will ask members of the class to volunteer suggestions. Please write two or three ideas on a sheet of paper. After students have been given 4 to 5 minutes to respond, ask for volunteers to share their suggested interventions and record them on the chalkboard. Osberg notes that students’ recommendations often include having the person increase the number of his or her activities or involvements, increase exercise, expand social networks, attend self-help or other group therapy sessions, begin journaling, and seek medication. After obtaining 8 to 10 suggestions, note how they reflect students’ underlying theories of depression. Osberg explains that students tend to favor behavioral or cognitive-behavioral strategies. However, as you review the various therapies discussed in the text, remind the class of the extent to which their suggestions reflected each approach. Osberg, T. (1996, August). Students as therapists: An activity for abnormal and clinical psychology courses. Paper presented at the Annual Convention of the American Psychological Association, Toronto. Classroom Exercise: Attitudes Toward Seeking Professional Psychological Help Psychologists Edward Fischer and Amerigo Farina have developed a scale to assess respondents’ attitudes toward seeking psychological help. In introducing this unit, you might have students complete the scale (see Handout 13–2). To score, students first need to reverse the numbers they placed before items 2, 4, 8, 9, and 10 (0 = 3, 1 = 2, 2 = 1, 3 = 0), and then add the numbers in front of all 10 items. Total scores can range from 0 to 30, with higher scores reflecting a more favorable attitude toward seeking professional psychological help. Fischer and Farina report mean scores of 19.08 and 15.46 for female and male undergraduates, respectively. You can use the scale to initiate a class discussion of possible obstacles to seeking help. Is it more difficult for people to seek help for psychological problems than for medical problems? What accounts for gender differ-ences in attitudes toward seeking professional psycho-logical help? In addition to gender differences, the authors report that within certain ethnic groups, those who hold strong cultural affiliations are less inclined to favor seeking professional help than are those who identify with the broader American culture. There is also a tendency for psychology and social science majors to be more favorably inclined toward seeking professional help. Among the major academic concen-trations, those with business concentrations were least in favor of it. What might account for these individual differences? A 2004 American Psychological Association (APA) poll reported that nearly half of Americans have had someone in their household seek mental health treat-ment at some time. Most (81 percent) continue to per-ceive cost and lack of insurance coverage (87 percent) as barriers to getting treatment. An increasing number of Americans (85 percent) believe that health insurance should cover mental health services, up from 79 percent when the same question was asked in December 2000. Poll results also showed that only 30 percent of Americans say that they would be concerned about other people finding out that they had seen a mental health professional, and only 20 percent say that stigma is a very important reason not to seek help. Nearly half (47 percent) say that the stigma surrounding mental health services has decreased in recent years and that the media gets the most credit for that (35 percent), although society in general (25 percent) seems to be more accepting as well. American Psychological Association. (2004, May 13). APA poll: Most Americans have sought mental health treatment but cost, insurance still barriers. APA Online. Retrieved February 14, 2009 from www.apa.org/ releases/practicepoll_04. html. Fischer, E. H., & Farina, A. (1995). Attitudes toward seeking professional psychological help: A shortened form and considerations for research. Journal of College Student Development, 36, 368–373. Lecture/Discussion Topic: The Availability and Adequacy of Treatment How many people who need therapy actually receive it? In Unit 12, we reported Ronald Kessler and his colleagues’ survey of the prevalence of psychological disorder. In their assessment of a representative sample of 9282 Americans, they also sought to determine whether people who suffer psychological disorder are receiving adequate treatment. Their study suggested that only a third of patients receive adequate care (treatments were considered effective if there was evidence that they led to significant improvement). A total of 41 percent of those with a disorder actually sought treatment in the past year; this rate is significantly higher than the 25 percent who obtained treatment a decade ago or the 19 percent who were treated two decades ago. About one-third of all visits for mental illness are to “alternative” practitioners such as herbalists or chiropractors, whose interventions show little evidence of effectiveness. About two of every five visits are to a mental health specialist who is not a psychiatrist— psychologist, marriage counselor, social worker, etc.; these people do best at offering well-established treat-ments. Those least likely to receive care are the elderly, racial minorities, and rural residents. On the other end of the continuum are the disproportionately affluent. Nearly a third of visits for mental health care are made by people who don’t have a disorder. “Maybe they’re nipping things in the bud,” said Kessler, “we just don’t know.” Men don’t seek care as quickly as White women. How long do people wait to go for treatment if they have symptoms of mental disorder? The average delay is almost a decade. The sooner in life an illness begins, the longer the delay and the more persistent the disor-der. Delay also depends on the specific disorder. Average time of delay for bipolar disorder is 6 years; for generalized anxiety disorder it is 9 years; for attention-deficit hyperactivity disorder, 13 years; and for specific phobia, 20 years. Elias, M. (2005, June 7). Mental illness: Surprising, dis-turbing findings. USA Today, p. 8D. Kessler, R. C., et al. (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. II. The Psychological Therapies (pp. 606–618) Feature Film: Ordinary People and Psychotherapy Winner of four Academy Awards, including the award for best picture, Ordinary People contains some of the best portrayals of psychotherapy in motion picture his-tory. Although the entire film is too long to show in most classes, you could assign it for out-of-class view-ing or show selected segments in class. Perhaps the most moving and powerful segment comes toward the end of the film as guilt-ridden Conrad Jarrett, with the help of his therapist, Dr. Berger, achieves a new per-spective on himself and his family. More specifically, Conrad gains insight into his involvement in the boat-ing accident that killed his oldest brother, Bucky. The segment vividly demonstrates the empathic, trusting, caring relationship between therapist and client that is one of the important commonalities among psychother-apies. The segment begins 98:07 minutes into the film and runs 7:15 minutes. If you show this scene, be sure to explain that it comes after many therapeutic sessions in which Conrad has wrestled with self-blame compli-cated by alienation from his parents, particularly his mother. Other brief clips that effectively portray psy-chotherapy are sprinkled throughout the film, including one of Conrad’s father’s first visit to Berger at 74:12 minutes (running 4:31 minutes). Indicating that he has come to talk about his son and voicing reservations about the utility of therapy, Calvin Jarrett eventually admits that he needs Berger’s help in understanding himself. Finally, to demonstrate obstacles to seeking therapy, you might show the restaurant scene beginning at 81:40 minutes (running 2:34 minutes) in which Conrad’s mother, Beth, demonstrates obvious defen-siveness. She tells her husband Calvin, “I don’t want to see any doctors or counselors. I’m me. This is my fami-ly. And if we have problems, we will solve them in the privacy of our own home. Not by running to some kind of specialist every time something goes wrong.” A. Psychoanalysis (pp. 606–608) Lecture/Discussion Topic: Good Candidates for Psychoanalysis Psychoanalysis is long and costly. Thus, before psycho-analysis begins, the therapist often has a series of ses-sions to determine how appropriate the treatment may be for the patient. Psychoanalysts seem to agree that the following four personal qualities are crucial to deter-mining whether analysis will be successful. 1 Motivation. The person needs strong internal moti-vation to persist in treatment that will require sev-eral sessions per week for several years. 2 Capacity to form interpersonal relationships. The potential patient must have the capacity to form, maintain, and ultimately detach from an intimate, trusting relationship. 3 Capacity for introspection and insight. The therapy requires natural curiosity about oneself and the capacity for self-scrutiny. 4 Ego strength. The person must be able to accept the “rules” of psychoanalysis and be open to painful facts and interpretations about himself or herself. Sarason, I., & Sarason, B. (2005). Abnormal psychology (11th ed.). Upper Saddle River, NJ: Prentice Hall. B. Humanistic Therapies (pp. 609–610) PsychSim 5: Computer Therapist This program is based on the famous ELIZA program. A person talks to the computer as he or she would to a nondirective therapist. The computer picks up certain key phrases and responds accordingly. The program also contains some historical information, along with a note on the limitations of computer therapy. Lecture/Discussion Topic: Computer-Assisted Psychotherapy There have been many attempts to use the computer in therapy. ELIZA (see the previous description in PsychSim) is only one. Roger Gould, a psychiatrist at UCLA, has designed the Therapeutic Learning Program (TLP) to help patients clarify their problems and gradu-ally to resolve conflicts by developing plans of action. At the beginning of each session, the patient “convers-es” with the computer. Later on, he or she talks with a “real” therapist. “It’s a computer-assisted psychothera-py,” explains Gould. An increasing number of psychi-atric hospitals are licensed to use TLP because it helps people talk to themselves much as a therapist would talk to them. The case of John, a businessman, provides a good example of how TLP works. In the first session, John reports a high degree of stress and a change in appetite and energy level. The computer offers the client several choices: “The stress I’m feeling in my work has to do with starting a new business . . . changing jobs or careers . . . being criticized . . . .” From 15 choices, John picks “being criticized.” The computer continues: “Are you feeling stress over your behavior in that you may be out-of-control in any of the following ways? Drinking too often . . . gam-bling too much . . . spending too much money . . .?” John answers that he drinks and spends too much. At the end of the session, the computer provides an analysis of John’s situation, as well as some advice. Speaking for John, the computer states, “It’s possible that these internal conflicts may be responsible for some of the difficulty I’m having in dealing with the other sources of stress in my life. It may even be that my loss of confidence in myself and my out-of-control behavior are causing or contributing to some of the other stresses.” At this point the issue is pursued with a “live” therapist. In the second session, with the continued help of the computer, John begins to define specific “action steps.” After acknowledging a need to be more assertive with his boss, Simon, John gets support from TLP. Again, speaking for John, the computer states: “The stress of being criticized in my work life makes me feel angry. This is complicated by the fact that I am being pressured to stop drinking. I have trouble dealing with this stress because I have difficulty stopping to think before reacting.” TLP recommends that John draw up an action plan. It has two parts. First, he must admit a need to accept reasonable criticism while pointing out to his boss the impossibility of his meeting short dead-lines without help. He will negotiate for more staff. Second, he must relieve the burden of stress caused by his own unrealistic work demands and become a person who can stand up for his rights. In subsequent sessions John weighs the possible adverse effects of taking these action steps. With the computer, he identifies 23 specific reservations. Once again, however, the computer is reassuring and identi-fies specific thinking errors as well as fears that may be based on “old but not forgotten rules” learned in child-hood. At the completion of the therapeutic process, John reports that he understands that he has been “unin-tentionally colluding” with his boss by trying to per-form in a “heroic” manner. He negotiates another full-time professional employee. His symptoms of stress disappear. James Reagan, a psychologist who has used TLP with many of his patients, notes that computer sessions sometimes help people whom therapists have been unable to reach. One woman who had been in and out of psychiatric hospitals for 20 years was asked by the computer to indicate what childhood events might be contributing to her problems. She checked off sexual abuse. It was the first time she’d said that. Either she hadn’t been asked the question before or had avoided it. Somehow, the computer enabled her to talk about it. Indeed, many people seem more willing to make intimate disclosures to a machine than to a counselor, at least in the early stages of therapy. In one study, patients at an alcohol treatment clinic admitted to drinking 30 percent more often when asked by a computer than when asked by a human. Women, in another study, were much more likely to disclose sexual problems to a com-puter than to a female psychiatrist. “The computer doesn’t blush,” says Reagan. “It doesn’t get judgmental, it doesn’t approve or disapprove. It’s just very patient.” Critics object. Psychiatrist T. Byram Karasu, for example, argues that human therapists—even those who think of therapy in terms of problem solving—do a lot more than transfer information. They spend time with their patients, they pay attention, they care. “The basis of psychotherapy is a human interaction, the genuine caring of a therapist for a patient,” says Karasu. “Until the computer is able to deliberate, then it is not a psy-chotherapeutic process.” Defenders counterargue. “Computers may be able to do better with some people,” says psychiatrist Kenneth Colby, “because those people won’t see a ther-apist at all.” For people who find the thought of psycho-logical help distasteful, it may be less disturbing to imagine sitting at a computer than lying on a couch. Marion Jacobs randomly divided 90 patients with mild to moderate psychological problems into two groups. In one group, each patient saw a psychothera-pist for 50 minutes each week for 10 weeks. In the other group, each patient used the TLP software program for 10 sessions supplemented by brief visits with the thera-pist for 10 to 15 minutes weekly. Participants in both groups showed a significant decrease in depression, anxiety, and perceived stress at the end of treatment. At a 6-month follow-up, patients in both groups reported treatment to have been effective. Patients generally pre-ferred the more intensive interaction with a therapist but they found the computer-aided treatment equally effective. C. Barr Taylor and Kristine Luce have provided a highly favorable review of computer-and Internet-based psychotherapy interventions. They conclude that com-puters can make psychological assessments more effi-cient, more accurate, and less expensive. In addition, computer-assisted therapy seems to be as effective as face-to-face therapy for treating anxiety disorders and depression. And, like assessment, it can be delivered at lower cost. Finally, the reviewers argue that the Internet can provide effective psychosocial support and group therapy. Studies indicate that Internet-based support groups are beneficial, with communication patterns being similar to those found in face-to-face groups. The reviewers call for more research to determine the spe-cific advantages and disadvantages of computer and Internetbased services. Nonetheless, they conclude that both are likely to play an increasingly important role in mental health assessment and intervention. As reported by Michael Price, psychologist Richard Munoz advocates the use of Internet-based interventions to underserved communities, particularly those in poor, rural areas. A single site can simultaneously serve a nearly unlimited number of people. Because many rural villages now have Internet cafés, interventions could reach those who would otherwise receive no help. With his colleagues, Munoz recently demonstrated the effectiveness of an Internet-based smoking cessation program that reached 4000 participants in 74 countries. Munoz maintains interventions could work with other serious problems, including depression, alcohol abuse, and pain management. A major challenge is to translate interventions into multiple languages and cultures. To fund his initiative, Munoz is looking for grants from the World Health Organization and from foundations and corporations interested in global health issues. Christensen, A., & Jacobson, N. (1994). Who (or what) can do psychotherapy: The status and challenge of non-professional therapies. PsychologicalScience,5,8–14. Davis, L. (1990, September/October). The doctor is on. InHealth,60–63. Hamilton, A. (1999, May 24). On the virtual coach. Time, 71. Jacobs, M. K., et al. (2001). A comparison of computer-based versus traditional individual psychotherapy. Professional Psychology: Research and Practice, 32, 92–96. Joyce, C. (1988, February). Learning to talk to yourself. Psychology Today, 47. Price, M. (2008, October). Underserved communities may benefit from Web interventions. Monitor on Psychology, p. 12. Taylor, C. B., & Luce, K. H. (2003). Computer-and Internet-based psychotherapy interventions. Current Directions in Psychological Science, 12, 18–22. Classroom Exercise: Understanding Empathy Carl Rogers encouraged therapists to exhibit empathy. When they accurately sense and reflect their clients’ feelings, he suggested, clients increase in self-under-standing and self-acceptance. The text suggests that establishing an empathic, trusting, caring relationship is one of the key components of all effective psycho -therapy. But how does one listen empathically? Peter and Dodge Fernald provide an exercise in which students imagine themselves in the role of counselor and consider what they might or might not say in displaying empathy. Handout 13–3, “Listening Empathically,” includes a statement by a client and 10 therapist responses (or thoughts) that students evaluate for empathic quality. Explain that empathy is the act of adopting the client’s perspective, of walking in the client’s shoes. The counselor’s task, argued Rogers, is To assume, in so far as he is able, the internal frame of reference of the client, to perceive the world as the client sees it, to perceive the client himself as he is seen by himself, to lay aside all perceptions of the external frame of reference while doing so, and to communicate some-thing of this empathic understanding to the client. After distributing the handout, give the following instructions: “As you listen to me role-play a client, pre-tend you are a counselor or a therapist. Your task is to adopt my perspective, that is, the client’s perspective. Try to see the world through my eyes. Imagine which of the ten statements listed at the bottom of the handout might run through your mind as you adopt my point of view. Check only those that demonstrate empathy.” Read the statement aloud with feeling so that the students have a sense of the client’s sadness and struggle. Give student about 5 minutes to check those responses that indicate an empathic perspective. Have students form small groups, then reach consensus on what statements constitute empathy. Alter-natively, ask volunteers from the full class to share their judgments. No doubt students will disagree. For example, some will argue that the first statement communicates empathy because it indicates the counselor’s desire to be helpful. However, it is not truly empathic because the client, even though he struggles to express himself, indicates no concern about getting started talking. Nor is the second statement empathic. Although the client’s statement may suggest indecisiveness, he indicates no specific concern about indecisiveness, nor does he refer to instances of indecisiveness. Continue the discussion by reviewing the remaining statements. Only items 3, 6, 7, 8, and 10 indicate empathic listening. Fernald, P. S., ! Fernald, L. D. (1999). Empathy: The cornerstone of counseling. In L. T. Benjamin, B. F. Nodine, R. M. Ernst, ! C. B. Broeker (Eds.), Activities handbook for the teaching of psychology (Vol. 4, pp. 393z396). Washington, DC: American Psychological Association. Classroom Exercise: Role-Playing to Demonstrate Client-Centered Therapy William Balch uses student volunteers to demonstrate Rogers’ client-centered therapy (also called person-centered therapy), which seems particularly well-suited for role-playing. Students who are interested, perhaps even majoring, in drama may be willing and eager participants. A week or so before the demonstration, recruit the volunteers and distribute Handout 13–4, which explains the situation and the roles to be enacted: Pat (male or female), who is faced with several conflicts, and Pat’s father, mother, and best friend. Each person discusses his or her problem with him in a series of improvised two-way dialogues. Each provides some directive advice, but Pat remains confused and uncertain. Finally, a nondirective therapist uses person-centered techniques to help him clarify his feelings. If you are a counseling psychologist, you should play the therapist; otherwise elicit the help of a counseling psychologist on campus. During the exercise you may wish to serve as a stage manager by introducing Pat, ushering in and out her parents, friend, and therapist, and providing appropriate commentary. Afterward, discuss the exercise with both the participants and the rest of the class. While the person-centered approach may be the easiest to role-play, other therapies also may be enacted, particularly if you have interested drama students. Balch reports that students usually play their roles plausibly and creatively. In a few cases they have become emotionally involved, particularly those playing Pat. It is probably wise to screen the participants carefully, then provide an opportunity for them to discuss their feelings after the demonstration. Balch notes one interesting phenomenon in con-ducting the exercise. When talking to the therapist, Pat typically speaks more slowly and at a lower pitch than when conversing with relatives or friends. He also engages in more eye contact with the therapist and, in general, seems more relaxed. Noting the effect may serve as a launching point for class discussion. Randy Larsen and David Buss suggest that empathic listening is a conversational strategy that can be developed. They suggest students practice with friends. You might assign your students the task of role-playing a client-centered approach in conversational dialogue with someone they know fairly well. They might ask a friend to describe a small problem from his or her life. Their task is two-fold. First, they should repeat what the person says, precisely as they understand it (e.g., “What I hear you saying is . . . .”). Their second task is to reflect back the friend’s feelings (e.g., “It seems you are feeling . . . about the situation.”). The friend will correct or elaborate on the problem or feeling. After a few minutes, they should switch roles, with the friend being the empathic listener and your student describing a small problem. If they role-play correctly, the two friends should feel greater mutual understand-ing and should be encouraged to explore their problem and feelings about it more fully. Have your students provide an informal report in class or brief written summary on their success in carrying out the project. Their report might include some reflection on the possible obstacles to empathic listening in everyday life. Balch, W. R. (1983). The use of role-playing in a class-room demonstration of client-centered therapy. Teaching of Psychology, 10(3), 173–174. Larsen, R. J., & Buss, D. M. (2008). Personality psychology: Domains of knowledge about human nature (3rd ed.). (p. 382). New York: McGraw-Hill. Classroom Exercise: The Self-Concealment Scale An important factor in effective humanistic therapy is providing clients with a safe environment in which they feel free to express themselves. This permits them to disclose negative emotions and distressing experiences, which is vital to their self-understanding and acceptance. Handout 13–5 is Dale Larson and Robert Chastain’s Self-Concealment Scale, which was designed to measure the extent to which people typically conceal or disclose personal information that they perceive as distressing and negative. Students can score their responses simply by totaling the numbers before all the items. Total scores range from 10 to 50, with higher scores reflecting a greater tendency toward self-concealment. Larson and Chastain reported that people who tended to conceal negative information about themselves were more likely to suffer from depression anxiety. In addition, several studies by other researchers suggest that honest self-disclosure improves self-understanding and helps people to come to terms with traumatic experiences. Although simply writing about the experience is often helpful, talking with a therapist seems to bring additional benefits. For example, in one study, researchers found that in comparison to those who simply wrote about traumatic events, those who talked about them in sessions with a therapist were less anxious or depressed. In addition, those who only wrote had a short-term increase in negative emotion, whereas those who expressed their feelings orally to a therapist did not show this effect. Research also indicates that self-disclosure may be beneficial for our physical health. For example, in one study, researchers contacted people who had lost a spouse through accidental death or suicide. They found that the more people had talked about the tragedy, the fewer health problems they had. Similarly, first-year students given the opportunity to write about the problems and emotions they experienced in leaving home and adjusting to college or university experienced fewer health problems and made fewer visits to the campus health center than those not given this opportunity. Burger, J. (2008). Personality (7th ed.). Belmont, CA: Wadsworth. Larson, D. G., & Chastain, R. L. (1990). Self-concealment: Conceptualization, measurement, and health implications. Journal of Social and Clinical Psychology, 9, 439–455. Student Project: Dibs and Play Therapy Virginia Axline, a student of Carl Rogers, has extended the client-centered approach to the treatment of children in play therapy. She has written Dibs: In Search of Self, a book that is extremely popular with students. Easily read in an evening, it can be assigned in preparation for class discussion of the humanistic therapies, and particularly of Rogers’ nondirective approach. Alternatively, you can have students write a paper identifying the important elements of client-centered therapy (e.g., active listening, genuineness, acceptance, empathy) used with Dibs. The more general humanistic themes of becoming aware of one’s feelings as they occur, of emphasizing conscious rather than unconscious material, of encouraging responsibility for one’s actions, and of promoting growth and fulfillment are also clearly evident in the book. Axline, V. (1964). Dibs: In search of self. Boston, MA: Houghton Mifflin. Classroom Exercise: The Imposter Phenomenon This exercise is appropriate for discussions of either humanistic or cognitive therapies. Fritz Perls has used the term “catastrophic fantasy” to refer to our tendency to deprive ourselves of present joy due to a largely un-conscious fear of being unmasked, that is, of being revealed as a fake and thus unworthy of the respect of those we love and admire. Clinical psychologist Joan Harvey has popularized findings on the imposter phenomenon (IP), a psychological syndrome based on intense, secret feelings of fraudulence in the face of success and achievement. In her book If I’m So Successful, Why Do I Feel Like a Fake?, she reports that a surprisingly large number of people in general, and approximately 70 percent of high achievers, suffer from the phenomenon. Many students are likely to experience “imposter” feelings. Handout 13–6 contains the Harvey Imposter Phenomenon Scale. In scoring their responses, students should reverse the numbers they circled for items 2, 4, 5, 7, 10, 11, and 14 (0 = 6, 5 = 1, 4 = 2, 3= 3, 2 = 4, 1 = 5, = 0 = 6). Then, they should add the numbers for all 14 items to obtain a final score. Total scores can range from 0 to 84. The higher the score, the more troubled one is likely to be by “imposter” feelings. Harvey provides many case studies of those suffering from IP. She opens her book with Leslie, a graphic designer. Leslie reports a feeling of fear, of always having the sense that she is not going to get the job done and that she’s not necessarily qualified to do it. In short, she feels she will not be able to give her employers what they want. Leslie states, “It creates a sense of panic in me that they’re going to find out I’m doing a terrible job and should be fired—and then I’ll never work again.” Harvey identifies three basic symptoms of IP: (1) the sense of having fooled other people into over-estimating one’s ability, (2) the tendency to attribute success to some factor other than one’s intelligence or ability, and (3) the fear of being exposed as a fraud. In recommending how to deal with IP sufferers, Harvey incorporates the goals and approaches of most of the psychotherapies discussed in the unit. For exam-ple, her suggestion to revise our ego ideal reflects the humanistic theme that we need to grow in self-under-standing and self-acceptance. Her advice to challenge our irrational beliefs—for example, that any mistake is a fatal flaw that must be camouflaged—suggests a cog-nitive approach. Change our thoughts, writes Harvey, and we change our feelings. Finally, she recommends tackling the IP by changing behavior. Her advice to relax, to change specific work patterns, and to reinforce ourselves when the goal is reached demonstrates princi-ples of classical and operant conditioning. Harvey, J. (1985). If I’m so successful, why do I feel like a fake? New York: St. Martin’s Press. C. Behavior Therapies (pp. 610–614) Feature Film: Harry Potter and the Prisoner of Azkaban Some clinicians have applauded this film’s central theme of overcoming fear by confronting it. In one memorable scene (DVD scene 10, at 32:00 minutes), the giant, good-natured Hagrid introduces Harry and his classmates to Buckbeak, a hippogriff. The large, menacing bird elicits immediate fear in everyone. All but Harry instinctively retreat. Harry hesitantly, inch-by-inch, approaches Buckbeak until he makes contact. Harry’s fear subsides only to be rekindled when Hagrid unexpectedly picks up Harry and places him on Buckbeak’s back. The bird takes off. Gliding above the trees, Harry’s apprehension is transformed into exhila-ration. At 37:45 minutes, they land safely and by then Buckbeak has become Harry’s friend. The scene mar-velously illustrates how exposure to what we fear can be therapeutic. In scene 11 (40:05 to 44:00 minutes), titled “Boggart in the Wardrobe,” the new Defense Against the Dark Arts teacher, Professor Lupin, teaches the stu-dents to visualize their worst fears and transform them into ridiculous, amusing portrayals. A giant spider is imagined wearing roller skates, the scary Professor Snape is morphed into a hunched-over grandmother in silly clothes, and a hissing snake is transformed into a gentle clown. Visualizing our fears as humorous and thus harmless can be helpful in the process of desensitization. Johnson, R. F. (2004, June 21). ‘Azkaban’ could have healing powers for kids’s fears. USA Today, p. 7D. Classroom Exercise: Using Systematic Desensitization to Treat Eraser Phobia Timothy Lawson and Michael Reardon describe a delightful classroom demonstration of systematic desensitization in treating a phobia of chalkboard erasers. You need a student volunteer from the back of the room who plays along with the exercise, and, ideal-ly, a photograph of a chalkboard eraser and a small cage in which you can lock a real eraser. Begin by reviewing the three major elements of systematic desensitization, including (1) the creation of an anxiety hierarchy that orders fear-producing stimuli from the lowest to highest, (2) the learning of the relax-ation response, and (3) the progressive association of each hierarchy item with relaxation. Explain that the therapist may accomplish this association by having the client imagine hierarchy items or by actually presenting the feared items. Often both strategies are used. Explain that your “client” has always sat at the back of the room because of a phobia of chalkboard erasers. Further, tell your class that you have already worked with him to develop an anxiety hierarchy, have taught progressive relaxation, and have desensitized him to a photograph of a chalkboard eraser. Show the class the photograph and move it toward the student to demonstrate that he has been desensitized. Explain that you now plan to desensitize him to items higher in the anxiety hierarchy. From under your desk produce a small metal cage with an eraser padlocked in it. Move it slightly in the direction of the student who should dis-play obvious anxiety. Ask him to take some deep breaths and invoke the relaxation response. Once he is relaxed in the presence of the padlocked eraser, remove it from the cage, and repeat the process. Move the eras-er closer and closer until, finally, the student can touch the eraser while remaining relaxed. At each step ask him if he is feeling anxious and move closer only after he reports his anxiety has subsided. End the demonstra-tion by noting that the student did not have real eraser phobia but that the technique is used in treating real phobias. You can give a longer demonstration by construct-ing an actual hierarchy along with a detailed description of how it was developed. Have the student volunteer report subjective units of discomfort at each step. You can also engage the class in a discussion of the relative merits of imagined, photographed, or actual fear stimuli. Finally, you may want to select the student volunteer a day or two before the actual exercise and coach him or her on how to respond to each step in the process. Lawson, T. J., & Reardon, M. (1997). A humorous demonstration of in vivo systematic desensitization: The case of eraser phobia. Teaching of Psychology, 24, 270–271. Student Project: Practicing Systematic Desensitization Students may practice systematic desensitization on themselves. First, they must identify a specific fear they would like to overcome—for example, the fear of taking tests. Next, they must construct an anxiety hierarchy. Handout 13–7, which is Jim Eison’s hierarchy for test anxiety, can be readily adapted by students to fit their own situation. Then, students must train themselves in progressive relaxation, as suggested by Anthony Grasha in Handout 13–8. It might be best for them to practice the procedure for a few days before combining relaxation with the steps of the anxiety hierarchy. Finally, they should try the actual desensitization procedure for 10 days. After relaxing, they are to imag-ine the first item in the hierarchy. If they feel no anxi-ety, they should proceed to the second step. If at any time they experience anxiety, they should switch off the mental image and go back to deep relaxation. A scene should be imagined over and over until they can feel completely relaxed while imagining it. Eventually, of course, they should practice the imagined behaviors in actual situations. You might have volunteers report back to class on their success. Eison, J. (1987). Using systematic desensitization and rational emotive therapy to treat test anxiety. In V. P. Makosky, C. C. Sileo, L. G. Whittemore, C. P. Landry, & M. L. Skutley (Eds.), Activities handbook for the teach-ing of psychology (Vol. 2, p. 162). Washington, DC: American Psychological Association. Grasha, A. (1987). Practical applications of psychology (3rd ed.). New York: HarperCollins. Lecture/Discussion Topic: Virtual Iraq Virtual reality exposure (VRE) therapy has been used to treat post-traumatic stress syndrome (PTSD). Virtual Iraq, developed by clinical psychologist Albert Rizzo, as reported by Sue Halpern, provides an excellent example. Victims of PTSD are often reluctant to under-go therapy because friends may see them as weak. In contrast, virtual reality therapy is often perceived as comparable to playing a video game. Telling buddies that you are going off to do VR is a lot easier than telling them you are going to see a shrink. Rizzo adapted the video game “Full Spectrum Warrior” to create his clinical tool. Virtual Iraq enables patients to work through their combat trauma in a computer-simulated environment. Similar to other virtual reality approaches, the intervention utilizes a head-mounted display (a helmet with a pair of video goggles), earphones, and a scent-producing machine. It requires the patient to revisit the trauma over and over again, and through eventual habituation rid it of its overwhelming power. The basic notion is to disconnect the memory from the painful reactions to the memory so that everyday events, such as a car backfiring or trash blowing across an expressway, no longer trigger fear or panic. Typically, there are 12 sessions in all, each lasting about 2 hours, over a 6-week period. In constructing Virtual Iraq, Rizzo began with two basic scenarios, an Iraqi street scene and a Humvee moving along an Iraqi highway. Therapists have a vari-ety of ways—visual, aural, tactile, even olfactory— to customize these basic scenes. At the click of a mouse, the therapist can put the patient in the driver’s seat of the Humvee, in the passenger’s seat, or in the turret behind the machine gun. The vehicle moves at a speed determined by the patient. A sandstorm can be raging (the driver can turn on the windshield wipers), a dog can be barking, the inside of the vehicle can smell rank. Giving the therapist so many options increases the like-lihood of evoking the patient’s actual experience. Engaging the patient on so many sensory levels allows for total immersion in the past experience. Trained therapists are crucial to the success of the intervention. New stimuli must be introduced gradually so that the experience is not overwhelming and thereby self-defeating. The therapist must understand the patient and know which stimuli to select and when to introduce them. Initially, a patient may only be able to sit in the Humvee. Rizzo claims that virtual reality exposure therapy for PTSD “is really intuitive. We provide a lot of options and put them into the hands of the clinician.” Currently, the Department of Defense is testing Virtual Iraq—one of three virtual-reality programs it has funded for PTSD—at six locations throughout the United States. Preliminary results from a relatively small sample suggest the intervention is effective. Halpern, S. (2008, May 13). Virtual Iraq. The New Yorker, 33–37. Lecture/Discussion Topic: Exposure Therapy— Improving Its Effectiveness Christopher Cain and his colleagues have studied fear extinction in mice, which may have important implications for the use of exposure therapy. In these techniques, with repeated exposure, people become less responsive to people, objects, or situations that once petrified them. The UCLA researchers taught mice to fear harm-less white noise by associating it with a mild shock delivered to the floor of the experimental cage. After only a couple of trials the mice “froze” for about 72 seconds, or 60 percent of the two minutes of white noise. The noise had come to function as a conditioned stimulus for fear. The researchers then separated the mice into three groups and assessed how easily they overcame their aversion to white noise when they heard it 20 times for two minutes each time without shocks. The groups differed only in the intervals between each 6, 60, or 600 seconds. Unlearning a fear typically takes much longer than acquiring it. Indeed, the mice feared the white noise after only two pairings with shock but needed far more than two exposures to overcome it. Nonetheless, Cain and his colleagues report that fear extinction occurred much more quickly when the time between stimulus presentations was relatively short. Indeed, the 6-second-gap mice stopped showing significant freezing after about 10 presentations of white noise, while the mice in the other two groups never really stopped freezing. “This very strong finding,” states co-author Mark Barad, “is already inspiring a search for a similar pattern of response in human anxiety patients. It’s part of a wave of important discoveries about fear extinction, findings that will transform both the practice of behav-ior therapy and the use of drugs as adjuncts to psychotherapy in the next few years.” Cain, C. K., Blouin, A. M., & Barad, M. (2003). Temporally massed CS presentations generate more fear extinction than spaced presentations. Journal of Experimental Psychology: Animal Behavior Processes, 29, 323–333. Lecture/Discussion Topic: Therapy and Totalitarian Control The behavior therapies—in particular, aversive conditioning—will have some older students conjuring up images of George Orwell’s 1984 and Stanley Kubrick’s film of A Clockwork Orange (available on DVD). In the latter, Alex, a young hoodlum, is appre-hended by police after a series of sexual and violent crimes. While in prison he volunteers for the “Ludoveck Treatment,” which presumably cures crimi-nals in a few weeks. Alex is injected with a drug that makes him violently ill; while under its influence, he is forced to view films that graphically portray sexual and aggressive actions. After repeated pairings of the conditioned stimulus (sexual and violent images) with the unconditioned stimulus (nausea-producing drug), sexual and violent thoughts come to make Alex extremely ill. Two points are worth making in regard to this fic-tional example. First, psychologists do not use aversive conditioning in this way. Typically, the client knows all about the procedure and consents to it. Moreover, its aim—for example, in the treatment of smoking or drinking—is toward increased self-control rather than control by others. Second, A Clockword Orange simpli-fies the situation. It overlooks the influences of cogni-tion. After treatment, Alex would know that sexual and violent actions would not induce illness. In short, peo-ple’s feelings and behavior cannot be so easily con-trolled as A Clockwork Orange implies. Classroom Exercise: Modeling You can extend the text discussion of the behavior therapies by explaining how therapists have used observational learning to help people overcome fears of snakes, spiders, and dogs. Nigel Barber describes a classroom demonstration in which modeling is used to reduce many students’ fear of a laboratory rat. Assuming that you have access to a laboratory rat and a transport cage, the demonstration can be an effective way to introduce the behavior therapies. It takes approximately 30 minutes. Begin by having students complete and score Handout 13–9, the Fear of Rats Scale (FRS). The total score is simply the sum of the ratings for all items, with higher scores reflecting greater fear. After students have completed the scale, have them turn the page over. Reveal the rat in its transport cage and give the following instructions. We now want to test your insight about rats. I want you to assess the age of the rat in days and write it on the back of your FRS. In order that everyone has a good chance to look at the rat, I want you to pass it around the room. When the cage has been passed to everyone and returned to you, make this additional request: Now I need the assistance of five volunteers to assess the friendliness of the rat. In order to do this, it is necessary to put your hand into the transport cage and pet the animal. Gloves are available for this purpose, if you wish to use them. If you wish to volunteer, please raise your hand. Barber suggests choosing both men and women volunteers to come forward and in full view of the class pet the rat until deciding on the animal’s level of friendliness. Have them then return to their desks and write the word volunteer on the back of their FRS. Also have them rate the rat’s friendliness on a 7point scale ranging from not friendly at all (1) to extremely friendly (7). Finally, have all students take and score the FRS again. Inform students that the purpose of the demonstration has been to show how modeling can be used in therapy. In participant modeling, the client is exposed to a feared object in the presence of the therapist and is encouraged to have contact with it. For example, a snake phobic approaches the snake and eventually handles it. This procedure is more effective than symbolic modeling in which the client merely observes an expert handling the snake. However, both strategies can reduce fear. Have students calculate whether their pretest and posttest FRS scores showed a decline in fear. A show of hands will confirm the effect. Collecting and analyzing the scores between class sessions will enable you to calculate and report whether participant modeling was more effective than symbolic modeling. Barber, N. (1994). Reducing fear of the laboratory rat: A participant modeling approach. Teaching of Psychology, 21, 228–230. Student Project: Modifying an Existing Behavior In Unit 6, we suggested a project in which students would modify some existing behavior. If you did not assign it then, you might do so now. It will not only demonstrate the application of operant conditioning but it will also show that the aim of behavior modification is often toward increased self-control rather than control by others. Classroom Exercise: Assessing Assertiveness An important behavior therapy is assertiveness training. Jim Eison designed Handout 13–10 to help students distinguish among assertive, nonassertive, and aggressive responses to common situations. He emphasizes that the test is designed simply to arouse student interest and to stimulate class discussion; reliability, validity, and normative data have not been collected. You might also ask students to devise their own assertive, nonassertive, and aggressive replies to the designated situations. Using the key below, students should tally the num-ber of nonassertive, aggressive, and assertive responses they gave to get some idea of their dominant style. Assertiveness training takes different forms. In Other forms of assertiveness training, the Broken some cases, the therapist models socially assertive Record and Fogging techniques, are sometimes used for behavior, then encourages the individual to practice the people who have difficulty denying requests. In the for-same behavior while the therapist provides feedback. the person is taught to deny a request, briefly This role-playing may also be practiced within a group explaining why, and then repeat the denial without variation each time the request is made. The film What Could I Say? (Research Press,. In the latter, the 18 minutes) presents 20 vignettes that illustrate com-person is taught to repeat in great detail every possible situations requiring assertive responses. After each reason for denying the request. scene, time is provided for viewers to discuss appropriate. People often worry that assertiveness will be per-ate responses. perceived as aggressiveness. A definition provided by Robert Alberti and Michael Emmons is useful in high-lighting the difference: “Assertion is behavior that enables a person to act in his own best interest and to stand up for himself without undue anxiety and to exercise his rights without denying the rights of others.” M. J. Smith has provided instructions to help people to be appropriately assertive and reduce the guilt they may feel about having been assertive. Note that these instructions reflect a bias (that self-interest comes first) and illustrate how values penetrate the recommendations of psychologists. You might ask students if they believe it’s always wise to follow them. The specific instructions appear in the right-hand column. I have the right to —say no —not do what someone, even someone close, asks me to do —enjoy myself —feel good about myself —not be responsible for other people’s problems —not do everything I can to help everyone —feel angry —be “illogical” —not care —not know the solution to a problem —change my mind —make mistakes —not pay forever for my mistakes Source: WHEN I SAY NO, I FEEL GUILTY by Manuel J. Smith, copyright © 1975 by Manuel J. Smith. Used by permission of Doubleday, a division of Random House, Inc. Eison, J. (1987). Assessing student assertiveness. In V. P. Makosky, C. C. Sileo, L. G. Whittemore, C. P. Landry, & M. L. Skutley (Eds.), Activities handbook for the teaching of psychology (Vol. 2, pp. 294–298). Washington, DC: American Psychological Association. Smith, M. J. (1975). When I say no, I feel guilty. New York: Doubelday. Yates, B. (1985). Self-management. Belmont, CA: Wadsworth Publishing Co. D. Cognitive Therapies (pp. 614–617) Lecture/Discussion Topic: Strategies to Correct One’s Thinking In The Feeling Good Handbook, David Burns, MD, a psychiatrist, suggests 10 ways to untwist the common cognitive distortions that typically underlie anxiety and depression. First, ask your students if they recognize any of the following cognitive distortions as their own. 1. All-or-nothing thinking: You look at things in absolute, black-and-white categories. 2. Overgeneralization: You view a negative event as a never-ending pattern of defeat. 3. Mental filter: You dwell on the negatives and ignore the positives. 4. Discounting the positives: You insist that your accomplishments or positive qualities “don’t count.” 5. Jumping to conclusions: (a) Mind reading—you assume that people are reacting negatively to you when there’s no definite evidence for this; (b) Fortune-telling—you arbitrarily predict that things will turn out badly. 6. Magnification or minimization: You blow things way out of proportion or you shrink their importance inappropriately. 7. Emotional reasoning: You reason from how you feel: “I feel like an idiot, so I really must be one.” Or “I don’t feel like doing this, so I’ll put it off.” 8. “Should statement”: You criticize yourself or other people with “shoulds” or “shouldn’ts.” “Musts,” “oughts,” and “have tos” are similar offenders. 9. Labeling: You identify with your shortcoming. Instead of saying “I made a mistake,” you tell yourself, “I’m a jerk,” or “a fool,” or “a loser.” 10. Personalization and blame: You blame yourself for something you weren’t entirely responsible for, or you blame other people and overlook ways that your own attitudes and behavior might contribute to a problem. Next, present Burns’ 10 suggestions for correcting the distortions. 1. Identify the distortion: Write down your negative thoughts so you can see which of the 10 cognitive distortions you’re involved in. This will make it easier to think about the problem in a more positive and realistic way. 2. Examine the evidence: Instead of assuming that your negative thought is true, examine the actual evidence for it. For example, if you feel that you never do anything right, you could list several things you have done successfully. 3. The double-standard method: Instead of putting yourself down in a harsh, condemning way, talk to yourself in the same compassionate way you would talk to a friend with a similar problem. 4. The experimental technique: Do an experiment to test the validity of your negative thought. For example, if, during an episode of panic, you become terrified that you’re about to die of a heart attack, you could jog or run up and down several flights of stairs. This will prove that your heart is healthy and strong. 5. Thinking in shades of gray: Although this method might sound drab, the effects can be illuminating. Instead of thinking about your problems in all-or-nothing extremes, evaluate things on a range from 1 to 100. When things don’t work out as well as you had hoped, think about the experience as a partial success rather than a complete failure. See what you can learn from the situation. 6. The survey method: Ask people questions to find out if your thoughts and attitudes are realistic. For example, if you believe that public-speaking anxiety is abnormal and shameful, ask several friends if they ever felt nervous before they gave a talk. 7. Define terms: When you label yourself “inferior” or “a fool” or “a loser,” ask, “What is the definition of ‘a fool’?” You will feel better when you see there is no such thing as “a fool” or “a loser.” 8. The semantic method: Simply substitute language that is less colorful and emotionally loaded. This method is helpful for “should statements.” Instead of telling yourself “I shouldn’t have made that mistake,” you can say, “It would be better if I hadn’t made that mistake.” 9. Re-attribution: Instead of automatically assuming that you are “bad” and blaming yourself entirely for a problem, think about the many factors that may have contributed to it. Focus on solving the problem instead of using up all your energy blaming yourself and feeling guilty. 10. Cost-benefit analysis: List the advantages and disadvantages of a feeling (like getting angry when your plane is late), a negative thought (like “No matter how hard I try, I always screw up”), or a behavior pattern (like overeating and lying around in bed when you’re depressed). You can also use the cost-benefit analysis to modify a self-defeating belief such as, “I must always try to be perfect.” Burns, D. (1999). The feeling good handbook (Revised Ed.). New York: Plume. Classroom Exercise: Frequency of Self-Reinforcement Questionnaire To complement and extend the text treatment of cognitive therapy, you may want to introduce students to the concept of self-reinforcement and its importance in pre-venting and overcoming depression. Handout 13–11 is Elaine Heiby’s Frequency of Self-Reinforcement Scale (FSRS). Students should score one point for a “True” response to items 1, 2, 4, 7, 10, 12, 14, 17, 18, 19, 20, 24, 25, 26, and 29 and one point for a “False” response to 3, 5, 6, 8, 9, 11, 13, 15, 16, 21, 22, 23, 27, 28, and 30. Total scores can range from 0 to 30, with higher scores reflecting a greater tendency to engage in self-reinforcement. The mean score for undergraduates is about 17. According to Heiby there are at least two important reasons that people may engage in a low level of self-reinforcement and be depressed. First, they may set unrealistically high goals for themselves; that is, they have aspirations beyond any hope of attainment. Second, they may fail to attend to or discriminate a tar-get response when it occurs; that is, they fail to acknowledge success. Research has indicated that self-reinforcement training can be an effective treatment for depression. Heiby, E. (1983). Assessment of frequency of self-reinforcement. Journal of Personality and Social Psychology, 44, 1304–1307. Lecture/Discussion Topic: Overcoming the Fear of Public Speaking Survey research indicates that the greatest fear of most Americans is speaking before a group. Michael Motley’s practical advice not only may help your stu-dents in dealing with their own phobia of public speak-ing, but it can also be used to introduce the cognitive therapies. Motley’s recommendations assume that feel-ings and responses to events are strongly influenced by thinking. The most familiar aspects of speech anxiety are its physical symptoms—sweaty palms, dry mouth, increased heart rate, butterflies in the stomach. A more important aspect of speech anxiety, notes Motley, is how we interpret the anxiety. Some people view the physical symptoms as a positive sign that they are emo-tionally ready for the speech. Most of us, however, interpret the feelings as fear. To justify our fear we begin to imagine horrible consequences if our speech is less than perfect: “The audience will ridicule me if I make a mistake. I’ll be embarrassed to death.” Motley argues that such beliefs are irrational, because audi-ences usually ignore errors and awkwardness as long as they get something out of the speech. Research has also found that most people report noticing little or no anxi-ety in a speaker. Indeed, there is little relationship between the evaluations of individuals trained to detect anxiety cues and the degree of anxiety actually felt by the speakers. Excessive anxiety, reports Motley, is especially common when a speech is viewed as a performance. Expecting to be evaluated or being uncertain about the proper way to behave arouses anxiety in almost any situation. A more useful and accurate orientation is to view speeches as communication, the sharing of ideas with others who are more interested in the content of the message than in analyzing or criticizing its presentation. Speech making should thus be viewed as a form of everyday conversation. Motley has a simple exercise to help students view public speaking in this new way. As the student speaker approaches the podium, Motley dismisses the audience temporarily and begins a conversation with the speaker. He instructs him or her to forget about giving a speech and simply talk spontaneously, using prepared notes as a guide. Most students follow his lead, speaking conversationally and without oratorical flair. They are then told to maintain the conversational style while the audience gradually returns, a few at a time. Motley gives these specific tips for speakers. 1. Decide on your specific objectives first. Know one or two major points you want to communicate. 2. Put yourself in your audience’s place. Speak to them on their terms, in their language. 3. Don’t memorize, don’t read. Except for a few memorable phrases or examples, be as spontaneous as possible. Use brief notes. 4. Speak to one person at a time. Looking at and talking with individuals in the audience helps keep you natural. 5. Try not to think about your hands and facial expressions. Concentrate instead on what you want to get across. Conscious attention to gestures leads to awkwardness. 6. Take it slow and easy. 7. Speak the way you talk. Speak as you do in casual conversation with someone you respect. 8. Ask for advice and criticism. Solicit frank criticism from someone you trust, focusing on what might have prevented you from accomplishing your objectives. Motley summarizes: “For most of us, giving a speech is an important and novel event. It’s natural and appropriate to feel some anxiety. A speaker’s aim should be to keep this natural nervousness from cycling out of control: not to get rid of the butterflies but to make them fly in formation.” At Georgia State University, psychologist Page Anderson is using virtual reality exposure therapy (VRE) to help people overcome public speaking phobia. Anderson intends to compare the efficacy of VRE with cognitive behavioral therapy. For those learning to over-come their fear of public speaking, Anderson’s virtual audience will be able to raise their hands and ask questions. VRE has been used primarily to help clients over-come fears of flying, heights, and, in some cases, animals. It is less commonly used in addressing interpersonal fears. Motley, M. (1988, January). Taking the terror out of talk. Psychology Today, 46–49. Tricoles, R. (2004, November 10). Head games: High-tech gear helps conquer fears. Message posted at www.gsu.edu/gastate_2200.html. Student Project: Mood-Memory Repair You can extend the text discussion of cognitive therapy for depression with a more detailed discussion of mood memory repair. In his helpful book Memories That Matter: How to Use Self-Defining Memories to Understand and Change Your Life, psychologist Jefferson Singer describes the research that underlies using mood memory repair in treating depression and then provides readers with specific strategies for applying it to their own lives. Mood memory repair recognizes that our memories are mood-congruent. As Myers notes in Unit 7A, Memory, our moods bias our recall of the past. We seem to associate good or bad events with their accompanying emotions, which in turn become retrieval cues. Being depressed sours our memories by priming negative associations, which we then use to explain our cur-rent mood. Similarly, being in a positive mood leads us to recall the world through rose-colored glasses. Our mood’s effect on retrieval helps explain why moods persist. Research on mood and memory, Singer argues, indicates that we can become mood repairers by (1) keeping our mental and physical energy at good, healthy levels; (2) arranging our immediate physical environment in ways that make it easier to access positive, specific memories; (3) taking steps to increase our store of positive memories filled with specific images and concrete evidence of the good things in our lives; (4) distracting ourselves from worries and negative thoughts; and (5) after we have broken the worry cycle, focusing on the positive aspects of our current experiences. To break depression’s vicious cycle or merely to raise our experience of well-being, Singer makes the following specific recommendations in his “mood-memory repair kit”: 1 Mood-memory makeover list: Survey the room in your residence hall, apartment, or home where you spend the most time for any objects that evoke negative memories—for example, photos, jewelry, cosmetic items, sports equipment. Replace them with comparable items that evoke positive memories. 2 Go-to memories: Recall five of your happiest memories. Visualize and savor these experiences until they become “go-to memories” that can be counted on to lift your spirits when they begin to sag. 3 Lemons-into-lemonade memories: Identify two strong negative memories. Try to identify positive aspects of both memories. For example, if it is memory of a past failure, think of how it may have redirected your life in some constructive way. If it is recall of a broken relationship, think of how it led to the formation of new friendships. 4 Positive distracting activities: Unhappy, depressed people often find that breaking the focus on them-selves is the healthiest antidote to the ruminating blues. Identify positive activities that fit your schedule and are both economical and convenient—making bread with friends, attending a movie or concert, or simply some enjoyable physical exercise—that can become ready distractions when you begin to worry. Don’t make this too complex. Start with one activity and when you build it into your routine, add a second or third. These four steps are crucial. Additional steps, what Singer calls “mood accessories,” include developing some surefire pick-me-up lines or key phrases that prime positive thoughts, such as “Remember the . . .” (a past positive experience), using the don’t-go-there rubber band (they do come in different colors!), and, finally, making “nose candy” readily available, that is, favorite smells that trigger favorite memories from your childhood (e.g., popcorn, hot dogs, perfumes, body washes, scented candles). Challenge students to follow Singer’s recommendations and report their impact either in writing or in an oral report to the class. If your students do this for even a few days or a week, they will surely come to a better understanding and appreciation of the cognitive-behavioral approach. Singer, J. (2005). Memories that matter: How to use self-defining memories to understand and change your life. Oakland, CA: New Harbinger. E. Group and Family Therapies (pp. 617–618) III. Evaluating Psychotherapies (pp. 619–628) A. Is Psychotherapy Effective? (pp. 619–622) PsychSim 5: Mystery Therapist Students should work this activity after they have read about the basic psychotherapies, and you have lectured on them. The activity reviews the major perspectives on psychological disorders and therapy and presents an interactive exercise in which students read brief fragments of case studies and are asked to identify the type of therapy exemplified in each case. Lecture/Discussion Topic: The Consumer Reports Study The November 1995 issue of Consumer Reports (CR) reported survey results on the effectiveness of psychotherapy. CR’s 180,000 readers had been asked to fill out the mental health section of a much longer survey “if at any time over the past three years you experienced stress or other emotional problems for which you sought help from any of the following: friends, relatives, or a member of the clergy; a mental health professional like a psychologist or a psychiatrist; your family doctor; or a support group.” Twenty-two thousand readers responded to the entire survey; of these, approximately 7000 completed the mental health section. Of these 7000, about 3000 had just talked to friends, relatives, or clergy and about 4000 had turned to some combination of mental health professionals, family doctors, and support groups. Of the 4000, a total of 2900 saw a mental health professional. As a whole, the respondents were well-educated and predominantly middle-class. About half were women and the median age of the sample was 46. Among the most important results were the following: • Psychotherapy helped 9 out of 10 patients feel significantly better. Almost half (44 percent) who reported their emotional health as having been very poor now reported feeling good. • Those in psychotherapy more than six months did the best. Long-term treatment was considerably more effective than short-term treatment. • Psychotherapy alone did not differ in effectiveness from medication plus psychotherapy. • No specific form of psychotherapy did better than any other for any disorder. • Psychologists, psychiatrists, and social workers did not differ in their effectiveness as treaters, but they all did better than marriage counselors and long-term family doctors. Martin Seligman contrasts the Consumer Reports large-scale survey study with the more traditional efficacy studies in psychology in which patients are randomly assigned into specific treatment groups of fixed duration. He argues that the studies complement each other and that both contribute to our understanding of the effectiveness of psychotherapy. In a more recent survey of 3079 readers, CR com-pared drug therapy with psychotherapy. Focusing on the disorders of depression and anxiety, the organization reported that a combination of “talk” therapy and drugs often proved most effective. CR concluded that each therapy worked at a different pace, with those taking drugs showing substantial improvement within a few visits. Those who chose mostly talk therapy improved more gradually. However, talk therapy was almost as effective as the combination if it lasted for 13 or more visits. (In the 1995 survey, respondents averaged well over 20 visits with a mental health professional; in the current survey, the average was 10 visits—a troubling trend, notes CR.) Although drugs worked more quickly, it often took trial and error to find one that did not have unacceptable side effects. For example, 40 percent of those who took antidepressants complained of adverse sexual side effects. CR also reported that primary-care doctors were effective in treating people with mild problems, but mental health specialists produced significantly better results for those with more serious disorders. Those respondents who expressed greatest satisfaction with their care and who had the best outcomes were more likely to: • Research their problem before seeking help. • Interview with more than one professional. • Ask therapists if they had experience treating their problem. • Bring a friend or family member along to an office visit. • Keep a written record of their treatment and emotional state. • Deliberately apply what they were learning in treatment to their daily lives. Not surprisingly, CR concluded that the last step was the best predictor of a favorable outcome. Only 1 percent of respondents followed all these steps; 18 per-cent followed none. Drugs vs. talk therapy. (2004, October). Consumer Reports, 22–29. Mental health: Does therapy help? (1995, November). Consumer Reports, 734–739. Seligman, M. E. P. (1995). The effectiveness of psychotherapy: The Consumer Reports study. American Psychologist, 50, 965–974. Lecture/Discussion Topic: Fringe Medicine The text discusses the difficulty of answering the question, “Is psychotherapy effective?” Clients and clinicians alike may have biased perceptions and hence selective and biased recall. Most people also tend to make judgments that confirm their beliefs. Thus, as the text notes, “alternative therapies can spread like wild-fire.” You can extend the discussion in class to a consideration of why many people believe in the effectiveness of any therapy, whether it’s for a psychological or physical problem. Karl Sabbagh’s analysis of “fringe medicine” supports the text’s argument that we need controlled research studies to assess the effectiveness of therapy. Practitioners of the fringe therapies (among them psychic healing, homeopathy, acupuncture) make exorbitant claims, which are simply not supported by careful research. Still, people continue to believe. A study by the U.S. Department of Health and Human Services indicated that 27 percent of U.S. adults have used one or more of these questionable health treatments at some point in their lives. In fact, report researchers, almost one-third of college or university graduates have tried at least one such treatment. For example, people have used snake venom and bee venom as cures for arthritis (they have actually put bees on themselves and been stung). The practice is based on the premise that some venoms reduce inflammation. One critic suggests that people believe in it because “anything feels better” once the bees stop stinging. A defender of the “therapy” explained the practice: Bees don’t get arthritis. Of course, responded the critic, “Bees don’t have joints.” Most obviously, people believe in fringe medicine because they want to. In response to the statement, “When you have a serious health problem, it’s worth trying almost anything,” 26 percent strongly agreed and 24 percent agreed somewhat. As an example of how fringe medicine works, Sabbagh describes Emil J. Freireich’s tongue-in-cheek “Experimental Plan,” which enables anyone to set him-or herself up as a therapist and is “guaranteed to pro-duce beneficial results.” The plan has two essential requirements. The first is a treatment of some sort; it doesn’t matter what. It can be a form of psychotherapy or some physical procedure, a type of rubbing or hand-waving or the administration of a drug, plant, or chemical. The second requirement is that the treatment be absolutely harmless. Freireich shows how any such fringe technique can lead to an outcome confirming its success. The crucial factor is the natural variability of all disease. Every disease has important periods of remission in which the patient feels better. This is true even when there is an inexorable trend downward. Guided by this principle, Freireich recommends that treatment be applied only after a period in which the patient has been getting progressively worse. If treatment is applied during one of the “ups” and the patient continues to improve, he or she can always say improvement would have occurred anyway. If the treatment is applied when the patient is getting worse, there are four possible outcomes: (1) The patient could improve, given the natural variability of the illness. Such an outcome immediately “proves” the treatment is effective. (2) The disease may remain stable, proving that the treatment has arrested the problem. (3) The patient may continue to get worse, which merely means the dosage was inadequate and must be increased. (4) The patient may die. In this case, the treatment was obviously delayed too long and applied too late. When a patient improves, one must reduce the treatment. Two possible outcomes will again “prove” the effectiveness of the therapy. If the patient continues to improve, the treatment was obviously effective. If he or she gets worse, reducing the treatment has obviously made the disease active again. Ruffenach, G. (1988, May 27). Unproven remedies tempt the ailing. The Wall Street Journal, p. 15. Sabbagh, K. (1985–1986). The psychopathology of fringe medicine. The Skeptical Inquirer, 10, 154–158. Lecture/Discussion Topic: Regression Toward the Mean The phenomenon of regression toward the mean was first noted by Sir Francis Galton in the nineteenth cen-tury. He observed that in any series of random events clustering around an average, an extraordinary event is, by mere chance, most likely to be followed by an ordi-nary event. Thus, very tall fathers are likely to have slightly shorter sons and very short fathers, somewhat taller sons. Regression toward the mean helps explain why great movies are often followed by poor sequels, why poor presidents often have better successors, and why extremely intelligent women tend to have slightly duller husbands. Paul Schaffner provides an excellent example of regression toward the mean that you can present in class. Participants in his study assumed the role of a teacher attempting to encourage a hypothetical student to arrive promptly for an 8:30 A.M. class. The student’s arrival time, which varied from 8:20 to 8:40 for 15 con-secutive days, was recorded on a computer. Each day the teachers could choose to praise, reprimand, or say nothing to the student. As expected, they praised him when he was early and reprimanded him when he was late. Unknown to the teachers, the student’s arrival time was preprogrammed and thus unrelated to the teacher’s response of the previous day. Due to regression alone, the student’s arrival time tended to improve, that is, regress to 8:30, after being punished for being late and to deteriorate (again by regressing to 8:30) after being praised for arriving early. Schaffner found that 70 per-cent of his teachers concluded that reprimand was more effective than praise in producing prompt attendance by the student. Regression toward the mean operates with regularity in sports, particularly when luck is mixed with skill. While sports commentators recognize its effect, they often offer different explanations. Amos Tversky notes, “Listen to the commentators at the Winter Olympics. If a ski jumper has done well on his last jump, they say, ‘He’s under immense pressure, so he’s unlikely to do as well this time.’ If he did poorly, they say, ‘He’s very loose and can only improve.’” Perhaps the so-called “Sports Illustrated Jinx” can also be understood in terms of regression toward the mean. According to sports folklore, the “Sports Illustrated Jinx” dooms teams or athletes appearing on the cover to lose after they are featured. For example, Earvin “Magic” Johnson of the Los Angeles Lakers graced the cover when his team was leading the NBA championship series. The Lakers then lost the title to the Boston Celtics in seven games. Similarly, the New York Islanders were on the cover going for their fifth straight Stanley Cup. They lost four straight to Edmonton. Tennis players and golfers seem to suffer the most after appearing on the cover. Researchers Tim Leone and Robbie Gluckson found that the perform-ance of these athletes fell off more than 83 percent of the time. The performance of swimmers, skiers, foot-ball rushers, and crew members also dropped off significantly after cover appearances. At the same time, the researchers found that baseball pitchers and teams, as well as basketball players and teams (“Magic” Johnson being one exception), did well more than 70 percent of the time after they were on the cover. Several observers have noted that athletes appear on the cover only after performing unusually well. Regression toward the mean would explain their poorer subsequent performance. McKean, K. (1985, June). Decisions, decisions. Discover, 22–31. Schaffner, P. (1985). Specious learning about reward and punishment. Journal of Personality and Social Psychology, 48, 1377–1386. Staff. (1984, July 14). Sports Illustrated cover no jinx, say researchers. The Grand Rapids Press, p. B7. Classroom Exercise: Regression Toward the Mean and Aspiration Level Jerry Karylowski suggests a simple classroom demonstration of regression toward the mean, which will work with students having no statistical background. Tell students that they will serve as your research assistants in a study of aspiration level, a relatively stable personality trait. Briefly explain how both very low and very high aspiration levels are maladaptive. Also tell them that you believe you have a special psychic ability that has a therapeutic influence on those whose aspiration levels are too high or too low. Then explain that although there are many ways to measure aspiration levels, none will be perfect. A test score will always be a function of at least two components: (1) the true score and (2) a combination of transient factors, such as the person’s mood, the person’s misunderstanding of some items, clerical errors in scoring, and so on. To illustrate, ask each student to think of three or four individuals they know well. A 6-point scale will be used to test the participants’ aspiration levels; scores 1 and 2 will indicate a tendency for aspirations to be lower than ability, scores 3 and 4 will indicate an appropriate aspiration level, and scores 5 and 6 will suggest an unrealistically high aspiration level. Testing will proceed in the following way: First, each participant will be assigned a true score on the basis of any information or intuitions students have about him or her. Second, each participant will be assigned a transient-factors score based on die tossing (or a number drawn out of a hat). Finally, assuming that true and transient scores are weighted equally, an average of the two will be the simulated test score. After students have identified their research participants and obtained the simulated test scores, create a distribution of all scores (they will range from 1 to 6) on the chalkboard. Select two extreme groups, the top 10 or 25 percent, and the bottom 10 or 25 percent. The top scores will be your highaspiration group, the bottom scores your low-aspiration group. Have students note the scores, perhaps even calculating separate means for the entire distribution and for each of the extreme groups. Announce that one day has passed since you applied your psychic treatment and that students are not to “retest” participants that fall into the extreme groups. Tell them that unless they believe in your psychic power, they should use the same true scores. Transient-factors scores, however, are to be assigned on the basis of a new round of die tossing. Finally, tabulate the post-treatment results for both the low-aspiration and the high-aspiration groups. Students will immediately see the regression toward the mean. The post-treatment test scores for the high-aspiration group will be lower and those for the low-aspiration group will be higher. Karylowski, J. (1985). Regression toward the mean effect: No statistical background required. Teaching of Psychology, 12, 229–230. Lecture/Discussion Topic: Thinking Errors and Clinical Judgment David Myers has described how the judgments of psy-chiatrists and clinical psychologists about the success of therapy may reflect common errors in thinking. Consideration of these errors not only stimulates stu-dents to think critically about the clinical process but also serves to reinforce material from Units 2 and 7B. A common error made by clinicians involves illu-sory correlations. Experiments conducted by Loren and Jean Chapman found that professional clinicians per-ceived expected associations—for example, between particular responses to Rorschach inkblots and homo-sexuality—even when the expected associations were absent. When we believe a relationship exists, we are more likely to notice confirming than disconfirming instances. Clinicians’ judgments may also be contaminated by the hindsight bias and overconfidence. For example, if a friend commits suicide, a common reaction is to think we should have been able to predict and therefore to prevent the suicide. In retrospect, we can see the pleas for help. Thus, after a tragedy, the hindsight bias can leave therapists feeling guilty. Conversely, Lee Ross and his colleagues have shown how such hindsight explanations might exaggerate a clinician’s self-confidence. In one experiment, Ross had participants read clinical case histories of people who, they were told, had committed suicide. They were then asked to use the case history to explain the event. Later they were informed that there actually was no available information on how the patient’s life ended. When asked to estimate the likelihood of several possible events, including the “suicide” they had explained, suicide now seemed quite likely. The mere activity of explaining and interpreting (which clinicians are engaged in constantly) may itself contribute to overconfidence in one’s judgments. (Remind students of the beliefperseverance phenomenon described in Unit 7B: The act of explaining and defending a belief enables one to understand how it might be true and thus to continue to believe it even when the data that inspired it are discredited.) Clients are also readily induced to give information that fulfills their clinicians’ expectations. In short, clinicians’ judgments may reflect a self-fulfilling prophecy. Mark Snyder and William Swann found, for example, that interviewers who questioned people to see if they had a particular trait treated them as if they had it. The questions selected to test for extraversion could not have been better calculated to elicit extraverted answers (“What would you do to liven things up at a party?”). Similarly, people tested for introversion were asked questions that necessarily elicited introverted answers (“What factors make it hard for you to open up to people?”). As a result, and as expected, targets being tested for extraversion described a more outgoing self, and those tested for introversion revealed a more reserved self. Additional research found that those asked “extraverted” questions not only later perceived them-selves as more extraverted but actually became notice-ably more outgoing. Myers, D. G. (2008). Social psychology (9th ed.). New York: McGraw-Hill. Lecture/Discussion Topic: Therapy and the Nature of the Problem The text concludes that therapy is most effective when the problem is specific. Those who suffer phobias can hope for improvement; those who want to change their whole personality are unlikely to benefit from psychotherapy alone. Martin Seligman’s What You Can Change and What You Can’t examines the degree to which various problems, personality types, and patterns of behavior are responsive to intervention. From those that are easiest to those most difficult to change, Seligman suggests this continuum: panic (curable), specific phobias (almost curable), sexual dysfunctions (marked relief), social phobia, agoraphobia, depression, and sex role (all moderate relief or change), obsessive-compulsive disorder and sexual preferences (moderate/mild relief or change), anger and everyday anxiety (mild/moderate relief), alcohol dependency (mild relief), overweight (temporary change), post-traumatic stress disorder (marginal relief), sexual orientation (probably unchangeable), and sexual identity (unchangeable). According to Seligman, what is changeable varies with the depth of the problem. Depth has biological, evidentiary, and power aspects. To the degree that a problem has biological underpinnings because it is predisposed or heritable, it will be harder to change. To the degree it is a learned habit, it is easier to change. As the text indicated earlier, we may be more biologically prepared to fear some objects such as animals or insects because they presented threats to our ancestors. Such fears will be harder to extinguish. Bipolar disorder, argues Seligman, may also be highly heritable because the cycling of energy with the sea-sons, from summer activity to winter hibernation, has an evolutionary basis. The evidentiary aspect of a disorder deals with how easy or difficult it is to get evidence for the belief underlying the problem as well as how difficult it is to get evidence that will disabuse one of the belief. For example, the belief underlying post-traumatic stress disorder—that the world is a miserable, unfair place—is easy to confirm. One only needs to read the front page of the daily newspaper. Similarly, the thought underlying obsessive-compulsive disorders—for example, “I will die if I don’t wash my hands five times before eating”—necessarily leads us to perform the ritual and we will never discover disconfirming evidence. The easier a belief underlying a problem is to confirm and the more difficult it is to disconfirm, the harder it will be to change. Finally, the power of a belief refers to how many facts it explains. A theory has low power if it explains only a few isolated beliefs. For example, the belief that robins are very dangerous is of low power. On the other hand, a belief has high power if it makes sense of a great deal of our world. The belief that I am an unlovable person or that I need to drink to get through the day has high power. To the degree that a belief underlying a problem has high power, it will be harder to change. Seligman, M. (1994). What you can change and what you can’t. New York: Knopf. B. The Relative Effectiveness of Different Therapies (pp. 654–655) Lecture/Discussion Topic: Writing About Emotional Experiences as Therapy In reviewing the success of many forms of psychotherapy, James Pennebaker suggests that the mere act of disclosure may be a powerful therapeutic agent. Research indicates that writing about personally upsetting experiences produces consistent and significant health benefits (see also Unit 8B). Typically, participants are to asked to write for three to five consecutive days, 15 to 30 minutes each day in response to these instructions: For the next 3 days, I would like you to write about your very deepest thoughts and feelings about an extremely important emotional issue that has affected you and your life. In your writing, I’d like you to really let go and explore your very deepest emotions and thoughts. You might tie your topic to your relationships with others, including parents, lovers, friends, or relatives; to your past, present, or your future; or to who you have been, who you would like to be, or who you are now. You may write about the same general issues or experiences on all days of writing or on different topics each day. All of your writing will be completely confidential. Don’t worry about spelling, sentence structure, or grammar. The only rule is that once you begin writing, continue to do so until your time is up. Pennebaker notes that the writing paradigm has been powerful for all age groups and ability levels. Essays reflect a range of traumatic experiences, including lost loves, deaths, and sexual and physical abuse. Given the opportunity, people disclose deeply personal aspects of their lives, and the vast majority report that the writing experience was valuable and meaningful in their lives. Findings have indicated that the disclosure is associated with significant drops in physician visits, improvement in immune function, and positive changes in autonomic and muscular activity. Behavioral changes include improvement in grades, faster reemployment following job loss, and lower rates of absenteeism. Self-reports indicate reductions in distress, negative affect, and depression. This research provides several other interesting findings: There were no differences as a function of personality, sex, education, or ethnic background. Writing once each week over a month may be more effective than writing four times within a single week. Talking into a microphone and writing seem to produce comparable effects. Talking and writing about emotional experiences are both superior to writing about superficial topics. Most interesting is the finding that social feedback seems unnecessary to produce ben-eficial results. Essays may be placed in an anonymous-looking box with the promise that they will not be linked to their names or even written on a “magic pad” (whereby the writing disappears when the person lifts the plastic writing cover). Two major explanations have been offered for the positive effects of writing. The first theory is that not disclosing important psychological phenomena is a form of inhibition. Letting go and talking about traumatic experiences reduces the stress of inhibition. The second explanation that receives support from more recent research is that writing probably does more than reduce inhibition. It may produce changes in basic cognitive and linguistic processing that prove therapeutic. For example, analyses of the essays indicate that three linguistic factors predict improved health. First, the more the individuals used positive emotion words, the better their subsequent health. Second, a moderate number of negative emotion words predicted health. Both very high and very low levels of negative emotion words correlated with poorer health. Third, and it seemed most important, an increase in both causal and insight words over the course of writing was strongly associated with improved health. It seemed that people who benefited from writing began with poorly organized descriptions and progressed to coherent stories by the last day of writing. Among the research questions to be answered is whether a story can ultimately result in the assimilation of an unexplained experience, thereby allowing the person to get on with life. Lyubomirsky, S., Sousa, L., & Dickerhoof, R. (2006). The costs and benefits of writing, talking, and thinking about life’s triumphs and defeats. Journal of Personality and Social Psychology, 90, 692–708. Pennebaker, J. W. (1997). Writing about emotional experiences as a therapeutic process. Psychological Science, 8, 162–166. Lecture/Discussion Topic: Psychological Treatments Versus Psychotherapy In 2001, David Barlow observes, psychology formally identified itself as a health care profession and codified this change in the bylaws of the American Psychological Association. At the same time, Barlow notes, there have been a number of obstacles to the inclusion of psychologists in health care systems. These include stigma against treating the psychological aspects of physical disorders, a strong emphasis on increased use of pharmacological treatments for most mental disorders, and questions regarding the effectiveness of psychological interventions in chronic conditions. However, in the last decade, research evidence shows that a new generation of powerful psychological interventions are as effective, or even more so, than popular medical approaches in the treatment of specific disorders. Drawing from studies in the prestigious New England Journal of Medicine (NEJM) and the Journal of the American Medical Association (JAMA), Barlow notes that, in some cases, psychological treatments have proven more successful than medication or routine medical care in treating: • • • • • stress incontinence in women insomnia Gulf War veterans’ illnesses panic disorder depression and physical health in patients with Alzheimer’s (delaying institutionalization) In each case, the psychological treatments were specifically tailored to the problem at hand and took into account the patients’ specific characteristics and settings. For example, when compared with standard medical care, a carefully crafted home-based exercise program coupled with caregiver training in behavioral management both delayed institutionalization and improved depression in people with Alzheimer’s. Similarly, compared with a pharmacological approach to treating insomnia in older adults, a specially designed program that combined cognitive therapy with sleep restriction and sleep hygiene better sustained sleep improvement. Most often, these interventions have emerged from research in cognition and learning along with strong input from the study of social psychology and interpersonal processes. Data suggest that these proven strategies require considerable clinical expertise, especially for helping the more severely ill patient. Barlow persuasively argues that in order to promote faster and more widespread dissemination of these interventions and to solidify the identification of psychology as a health care profession, we should label the approaches as psychological treatments. This would distinguish them from more generic psychotherapy that is practiced by a variety of professionals and nonprofessionals. Because in-depth training in cognitive and behavioral science and social and interpersonal processes is critical to the use of these more sophisticated treatments, Barlow contends that a doctorate in psychology and a license are the sine qua non for the administration of these treatments, much as a doctoral degree and license in medicine are required to administer medical treatments for physical diseases. Barlow, D. H. (2004). Psychological treatments. American Psychologist, 59, 869–878. C. Evaluating Alternative Therapies (pp. 655–657) Lecture/Discussion Topic: Pets in Therapy Ask your students: What effect does your pet have on your psychological well-being? Social workers and physical therapists have used “animal-assisted” therapy for many years. Now a few psychologists have also begun using animals in therapy (see the Close-Up in text Appendix C, p. C-5). Previous research has found a positive relationship between pet ownership and well-being among children, people with disabilities, and senior citizens. University of California, Los Angeles, psychologist Judith M. Siegel and her research team reported that pets may also provide a buffer against depression for men suffering from AIDS. They surveyed more than 1800 gay and bisexual men in three U.S. cities who were participants in the long-term Multicenter AIDS Cohort Study con-ducted to track the AIDS epidemic. Almost 40 percent of the men surveyed were HIV-positive and more than 10 percent had developed AIDS. Results indicated that AIDS-infected men without pets were three times more likely to report depression than men without AIDS. However, AIDS-infected men who owned pets were only 50 percent more likely to suffer from depression. The benefits of pet ownership were greatest for those who had few confidants but had a close relation-ship with their pets (e.g., sleeping in the same room). Siegel explains that pet ownership helps reduce the isolation that can accompany AIDS. “Not only is AIDS often a stigmatizing condition, but many of these men lose friends and companions, too,” she observes. “The attachment and tactile comfort that a pet provides can reduce feelings of stress and loneliness.” Murray, B. (1999, September). Pet ownership provides buffer against depression for AIDS-infected men. APA Monitor, 6. Siegel, J. M., Angulo, F. J., & Detels, R.,Wesch J., & Mullen A. (1999). AIDS diagnosis and depression in the Multicenter AIDS cohort study: The ameliorating effect of pet ownership. AIDS Care, 11, 157–170. Lecture/Discussion Topic: Trepanation A more extreme form of alternative therapy than those described in the text is trepanation, the ancient practice of drilling holes into the skull. Proponents claim it increases the volume of blood to the brain that in turn fosters awareness, energy, and well-being. “More blood is available, and parts of the brain come into function that were undernourished and starving,” claims Peter Halvorsen, a Pennsylvania jeweler credited with introducing Americans to the practice through his Web site at www.trepan.com. “They wake up, and feel, ‘Oh, I’m taking in new data. There is a sensory world out there that is neat.’” A clinic in Monterey, Mexico, performs the operation for $2500, including MRI scans and a follow-up examination. Performed solely on the skull bone, trepanation does not include puncture of the brain. The procedure leaves about a 14-mm hole in the head that is eventually closed with scalp tissue. William Lyons and his wife, Betty, who traveled more than 1300 miles for the surgery, claim it increased their awareness, gave them a sudden surge in creative juices, and heightened their spirituality. Betty claims it lifted her lifelong depression. “It was like an explosion went off in my mind and body,” she said. “Life came back for me for the first time since I was a kid.” Amanda Fielding, a British proponent of the procedure, performed trepanation on herself. After she applied a local anesthetic to her scalp and taped glasses to her face to prevent blood dripping into her eyes, she used an electric foot-operated dentist’s drill to bore a half-inch wide hole just above the hairline. She used a mirror for guidance and had a friend film the procedure. She says she immediately felt better: “I found it gave me more energy, lifted me up, made me more buoyant.” After the effect faded, she and her husband traveled to Mexico and both had holes drilled in their skulls. The procedure received national attention when ABC’s 20/20 profiled William Lyons and Peter Halvorsen’s attempt to trepan a woman in Beryl, Utah. Before they had a chance to complete the procedure, they were arrested and charged with practicing medicine without a license. Both pleaded guilty and were sentenced to three years probation. Not surprisingly, neurosurgeons say there is no scientific evidence to suggest that trepanation is anything but dangerous. “It’s an assault, it’s not a procedure,” reported Michael Sisti, a neurosurgeon at Columbia Presbyterian Medical Center in New York. On ABC’s 20/20, he suggested that trepanation is really a form of self-mutilation. Trepanning, one of the oldest forms of surgery, dating back thousands of years, may have originally been performed to treat individuals who had suffered massive head trauma in combat. Early surgeons probably used the procedure to remove splinters of skull bone and to relieve pressure from blood clots. Horiuchi, V. (2001, May 6). Surgery is a real hole in the head. Grand Rapids Press, p. A-4. Lawson, W. (2001, September 27). Cutting the cranium. ABC News. Retrieved May 14, 2002 from http://more. abcnews.go.com/sections/science/dailynews/ trepanation000927.html). Lecture/Discussion Topic: Autobiographies Many psychologists argue that autobiographies by people with mental disorders can help those in treatment. In addition to providing insight and concrete strategies, they instill hope for recovery. John C. Norcross suggests that they offer clients a view of mental disorder from someone who has lived it. “Scientists and educators may cry over a list of figures, but laypeople are more impressed by the dramatic personal narrative,” Norcross argues. “Reading a narrative helps normalize and universalize what the patient’s experiencing and can have far more powerful ramifications than just our words.” Norcross and his colleagues asked 362 psychologists whether they had used self-help books in their practice. Although almost 90 percent claimed that they did, only a third had used patient autobiographies. At the same time, those who did were in agreement that they were “very” or “somewhat” helpful. When asked to rank the top 40 autobiographies by editorial quality and helpfulness to patients, the respondents gave the following responses (in order from first to eleventh): 1. An Unquiet Mind by K. R. Jamison (bipolar disorder) 2. Nobody Nowhere: The Autobiography of an Autistic by D. Williams (autism) 3. Darkness Visible: A Memoir of Madness by W. Styron (depression) 4. Out of Depths by A. T. Boisin (schizophrenia) 5. Girl, Interrupted by S. Kaysen (borderline personality disorder) 6. Too Much Anger, Too Many Tears by J. Gotkin and P. Gotkin (schizophrenia) 7. Undercurrents: A Therapists Reckoning With Her Own Depression by M. Manning (depression) 8. Getting Better: Inside Alcoholics Anonymous by N. Robertson (alcoholism) 9. Am I Still Visible? A Woman’s Triumph Over Anorexia Nervosa by S. Heater (anorexia) 10. Welcome Silence: My Triumph over Schizophrenia by C. L. North (schizophrenia) 11. A Brilliant Madness: Living With Manic-Depressive Illness by P. Duke (bipolar disorder) In addition to using these autobiographies as case studies in lecture material, you can also make them the basis of a writing assignment, even perhaps for extra credit. Clifford, J. S., Norcross, J. C., & Sommer, R. (1999). Autobiographies of mental health clients: Psychologists’ uses and recommendations. Professional Psychology: Research and Practice, 30, 56–59. Norcross, J. C., Sommer, R., & Clifford, J. S. (2001). Incorporating published autobiographies into the abnormal psychology course. Teaching of Psychology, 28, 125–128. D. Commonalities Among Psychotherapies (pp. 625–626) Lecture/Discussion Topic: Evaluating Self-Help Resources Millions of Americans, including your students, turn to self-help materials for psychological advice. Books, magazines, Web sites, even films offer help. Some pro-vide high-quality information; others may be misleading, inaccurate, and even harmful. Which ones are helpful, and how does one decide? John Norcross and several coauthors provide the Authoritative Guide to Self-Help Resources in Mental Health (Rev. ed.), an extremely helpful resource that evaluates all the major resources, organized by topic. Based on the results of 8 national studies involving 3000 mental health professionals, the guide addresses 36 common clinical disorders and life challenges from ADHD to weight management. The concluding chapter provides specific “strategies for selecting self-help resources,” which include the following: 1. Be careful not to select a self-help resource on the basis of its cover, title, or glitzy advertising campaign. Go beyond celebrities’ testimonies, fancy ads, and the bookstore’s elaborate display. Several of the volume’s “Not Recommended” books were, in fact, national bestsellers. 2. Select a resource that makes realistic rather than grandiose claims. Those that make grandiose claims can be the most alluring, but most problems do not arise overnight and most can’t be solved overnight. In short, be skeptical of anything that sounds easy, magical, and wondrous. 3. Examine the evidence reported in the self-help resource. The author’s anecdotal experiences or personal testimonies do not count. Authors of the most effective strategies typically describe the research and clinical evidence on which the approach is based. 4. Select self-help resources that acknowledge that problems have multiple causes and alternative solutions. Problems are typically not so simple that they have a single cause and a simple solution. 5. Self-help resources that focus on a specific problem are better than those that claim to be a general approach to solving all your problems. The best books don’t try to reel everyone in and don’t pre-tend to be all things to all people. Rather, they focus on particular problems and offer specific solutions to those problems. 6. Choose self-help resources that clearly identify their limits. Many resources promise that their advice and products will meet every conceivable life challenge. Be wary of such claims. Good books and Web sites will describe when their specific strategies should be used and with whom as well as when they are not applicable or unlikely to be helpful. 7. Don’t be confused by psychobabble and slick writing. Too many authors say things like “To solve your problem you need some high energy experiences,” “You’ve got to get in touch with your feelings,” or “You are sending off the wrong vibes.” Such resources often regress into motivational cheerleading or inspirational sermons. 8. Check the author’s educational and professional credentials. Is he or she a mental health profession-al who has gone through rigorous educational training at a respected university and who has spent years providing professional treatment? 9. Beware of authors who reject the conventional knowledge of mental health professionals. Some will actually attack psychologists and psychiatrists as being too conservative and too concerned with scientific evidence. Although there is nothing wrong with new techniques, there should be reliable evidence of their effectiveness and safety. 10. Distinguish between useful information and subtle advertising. The Internet is not highly controlled and so you cannot always distinguish between reli-able information and advertising. Check the “Who Are We?” and “Privacy Sections” of the site. Be cautious if such information is not provided or is incomplete. 11. Use the Authoritative Guide to Self-Help Resources in Mental Health as a guide. Its recommendations are based on the knowledge of hundreds of the most highly trained and experienced mental health professionals in the United States. Norcross, J. C., Santrock, J. W., Campbell, L. F., Smith, T. P., Sommer, R., & Zuckerman, E. L. (2003). Authoritative guide to self-help resources in mental health. (Rev. ed.). New York: Guilford. E. Culture and Values in Psychotherapy (pp. 626–628) Lecture/Discussion Topic: Mental Health Values of Professional Therapists Jay P. Jensen and Allen E. Bergin conducted a national survey of clinical psychologists, psychiatrists, social workers, and marriage and family therapists to assess values judged relevant to the practice of psychotherapy and important for a mentally healthy life-style. Drawing from hundreds of statements, they finally condensed the value themes in the psychology literature into the following groupings: 1 Competent perception and expression of feelings—e.g., increase sensitivity to others’ feelings, be open, genuine, and honest with others. 2 Freedom/autonomy/responsibility—e.g., assume responsibility for one’s actions, increase one’s capacity for self-control, experience appropriate feelings of guilt. 3 Integration, coping, and work—e.g., develop effective strategies to cope with stress, find fulfillment and satisfaction in work, strive for achievement. 4 Self-awareness/growth—e.g., become aware of inner potential and the ability to grow, discipline oneself for the sake of growth. 5 Human relatedness/interpersonal and family commitment—e.g., develop the ability to give and receive affection, be faithful to one’s marriage partner, become self-sacrificing and unselfish. 6 Self-maintenance/physical fitness—e.g., practice habits of physical health, apply self-discipline in use of alcohol, tobacco, and drugs. 7 Mature values—e.g., have a sense of purpose in living, regulate behavior by applying principles and ideals. 8 Forgiveness—e.g., forgive others who have hurt you, make restitution for one’s own negative influence. 9. Regulated sexual fulfillment—e.g., understand that sexual impulses are a natural part of oneself, have sexual relations exclusively in marriage, prefer a heterosexual sex relationship. 10. Spirituality/religiosity—e.g., seek strength through communion with a higher power, actively participate in a religious affiliation. Hundreds of mental health professionals were asked to rate the importance of each value for a positive, mentally healthy life-style and to indicate the pro-portion of clients for whom the value was considered important in the process of psychotherapy. Contrary to the notion that therapists should be neutral on values, the survey results indicated that there was considerable agreement that certain basic values are important for mentally healthy life-styles as well as for guiding and evaluating psychotherapy. In fact, there was surprising consensus on many of the value themes with broad endorsement of the first eight value themes. Sex and religion were two themes that elicited considerable disagreement. For example, “having sexual relations exclusively within marriage” and “preferring a heterosexual relationship” received “high” or “medium” support from only 49 and 43 percent of the mental health professionals, respectively. “Seeking strength through communion with a higher power” and “actively participating in a religious affiliation” received support from only 34 and 28 percent, respectively. In discussing these results, you might ask students to reflect on whether they think there would be any differences from respondents in other cultures or, if the study were repeated today (it was published in 1988), in the United States. The authors conclude by raising the important question of how therapists should approach their clients’ values and life-styles, particularly if the therapist’s intent is to modify them. First, client self-determination must be respected. Therapists cannot improve mental health by undermining autonomy, which would be the case in any force-feeding of values. Therapists have to decide how best to optimize their clients’ functioning and only then collaborate with their clients in arriving at goals that will facilitate change. Second, therapists must be explicit. Being open about values protects clients by making the agenda and alter-natives clear and makes it less likely that clients will be manipulated by subtle shaping. Jensen, J. P., & Bergin, A. E. (1988). Mental health values of professional therapists: A national interdisciplinary survey. Professional Psychology: Research and Practice, 19, 290–297. Copyright 1988. Reprinted by permission of the authors. Student Project: Applying the Major Therapies To conclude discussion of the psychological therapies, present students with a case study of a psychological disorder and ask them to describe how each major therapy—psychoanalysis, humanistic therapy, behavior therapy, and cognitive therapy—would approach the client. You can present a new case of your own or refer students back to one of the examples given in the previous unit, e.g., the case of Marc (obsessive-compulsive disorder), Greta (depression), or Stuart (schizophrenia). You can make this an individual writing project or divide your class into small groups to complete the assignment. Conclude the exercise with a full-class discussion of how different therapists would approach the case. IV. The Biomedical Therapies (pp. 628–637) A. Drug Therapies (pp. 628–632) Lecture/Discussion Topic: SSRI Antidepressants Introduced in 1987, Prozac became the world’s most widely prescribed antidepressant. In fall 2001, it fell to third place when it lost market exclusivity to generic competition. It’s cousins Zoloft and Paxil became close competitors for first place. Curiously, research suggests that these SSRI drugs show virtually no difference in effectiveness, safety, and side effect profile. Pharmaceutical commercials for the drugs increased dramatically after the September 11, 2001, terrorist attacks. In fact, Pfizer, the world’s largest pharmaceutical company, spent $5.6 million promoting the benefits of Zoloft in treating post-traumatic stress disorder during October 2001. In the past, antidepressants have been one of two basic types: tricyclics or monoamine oxidase inhibitors (MAOIs). Both strengthen the action of serotonin and norepinephrine, two of the chemicals that transmit impulses through the nervous system. The tricyclics work by blocking the reabsorption of the messengers by the nerve cells that release them. The MAOIs interfere with the enzymes that break the messengers down. Although the SSRIs work like the tricyclics—that is, they keep a neurotransmitter in circulation by blocking reabsorption—they work exclusively on serotonin, not norepinephrine. “Instead of using a shotgun, you’re using a bullet,” observes psychiatrist James Halikas of the University of Minnesota. The SSRIs’ advantage is not that they are inherent-ly more effective in treating depression but rather that they are easier to prescribe and have fewer side effects. They also have a broader range of uses than competing drugs. SSRIs’ side effects have included headaches, nausea, insomnia, and weight loss. However, these are far less serious than the low blood pressure, heart disturbances, blurred vision, and weight gain produced by the older drugs. People unable to tolerate the tricyclics or MAOIs are successfully taking the SSRIs. Doctors are now using the drugs not only as a treatment for depression but also to treat anxiety, obsessive-compulsive disorder, and post-traumatic stress disorder. Neurologist Ruth Brunn explains, “Some people respond to one and not the other. But most are helped by one or the other. The new drugs have absolutely revolutionized treatment of this disorder.” Cowley, G., et al. (1990, March 26). The promise of Prozac. Newsweek, 38–41. Rosack, J. (2002, March 1). “Drug makers find September 11 a marketing opportunity,” and “SSRIs show little difference as first-line treatment,” Psychiatric News, 9 and 25. Lecture/Discussion Topic: Cosmetic Psychopharmacology Prozac was labeled the wonder drug of the 1990s. As noted above, it not only treats depression effectively, it works in alleviating the symptoms of other psychological disorders. In Listening to Prozac, Peter Kramer describes the global effects of the drug, which makes some people feel “better than well.” In describing the drug’s ability to alter personality style, he tells of trans-formed lives in which patterns of withdrawal, compulsiveness, and timidity are replaced with radically different and personally satisfying ways of interacting with the world. Overall self-image improves, energy levels increase dramatically, and greater social popularity is achieved. People experience greater success and satisfaction in most every aspect of life. Kramer raises a number of important issues that make excellent discussion-starters for class. For example, he asks how proper it is to prescribe Prozac to those who suffer no specific psychological disorder but who want to function more effectively in their personal and social lives. Is this not “cosmetic psychopharmacology,” akin to a psychological nose job? Kramer notes that our discomfort may arise in part from our belief that it is all very well for drugs to do small things—for example, to induce sleep, allay anxiety, reduce depression—but not to transform entire lives. For a drug to have such a pronounced effect is inherently unnatural, unsafe, even uncanny. While we might respond to the dilemma by saying let each person choose, to the degree that Prozac becomes widely used, it ups the stakes with respect to social competition in much the same manner that steroids up the stakes in Olympic competition. While people can choose not to take the drug, where does that place them in a culture in which cosmetic psychopharmacology stands as the norm? At best it becomes “free choice under pressure.” Prozac (as well as its cousins Zoloft and Paxil) is clearly effective in reducing negative emotions. For example, it seems to possess the potential to obviate grief. Isn’t it wonderful to find relief from debilitating grief and to become able once again to live one’s life? Or is grief natural and even healthy? More generally, is it possible that transforming medication interferes with the process of self-examination that often accompanies our negative emotions? Kramer also ponders whether Prozac serves to enforce arbitrary cultural values. He notes the popularity of Valium as a treatment choice for anxious women during the 1950s and 1960s. Many would argue that Valium helped to keep them in their place. Yet anxiety and discontent may have been appropriate responses for women of that era, given the restrictive expectations placed upon them. Now that women are expected to be active, productive, and assertive, Prozac may paradoxically serve the same function, that of molding them to the current cultural ideal. Kramer, P. (1993). Listening to Prozac: A psychiatrist explores antidepressant drugs and the remaking of the self. New York: Viking. Lecture/Discussion Topic: A Pill for Stage Fright (Anxiety) Michael Skoler reports that Inderal, a heart medication (known generically as propranolol), is the antianxiety drug for intellectuals. Unlike tranquilizers, Inderal does not cloud the mind or impair physical coordination. Professional musicians, lawyers, undergraduate students, and even physicians now take this beta blocker before important presentations or tests. The FDA has not approved Inderal specifically for anxiety, but when a drug has been approved for one condition, physicians can legally prescribe it for others. In the early 1960s, beta blockers were approved to treat high blood pressure and hardening of the arteries. Patients who took the medication experienced a pleas-ant side effect: The drugs kept them calm in stressful situations, which should not have been surprising because beta blockers reduce the symptoms that often accompany nervousness. That is, they keep blood pres-sure from rising and the heart from racing by blocking the chemical messengers that produce these changes. In a test of the effectiveness of Inderal, professional musicians were given either a sugar pill or Inderal before performing for three judges and a small audience. The musicians who took Inderal reported feeling more in control and their heart rates were slow and even (without the drug their heart rates were 40 beats a minute faster). More important, the judges evaluated their performances as significantly better. A 1987 survey indicated that 27 percent of professional musicians had used the drug. Psychiatrists estimate the number is much higher. Inderal has also been tested with high school students who freeze when they take the SAT. Twenty-five students took the test twice, using the beta blocker the second time. Combined verbal and math scores went up an average of 120 points. Normally, a combined score goes up only 22 points. After these results were reported in the press, dozens of parents called asking for the name of the drug and correct dosage, so that their doctors could prescribe it for their children. “We could easily teach students that the only way they can face a test is to take an Inderal tablet,” says Harris Faigel, who is conducting the research. “It makes me wonder whether we should continue the study.” Psychologist Mark Siegert believes Inderal is useful for helping people whose stage fright is primarily a physical problem. Some people’s bodies simply overreact to fear. He is concerned, however, that others will view the drug as “a way to perform free of anxiety.” And, he concludes, “In my experience anxiety is some-thing we have to live with.” The controversy surrounding the use of Inderal by musicians is reflected in the case of Ruth Ann McClain, who taught flute at Rhodes College. She was fired after recommending the drug to adult students afflicted with performance anxiety. College officials claimed that recommending drugs fell outside the studentinstructor relationship. They also charged that Ms. McClain, who had taught at Rhodes for 11 years, had asked a doctor for medication for her students. McClain said she mere-ly recommended that the students consult a physician about obtaining a prescription. “If I am looking out for the welfare of my students,” she stated, “I cannot in good conscience not tell them about beta blockers.” Some critics have also questioned the ethics of better performance through chemistry. For example, in auditions, which are even more nerve-racking than regular performances, do those on drugs have an unfair advantage over those who do not? Might drug testing apply to performers, just as it does to some athletes and to job applicants at some companies? Some wonder whether professional musicians might some day join professional athletes in scandals involving performance-enhancing drugs. Obviously, beta blockers such as Inderal differ significantly from steroids, which use testosterone to increase muscle mass, strength, and speed. One physician noted that, rather than enhance, Inderal enables by removing debilitating symptoms. It does not improve tone or technique, nor does it compensate for inadequate preparation. Skoler, M. (1988, March/April). Upstaging fright with a pill. Hippocrates, 26–28. Tindall, B. (2004, October 17). Better playing through chemistry. New York Times. Retrieved from http://query.nytimes.com/gst/fullpage.html?res=940DE7DC1E3BF934A25753C1A9629C8B63. B. Brain Stimulation (pp. 632–635) Lecture/Discussion Topic: Electroconvulsive Therapy Harold Sackeim has attempted to correct misconceptions surrounding ECT and to prove that it is a valid, even life-saving option. While the public often believes that the treatment is only imposed on troublesome or unwilling patients, such as those portrayed in Ken Kesey’s One Flew Over the Cuckoo’s Nest, the typical ECT patient is White, female, middle-aged, and from a middle-to-upper-income background. She usually receives treatment in a private or university hospital after drug therapy has proved ineffective. Because the therapy is a relatively expensive and complicated procedure, requiring specially trained psychiatrists, anesthesiologists, and nurses, it is used far less extensively in public hospitals. The aim of ECT is to produce a seizure in the brain, similar to what occurs spontaneously in some types of epilepsy. In fact, research suggests that without a seizure, ECT is ineffective. A small electric current passes through two electrodes placed on the patient’s head. Only a portion of this current reaches the brain because most of it is deflected by the skull. Since muscle relaxants may interfere with breathing, an anesthesiologist administers oxygen. The muscle relaxants often block all outward signs of a seizure, and so the patient’s brain waves must be monitored. The procedure takes about 5 minutes, and complications are rare. Since patients sleep through the therapy, it should come as no surprise that in one study, 82 percent rated ECT as equally or no more upsetting than going to the dentist. Irwin and Barbara Sarason review the important improvements that have been made in ECT since it was first introduced and that have greatly improved its safety. For example, the intensity of the electrical charge has been cut in half and its duration has been reduced from one second to one-twenty-fifth of a second. The sessions have been reduced from three a day to no more than three a week. In addition, the length of treatment has been decreased from more than 20 sessions to typically 10 or fewer. In contrast to earlier treatments, both anesthetics and muscle relaxants are now used and brain waves and the electrical functioning of the heart are monitored through EEG and EKG. Whereas electrodes were formerly placed on both sides of the head, they are now placed on the nondominant side only. Researchers in Iowa found that more than 10 per-cent of untreated patients diagnosed as suffering from major depressive disorder died within three years. Although some were suicide victims, 75 percent of those who died did so as a result of illnesses such as heart attack and cancer. Only 2 percent of patients who received ECT died within three years. Sackeim provides a case history to illustrate ECT’s potential effectiveness. Anna, a 36-year-old teacher and mother of two, had a history of recurrent depression and had been in psychotherapy for several years. She also had been treated with antidepressant drugs, which were ineffective. Finally hospitalized, Anna described life as a “living hell.” She slept poorly, had little appetite, and experienced significant weight loss. Her concentration was so poor she could barely read a newspaper headline. Obsessed with the notion that she had ruined her children’s lives, she threatened to kill herself. With her consent, psychiatrists began ECT. After five treatments, she had completely recovered and returned to her family and job. How does ECT compare with alternative treatments for depression? When compared with antidepressant drugs, ECT has proved either as effective or more effective. Overall, Sackeim reports, it can help 70 to 80 percent of all people with major depressive disorder. He cautions, though, that it should not be viewed as a cure. Patients, particularly those with a history of recurrent depression, are likely to relapse unless they receive some form of medication or therapy following ECT. When compared with other treatments for anxiety and personality disorders, ECT has been found to be of little value. Except in cases of catatonia, there is little evidence that the treatment is effective with schizophrenia patients. At one time, some psychiatrists wrongly believed that because schizophrenia was rare in epileptics, seizures might protect against schizophrenia. As a result, thousands of schizophrenia patients throughout the world were treated with ECT. Sackeim, H. (1985, June). The case for ECT. Psychology Today, 36–40. Sarason, I., & Sarason, B. (2005). Abnormal psychology (11th ed.). Upper Saddle River, NJ: Prentice Hall. C. Psychosurgery (pp. 635–636) Lecture/Discussion Topic: Cingulotomy By 1949, when Egas Moniz won a Nobel Prize for developing the lobotomy, tens of thousands had been lobotomized—alcohol abusers, criminals, and people with mental retardation, including Rosemary Kennedy, sister of the future president. During the 1950s, calming drugs became available and psychosurgery was largely abandoned. The text notes that lobotomies are no longer performed and that other psychosurgery is used only in extreme cases. For the most part, psychosurgery has become taboo, even though refinements targeting very limited areas in the brain are now much safer. Neurosurgeons perform operations at the risk of being picketed. Students may be interested in learning that Moniz himself was shot and left partially paralyzed by one of his lobotomized patients. One notable exception is a procedure known as cingulotomy, which has been performed at Massachusetts General Hospital. Bearing little relation to the lobotomy, the procedure involves passing an electrode needle through two small holes in the skull and searing a tiny lesion in the cingulum, a bundle of nerve fibers linking the emotional centers of the brain with the thought centers in the cortex. Since 1962, about 700 patients have received cingulotomies, averaging about 20 operations annually. Used primarily in the treatment of obsessive-compulsive disorder, certain phobias, and depression, the surgery is offered only to those who have been ill for years and, in many cases, are at risk for suicide. In addition, patients must provide extensive documentation that they have tried every other available form of thera-py and drug treatment. No surgery is ever performed without the patient’s informed consent. Although case reports indicate extraordinary turn-arounds for some very sick people, experts do not agree on the overall success rate of this surgery. The hospital’s chief surgeon G. Rees Cosgrove puts the improvement rate as high as 60 to 70 percent for depression, some-what less for obsessivecompulsive disorder. All agree, however, that the procedure is relatively benign, causing none of the disastrous side effects associated with lobotomies. A new surgical tool called the Gamma knife permits the procedure to be performed without piercing the skull. It shoots hundreds of beams of radiation from different angles at the target site in the brain. Although no single beam damages tissue, where the beams converge, a lesion is created. Beck, M. (1990, March 26). Beyond lobotomies. Newsweek,, 44. D. Therapeutic Life-Style Change (pp. 636–637) Lecture/Discussion Topic: Therapeutic Life-Style Change You can readily extend the unit’s brief treatment of therapeutic life-style change, including more specific recommendations to students on how they might implement each of the six crucial components. At their helpful Web site (www.psych.ku.edu/tlc), Stephen Ilardi and his colleagues include the following advice: 1 Aerobic exercise: Aerobic exercise is anything— running, walking fast, biking, or playing basketball, for example—that gets your heart rate elevated to about 120 to 160 beats per minute. Anaerobic exercise (such as yoga or weightlifting) is better than nothing, but aerobic exercise produces the strongest antidepressant effects. Many people find that a regular exercise routine and an exercise partner help them remain motivated. 2 Adequate sleep: Go to sleep and wake up at the same time every day. Prepare yourself by having a “bedtime ritual.” Dim the lights, turn off the TV and computer, and put on your PJs. Engage in a quiet activity such as reading. Avoid caffeine and alcohol several hours before you plan to go to bed. 1 Light exposure: If you cannot go outside, get light exposure from a special light box that emits 10,000 lux. A good one costs about $170 (www.Light TherapyProducts.com). Try to get light exposure at the same time each day. Some prefer to sit by it while they eat breakfast and read the paper. Others like it on while they read or study in the evening. Experiment to see what works best for you. Try your best to avoid missing a day since this is some-thing that will only work for you cumulatively if you are consistent. 2 Social connection: Recognize that as you become more depressed, you are less motivated to seek out others for socializing. Spend as much time as possible with others. This is a powerful way to distract yourself from rumination. 3 Anti-rumination: Rumination is a habit that many depressed people fall victim to as their negative thoughts spiral out of control. Put a stop to it immediately. Call a friend, exercise, write down the negative thoughts in a journal, or engage in some pleasant activity (e.g., knitting, reading, or another favorite hobby). 4 Nutritional supplements: You can buy omega-3 fatty acid supplements at a drugstore or health food store. Look for a brand that gives you 1000 mg of EPA and 500 mg of DHA per day. This is the amount that has been shown to be beneficial to people with depression. These can be taken even if you are on an antidepressant. To avoid aftertaste, freeze the pills and take them right before a meal. Some people prefer to take the supplements in liquid form. In presenting these specific recommendations, you might emphasize that Ilardi’s goal is to enable people to fight depression without prescription drugs whenever possible. According to Ilardi, research indicates that these behavioral changes produce the same beneficial brain change that come from medication but without the risks and side effects. Moreover, many people who take drugs such as Prozac or Zoloft gain relief simply because of a placebo effect. More recent studies (as reported by Ilardi to Katie Greene) also show that some medications could increase the risk of suicidal behavior. Impulsive violent behavior, sexual side effects, and even emotional numbing are also potential risks. Finally, “As soon as they stop taking the medication,” observes Ilardi, they have about a 50/50 chance of having the depression return in under a year.” Greene, K. (2005). Change your life, change your mind. Kansas Alumni Magazine, 2, 23–27. Ilardi S. S., Karwoski, L., Lehman, K. A., Stites, B. A., & Steidtmann, D. (2007). We were never designed for this: The depression epidemic and the promise of thera-peutic lifestyle change. Unpublished manuscript, University of Kansas. V. Preventing Psychological Disorders (pp. 637–638) Lecture/Discussion Topic: Positive Psychotherapy You can extend the discussion of preventing psychological disorders to consideration of Martin Seligman’s positive psychotherapy (PPT) that emphasizes human flourishing (see also text Unit 10). In early research, PPT was combined with more traditional therapeutic approaches in the treatment of depression. Clearly, however, PPT strategies can be applied more generally in preventing psychological disorder. PPT contrasts with standard therapies in its emphasis on building positive emotions, character strengths, and purpose in life. Depression in particular seems to be marked by a lack of positive emotion, absence of engagement, and lack of felt meaning. The exercises that Seligman and his research team utilize include the following: 1 Using your strengths. Participants complete a questionnaire assessing their top five strengths and then consider specific ways of using those strengths in everyday life. 2 Three Good Things/Blessings: Each evening participants write down three good things that happened in the course of the day and why they think they happened. 3 Obituary/Biography: Participants anticipate passing away after living a fruitful and satisfying life and then write a brief essay summarizing what they would like to be remembered for most. 4 Gratitude Visit: Participants think of someone to whom they are grateful, compose a letter describing their gratitude, and read the letter by phone or in person. 5 Active/Constructive Responding: At least once a day, participants react in a visibly positive and enthusiastic way to good news from someone else. 6 Savoring: Once a day, participants take time to enjoy something that they usually rush through (e.g., eating a meal, taking a shower). When it’s over, they write down what they did, how they did it differently, and how it felt compared with when they rush through it. Two preliminary studies by Seligman and his research team suggest that PPT (using the elements just described) is effective. In the first study, PPT delivered to groups significantly decreased levels of mild-to-moderate depression through a 1-year follow-up. In a second study, PPT delivered to outpatients suffering major depressive disorder proved more effective than “treatment as usual” (including cognitivebehavioral therapy) and “treatment as usual plus medication.” Seligman, M. E. P., Rashid, T., & Parks, A. C. (2006). Positive psychotherapy. American Psychologist, 61, 774–788. Lecture/Discussion Topic: From a Disease Focus to a Wellness Model Emory Cowen, former professor of psychology and psychiatry at the University of Rochester and director of the university’s Center for Community Study, argued that we must replace the pervasive “disease” model in psychology with a “wellness” model. We must shift from emphasizing people’s weaknesses to shoring up their strengths. The task will not be easy, he suggests, for even the mental health field “simply and naturally thinks sick more, and long before, it thinks well.” Four specific concepts currently being researched and tested in programs such as Head Start and the Perry Preschool Project (which target inner-city children from high-risk families) illustrate what Cowen means by a new emphasis on wellness. The first is teaching competence. This refers to both practical skills, such as those necessary to do a job well, and social skills, such as the ability to communicate and control anger. “The presence of these skills,” says Cowen, “relates to wellness, and their absence to maladaptation.” Although acquiring competence is life-long, the best time to lay the foundation is in childhood. Another concept is resilience, or the ability to with-stand pressure and emerge stronger for it. Cowen advocates examining in greater detail youngsters who live “in the chronic shadow of what psychologist Norman Garmezy so aptly called ‘stressors of marked gravity.’” Studying those who thrive in this environment could help others living under chronically stressful conditions. Two socially oriented concepts are also important in Cowen’s model. One is social-system modification, that is, helping foster environments that promote wellness. Institutions such as schools, churches, and the workplace are especially important to target because they are rarely neutral in their impact on people. “Whereas some act coincidentally to enhance wellness,” says Cowen, “others, oblivious to incidental outcome effects, may pose unintended obstacles to wellness.” The other social concept is empowerment. For many people, the roots of maladaptation, or problems in living, reside less in personal failings than in de facto aspects of the macrosystem that deprive them of power, justice, and opportunity. A major goal then is to pro-mote policies and conditions that enable people to gain control over their lives on the assumption that this will reduce problems in living and enhance wellness. Cowen, E. L., Hightower, A. D., Pedro-Carroll, J. L., Work, W. C., Wyman, P. A., & Haffey, W. G. (1996). Schoolbased prevention for children at risk: The primary mental health project. Washington, DC: American Psychological Association. De Angelis, T. (1990, December). Should wellness model replace disease focus? APA Monitor, 30. Lecture/Discussion Topic: Principles of Effective Prevention Programs In a review of reviews, Maury Nation and his colleagues sought to identify successful prevention strategies for addressing problems of substance abuse, risky sexual behavior, school failure, and juvenile delinquency. They identified nine characteristics that were consistently associated with effective programs. 1 Comprehensive: Each strategy used multiple interventions across several critical domains—e.g., family, peers, community—that affected the development and perpetuation of the problems to be prevented. 2 Varied teaching methods: These methods all focused on increasing the patient’s awareness and understanding of the problem behaviors as well as on acquiring and enhancing relevant skills. 3 Sufficient dosage: Programs provided enough intervention to produce the desired effects and provided necessary follow-up to maintain the results of the program. 4 Theory-driven: Programs had a theoretical justification, were based on accurate information, and were supported by empirical research. 5 Positive relationships: Programs provided exposure to adults and peers in a way that fostered strong interpersonal connections and support. 6 Appropriately timed: Programs were started early enough to have an effect on the development of the problem behavior and were sensitive to the developmental needs of the participants. 7 Socioculturally relevant: Programs were sensitive to the community and cultural norms of the participants and made deliberate efforts to include the tar-get group in program planning and implementation. 8 Outcome evaluation: Programs had clear goals and objectives and made an attempt to systematically document their results relative to the goals. 9 Well-trained staff: Program staff supported the pro-gram and were trained in the implementation of the intervention. The researchers conclude that their review offers important guidelines for conceptualizing and develop-ing future prevention strategies. Moreover, they argue for “multiple-problem” prevention programs because at-risk children tend to be vulnerable to a variety of disorders as a result of dysfunctional families, neighbor-hoods, schools, and peer relationships. Nation, M., et al. (2003). What works in prevention: Principles of effective prevention programs. American Psychologist, 58, 449–456. Classroom Exercise: The Personal Growth Initiative Scale (PGIS) Christine Robitschek’s (1998) Personal Growth Initiative Scale (PGIS), Handout 13–12, provides an excellent conclusion to this unit and, specifically, to the topic of preventing psychological disorder. Personal growth, suggests Robitschek, is a person’s active, intentional involvement in changing and developing. Growth, she suggests, must be an intentional process. To obtain a total score, students add the numbers they gave in response to each statement. PGIS scores range from 0 to 45. High scorers (above 22.5, the mid-point) recognize and capitalize on opportunities for personal change. More important, they search out and create situations that will foster their growth. In contrast, those with low scores actively avoid situations that challenge them to grow. PGIS scores seem to have a strong positive relationship to psychological well-being and a negative relationship to psychological distress. So the higher the PGIS score, the less psychological distress the person seems to feel. Robitschek and her colleagues are presently examining whether PGI might also defend against distress by leading people to seek help earlier— when they first experience negative events—thus reducing the extent and effects of stress. PGIS scores are positively linked to assertiveness, internal locus of control, and instrumentality (knowing how to reach important goals). No differences in scores are found between men and women or between ethnic minority and majority groups. Robitschek, C. (1998). Personal growth initiative: The construct and its measure. Measurement and Evaluation in Counseling and Development, 30, 183–198. Robitschek, C. (1999). Further validation of the Personal Growth Initiative Scale. Measurement and Evaluation in Counseling and Development, 31, 197–210. Robitschek, C., & Cook, S. W. (1999). The influence of personal growth initiative and coping styles on career exploration and vocational identity. Journal of Vocational Behavior, 54, 127–141. Whittaker, A. E., & Robitschek, C. (2001). Multidimen-sional family functioning as predictors of personal growth initiative. Journal of Counseling Psychology, 48, 420–427. PLEASE NOTE: Due to loss of formatting, the Handouts are only available in Adobe