THALIDOMIDE FOR SEVERE SYSTEMIC ONSET JUVENILE RHEUMATOID
ARTHRITIS: A MULTICENTER STUDY
THOMAS J. A. LEHMAN, MD, SHARON J. SCHECHTER, BS, ROBERT P. SUNDEL, MD, SHEILA K. OLIVEIRA, MD,
ANNA HUTTENLOCHER, MD, AND KAREN B. ONEL, MD
Thirteen children with difficult systemic onset juvenile rheumatoid arthritis were treated with thalidomide. At 6 months, 11 of
the 13 were able to reduce their use of prednisone (P < .002), with a concurrent improvement in erythrocyte sedimentation rate
(P < .0001) and an increase in hemoglobin level (P < 0.005). Juvenile rheumatoid arthritis improvement scores $50% were
obtained by 10 of the 13 children. (J Pediatr 2004;145:856-7)
hildren with severe systemic onset juvenile rheumatoid arthritis (SoJRA) often have a poor outcome because of chronic
inflammation and corticosteroid side effects.1 Current alternatives to corticosteroids include autologous stem cell
transplantation, cyclosporine, azathioprine, cyclophosphamide, intravenous gammaglobulin, etanercept, and infliximab.
None is consistently successful.2-6
Thalidomide is a unique anti-inflammatory agent that suppresses angiogenesis, cellular adhesion molecule expression, and
production of tumor necrosis factor-a and interleukin-6.7 We previously reported the use of thalidomide in 2 children with
SoJRA.8 This report includes 13 children with SoJRA treated at 4 institutions. Our findings suggest that thalidomide is a useful
corticosteroid-sparing agent with an acceptable level of side effects when used in low dosage.
C
METHODS
The patients were drawn from four different institutions (Hospital for Special
Surgery in New York, NY; Children’s Hospital Medical Center in Boston, Mass;
Universidade F Rio De Janeiro, Brazil; and the University of Wisconsin, School of
Medicine, Madison, Wis). Two were reported previously.8 Patients were selected for
inclusion because they had failed conventional therapy according to their attending
physicians.
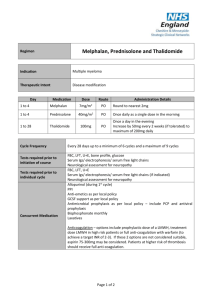
Thalidomide was given at an initial dose of 2 mg/kg per day, rounded to the nearest 50
mg. If no toxicity was noted in 2 weeks, the dose was increased to 3 to 5 mg/kg per day if
necessary (7 of 13 patients). Informed consent was obtained, and all US patients were entered into the system for Thalidomide education and prescribing safety (STEPS) program.9
Monthly visits included physical examination, joint count, complete blood count,
erythrocyte sedimentation rate, and biochemical profile. Prednisone dosage, thalidomide
dosage, and evidence of thalidomide toxicity were recorded at each visit. Statistical analysis,
including testing for normality and paired t tests, was performed with the use of GraphPad
InStat GraphPad Software, Inc (San Diego, Calif).
RESULTS
Seven girls and six boys with a mean age of 10.15 ± 1.66 years were included. All
patients were #16 years of age at the onset of SoJRA. When studied, their ages ranged
from 3 to 23 years. All patients were followed for 6 months. Prior therapy included
nonsteroidal anti-inflammatory drugs, methotrexate, etanercept, and corticosteroids in all
cases. Five had received cyclosporine A and azathioprine and two had received
SoJRA
STEPS
856
Systemic onset juvenile rheumatoid arthritis
System for Thalidomide education and prescribing safety
From the Division of Pediatric Rheumatology, Hospital for Special Surgery, and the Department of
Pediatrics, Sanford Weill Medical College of Cornell University, New York,
New York; the Division of Immunology, Children’s Hospital Medical Center, Boston, Massachusetts; Pediatric
Rheumatology, Universidade F Rio
De Janeiro, Rio de Janeiro, Brazil;
and the Department of Pediatrics,
University of Wisconsin Medical
School, Madison, Wisconsin.
Dr Lehman is the recipient of a grant
from Celgene to measure cytokine
levels before, during, and after thalidomide therapy in children with systemic onset juvenile rheumatoid
arthritis.
Submitted for publication Mar 28,
2004; last revision received Jun 2,
2004; accepted Aug 4, 2004.
Reprint requests: Thomas J.A.
Lehman, MD, Division of Pediatric
Rheumatology, Hospital for Special
Surgery, 535 E 70th St, New York,
NY 10021. E-mail: goldscout@aol.
com.
0022-3476/$ - see front matter
Copyright ª 2004 Elsevier Inc. All rights
reserved.
10.1016/j.jpeds.2004.08.020
cyclophosphamide. None had achieved adequate disease
control defined as a sustained rise in hemoglobin above 11
g/dL or reduction in erythrocyte sedimentation rate by at least
50% and absence of fever (present in 8 of 13), rash (9 of 13), or
other systemic manifestations.
Eleven of the 13 patients had a sustained response to
thalidomide with adequate disease control. Most showed
improvement within 4 weeks. For the 13 patients, the mean
prednisone dosage decreased from 14.8 ± 3.8 mg/d to 5.1 ± 2.3
mg/d (P < .002) over the 6 months, and 6 were able to
discontinue prednisone.
The mean erythrocyte sedimentation rate fell from 54 ±
8.2 to 23 ± 6.3 mm/h (P < .001.) In 7 of the 13 children, the
erythrocyte sedimentation rate was normal after 6 months.
Ten of the 11 patients had a sustained rise in serum
hemoglobin. The mean serum hemoglobin concentration rose
from 10.4 ± 0.53 to 12.0 ± 0.40 g/dL (P < .005). Four patients
had a rise in serum hemoglobin level $2 g/dL.
The mean joint count fell from 19.1 ± 8.2 to 6.1 ± 2.6
(P = .07). No patient had a rise in joint count. Ten of the 13
children achieved JRA improvement scores $50%, according
to the criteria for the preliminary definition of improvement in
juvenile arthritis.10
Side effects were minor. No child had clinically evident
neurotoxicity. Short-lived paresthesiae (15 to 30 minutes)
manifested as numbness and tingling were common during the
first weeks of thalidomide administration. In all cases, the next
dose of thalidomide was held until these symptoms resolved.
All of the patients in the study were able to continue
thalidomide at the same (9 of 13) or a decreased dosage at the
investigator’s discretion. Sedation was a common effect.
Giving the daily dose at bedtime minimized inconvenience.
Improved sleep patterns were noted by families. Constipation
was reported by some but resolved with dietary adjustments.
Thalidomide is a well-known teratogen. All subjects of
reproductive age agreed to use effective forms of birth control
and were carefully monitored for possible pregnancy according
to the STEPS protocol. No patient became pregnant during
the course of this study.
DISCUSSION
This report expands our report of two SoJRA children
who improved dramatically with thalidomide.8 It documents
the efficacy of thalidomide in 11 additional children with
SoJRA at varied institutions treated by different physicians.
Previously, all had failed conventional therapy.
Children receiving thalidomide must be monitored for
prolonged paresthesiae or other evidence of neurotoxicity.
Several children in this series had brief paresthesiae, but none
required discontinuation of thalidomide. Sedative effects and
constipation remain manageable concerns. Thalidomide is
well known as a teratogen and must not be used by women
who are at risk of becoming pregnant. This risk is not present
in young children and can be minimized in adolescents by
rigorous use of the STEPS protocol. These potential side
effects suggest that thalidomide should be restricted to
Thalidomide for Severe Systemic Onset Juvenile Rheumatoid
Arthritis: A Multicenter Study
children with SoJRA who are inadequately responsive to
other agents.
Thalidomide is the progenitor of a novel class of
immunomodulatory agents that downregulate the inflammatory mediators tumor necrosis factor-a, interleukin-6, and
nuclear factor-kB as well as affecting angiogenesis, apoptosis,
and endothelial cell signaling.11 New derivatives termed
ImiDs, which appear to share the anti-inflammatory activities
of thalidomide without the teratogenic or sedative effects or
neurotoxicity, are under active investigation.7,11
In summary, we report beneficial effects of thalidomide
in 11 of 13 children with severe SoJRA who had failed
previous therapy. Although the risk of toxicity from
thalidomide is real, none of our patients had deleterious side
effects. The risks of the low dosage of thalidomide used in this
study are acceptable when compared with the permanent
physiologic and psychologic sequelae associated with prolonged high-dose corticosteroid therapy. Further, the possible
toxicities of thalidomide are small when compared with those
of autologous stem cell transplantation and other proposed
salvage therapies for severe SoJRA. Until a larger controlled
study is completed, therapy with thalidomide should be
reserved for those children with SoJRA who have failed
conventional therapy.
REFERENCES
1. Lomater C, Gerloni V, Gattinara M, Mazzotti J, Cimaz R, Fantini F.
Systemic onset juvenile idiopathic arthritis: a retrospective study of 80
consecutive patients followed for 10 years. J Rheumatol 2000;27:491-6.
2. Wulffraat NM, Brinkman D, Ferster A, Opperman J, ten Cate R,
Wedderburn L, et al. Long-term follow-up of autologous stem cell
transplantation for refractory juvenile idiopathic arthritis. Bone Marrow
Transplant 2003;32(Suppl 1):S61-4.
3. Silverman ED, Cawkwell GD, Lovell DJ, Laxer RM, Lehman TJA,
Passo MH, et al. Intravenous immunoglobulin in the treatment of systemic
juvenile rheumatoid arthritis: a randomized placebo controlled trial: Pediatric
Rheumatology Collaborative Study Group. J Rheumatol 1994;21:2353-8.
4. Wallace CA, Sherry DD. Trial of intravenous pulse cyclophosphamide
and methylprednisolone in the treatment of severe systemic-onset juvenile
rheumatoid arthritis. Arthritis Rheum 1997;40:1852-5.
5. Shaikov AV, Maximov AA, Speransky AI, Lovell DJ, Giannini EH,
Solovyev SK. Repetitive use of pulse therapy with methylprednisolone and
cyclophosphamide in addition to oral methotrexate in children with systemic
juvenile rheumatoid arthritis: preliminary results of a long-term study.
J Rheumatol 1992;19:612-6.
6. Gattorno M, Buoncompagni A, Faraci M, Pistoia V. Early treatment of
systemic onset juvenile chronic arthritis with low-dose cyclosporin A. Clin
Exp Rheumatol 1995;13:409-10.
7. Weber D. Thalidomide and its derivatives: new promise for multiple
myeloma. Cancer Control 2003;10:375-83.
8. Lehman TJA, Striegel KH, Onel KB. Thalidomide therapy for
recalcitrant systemic onset juvenile rheumatoid arthritis. J Pediatr 2002;140:
125-7.
9. Zeldis JB, Williams BA, Thomas SD, Elsayed ME. STEPS:
a comprehensive program for controlling and monitoring access to
thalidomide. Clin Ther 1999;21:319-30.
10. Giannini EH, Ruperto N, Revelli A, Lovell DJ, Felson DT, Martini A.
Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum
1997;40:1202-9.
11. Dredge K, Marriot JB, Dalgliesh AG. Immunological effects of
thalidomide and its chemical and functional analogs. Crit Rev Immunol
2002;22:425-37.
857