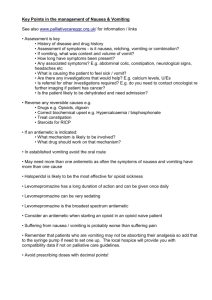
Medications Chart Completed

Medications:
Postpartum
Prenatal Vitamin/
PNV
Classification,
Action, & Use
To make sure woman gets all the supplements she needs when pregnant.
Has increased level of folic acid as required to decrease the incidence of neural tube defects.
Ferrous Sulfate Iron preparation. To correct simple iron deficiency and to treat iron deficiency anemias
Docusate Sodium Gastrointestinal agent, stool softener. For people who should avoid straining during defecation and for treatment of constipation associated with hard, dry stools.
Dose &
Route
1 tablet PO every day.
Recommended to take 400 mcg folic acid, 3 months before conception to ↓ incidence of neural tube defects (NTD).
Po 50-500 mg/d. PR 50-
100 mg added to enema fluid
Side Effects &
Adverse Reactions
Gastrointestinal:
Abdominal pain, constipation, dark stools, diarrhea, nausea, vomiting
Miscellaneous:
Allergic reaction
PO Iron deficiency: 750-
1500mg/d in 1-
3 divided doses.
Iron supplement: pregnancy ,
300-600mg/d in divided doses
Nausea, heartburn, constipation, black stools, yellow browndiscoloration of eyes, rickets, massage overdosage, which cause shock, cardiovascular collapse, liver necrosis, and death.
Diarrhea, throat irritation, rash, nausea, and bitter taste.
Contraindications &
Precautions
Due to calcium content, use caution with kidney stones. Iron supplementation should not be used with hemochromatosis and hemosiderosis. Use caution with severe renal or hepatic dysfunction or failure.
Peptic ulcer, regional enteritis, ulcerative colitis; and hemolytic anemia. Caution use in pregnancy and lactation
Atonic constipation, nausea, vomiting, abdominal pain, fecal impaction, structural anomalies of colon and rectum, intestinal obstruction or perforation. Take with caution if have history of
CHF, edema, diabetes mellitus.
Nursing Considerations &
Patient Teaching
Pre natal vitamins should be taken daily, to insure the women obtains the necessary vitamins during pregnancy. Woman can obtain the vitamins as well in a balanced diet. Megadoses of vitamins should be avoided, look for signs and symptoms of toxicity like nausea, and loss of hair, and make sure to take special precaution when taking vitamins
Iron absorption is inhibited by eggs and milk.
Teach pt. to avoid taking other OTC vitamins because can cause toxicity or encourage her to check with her HCP before doing so.
Monitor Hgb and reticulocyte values during therapy. Continue iron therapy for 2-3 months after the hemoglobin level has returned to normal.
Monitor bowel movements as constipation is a common adverse effect.
Consuming citrus fruit or tomato juice with iron preparation may increase it’s it absorption
Milk, calcium, eggs, or caffeine beverages when taken with the iron preparation may inhibit absorption. Cause dark green or black stool. Do not breast feed while taking drug. Take on an empty stomach one hr. before or 2 hrs. after meals to increase absorption with Vitamin C
(OJ).
Withhold drug if diarrhea develops and notify physician, note therapeutic effectiveness.
Take sufficient liquid with each dose and increase fluid intake during the day, if allowed. Do not take with mineral oil. Do not take for prolonged periods in lieu of proper dietary management or treatment of underlying causes of constipation
Increase fluids - take with a glass of water.
Teach to eat fruit, vegetables, and fiber to help promote optimal bowel function.
Medications:
Postpartum
Ibuprofen
Percocet
Classification,
Action, & Use
Analgesic, antipyretic, and NSAID. Blocks prostaglandin synthesis.
Has a nonsteroidal antiinflammatory, analgesic, and antipyretic effect.
Inhibits platelet aggregation and prolongs bleeding.
Dose &
Route
Po
Inflammatory disease 400-
800mg tid or qid.
Mild to moderate pain
400mg q4-6h up to 1200.
Fever 200 –
400mg tid or qid
Narcotic analgesic. For moderate to moderately sever pain. Can be used in aspirin sensitive women
Po oxycodone hydrochloride
5mg, acetaminophen
325mg. 1-2 tablets every 4 hours prn
Tucks Pads
Dermoplast
Spray
Pads soaked in Witch
Hazel. Relieves pain of lacerations/hemorrhoids
Sparingly.
External use only
Topical Anesthetic
Numbs/relieves pain of lacerations and cuts
Sparingly.
External use only
Side Effects &
Adverse Reactions
Headache, dizziness, anxiety, drowsiness, depression, blurred vision, impaired healing, heartburn, nausea, occult blood loss, aplastic anemia, acute renal failure, rectal itching, toxic hepatitis, and anaphylaxis.
Acetaminophen: hepatotoxicity, headache, rash, hypoglycemia
Oxycodone: respiratory depression, apnea, circulatory depression, euphoria, facial flushing, constipation, suppression of cough reflex, urethral spasm, and urinary retention
Rash, irritation, burning. Cold sensation when used initially.
Rash, irritation, burning. Cold sensation when sprayed initially.
Contraindications &
Precautions
Patient in whom urticaria, severe rhinitis, bronchospasm, angioedema, nasal polyps are precipitated by aspirin and other
NSAIDS.
Caution use in people with hypertension, history of GI ulceration, and impaired hepatic renal function
Ineffective breathing pattern related to drug therapy and constipation related to slowed gastrointestinal activity
Avoid if allergic to any of its components.
Avoid if allergic to any of its components. Keep away from face.
Nursing Considerations &
Patient Teaching
Monitor therapeutic effectiveness, monitor patient for history of cardiac decompensation closely for evidence of fluid retention and edema, monitor for
GI distress and signs and symptoms of bleeding
Notify physician immediately of passage of dark tarry stools, frankly blood emesis, as well as blood or protein in the urine. Do not engage in other potentially hazardous activities until response of drug is known, avoid alcohol with this drug, do not breastfeed while taking this without notifying physician
Take with food or milk to decrease potential GI side effects of nausea/vomiting.
Determine whether a woman is sensitive to acetaminophen or codeine; has bronchial asthma, respiratory depression, convulsive disorder.
Observe women carefully for respiratory depression if given with barbiturates or sedative/hypnotics.
Consider that postcesarean-birth woman may have depressed cough reflex. Monitor bowel sounds, urine, and bowel elimination. Oxycodone is excreted in breastmilk so observe infant for sedation, GI effects, and change in feeding pattern.
Teaching should include name of drug, expected effect, possible adverse effects.
Teach may cause dizziness, drowsiness so avoid driving when taking med. Alcohol potentates effect so warn against taking it with alcohol.
Teach to apply to episiotomy, lacerations, & hemorrhoids to relieve pain and discomfort prn.
Warn pt. it feels cold when applied initially.
Teach to apply to episiotomy, lacerations, & hemorrhoids to relieve pain and discomfort prn.
Warn pt. it feels cold when sprayed.
Medications:
Postpartum
Lanolin
Ointment
RhoGAM
Classification,
Action, & Use
Ointment to keep nipples supple/soft and prevent cracking.
Rubella
Dose &
Route
Apply sparingly to nipples
Side Effects &
Adverse Reactions
Rash if allergic to anything in the ointment.
Contraindications &
Precautions
Do not use if allergic to wool.
Nursing Considerations &
Patient Teaching
Allow nipples to air dry after expressing a drop of breast milk on the end of the nipples. Apply sparingly if expressed milk not sufficient.
Prevention of sensitization to the RH factor in RH negative women and to prevent hemolytic disease in the newborn in subsequent pregnancies
Stimulate active immunity against rubella virus
One vial IM within 72 hours of birth.
Antepartal: One vial microdose
RhoGAM IM at
28 weeks in
RH- negative women, after amniocentesis, and spontaneous therapeutic abortion
Single-dose vial, inject subcutaneously in outer aspect of the arm
Soreness at injection site
Contradicted in Rho (D) positive patient, thrombocytopenia, and bleeding disorders.
Cautious use in pregnancy.
Burning or stinging at the injection site sore arm, redness at injection site, joint aches or pain; about
2-4 weeks later may have a rash, malaise, sore throat, or headache,
Pregnancy
Confirm criteria for administration is present.
Ensure correct vial is used for the patient. Inject entire content of vial
Teach name of drug, expected action, possible adverse effect, report soreness at injection site to nurse, woman should carry information regarding RH status and dates of RhoGAM injections with her at all times.
Chances of serum sickness is possible but only
~0.2% chance so teach pt. to report if they feel nauseated, or have a rash, or any change in condition after receiving injection. This medication comes from human serum.
Determine weather a woman has sensitivity to neomycin, gelatin, other immunizations, is immunosupressed, or has received blood transfusions (not to be administered within three months of transfusion). To be given at discharge
Teach name of drug, expected effect – sore arm, burns like bee sting, muscle aches/pains, slight fever, possible adverse effects, and comfort measures to use if adverse effects occur.
Rubella titer should be reassessed in about three months if
RhoGAM given at the same time because it can interfere with developing immunity to Rubella.
Instruct women to avoid pregnancy for about one month following vaccination due to potential teratogenic effects to fetus. Otain verbal agreement before giving and document.
Medications:
Postpartum
DepoProvera
Classification,
Action, & Use
Progestin contraceptives.
Provides highly effective birth control for three months when administered every 3 months.
Dose &
Route
IM injection of
150 mg
Side Effects &
Adverse Reactions
Menstrual irregularities, headache, weight gain, breast tenderness, depression, severe chest pain, leg pain, abdominal pain.
Return of fertility may be delayed for an average of nine months.
Contraindications &
Precautions
Do not use if pregnant and caution with breastfeeding.
Undiagnosed abnormal vaginal bleeding; history of or current thrombophlebitis or venous thromboembolic disorders (including
DVT, PE); active or recent (within 1 year) arterial thromboembolic disease (eg, stroke, MI); carcinoma of the breast; estrogen-dependent tumor; hepatic dysfunction or disease; pregnancy
Nursing Considerations &
Patient Teaching
Nurse makes sure that patient has chosen the best method of contraception. Provide accurate information in a non judgmental way, focus on open discussion, provide written handout identifying the warning signs and the actions a women should take.
Teach to get injection every 3 months. Depo does not protect against STD’s - need to use a barrier method for STD protection.
Prolonged use may result in the loss of bone mineral density (BMD).
The warning specifically applies to the use of medroxyprogesterone contraceptive injection. Bone density loss is related to the duration of use, and may not be completely reversible on discontinuation of the drug. The impact on peak bone mass in adolescents, as well as the loss of
BMD which accompanies pregnancy and lactation, should be considered in treatment decisions. Longterm use (ie, >2 years) should be limited to situations where other birth control methods are inadequate.
Medications:
Post/Op
Duramorph
Narcan
Zofran
Ketorolac/Tordol
Classification,
Action, & Use
Opiate, analgesic, bind with opioid receptors to alter pain.
Displaces opiates at receptor sites, reverse sedation, increase resp. rate and corrects BP
Antiemetic.
Prevention and treatment of postoperative nausea and vomiting
NSAID, analgesic, antipyretic for short-term ( 5 days) management of moderatelysevere acute pain requiring analgesia at the opioid level
Dose &
Route
10-30mg Q4hr
PO
0.4-2mg IV
I.M., I.V.:
Postoperative nausea and vomiting: 4 mg as a single dose approximately
30 minutes before the end of anesthesia, or as treatment if vomiting occurs after surgery
PO, IM
I.V.: 30 mg as a single dose or 30 mg every 6 hours
(maximum daily dose: 120 mg)
Side Effects &
Adverse Reactions
Dizziness, nausea, vomiting, hypotension, sedation, respiratory. depression, muscle flaccidity, cold skin, constipation.
NV, tremors, sweating, increase BP, tachycardia, hypo and hypertension
Constipation.
Dizziness, HA, sedation, diarrhea, dry mouth, constipation, purities, rash, malaise, fatigue, urinary retention, Overdose or toxic reactions are: sudden transient blindness, severe constipation, hypotension and if these occur give symptomatic support.
Drowsiness; HA,
Nausea, GI pain, constipation, dizziness.
Antihypertensive medications and diuretics may have a decreased effect when taking Ketorolac so monitor BP and effects of diuretics.
Contraindications &
Precautions
Not with CNS depressants, sedatives, alcohol
Respiratory depression, opiate dependent pts., cardiovascular disorders
Be aware that HA requiring an analgesic for relief is a common adverse effect
Nursing Considerations &
Patient Teaching
Check VS especially respiratory rate and report RR
< 9/min., check voiding and stools, deep breathing, assess for pain relief, no sudden movements, avoid alcohol. Teach pt. can cause drowsiness, dizziness so ask for assistance as needed.
Narcan reverses effects so have available.
Maintain clear airway, monitor VS, monitor for reoccurrence of respiratioy depression, assess for increase pain.
Be aware that HA requiring an analgesic for relief is a common adverse SE. Single doses for prevention of postoperative nausea and vomiting may be administered I.V. over 2-5 minutes as undiluted solution. May cause dizziness/drowsiness.
May increase methotrexate levels and toxicity. Muscle relaxants: Concomitant use has resulted in apnea. NSAIDs, salicylates &Probenecid:
Concomitant use increases NSAIDinduced adverse effects; contraindicated.
Watch for S&S of GI ulceration and bleeding;
Consult prescriber if breastfeeding; Do not use other NSAIDS while taking this drug. Administer
I.V. bolus over a minimum of 15 seconds; onset within 30 minutes; peak analgesia within 2 hours.
Anticoagulants: Increased risk of bleeding complications so monitor for this if patient is on anticoagulants.
Medications:
Post/Op
Nubain
Benadryl
Morphine Sulfate
Pitocin
Classification,
Action, & Use
Opiate, narcotic analgesic
Anti-histamineH1 receptor blocker allergies
Opiate analgesic
CNS agonist, binds receptors, severe pain control
Induction of labor at term; control of postpartum bleeding; adjunctive therapy in management of abortion. Produces phasic contractions
Dose &
2.5-15 mg, q4h
IV
5-20 mg, q4h IM
Side Effects &
Route Adverse Reactions
IM, IV, SO
Adults: 10 mg/70 kg every 3-6 hours; maximum single dose: 20
Nausea; Vomiting,
Sedation; Dizziness;
Sweaty, clammy skin
Constipation. mg; maximum. daily dose:160 mg
25-50 mg tid PO Drowsiness, dizziness,
Headache, nausea, and vomiting, tachycardia, nervousness, ↓ BP.
Constipation and decreased respirations
Prolongs labor
IV, nasal
Induction or stimulation of labor: Add oxytocin 10 units to NS or LR
1000 mL to yield a solution containing oxytocin 10 milliunits/mLPos tpartum uterine bleeding: Add oxytocin 10-40 units to running
I.V. infusion; maximum: 40 units/1000 mL
Edema, redness of the skin, neonatal jaundice, fetal trauma from too rapid propulsion through the pelvis. May produce antidiuretic effect (ie, water intoxication and excess uterine contractions); high doses or hypersensitivity to oxytocin may cause uterine hypertonicity, spasm, tetanic contraction, or rupture of the uterus;
Contraindications &
Precautions
Alcohol and other CNS depressants add to CNS depression, crosses placenta and can cause respiratory depression in the newborn if given too close to delivery.
Pregnancy, neonates,
Lactation, and history of asthma
Don’t administer with other narcotics
Use caution with labor
Nursing Considerations &
Patient Teaching
Watch for respiratory depression of newborn if this drug is used during labor and delivery; Excretion in breast milk unknown/use caution. Teach pt. may be dizzy, drowsy, cause fatigue-monitor for SE’s.
Ambulate because it’s anti-cholinergic Monitor cardiovascular effects. Don’t mix with other CNS depressants. Use caution with breastfeeding. May cause dizziness/drowsiness so warn pt.
Monitor pain relief and breathing closely
Monitor infant for sleepiness.
Monitor for dizziness and teach pt. to ask for help if dizzy with ambulation.
Unfavorable fetal position, fetal distress, hypertonic or hyperactive uterus, contraindicated vaginal delivery.
Severe water intoxication with convulsions, coma, and death is associated with a slow oxytocin infusion over 24 hours
Be aware of purpose and anticipated effect of oxytocin. Monitor blood pressure, fluid intake and output, and labor closely if using oxytocin for induction; fetal monitoring is strongly recommended (see Adverse Reactions).
Pregnancy risk factor X.
Note breast-feeding caution.
Must be given with infusion pump for induction of labor and uterine contractions observed for hyperstimulation and/or fetal distress. Turn off medication if this occurs and notify health care provider.
Report sudden, severe HA immediately to healthcare providers.
Medications:
L&D
Terbutaline
BiCitra
(Sodium Citrate)
Cytotec
Classification,
Action, & Use
Bronchodilator in reversible airway obstruction and bronchial asthma; tocolytic agent
Has been used prior to anesthesia induction as a preoperative antacid to prevent aspiration
PNEUMONITIS; effectiveness is controversial
Prostaglandin, cervical ripening and induction of labor
Dose &
Route
PO, SQ
Injection, solution, as sulfate: 1 mg/mL
(1 mL)
Tablet, as sulfate: 2.5 mg, 5 mg
15ml po 10-30 mins. Prior to
C/S.
PO; vaginal into cervical os
Side Effects &
Adverse Reactions
Nervousness, tremor,
HA, fatigue, seizures, tachycardia, nausea, vomiting. When used for tocolysis, there is some risk of maternal pulmonary edema, which has been associated with the following risk factors, excessive hydration, multiple gestation, occult sepsis and underlying cardiac disease. To reduce risk, limit fluid intake to 2.5-
3 L/day, limit sodium intake, maintain maternal pulse to <130 beats/minute.
Diarrhea, N/V, mild stomach pain. Black, tarry stools - Confusion
Seizures - Severe diarrhea, nausea, or vomiting - Severe stomach pain - Trouble breathing
Diarrhea, nausea, abdominal pain, vomiting, uterine contractions
Contraindications &
Precautions
Angina, stroke, HTN,
DM, kidney and liver function
Renal impairment or sodium restricted diets.
Electrolyte imbalance.
Addison's disease, diabetes, heart or kidney disease, high blood pressure, hypocalcemia, intestinal blockage, or stomach problems.
Renal impairment.
Safety in children less than 18 years is not established.
Nursing Considerations &
Patient Teaching
Keep appointments with physician for evaluation of continued drug effectiveness and clinical condition.
If pt. has diabetes, monitor blood sugar closely.
Serum glucose may be elevated. May experience nervousness, dizziness, or fatigue (use caution when driving or engaging in tasks requiring alertness until response to drug is known); or dry mouth, stomach upset (small, frequent meals, frequent mouth care, chewing gum, or sucking hard candy may help).
Report unresolved GI upset; dizziness or fatigue; vision changes; chest pain, rapid heartbeat, or palpitations; insomnia, nervousness, or hyperactivity; muscle cramping, tremors, or pain; unusual cough; or rash (hypersensitivity).
Preterm labor: Notify prescriber immediately if labor resumes or adverse side effects are noted
Monitor serum electrolytes, especially bicarbonate, in patients with renal disease.
Monitor for SE’s.
Warn it has a sweet/sour taste.
Do not breast feed while taking this drug. Can cause miscarriage in pregnant pt. Not FDA approved for induction
Medications:
L&D
Demerol
Phenergan
Classification,
Action, & Use
Narcotic
Analgesic; synthetic morphine-like compound; control of moderate to severe pain and obstetric analgesia
Antiemetic; antihistamine activity; relief of allergic conditions
& prophylaxis of motion sickness, nausea & vomiting
Dose &
Route
Obstetric=IM/SC
50-100 mg; Pain
PO/SC/
IM/IV50-150mg
Side Effects &
Adverse Reactions
Respiratory depression, convulsions, constipation, sedation, cardiovascular collapse/arrest
Contraindications &
Precautions
Contraindicated if convulsive disorder, acute abdominal condition, pregnancy prior to labor; use caution if impaired liver or kidney function
Nausea: PO/PR/
IM/IV 12.5-25 mg q4-6h
Allergic reactions: I.M.,
I.V.: 25 mg, may repeat in 2 hours when necessary; switch to oral route as soon as feasible
Onset of action:
I.M.: ~20 minutes; I.V.: 3-
5 minutes
Duration: 2-6 hrs.
Respiratory depression, agranulocytosis, blurred vision, dry mouth, drowsiness. May cause extrapyramidal symptoms, including pseudoparkinsonism, acute dystonic reactions, akathisia, and tardive dyskinesia. May be associated with neuroleptic malignant syndrome (NMS).
Contraindicated for lactation, newborn or premature infants; use cautiously if impaired liver function, cardiovascular disease, asthma, HTN
Phenothiazines may cause anticholinergic effects (constipation, xerostomia, blurred vision, urinary retention); therefore, they should be used with caution in patients with decreased gastrointestinal motility, urinary retention, BPH, xerostomia, or visual problems. Conditions which also may be exacerbated by cholinergic blockade include narrow-angle glaucoma
Nursing Considerations &
Patient Teaching
Give in smallest dose possible; note respiratory rate ; do not smoke and walk without assistance after receiving the drug; be aware of nausea, vomiting and dizziness associated with fall in BP; caution if breast feed while taking, do not take with alcohol or another CNS depressant. And causes dizziness and drowsiness.
Supervise ambulation; monitor respiratory function; relieve dry mouth by frequent rinses with water; caution if breastfeeding, avoid prolonged exposure to sun; do not drive; avoid alcohol and other CNS depressants.
Administration: I.M. Preferred route of administration; administer into deep muscle
Administration: I.V.
Due to the possibility of orthostatic hypotension, I.V. administration is not the preferred route. Solution for injection may be diluted in 25-100 mL NS or D
5
W (maximum concentration of 25 mg/mL) and infused over 15-30 minutes at a rate 25 mg/minute. Rapid I.V. administration may produce a transient fall in blood pressure
Very irritating to the vein so should be diluted in
NS and infused slowly.
Medications:
L&D
Methergine
(mrthylergonovine maleate)
Prostin
(Hemobate)
Medications:
Newborn
Vitamin K/
AquaMEPHYTON
Illotycin/
Erythromycin
Hepatitis B
Vaccine
Classification,
Action, & Use
Autonomic nervous system agent/ adrenergic agonist
Ergot-derivative
not to be administered prior to delivery of the placenta
Termination of pregnancy and refractory postpartum uterine bleeding
Classification,
Action, & Use
Vitamin, to prevent hemorrhagic disease of the newborn Newborn has a sterile bowel at birth and thus lacks bacteria necessary to make Vitamin K.
Antiinfective, antibiotic.
Given to NB’s to prevent opthalamic neonatorium
(neonatal blindness)
Antiinfective
Vaccine. Give HBIG to
NB if mom is Hepatitis
B + within 12 hrs. birth.
Dose &
Route
Uterine subinvolution:
0.2 mg IM/Very cautious with IV!
(may be repeated at 2-4 hr intervals up to 5 doses) then 0.2 mg ORALLY 3-
4 times a day
IM Adults:
Refractory postpartum uterine bleeding:
Initial: 250 mcg; may repeat at 15- to 90-minute intervals to a total dose of 2 mg
Dose &
Route
Prophyla xis: I.M.:
0.5-1 mg within 1 hour of birth
0.5% topical, inner canthus
IM 5 mcg
Side Effects &
Adverse Reactions
Nausea/vomiting, hypertensive episodes, bradycardia, allergic reactions, ergotism tinnitus dizziness, sweating – rare MI and severe hypertension.
Headache, nausea/vomiting, diarrhea, uterine rupture, dyspnea, hiccups, fever, flushing
Side Effects &
Adverse Reactions
Pain, tenderness, edema at injection site. Allergic reactions, such as rash and urticaria, may also occur.
Edema and inflammation and inability to focus.
Usually disappear in 24-
48 hrs.
Soreness at injection site, erythema, swelling, warmth, induration, irritability, slight fever
Contraindications &
Precautions
Do not take for more than 1 week
If give IV, monitor BP and HR and give over 1 minute. IV not preferred method.
Use with caution in patients with history of asthma, hypotension or hypertension, cardiovascular, adrenal, renal or hepatic disease, anemia, jaundice, diabetes, epilepsy or compromised uteri
Contraindications &
Precautions
Severe liver disease, hypersensitivity to
AquaMEPHYTON
Hypersensitivity of erythromycins.
History of allergic reactions to hep B vaccine or to any ingredient in vaccine.
Nursing Considerations &
Patient Teaching
Monitor BP, notify physician if BP suddenly increases or frequent periods of uterine relaxation,
Excretion in breast milk unknown/not recommended
Causes uterine cramping so medicate as needed for pain.
Should not be routinely administered I.V. because of possibility of inducing sudden hypertension and cerebrovascular accident
Observe carefully for reports of wheezing and chest pain, changes in BP and pulse, monitor for contractions and excessive cramping, nausea, vomiting, diarrhea, fever may result. Monitor vaginal bleeding and SE’s. Premedication with an antiemetic should be considered. Monitor effectiveness and adverse reactions. Assess knowledge/instruct patient on adverse symptoms to report. Pregnancy risk factor X.
Nursing Considerations &
Patient Teaching
Observe for generalized ecchymoses or bleeding from umbilical cord, circumcision site, GI track.
Observe for jaundice and kernicterus, especially in preterm infants. Observe for local inflammation.
Protect med from light. Give before circumcision procedure.
Instill ¼” along lower conjunctival surface of each eye starting at inner canthus. May wipe away excess after 1 minute. Effective against Gonorrhea and
Chlamydia infections.
Learn potential adverse reactions
Needs injection 0, 1, and 6 months to complete the series.






![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)

