Drugs and Dialysis
advertisement

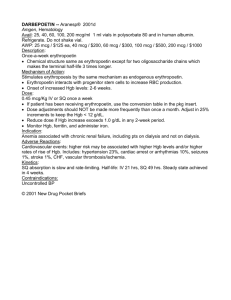
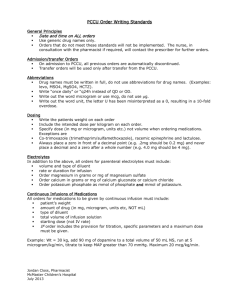
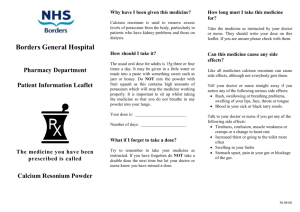
Drugs and Dialysis: Commonly Used Medications Karen Shalansky, Pharm.D. Elaine Cheng, Pharm.D. Vancouver General Hospital August 12, 2014 Typical Medication List 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Darbepoetin (Aranesp) 20 mcg IV once weekly Iron gluconate (Ferrlecit) 125 mg IV monthly Alfacalcidol 0.25 mcg PO 3X weekly TUMS Regular 2 tablets PO TID with meals Ramipril 10 mg PO once daily Metoprolol 25 mg PO twice daily Amlodipine 10 mg PO once daily Renavite 1 tablet PO once daily Docusate 200 mg PO BID Lactulose 30 mL PO HS prn Hydroxyzine (Atarax) 10 mg po HS prn Session Outline 1. 2. Darbepoetin 20 mcg IV once weekly Iron gluconate 125 mg IV monthly Anemia 3. 4. Alfacalcidol 0.25 mcg PO 3X weekly TUMS Regular 2 tablets PO TID CC CKD-MBD 5. 6. 7. Ramipril 10 mg PO once daily Metoprolol 25 mg PO BID Amlodipine 10 mg PO once daily Blood pressure 8. Renavite 1 tablet PO once daily Vitamins 9. 10. Docusate 200 mg PO BID Lactulose 30 mL PO HS prn Bowels 11. Hydroxyzine 10 mg PO HS prn Itch BC Provincial Renal Agency BC PRA provides 100% coverage of medications essential in the care and treatment of CKD patients Separate formulary for CKD Patients Not on Dialysis and Dialysis Patients Billing goes through PharmaCare first, then BC PRA picks up remainder of cost Must use a community pharmacy that has a contract with BC PRA, otherwise patient pays as per usual Pharmacare rules or non-prescription items paid in full by patient e.g. Macdonald’s Pharmacy on West 6th Avenue Anemia Management Role of Erythropoietin Decreased oxygen delivery to kidneys Renal interstitial peritubular cells detect low blood oxygen levels Erythropoietin (EPO) secreted into blood Increased oxygen delivery to tissues EPO stimulates proliferation and differentiation of erythroid progenitors into reticulocytes and prevents apoptosis More reticulocytes enter circulating blood Reticulocytes differentiate into erythrocytes (RBCs) www.anemia.org/professionals/resources/slides/ckd.ppt Anemia Target Values HEMOGLOBIN TARGET: BC = 100 to 120 g/L Hemoglobin KDOQI 2007: 110-120 g/L (Do not exceed 130 g/L) KDIGO 2012: 100-115 g/L CSN 2013: 95-115 g/L Monitor Q4-6 weeks (Minimum 2-3 weeks post dose change) Initiate ESA (erythropoiesis-stimulating agent) when Hgb < 90 g/L in CKD patients (TREAT 2009) and Hgb < 100 g/L in dialysis patients (KDIGO 2012) IRON TARGET Serum Ferritin 100-1000 mcg/L (PD/CKD) Monitor Q3months 200-1000 mcg/L (HD) (upper limit controversial) TSAT 20-50% (Same for all 3 groups) Monitor Q3months Anemia Target Values Why not higher Hgb levels? Hypertension ↑ thrombosis from altered blood viscosity No cardiovascular benefit; some improvement in QOL (CREATE 2006) ↑ mortality, non-fatal MI and hospitalization with Hgb > 130 g/L; no improvement in QOL (CHOIR 2006, NEJM 1998) stroke (TREAT 2009) Comparison of ESAs Endogenous human EPO composed of 165 amino acids, 4 carbohydrate groups and 2 disulfide bonds that maintain the shape of the molecule Epoetin alfa (Eprex®) identical to human EPO Darbepoetin alfa (Aranesp®) different from human EPO 165 amino acids but with 5 substitutions 5 vs. 3 N-linked carbohydrate chains < 22 vs. < 14 sialic acid residues 51% vs. 40% carbohydrate Comparison of ESAs Epoetin alfa (Eprex®) Darbepoetin alfa (Aranesp®) t1/2 SC 18-24 hrs 48 hrs t1/2 IV 8.5 hrs 25.3 hrs Starting dose 100 IU/kg weekly divided into 1-3x/week 0.45 mcg/kg qweekly IV and SC IV dose 30% more than SC dose IV dose = SC dose Monitoring Min 2 weeks post change Min 3 weeks post change Max Hgb 20 g/L in 4-week period 20 g/L in 4-week period Adjustment or by 25% or by 25%* *If Hgb >130 g/L - Hold Aranesp, check CBC q2weeks, restart when Hgb 125 g/L ESA Resistance EPO (Eprex®): > 300 units/kg SC or > 450 units/kg IV Darbepoetin (Aranesp®): > 1.5 mcg/kg IV/SC Causes: Blood loss Infection Iron deficiency High iPTH (> 100 pmol/L) MDS PRCA (Pure Red Cell Aplasia) Thalassemia Iron Therapy Oral Iron Products Iron Salt % Elemental Iron Elemental Iron (mg) in 300 mg Tablet Ferrous gluconate 12 36 Ferrous sulfate 20 60 Ferrous fumarate 33 99 Goal: 150-200 mg elemental iron/day Give HS to prevent interaction with calcium products Iron Therapy Intravenous Iron Products Test Dose Infusion Rate Cost Per 500 mg Dose Iron dextran (Dexiron®) Yes 100 mg/hr $84.15 Iron sucrose (Venofer®)* No 100 mg/hr $185.00 Iron Product Iron*Lower gluconate (Ferrlecit®)* No to iron 125 mg/hr $96.00 incidence of side effects compared dextran, e.g. anaphylaxis, back pain, hypotension, pruritus Ferumoxytol (Feraheme®)* (Superparamagnetic iron) No 510 mg IV over 1 min $186.00 *Lower incidence of side effects compared to iron dextran, e.g. anaphylaxis, back pain, hypotension, pruritus IV Iron Dosing Hemodialysis Patients: TSAT (%) Ferritin (mcg/L) Dose < 20 < 200 100-125 mg IV qHD x 8-10 runs (Total dose = 1 g), then 100-125 mg IV qweekly 20-34 200 – 800 100-125 mg IV qweekly or q2weeks 35-50 200 – 800 100-125 mg IV q4weeks > 50 Any value Stop iron and reassess after 3 months < 20 > 800 Depends on Hgb CKD or PD Patients: Iron sucrose (Venofer) 300 mg IV qweekly x 1-3 doses or Ferumoxytol (Feraheme) 510 mg IV q2-7days x 1-2 doses Case #1: Anemia SK 68 yo female New HD patient Wt = 58.2 kg Labs: Hgb TSAT Ferritin Sept/10 122 0.18 158 Current Meds: - Aranesp 30 mcg IV qweekly - Ferrous sulfate 600 mg po qhs What to do? Case #1: Anemia Later… Hgb TSAT Ferritin Sept/10 Dec/10 122 0.18 158 140 0.26 412 What to do? Chronic Kidney Disease – Mineral and Bone Disorder Pathophysiology Pi, Ca Renal Osteodystrophy Disorder of bone remodelling high turnover - iPTH (Osteitis Fibrosa) low turnover - iPTH (adynamic),aluminum (osteomalacia) mixed - hyperparathyroidism + defective mineralization Starts when GFR declines below 60mL/min (Stage 3) Consequences: Parathyroid gland hypertrophy ( iPTH, Ca and Pi) Metastatic calcification (Ca x PO4 precipitate) Bone pain, fractures, itching, resistance to EPO May require parathyroidectomy (iPTH > 100) CKD-MBD Targets: Stage 5 Dialysis KDOQI 2003 CSN 2006 KDIGO 2009 Calcium (N=2.1-2.55) Low normal range (preferably < 2.4 mmol/L) Normal range Normal range Avoid hypercalcemica Phosphate (N=0.8-1.45) 1.1-1.8 mmol/L Normal range Normal range iPTH (N=1.5-7.6) 16.5-33 pmol/L 10.6-53 pmol/L 2-9 times the upper limit of normal (15.2-68.4 pmol/L) Treatment Options Goals: PO4, Ca, iPTH Dietary phosphate restriction Phosphate Binders Vitamin D Analogues Calcium Salts Sevelamer hydrochloride (Renagel®) Lanthanum carbonate (Fosrenol®) Aluminum products – anemia, dementia, osteomalacia Alfacalcidol (One-Alpha®), Calcitriol (Rocaltrol®) Calcimimetic – Cinacalcet (Sensipar®) Parathyroidectomy Phosphate Binders: Calcium Salts Strength Elemental Ca++ Cost/tab TUMS Regular® 500 mg 200 mg $0.04 TUMS Extra Strength® 750 mg 300 mg $0.05 TUMS Ultra Strength® 1000 mg 400 mg $0.07 Apo-Cal® 625 mg 1250 mg 250 mg 500 mg $0.03 $0.04 Calcium acetate* 667 mg 169 mg $0.11 Calcium Salt Calcium carbonate *Calcium acetate better binder and less absorption Adverse effects: constipation, Ca, PO4 Max: 1500 mg elemental calcium/day (soft guideline) Factors Associated with Cardiac Calcification • Survey of 39 dialysis pts < 30 yrs vs. 60 normals • 36% calcification (EBT) in dialysis vs. 5% controls Ca++ Intake from Binders, mg/day Serum P, mmol/L Ca x P product, mmol2/L2 Age, years Mean Duration of Dialysis, years Coronary Calcification (N = 14) No Calcification (N=25) P value 2582 1330 0.02 2.21 2.02 0.06 5.4 4.7 0.04 26 15 < 0.001 14 4 < 0.001 New Engl J Med 2000;342:1478-83 Phosphate Binders: Sevelamer (Renagel®) Mechanism of Action Non-calcium/aluminum based Non-absorbed phosphate binder Indication (need to fill out form) Failure on calcium therapy Ca >2.6 mmol/L and PO4 >1.8 mmol/L Adverse Effects Bloating, diarrhea, pill burden Acidosis, esp if not combined with CaCO3 or calcium acetate Dose 800 mg tabs 1-5 tabs po tid (Max: 12 g/day); $1.61/800 mg Phosphate Binders: Lanthanum (Fosrenol®) Mechanism of Action Non-calcium/aluminum based Earth metal on periodic table (similar to aluminum) Minimal absorption <0.1% but some accumulation in rat bone Indication Same as for Sevelamer (Renagel®) Adverse Effects Large chewable tablet, nausea/vomiting Dose 500-1000 mg po tid (Max: 3 g/day); $3.00/750 mg Relative Potency of PO4 Binders: Aluminum/Lanthanum > Calcium acetate > CaCO3 > Sevelamer Calcium vs. Non-Calcium Based Binders Is there a mortality benefit? Cochrane Review 2011 10 RCTs: Sevelamer vs. Calcium binders No reduction in all-cause mortality (RR 0.73, 95% CI 0.46-1.16) No difference in coronary artery calcification Lancet Meta-Analysis 2013 11 RCTs: Sevelamer x 10; Lanthanum x 1 Significant reduction in all-cause mortality (RR 0.78, 95% CI 0.61-0.98) Significant reduction in coronary artery calcification at 12 months VITAMIN D METABOLISM Commercially available: Vitamin D3 (cholecalciferol) Vitamin D2 (ergocalciferol - plant) One Alpha® (alfacalcidol) - 1- cholecalciferol Rocaltrol® (calcitriol) - 1-,25 cholecalciferol Vitamin D Analogues: Alfacalcidol (One-Alpha®) and Calcitriol (Rocaltrol®) Mechanism of Action ↑ absorption of calcium Direct inhibition of iPTH release Negative feedback inhibition of parathyroid gland Indication iPTH > 65 pmol/L (Ca <2.6 mmol/L and PO4 <1.8 mmol/L) Adverse Effects ↑ Ca and ↑ PO4 Dose 0.25 mcg po 3X/week up to 1-1.5 mcg/day Calcimimetic: Cinacalcet (Sensipar®) Mechanism of Action ↑ sensitivity of iPTH gland to calcium ↓ iPTH, Ca, PO4 levels Indication (need to fill out form) Failure on vitamin D therapy (alfacalcidol) iPTH >88 pmol/L x 2 readings Not a candidate for parathyroidectomy or waiting for one Note: clinical endpoints not assessed long-term Adverse Effects Hypocalcemia, GI upset Dose 30 mg po daily ($10/30 mg) ↑ dose q4-6weeks by 30 mg/day to max 120 mg/day Onset: hours (vs. hours to day with vitamin D) Case #2: CKD-MBD 66 yo, 100 kg female on HD x 5 years AVR 2° aortic stenosis 2006 CRF 2° diabetic nephropathy Echo Oct 2010 showed Ca deposits on aortic valve Labs (May-Oct 2010) Ca 2.1-2.33, PO4 1.39-1.81, iPTH 10.9-12 Meds: Calcium carbonate 1500 mg po tid and Alfacalcidol 0.25 mcg po daily What to do? Chronic Opioids in Renal Failure Opioids Reason Appears Safe Fentanyl Methadone No active metabolites Use Carefully Hydromorphone accumulation of active metabolite (HM-3-glucuronide) Oxycodone <10% excreted unchanged in urine Codeine Morphine - 10% metabolized to morphine - Active metabolite (M-6 glucuronide) can be neurotoxic (myoclonus,sedation) - Active metabolite (normeperidine) can cause seizures Best to Avoid Meperidine J Pain Symptom Management 2004;28:497-504 Bowel Regulation Constipation Low fibre diet – fruit and vegetable restriction Limited fluid intake Limited exercise Medications – calcium and iron Treatment Stool softener – docusate 200 mg po bid Stimulant laxative – sennosides 24 mg po hs prn Osmotic laxative – lactulose 30 mL po bid prn or polyethylene glycol (PegLyte 1-4 L or Lax-A-Day 17 g/dose) AVOID: Fleet Enema (sodium phosphate), Milk of Magnesia (magnesium hydroxide), Fruitlax (High in K+ = 45 mg/15 g) Vitamins Nutritional Deficiencies Water soluble vitamins, e.g. B vitamins, vitamin C, and folic acid, are dialyzable Avoid multivitamins (fat soluble vitamins) Renavite or Replavite 1 tab po daily (B vitamins, vitamin C 100 mg, folic acid 1 mg) Vit A accumulates - associated with renal osteodystrophy Vit D ineffective – needs to be hydroxylated Zinc 10-20 mg/day x 3 months Impaired taste, impaired wound healing, hair loss Anticoagulation in Dialysis Pts Anticoagulation in Dialysis Pts Prophylaxis Heparin 5000 units SC Q12h Dalteparin 5000 units SC daily Data up to 10-30 days safe in eGFR < 30mL/min Enoxaparin 30 mg SC daily (i.e. half dose) Will accumulate with full dosing Treatment Unfractionated heparin preferred as inpatient Outpatient bridge therapy: Tinzaparin 175 units/kg SC daily (preferred over other LMWH) Target peak anti-Xa 0.6-1.5 units/mL (> 7-10 days) Antibiotic Dosing and Dialysis VA Anti-infective Comparison Card Cephalosporin Dosing in HD 1st generation Cefazolin 2 g IV qHD for MSSA Superior to vancomycin for MSSA (CID 2007) Long half-life – primarily renally eliminated Post-antibiotic effect 3rd generation Cefotaxime 2 g IV qHD Active metabolite has long half-life Alternative to Ceftriaxone, which must be dosed Q24H as primarily eliminated by liver Ceftazidime 2 g IV qHD Pseudomonas and other Gram negative organisms Vancomycin Dosing in HD ~30% vancomycin is dialyzed out Loading Dose: Maintenance Dose: 25 mg/kg if dialyzing; 20 mg/kg if no dialysis **Use goal weight** < 70 kg – 500 mg qHD; > 70 kg – 750 mg qHD Adjust dosage in increments of 250 mg Target pre-HD trough of 15-20mg/L Vancomycin Case 80 kg male on HD with MRSA CVC line infection Vancomycin dose: Duration of treatment: When to check a level: Pre-HD trough level prior to 2nd vancomycin maintenance dose is: 12 mg/L – What to do? 24 mg/L – What to do? Aminoglycoside Dosing in HD Gentamicin and Tobramycin Loading dose: 2 mg/kg **Use goal weight (round down if obese)** Treatment: 1.5 mg/kg post HD Target pre-HD trough < 3.5 mg/L Synergy or UTI: 1 mg/kg post HD Target pre-HD trough < 2 mg/L Adjust dosage in increments of 10 mg e.g. 78 kg male on HD with gram (-) bacteremia On-line References Dialysis of Drugs Handbook http://renalpharmacyconsultants.com/ass ets/2013dodbooklet.pdf Drug Prescribing in Renal Failure www.kdp-baptist.louisville.edu/renalbook/ Dialyze IHD www.dialyzeihd.com/