BACTERIAL PNEUMONIA
by
Kevin T. Martin
BVE, RRT, RCP
RC Educational Consulting Services, Inc.
16781 Van Buren Blvd, Suite B, Riverside, CA 92504-5798
(800) 441-LUNG / (877) 367-NURS
www.RCECS.com
BACTERIAL PNEUMONIA
BEHAVIORAL OBJECTIVES
UPON COMPLETION OF THE READING MATERIAL, THE PRACTITIONER WILL BE
ABLE TO:
1. Define bacterial pneumonia.
2. List three predisposing factors to bacterial pneumonia.
3. Define nosocomial pneumonia.
4. List three types of patients who are at especially high risk for contracting bacterial
pneumonia.
5. List and define the four types of bacterial pneumonia.
6. Describe the most common physical presentations of the patient with bacterial pneumonia.
7. Summarize the laboratory findings which would indicate a bacterial infection.
8. Describe the radiologic findings of bacterial pneumonia.
9. List the three major foci in the treatment of pneumonia.
10. Briefly summarize the findings in atypical pneumonia syndrome.
11. Explain the pathology of ventilator-associated pneumonia.
COPYRIGHT © 1991 By RC Educational Consulting Services, Inc.
COPYRIGHT © April, 2000 By RC Educational Consulting Services, Inc.
(# TX 0-480-589)
Authored by: Kevin T. Martin, BVE, RRT, RCP
Revised 1994, 1997 by Kevin T. Martin, BVE, RRT, RCP
Revised 2001 by Susan Jett Lawson, RCP, RRT-NPS
Revised 2004 by Helen Schaar Corning, RRT, RCP
Revised 2007 by Michael R. Carr, BA, RRT, RCP
ALL RIGHTS RESERVED
This course is for reference and education only. Every effort is made to ensure that the clinical
principles, procedures and practices are based on current knowledge and state of the art
information from acknowledged authorities, texts and journals. This information is not intended
as a substitution for a diagnosis or treatment given in consultation with a qualified health care
professional.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
2
BACTERIAL PNEUMONIA
TABLE OF CONTENTS
DEFINITION AND INTRODUCTION ........................................................................................ 6
TYPES OF BACTERIAL PNEUMONIA ..................................................................................... 6
Community Acquired................................................................................................................ 6
Hospital Acquired ..................................................................................................................... 7
Typical ...................................................................................................................................... 7
Atypical..................................................................................................................................... 8
PATHOLOGY ............................................................................................................................... 8
Pathogenic Mechanisms Responsible For Pneumonia ............................................................. 9
PREDISPOSING FACTORS ..................................................................................................... 10
Nosocomial Pneumonia .......................................................................................................... 11
Neisseria Meningitidis ............................................................................................................ 11
High Risk Situations In The Hospital ..................................................................................... 12
Predisposing And High Risk Factors Of Nosocomial Pneumonia ......................................... 13
DIAGNOSIS ................................................................................................................................ 14
HISTORY AND CLINICAL PRESENTATION ........................................................................ 14
History..................................................................................................................................... 16
Physical................................................................................................................................... 16
LABORATORY EVALUATION ............................................................................................... 17
Laboratory Studies .................................................................................................................. 18
INVASIVE DIAGNOSTIC TECHNIQUES ............................................................................... 18
Invasive Diagnostic Procedures.............................................................................................. 19
RADIOLOGIC EVALUATION.................................................................................................. 19
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
3
BACTERIAL PNEUMONIA
Imaging Studies....................................................................................................................... 20
Chest X-Ray............................................................................................................................ 20
CT Scan................................................................................................................................... 20
Diagnosis Of Pneumonia ........................................................................................................ 20
TREATMENT ............................................................................................................................. 21
Antibiotics ............................................................................................................................... 21
Summary Of Antibiotic Therapy For Bacterial Pneumonia ................................................... 22
Correction Of Reversible Patient Abnormalities .................................................................... 23
Supportive Care....................................................................................................................... 23
Treatment Of Pneumonia ........................................................................................................ 24
COMPLICATIONS ..................................................................................................................... 24
Additional Complications Of Bacterial Pneumonia ............................................................... 25
TREATMENT AND CLINICAL MANISFESTATION OF STREPTOCOCCUS
AND STAPHLOCOCCUS PNEUMONIA ................................................................................. 25
STREPTOCOCCUS PNEUMONIA (PNEUMOCOCCUS) - (TYPICAL PNEUMONIA) ....... 25
Clinical Manifestation............................................................................................................. 26
Treatment ................................................................................................................................ 27
STAPHYLOCOCCUS AUREUS - (TYPICAL PNEUMONIA) ................................................ 27
Clinical Manifestation............................................................................................................. 29
Treatment ................................................................................................................................ 29
HEMOPHILUS INFLUENZA - (ATYPICAL PNEUMONIA).................................................. 30
Clinical Manifestation............................................................................................................. 30
Treatment ................................................................................................................................ 31
KLEBSIELLA PNEUMONIA - (HOSPITAL ACQUIRED) ..................................................... 31
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
4
BACTERIAL PNEUMONIA
Clinical Manifestation............................................................................................................. 31
Treatment ................................................................................................................................ 32
PSEUDOMONAS AERUGINOSA - (HOSPITAL ACQUIRED).............................................. 32
Clinical Manifestation (Nonbacterial vs bacterial) ................................................................. 33
Treatment ................................................................................................................................ 34
Anaerobic Bacteria.................................................................................................................. 34
Clinical Manifestations ........................................................................................................... 34
Microbiological Diagnosis ...................................................................................................... 35
Treatment ................................................................................................................................ 35
Prevention ............................................................................................................................... 36
ATYPICAL PNEUMONIA SYNDROME ................................................................................. 36
Epidemiology.......................................................................................................................... 36
Clinical Manifestations .......................................................................................................... 36
Treatment And Prevention...................................................................................................... 37
VENTILATOR-ASSOCIATED PNEUMONIA ......................................................................... 37
Diagnosis In The Mechanically Ventilated Patient ................................................................ 38
CLINICAL PRACTICE EXERCISE .......................................................................................... 39
SUMMARY................................................................................................................................. 39
PRACTICE EXERCISE DISCUSSION...................................................................................... 40
SUGGESTED READING AND REFERENCES ....................................................................... 42
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
5
BACTERIAL PNEUMONIA
DEFINITION AND INTRODUCTION
P
neumonia is an acute inflammation of the pulmonary parenchyma caused by bacteria,
viruses, mycoplasma and other agents. According to recent Center for Disease Control
(CDC) reports, pneumonia is the fourth leading cause of death in geriatric patients in the
United States. There are over three million cases of pneumonia per year in the U.S.
Pneumonia (nosocomial) is responsible for the greatest mortality of patients in hospitals, at a rate
ranging from 30% to 60%. This pulmonary infection accounts for approximately 50,000 deaths
per year. Nosocomial pneumonia occurs in approximately 27% of patients on mechanical
ventilation.1 Approximately 12-29% of critically ill, hospitalized patients develop pneumonia.
Around 50-60% of ARDS patients develop some form of pneumonia. This course is primarily,
but not limited to discussing bacterial pneumonia, since it is the one most often encountered in
the acute care setting.
Bacterial pneumonia is caused by a pathogenic infection of the lungs from bacteria.
Streptococcus pneumoniae is the most common source of bacterial pneumonia.2 Bacterial
pneumonia is also the most common fatal nosocomial (iatrogenic) infection. Most fatalities of
bacteremic pneumonia occur in less than 7 days. Survivors are hospitalized 3 weeks or more.
Pneumonia is more likely to occur in the winter months, when upper and lower track respiratory
infections caused by viruses precipitate a bacterial superinfection. There is a higher incidence in
males than in females. The elderly are at a higher risk due to fewer defenses against aspiration
and less receptive immune responses.
TYPES OF BACTERIAL PNEUMONIA
T
here are four types of bacterial pneumonia based upon how it is acquired and its clinical
course. Bacterial pneumonia may be community or hospital-acquired. The clinical
course can take a typical or atypical path. I use this classification system for the following
discussion. Others choose to use a classification system based upon the type of host and nature
of the organism. This system also delineates four types of pneumonia: normal/abnormal host
and usual/unusual organisms. The former refers to whether the host (patient) has normal, or
abnormal defense mechanisms against infection, the latter is self-explanatory. “Usual”
organisms consist of Streptococcus pneumoniae (pneumococcus), Hemophilus influenzae,
Chlamydia species, Mycoplasma pneumoniae, or common viruses. “Unusual” organisms consist
of Legionella pneumophila, Mycobacterium tuberculosis, Bacillus anthracis, group A betahemolytic streptococcus, Meningococcus, and endemic fungi.
Another classification system in the causes for development of pneumonia is extrinsic and
intrinsic differentiation. Extrinsic includes exposure to the causative agent, exposure to
pulmonary irritants or direct pulmonary injury. Intrinsic factors are related to the host only.
(1) Community Acquired - The patient usually presents with a cough, fever and consolidation
on the chest x-ray (CXR) with community-acquired pneumonia. Pneumococcus is probably the
most common causative agent. This type of pneumonia generally responds readily to treatment
and causes few serious problems. Approximately 95% of normal adults with community
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
6
BACTERIAL PNEUMONIA
acquired pneumonia have “usual” organisms.
(2) Hospital Acquired - Nosocomial or iatrogenic pneumonia accounts for about 15% of all
hospital-acquired infections, and 31% of those in ICU. An average 27% of mechanically
ventilated patients and 12-29% of ICU patients acquire nosocomial pneumonia. Nosocomial
pneumonia is responsible for up to 33% of all nosocomial deaths.1 It increases hospital length of
stay from 4-13 days and is the most expensive infection by site. About 60% of nosocomial
pneumonias are gram-negative organisms. The most common organisms, which comprise 50%
of isolates from cultures of respiratory tract specimens, include: Pseudomonas aeruginosa,
Klebsiella pneumoniae, Enterobacter species, Escherichia coli, Serratia marcescens, and Proteus
species. However, gram-positive cocci have emerged recently as isolates, with increasing
frequency. Gram-positive cocci causing concern include Staphylococcus aureus, and
Streptococcus pneumoniae.
The integrity of the pulmonary defenses is a critical factor in assessing the risk for nosocomial
pneumonia. Severe underlying disease makes a patient very high-risk for nosocomial
pneumonia. Those in ICU, intubated, and mechanical ventilated are an even higher risk.
Immunodeficiency states (neutropenia, hematologic malignancy, immunosuppression therapy,
AIDS) are susceptible to a wide variety of pathogens thereby increasing the risk of nosocomial
pneumonia.
Once the diagnosis of pneumonia is suspected on a patient, a sputum and blood culture should be
obtained. Empirical therapy can be instituted based upon gram stain results and the
susceptibility patterns for organisms in the particular institution. A note of caution is warranted
with decisions based on sputum cultures. Sputum cultures reveal the causative agent of
pneumonia only around 50% of the time.
(3) Typical - Streptococcus pneumoniae is the most common typical pneumonia. Hemophilus
influenzae and Klebsiella pneumoniae have an identical clinical picture to streptococcus. All
begin with an abrupt onset of fever and shaking chills. A productive cough of purulent sputum is
also common and, patients complain of pleuritic chest pain. Patients may have had symptoms of
an upper respiratory infection prior to the pneumonia. Elderly and debilitated patients may also
be hypothermic.
Physical examination of a typical pneumonia patient reveals consolidation with dullness to
percussion. The patients’ white blood count (WBC) is usually increased, but can be normal or
low, particularly in the COPD or immunodeficient patient. An increase in immature white blood
cells and toxic granulations are usually found. Sputum gram stains show many white blood cells
and predominant bacteria, indicative of the causative organism. A predominant and/or causative
organism may not be present if the patient has taken antibiotics before the test.
The CXR confirms consolidation and may show a variety of findings that include
bronchopneumonic infiltrates and/or interstitial infiltrates. Pleural effusions are common on
CXR but usually small in volume. Cavitation of the lung is unusual but suggests staphylococcus
aureus or endocarditis (particularly in IV drug users), gram-negative bacilli, or a mixed
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
7
BACTERIAL PNEUMONIA
anaerobic infection. Other causes of cavitation include mycobacterium tuberculosis,
malignancies, and aocardiosis. Hemophilus influenzae produces a multilobar or segmental
consolidation and a large pleural effusion may rapidly accumulate. Klebsiella pneumoniae is
characterized by accumulation of large amounts of inflammatory exudate. The CXR often
reveals upper lobe consolidation, abscess formation, and bulging interlobular fissures.
Aspiration pneumonia develops in the pulmonary segments that were dependent when the
aspiration occurred. Pleural effusion and eventual cavitation are common in these patients.
Patients presenting with symptoms indicating a typical bacterial pneumonia should be assumed
to have pneumococcal disease until proven otherwise. This organism accounts for the majority
of pneumonias in this category. Penicillin is recommended for treatment but erythromycin may
be substituted. Many strains have become resistant to traditional antibiotics. (Individual
organisms and medications are discussed in detail later).
(4) Atypical - This differs from typical pneumonia in several respects. The onset is insidious
and headache, sore throat, muscle pain, and fatigue are common. Fever is present, but chills are
uncommon. Physical examination reveals scattered rhonchi or crackles. Evidence of
consolidation is minimal or absent. Sputum examination shows neutrophils but few organisms.
The WBC may be slightly elevated and the blood culture negative.
Mycoplasma pneumoniae accounts for the majority of atypical cases in the United States.
Respiratory viruses, legionella species and other unusual organisms account for the remainder.
The CXR in mycoplasma pneumonia may show a subsequent infiltrate in the lower lobes or a
diffuse reticulonodular interstitial infiltrate. The CXR in legionella infections is more variable
and may progress dramatically.
PATHOLOGY
he first phase of pneumonia is the invasion of body tissues. It is important to note that
invasion, not simply contamination or colonization, is the key word. Many patients are
contaminated, but invasion does not take place. These cases do not progress to pneumonia
because invasion of body tissues requires bacterial adherence to host cells. Severe illness,
malnutrition, surgery, and intubation enhance adherence and aid invasion. Some invading
organisms have an increased affinity for particular types of host cells. For example,
Pseudomonas, has a higher affinity for tracheal and lower respiratory tract cells than cells of the
upper respiratory tract. Therefore, it is more likely to cause pneumonia than an upper respiratory
infection. The initial invasion of tissue is usually from a few bacteria that multiply rapidly. This
results in numerous body responses.
T
Lymph cells within the tracheobronchial (TB) tree begin producing and secreting
immunoglobulins (antibodies) into respiratory tract secretions. Additional immunoglobulin is
transferred from the bloodstream to the respiratory tract. Immunoglobulin G (IgG) and
immunoglobulin A (IgA) coat the invading organism. The process of coating this organism with
immunoglobulin aids in its attachment to the surface of a macrophage. This procedure is known
as Opsonization. Opsonization enhances phagocytosis by alveolar macrophages.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
8
BACTERIAL PNEUMONIA
Alveolar macrophages begin releasing chemotactic materials to cause an influx of edema fluid in
the area. This is followed by migration of leukocytes (WBC’s) and erythrocytes (RBC’s) into
the lung. A leukocyte-rich exudate therefore forms in the alveolus.
The leukocytes begin phagocytosis by compressing invading bacteria against the alveolar wall or
other leukocytes. Cytoplasmic pseudopods are then extended to surround and ingest the foreign
organism.
Several distinct zones gradually develop within the alveolus during this process. The lowermost
zone is filled with dead bacteria, leukocytes, and fibrin. The middle zone contains active
bacteria and leukocytes conducting phagocytosis. The upper zone is primarily edema fluid. This
upper zone supports further bacterial multiplication. These zones are similar to battlefields. The
middle zone is where the battle is currently raging. The upper zone is where the bacteria have
control and the lower zone is where the leukocytes have control. The entire process is enhanced
by the appearance of a specific antibody (such as IgG or IgA) to the invading organism. This
intensifies the body’s response. When the invasion is stopped, resolution begins in the lower
zone with absorption of fluid.
During the acute phase the affected area remains perfused but there is no gas exchange. A rightto-left shunt exists, resulting in a decrease in PaO2 . If the ventilatory reserve is normal,
remaining areas are hyperventilated. This results in a decrease in PaCO2 . However, if the
patient is unable to compensate for the loss of consolidated alveoli, the PaCO2 increases, and can
result in respiratory failure. On any given patient, the effect on arterial blood gases is related to
the extent of consolidation and ventilation of the remaining lung area.
Initially, the consolidated area is firm, airless, and reddish in color. This is commonly referred to
as the “red hepatization” stage. These alveoli are filled with RBC’s, fibrin, and contain relatively
few leukocytes (primarily neutrophils). Alveolar capillaries are congested around consolidated
areas in the red hepatization phase.
In the “grey hepatization” stage, consolidation composition changes to many neutrophils and
relatively few RBC’s in the alveoli. The capillaries are less congested and phagocytosis
continues. The alveolar exudate begins to loosen and be disposed of via coughing. Fluid is
readily reabsorbed through the alveolar wall. However, larger exudative particles and molecules
cannot be absorbed back through the alveolar wall. These larger particles/molecules often
become scar tissue. Therefore, fibrosis, hyaline membranes, abscess, and loss of lung
parenchyma may remain following resolution of pneumonia.
Pathogenic Mechanisms Responsible for Pneumonia:
•
Aspiration of colonizing organisms in the oropharynx can result in aspiration
pneumonia, Nosocomial pneumonia, and community-acquired bacterial pneumonia.
•
Inhalation of aerosolized infectious particles can result in Tuberculosis,
Legionellosis, Histoplasmosis, Cryptococcosis, Blastomycosis, Coccidiodomycosis,
Aspergillosis, or Q fever.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
9
BACTERIAL PNEUMONIA
•
Direct inoculation of infectious organisms into the lower airway can result in
nosocomial pneumonia.
•
Spread of infection from the blood to the lungs can result in S. aureus pneumonia, or
parasitic pneumonia.
•
Spread of infection from adjacent structures to the lungs can result in mixed
anaerobic and aerobic pneumonia, or amebic pneumonia.
•
Reactivation of a latent infection (usually occurs in immunocompromised patients)
can result in Reactivation tuberculosis, P. carinii pneumonia, or cytomegalovirus.4
PREDISPOSING FACTORS
P
redisposing factors to pneumonia are related to virulence of the organism and deficiencies
in the patient’s immunity, particularly lung immunity.
The presence of a protective polysaccharide capsule surrounding the organism increases its
virulence. Organisms with such a capsule require a specific immunoglobulin for phagocytosis to
occur readily. Without such a specific immunoglobulin, phagocytosis is impaired and bacterial
multiplication proceeds rapidly. Streptococcus pneumoniae is an example of an organism with a
polysaccharide capsule. Other organisms produce toxins, such as, coagulase and leukocidin,
making them more virulent. These toxins delay phagocytosis and may be toxic to leukocytes.
Staphylococcus is an example of such an organism. It produces both coagulase and leukocidin
along with other toxins.
Many deficiencies of patient immunity are possible. There can be an overall deficiency or a
specific lung deficiency. General deficiencies include: debilitation, malnutrition, chronic
diseases, alcoholism, smoking, immunosuppressive therapy and hypogammaglobinemia or
disgammaglobinemia. These general deficiencies make a patient more susceptible to any
infection. Specific lung deficiencies make the lung more susceptible to infection. For example,
a deficiency in lung IgG means no opsonization of invading bacteria. Therefore, there is little
phagocytosis and bacterial multiplication is unhindered.
Infection is also more likely if the respiratory epithelium is damaged from acute or chronic
pulmonary disease. An upper respiratory tract infection (URI) or previous pulmonary disease
therefore make invasion more likely. Intubation renders all the upper airway defenses useless so
it obviously predisposes to pneumonia.
There are numerous other predisposing factors to pneumonia. Diabetes and chronic renal disease
also lower one’s defenses. Travel and/or exposure to wild animals can predispose to tularemia,
plague, or psittacosis. Alcoholic intoxication, stroke and other conditions that disrupt the normal
glottic reflexes increase the amount of aspirated material during sleep. Even small amounts of
aspirated material can produce a chemical or bacterial pneumonia. Most people aspirate minute
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
10
BACTERIAL PNEUMONIA
amounts of oral secretions during sleep that causes no problems. Neurological impairment
increases the amount and can result in pneumonia.
Nosocomial Pneumonia - Nosocomial pneumonia has additional predisposing factors to those
listed above. Intubation and mechanical ventilation increase the risk of a hospital-acquired
pneumonia considerably. The risk increases significantly after three days of intubation.
Thereafter, the rate of infection increases approximately 1% per day for each day of intubation.
Frequent changes of tubing attached to the airway are associated with an increased incidence of
infection. In the past it was believed that frequent changes of contaminated tubing prevented
infection. This has been proven false. The more frequently the circuit is “opened” from circuit
changes, suctioning, or other procedures, the greater the risk of infection.
Critical Care Unit patients have a higher incidence of nosocomial pneumonia, particularly those
in surgical intensive care. These patients are more likely than the general hospital population to
develop pneumonia. Additional factors are advanced age (more than 65 years old),
inappropriate antibiotic or antacid therapy. The latter increases gastric pH allowing an increase
in gastric colonization. If aspiration occurs, there is a significant increase in the number of
organisms present. Nasogastric feeding and continuous enteral feeding are additional risk factors
for nosocomial pneumonia. Patients often aspirate subclinical amounts of tube feedings over
extended periods. This leads to pneumonia.
Neisseria Meningitidis - This is an unusual and sporadic cause of pneumonia, but is welldocumented as a cause of epidemic pneumonias, particularly among military recruits. Five to ten
per cent of asymptomatic individuals transiently carry neisseria in the nose. Transmission is
mainly through aerosol droplets, but direct hand contact also may be a means of transmission.
Neisseria is an aerobic, oxidase-positive, gram-negative, diplococcus. It will not survive drying
or exposure to cold, so rapid processing of specimens is essential. Blood, cerebrospinal fluid,
and pleural fluid rarely yield the organism. Diagnosis depends upon a sputum or TTA specimen.
TTA is the most appropriate way to document invasive infection. If an epidemic is present,
recovery from expectorated sputum is sufficient for diagnosis. Clinical course and prognosis for
neisseria pneumonia are excellent. There are few deaths and the incidence of empyema or
septicemia is low.
Clinical manifestation is of URI, fever, chills, productive cough, and chest pain at the onset.
Pharyngitis and scattered crackles are typical. Frank consolidation occurs, particularly in the
right lower and middle lobes. Neisseria infection is usually confined to the lungs. The CXR
shows a lower lobe bronchopneumonia, or in some cases, multilobar involvement. Pleural
effusion occurs in about 20% of patients.
Aqueous penicillin G is again the therapeutic choice. In adults, 4-6 million units given IV for 10
days is recommended. The dose should be increased to 20 million units per day for septicemia
or meningitis. Chloramphenicol is used for those allergic to penicillin. Some types of neisseria
are resistant to sulfonamide antibiotics. Patients should be placed in respiratory isolation for the
initial days of treatment. Chemoprophylaxis with rifampin, 600 mg twice daily for 2 days, is
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
11
BACTERIAL PNEUMONIA
advisable for those with close contact with the patient.
High-Risk Situations In The Hospital - There are several high-risk situations for bacterial
pneumonia that are worth mentioning. Granulocytopenia, corticosteroid therapy, bone marrow,
heart or renal transplantation, dental procedures, antibiotics, and autoimmune deficiency
syndrome (AIDS) put a patient in a high-risk category for pneumonia. Lower respiratory tract
infections in these patients are a common cause of morbidity and mortality.
Granulocytopenia is a frequent complication of treatment for malignancies. A low granulocyte
count also can be the result of primary disease. Patients may be selectively or completely
immunodeficient. Since there is a decrease in the systemic supply of phagocytic cells, the lungs
lack these cells when pneumonia develops. Therefore, there are no granulocytes to attract into
the site of infection. The lung must rely solely on the alveolar macrophages for phagocytosis.
This gives the infection more time to become established, since there are fewer cells fighting it.
A granulocyte (neutrophils, eosinophils, basophils) count less than 1000 cells/cu mm is a highrisk situation. The incidence of infection and mortality is directly related to the decrease in the
number of granulocytes. Empirical therapy with antipseudomonal penicillin or cephalosporin
and an aminoglycoside should be instituted for pneumonia after appropriate cultures have been
obtained in these patients. Antibiotics with bactericidal activity should be used and an
antistaphylococcal agent is recommended. Relapses occur if the antibiotic is discontinued before
the granulocytes have recovered. A relapse can occur even if the patient has clinically improved.
One must note the chest X-ray may underestimate the severity of the infection because the
inflammatory response is decreased in these patients. Vascular congestion, fluid migration, and
consolidation do not show up on the CXR as readily as with other patients since they have a
minimal inflammatory response.
Corticosteroid therapy increases the risk of all infections. Corticosteroids impede the migration
of white blood cells into the infection site, decrease phagocytosis by macrophages, and interfere
with white blood cell chemotaxis. Obviously, this increases the possibility of pneumonia.
Steroids also interfere with lysosomal enzymes released from white blood cells and
macrophages. This decreases their ability to kill the invading organism. Cytotoxic drugs used
for malignancies also decrease the inflammatory response. They impede development of
immunoglobulin-producing cells that manufacture antibodies. Radiation therapy can have the
same effect.
Pulmonary complications are a frequent complication in bone marrow transplantation. If
interstitial infiltrates develop within two weeks of the transplant, it may be a toxic reaction to
radiation or chemotherapy. Some patients develop a fatal, progressive interstitial infiltrate from
two weeks to several months after the transplant. These are usually due to cytomegalovirus
(CMV). Cytomegalovirus is often the cause of progressive interstitial pneumonia in heart and
renal transplants. There is also a high mortality in these patients.
Recent dental procedures and/or antibiotic use predispose to pneumonia. Dental procedures
introduce many organisms into the lower respiratory tract. Antibiotics give opportunistic
pathogens a chance to cause infection by reducing competing pathogens. Malignancy,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
12
BACTERIAL PNEUMONIA
particularly with poor nutrition, is associated with decreased cell-mediated immunity and an
increase in infection that may result in pneumonia. Lymphoproliferative disorders and other
immune deficiency states are also predispose to pneumonia from opportunistic pathogens.
The incidence of pulmonary complications in patients with autoimmune deficiency syndrome is
high. Approximately 65% of AIDS patients develop pneumocystis carinii pneumonia.
Approximately 70% of these patients survive the first episode if treated with trimethoprimsulfamethoxazole or pentamidine. Prompt diagnosis and treatment are therefore critical. The
relapse rate is around 20% for these patients and mortality increases with successive infections.
Transbronchial biopsy and bronchoalveolar lavage (BAL) detect pneumocystis in 100% of AIDS
patients. Sputum inductions are effective 50% of the time in detection. Pneumococcal
pneumonia with bacteremia and tuberculosis also are increased in AIDS.
Predisposing And High Risk Factors Of Nosocomial Pneumonia:
•
Over age 65
•
HIV or AIDS
•
Kidney disease
•
Cancer
•
Organ and tissue transplantation
•
Taking immunosuppressive medications
•
Have a weak immune system from any cause
•
Acute or chronic disease such as pulmonary disease, heart disease, or diabetes
•
Intubation
•
Debilitation
•
Malnutrition
•
Alcoholism
•
Granulocytopenia
•
Recent dental procedures
•
Recent antibiotic use.2
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
13
BACTERIAL PNEUMONIA
DIAGNOSIS
E
PIDEMIOLOGY - Geographical data, seasonal timing and/or a history of occupational or
unusual exposures may be critical for determining etiology. A history of travel to
Southeast Asia raises the possibility of melioidosis (an infection caused by the gramnegative bacillus). Rural areas suggest exposure to zoonotic pneumonias. An important
difference between hospital and community-acquired pneumonias to note is that the former is
less likely to be pneumococci or mycoplasma. Hospital-acquired pneumonia is more likely to be
staph aureus or enteric gram-negative bacilli.
Unlike viral pneumonia, bacterial pneumonia shows little seasonal variation. An exception is
those that occur as a complication of a preceding viral infection. Influenza is typically involved,
but measles, rubella, and varicella are reported to precede beta-hemolytic streptococcus,
particularly in pediatric patients. Contact with birds suggests psittacosis and contact with wild
animals raises the possibility of tularemia or plague. A simultaneous or recent illness among the
family is not commonly seen with a bacterial pneumonia. Such a history may indicate
mycoplasma or a virus. Occupational history provides information on exposure to animals,
animal products, or specific pathogens. The latter is particularly important for lab workers.
HISTORY AND CLINICAL PRESENTATION
A
ge, underlying illnesses, and social habits predispose a patient to specific types of
pneumonia. Chlamydia trachomatis is found primarily in neonates, mycoplasma in older
children and young adults, and gram-negative bacilli predominate in the elderly.
Bacterial pneumonias increase frequently in patients with underlying medical conditions. COPD
patients are predisposed to staphylococcus pneumoniae and hemophilus influenzae infections.
Alcoholism predisposes to anaerobic lung abscess and IV drug use to bacteremic staphylococcus
pneumonia. Staphylococcus aureus is most likely the causative agent in diabetics, renal or liver
failure, influenza, cystic fibrosis, and in defects of the skin continuity. Enterobacter and
pseudomonal organisms cause lung infections in the chronically debilitated/hospitalized,
immunosuppressed, intubated, or those who have had prior broad-spectrum antibiotics. A classic
history for pneumococcal pneumonias includes the sudden onset of chills, pleuritic chest pain,
dyspnea, and rusty sputum. A classic legionella pneumonia produces diarrhea, fever, headache,
confusion and muscle pain.
The physical examination should be thorough. The exam should include looking for the
complications of pneumonia also. These include pleural effusion, pericarditis, endocarditis,
meningitis, and brain abscess. Begin with an evaluation of heart rate. Normally, the pulse
increases approximately 10 per minute for each degree (Celsius) increase in temperature. The
presence of a “bradycardia” relative to the amount of fever is associated with legionella,
psittacosis, mycoplasma and tularemia. Fever is usually present around the clock but peaks
between 6-10 PM. Pseudomonas, miliary tuberculosis, typhoid fever and brucellosis peak
between 6-10 AM. Temperature for gram-negative pneumonias are high. (Pseudomonas
infections average 103.6o F). Fever usually persists for 1-2 weeks in uncomplicated cases. The
elderly, those in shock, or who have myxedema (cretinism) may have no fever. Rigors or severe
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
14
BACTERIAL PNEUMONIA
shaking chills may suggest pneumococcal pneumonia more often than the other bacterial
pathogens.
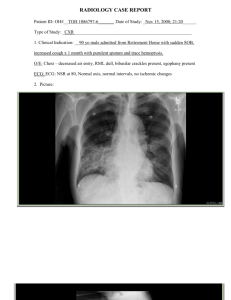
Pneumococcal Pneumonia (Right Middle Lobe)
The persistence of fever and leukocytosis with patients on appropriate antibiotics usually indicate
a complication, such as, empyema or abscess. The persistence of fever is not as important as its
slope. The peak temperature every 24 hours provides an objective measurement of the severity
of the infection. The slope over several days indicates the improvement or worsening of the
pneumonia.
Any severe pneumonia associated with necrosis of the alveoli can produce hemoptysis. It is
rarely life-threatening. Most often, the sputum is merely blood-streaked. Most cases involving
hemoptysis are a result of gram-negative organisms.
The color of the sputum provides diagnostic information. Rust-colored or blood streaked sputum
is produced by pneumococcus. Klebsiella produces brick-red, tenacious, gelatinous (currant
jelly) mucus. Staphylococcal pneumonias produce a salmon-pink or cream-colored sputum.
Pseudomonas, Haemophilus and Pneumococcus may produce green sputum. The sputum in
anaerobic infections may be foul-smelling. Influenza viruses produce blood-tinged sputum.
It is difficult to diagnose pneumonia in the severely ill. Pneumonia must be differentiated from
other conditions that cause cough, decreased blood gases, and an abnormal CXR. The
differential diagnosis includes: pulmonary embolism with infarction, adult respiratory distress
syndrome (ARDS), atelectasis, and fluid overload, to name a few. The appearance of a new
organism on the gram stain, or an increased purulence of sputum associated with a fever and
other respiratory signs, suggest a pneumonia in the critically ill. The WBC is not always helpful
in these patients. The WBC may be normal or low in some patients, such as, those on
immunosuppressive therapy or the COPD patient.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
15
BACTERIAL PNEUMONIA
HISTORY
•
Character of sputum
•
Rigors and chills
•
Headache
•
Malaise
•
Nausea, vomiting and diarrhea
•
Myalgia
•
Exertional dyspnea
•
Pleuritic chest pain
•
Abdominal pain
•
Anorexia and weight loss
PHYSICAL
•
Fever
•
Tachypnea
•
Tachycardia or bradycardia
•
Cyanosis
•
Decreased breath sounds
•
Wheezes, rhonchi and rales
•
Egophony on auscultation
•
Pleural friction rub
•
Dullness to percussion
•
Altered mental status
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
16
BACTERIAL PNEUMONIA
LABORATORY EVALUATION
T
he WBC helps separate atypical pneumonia from the more typical bacterial pneumonia.
A normal or minimal increase in the WBC is compatible with atypical pneumonia
(mycoplasma, psittacosis, around the clock fever and nonbacterial pneumonia). There is a
marked increase in the WBC with pneumococci, Hemophilus and gram-negative bacilli.
However, overwhelming infection also can result in a lower than normal WBC (leukopenia). It
is also important to note the WBC may not rise significantly in the COPD patient with
pneumonia. Therefore, one should not rule out pneumonia in a patient, particularly one with
COPD, based upon low WBC results. Neutrophilia is the norm in bacterial pneumonias but
eosinophilia occurs in coccidioidomycosis. Legionnaires disease can cause an abnormality of
liver enzymes, electrolytes, and urinalysis.
The recovery of the pathogen is important to verify the clinical diagnosis and optimize therapy.
Specimens need to be obtained before initiation of antibiotic therapy, if possible. Blood samples
and pleural fluid specimens (if present) should be obtained on hospitalized patients. If
meningitis is a possibility, CSF fluid should be obtained. A positive culture usually establishes a
specific diagnosis. However, the yield is less than 20% for all cases of bacterial pneumonia with
the above specimens, depending upon the specific etiology. Microbiological diagnosis is usually
dependent upon recognition of the pathogen in the sputum.
Examination of expectorated sputum is the easiest and least invasive method of diagnosis.
However, there are a number of problems with expectorated sputum. They include inability to
get an adequate specimen, contamination with oral flora, and the unsuitability of the specimen
for anaerobes. The first two are minimized with careful lab screening and specimen collection
techniques.
If expectorated sputum is believed to be representative of the lower respiratory tract, it should be
gram-stained. A predominant flora may be identified when examined under 1000x
magnification.
Other procedures are used to detect specific organisms or microbial antigens. These include:
coagglutination, latex agglutination, counterimmunoelectrophoresis, the quellung reaction,
monoclonal antibody reagents and DNA probes. However, a gram stain of the sputum provides
reliable presumptive information if it is done before antibiotics are started.
A sputum culture yields definitive information, assuming the specimen is actually sputum and
has been cultured properly. Many organisms are lost if the specimen is not processed quickly,
even if refrigerated. Sputum cultures are also unreliable for anaerobes due to the profuse amount
of normal aerobic flora. Representative sputum is usually unavailable for fungal, parasitic, or
viral pneumonias. Pulmonary infections with escherichia coli, torulopsis, adenovirus, or
cytomegalo virus (CMV) often have the organism in the urine also.
In most pneumonias, the lymph nodes produce pathogen-specific IgM and IgG antibodies. IgA
is produced in cases of pharyngitis. Parasitic infections or inhaled antigens increase IgE levels.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
17
BACTERIAL PNEUMONIA
A fourfold increase in antibodies to the causative organism is not unusual, usually occurring
during recovery. Rapidly fatal cases are often related to the patient’s inability to develop
adequate antibodies. Measurement of antibodies is interesting but is of limited benefit in
diagnosis of pneumonia.
Mature white blood cells leave the bone marrow in acute bacterial infections. Later, younger
leukocytes enter the circulation and cause a “shift to the left” on the differential WBC. The
aged, debilitated, alcoholics, or immunosuppressed patients fail to have a reserve of mature
leukocytes so they get a very rapid shift to the left. At the start of severe pneumonias, the
synthesis of albumin by the liver also ceases and maturation of RBC’s in bone marrow slows.
These lead to anemia and hypoalbunemia if the pneumonia persists longer than two weeks.
The initial WBC in patients with gram-negative bacterial pneumonia averages 15,000 cells/cubic
mm. The maximum is usually less than 19,000. Less than 5000 is unusual, except for the severe
alcoholic or immunosuppressed patient. Leukocytosis and a shift to the left sometimes occur
within the first 24-48 hours after the onset of viral pneumonia. A normal WBC with a relative
lymphocytosis after the first few days is the norm.
Laboratory Studies
•
Leukocytosis with a left shift (absence does not exclude a bacterial infection,
especially in the elderly)
•
Leukopenia (< 5,000)
•
Arterial blood gases (hypoxia and respiratory acidosis)
•
Culture and Gram stain pleural effusions or frank empyema fluid
•
Pulse oximetry (< 95%)
•
Sputum examination in addition to culture and gram stain
INVASIVE DIAGNOSTIC TECHNIQUES
I
nvasive techniques other than the above to diagnose pneumonia include transtracheal
aspiration (TTA), transthoracic lung aspiration (TLA), and bronchoscopy. TTA is the safest
and easiest procedure with the highest diagnostic yield. A direct sample of lower respiratory
tract secretions is made through a needle inserted into the trachea via the cricothyroid membrane.
TTA specimens are free of colonizing oral flora and are suitable for anaerobic culture.
Complications of TTA include bleeding, paratracheal and cutaneous infection, subcutaneous or
mediastinal emphysema, hypoxia, and vasovagal reactions. The overall incidence of significant
complications is low when an experienced person performs the procedure. TTA is ideally used
when oropharyngeal contamination is a problem. It is the procedure of choice for anaerobic
cultures. TTA is advantageous for those patients likely to have oral contamination with gramnegative bacilli and staph aureus, such as, hospitalized patients and alcoholics. It is also useful
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
18
BACTERIAL PNEUMONIA
for patients not producing sputum.
Transthoracic lung aspiration obtains a specimen directly from the lung parenchyma. TLA is a
successful method for diagnosing malignant pulmonary lesions, but is less successful for
infections. A small-bore needle is inserted between the ribs into the affected area and material is
aspirated. Those who cannot survive a total pneumothorax should not be done since this occurs
in approximately 25% of patients. Additional contraindications are bullous emphysema,
bleeding abnormalities, uncooperative patients, uncontrollable coughing, and patient’s receiving
mechanical ventilation. Complications are more frequent with TLA than with TTA. TLA is
probably the procedure of choice when pulmonary malignancy is the leading diagnosis because
of its high yield for cytological exam. It also may be the preferred invasive procedure in young
infants and children.
Bronchoscopy provides aspirated specimens of lower respiratory tract secretions or bronchial
brushings. A brush specimen increases the yield for pathogenic fungi and mycobacteria.5
Protected brush designs increase the yield further and help eliminate oropharyngeal
contamination. One needs strict attention to procedural details and quantitative culture
methodology for valid results on bronchoscopy specimens.
Invasive Diagnostic Procedures
•
Bronchoscopy
•
Transtracheal aspiration for culture
•
Thoracentesis
RADIOLOGIC EVALUATION 6
T
he chest X-ray is used to document both the presence and extent of pneumonia. Changes
are very subtle in the early stages of pneumonia. Minimal X-ray changes do not therefore
preclude the diagnosis. The location and character of the infiltrate are noted on the film.
Look for evidence of pleural effusion, cavitation, adenopathy, calcification, mediastinal shifting
and volume loss. Pneumonia as a result of aspiration is most often located in the posterior
segment of the right upper lobe or the superior segment of the right and left lower lobes. These
areas are usually dependent when aspiration occurs.
Follow-up chest X-rays are necessary to document resolution, exclude the possibility of an
underlying neoplasm, and evaluate for damage and fibrosis. The CXR may take up to 3 months
to clear completely for some pneumonias. Those with a satisfactory clinical improvement do not
need multiple, and sequential CXR’s, except for smokers older than 35 years old. They have an
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
19
BACTERIAL PNEUMONIA
increased risk of cancer and should continue to be followed with X-rays.
Imaging Studies
Chest X-Ray
•
Air bronchograms may be seen in S. pneumoniae.
•
Cavitary lesions and bulging lung fissures may be seen with Klebsiella pneumoniae.
•
Cavitation and associated pleural effusions are noted in Staphylococcus aureus,
anaerobic infections, gram-negative infections and tuberculosis.
•
Legionella has an affinity for the lower lung fields.
•
Klebsiella has a tendency to infect the upper lung fields.
CT Scan
•
High resolution scanning may aid in diagnosis.
Diagnosis Of Pneumonia
•
History and Clinical Presentation
travel exposure
underlying medical conditions
occupational exposure
sudden onset of fever and chills
pleuritic chest pain
dyspnea
•
Laboratory
increased WBC (in most pneumonias and patients)
cultures
anemia (prolonged illness)
hypoalbuminemia (prolonged illness)
•
Radiology
infiltrates
effusions
cavitation
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
20
BACTERIAL PNEUMONIA
TREATMENT
M
ost patients with bacterial pneumonia should be hospitalized. An exception is a young,
otherwise healthy individual with mycoplasma pneumonia. Other patients with no
associated hypoxemia, toxicity, underlying medical conditions, immunocompromise,
leukopenia, extrapulmonary infection, or extensive disease on the CXR also can be managed as
outpatients. The therapeutic plan for pneumonia revolves around the choice of antibiotic,
correction of reversible patient abnormalities, and general supportive care. Each of these is
discussed below.
Antibiotics – The mainstay of drug therapy for bacterial pneumonia is antibiotic treatment.
Ideally, one wishes to obtain culture specimens as a first step, if a patient is not severely ill.
However, one should not wait for extended periods to institute therapy just to get a specimen.
The choice of the therapeutic agent depends upon which bacteria is suspected. The bacteria
suspected is, in turn, based upon the clinical setting and the results of preliminary tests. Severely
ill patients should get broad-spectrum coverage for all pathogens appropriate to the clinical
setting. Those with mild to moderate illness should have therapy specifically aimed at the
predominant flora on a gram stain. For example, if gram positive elongated diplococci are seen,
give penicillin. If gram-negative pleomorphic coccobacilli (H. influenzae) are predominant, give
ampicillin or trimethoprim-sulfamethoxazole.
One needs to differentiate hospital from community-acquired infections. An atypical pneumonia
syndrome is more probable for the latter. Staph aureus, gram-negative bacilli, and pseudomonas
is more common for the former. Erythromycin is effective for most community-acquired
pneumonias with mild to moderate illness (except Chlamydia TWAR). It is seldom appropriate
for nosocomial infections. Broad-spectrum coverage for either staphylococcus or gram-negative
bacilli is more appropriate for nosocomial infection, depending upon the results of sputum gram
stains.
When the etiological bacteria has been identified, the initial regimen is changed to a specific
antibiotic. The ideal drug for a known pathogen should have the narrowest spectrum of activity,
be the most effective, least toxic, and least costly. Organisms cultured from the blood, pleural
fluid, TTA, or TLA are assumed to be the pathogen. Expectorated sputum cultures are less
reliable. They must be interpreted based upon the quality of the specimen and the clinical
impression.
Typically, staph aureus and gram-negative bacilli are easily recovered from respiratory
secretions. If they are not recovered after 24 hours of incubation, consider eliminating coverage
for them. An exception is patients who are high-risk, i.e., a patient with decreased white blood
cells. If the pathogen is not identified, re-evaluate therapy based upon patient response. A good
clinical response obviously indicates continued therapy. If a multiple-drug regimen has been
used, consider narrowing the spectrum when there is patient improvement.
Successful treatment of hospital-acquired pneumonia depends upon the presence and type of
underlying disease(s), the specific causative organism, and the timeliness and appropriateness of
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
21
BACTERIAL PNEUMONIA
therapy. The choice of antibiotic is dependent upon gram stains and cultures, patient-specific
history of recent antibiotics, institution-specific infection rates by certain pathogens, patient drug
allergies, and underlying disease states, such as, immunosuppression.
Choice of antibiotic also depends upon the pharmacokinetics and pharmacodynamics of the drug
in question. These factors affect the drugs ability to penetrate the respiratory tract. To kill a
pathogen the drug must pass through the blood vessel wall, interstitium, alveolar/airway wall,
and enter the secretions. One must get the “drug to the bug” for it to be effective. Molecular
weight, electrical charge, solubility, and many other factors affect its penetration ability.
Fluoroquinolones (Ciprofloxacin, Ofloxacin) penetrate the respiratory tract best, followed by the
cephalosporins and penicillins.
Aminoglycosides are the most effective agents against gram negative nosocomial infections.
They penetrate poorly, so high serum concentrations must be maintained. Aminoglycosides are
usually used in combination with a broad-spectrum cephalosporin or penicillin. This
combination covers both gram positive and anaerobic organisms. It also prevents development
of resistant gram-negative organisms. Institutions with high Legionella rates should add
erythromycin to the initial regimen. The duration of therapy for nosocomial pneumonia depends
upon the pathogen and patient response. Streptococcus pneumoniae should be treated for 7-10
days, hemophilus influenzae 10-14 days, staphylococcus aureus and gram-negative bacilli 14-21
days.
Summary Of Antibiotic Therapy For Bacterial Pneumonia 3,8
•
Penicillins: penicillin G, ampicillin, amoxicillin
•
Semisynthetic penicillins: oxacillin, nafcillin
•
Macrolides: Erythromycin, clarithromycin, azithromycin
•
First generation cephalosporins: cefazolin
•
Second generation cephalosporins: cefuroxime, cefamandole
•
Third generation cephalosporins: cefotaxime, ceftriaxone, ceftizoxime
•
Antipseudomonal cephalosporins: ceftazidime, cefepime
•
Quinolones: ciprofloxacin, levofloxacin
•
Tetracyclines: doxycycline
•
Carbapenems: imipenem, meropenem
•
Monobactams: aztreonam
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
22
BACTERIAL PNEUMONIA
•
Beta-lactam/beta-lactamase inhibitor combinations:
Ampicillin/sulbactam
Ticarcillin/clavulanate
Piperacillin/tazobactam
•
Vancomycin (Vancocin)
Depending on the type of pathogen, recommended antibiotic therapy may include just one, or a
combination of these antibiotics.
Correction Of Reversible Patient Abnormalities - Purulent collections can occur in the
mediastinum, pericardium, or peritoneum from pneumonia. Surgical drainage of such
collections is critical. Parenchymal lung abscess is not considered for surgical drainage because
it communicates with a bronchus. Undrained collections as a result of tumor, foreign bodies,
secretions, etc., can become a closed-space infection in the lung. If so, removal is necessary via
bronchoscopy, local radiation, or chemotherapy.
Excessive secretions are mobilized with chest physical therapy (CPT) for patients who have
difficulty clearing their secretions. Most patients with acute, uncomplicated, bacterial
pneumonia do not require CPT. (CPT is more appropriate for cystic fibrosis and bronchiectasis).
For those who have difficulty with secretions, aerosol treatments with bland aerosols or
acetylcysteine (Mucomyst®) to thin the mucus is of benefit. However, bland aerosol
administration has not been conclusively “proven” to be effective in thinning secretions.
Defects of the immune system predispose to infection and a slow recovery. Many defects cannot
be reversed, but drug-related suppression may be improved. Stopping the immunosuppressive
drug or tapering the dosage should be attempted, if possible. A decrease in white blood cells is
often caused by chemotherapy and is associated with antibiotic-resistant pneumonias. White
blood cell transfusions are logical, but have not been very successful to date. They may be
useful in combination with appropriate antibiotic therapy for gram-negative sepsis.
Supportive Care - Dehydration is common and may lead to electrolyte abnormalities.
Therefore, adequate hydration must be maintained. Extensive cavitary disease or persistent
empyema may cause a negative nitrogen balance so adequate nutritional and caloric intake must
be ensured with long-term illness. Most pneumonias are short-lived, so this is usually not a
problem.
The need for ventilatory support is determined by the extent of the pulmonary infection and the
state of the patient’s respiratory function. The majority of patients with pneumonia do not
require ventilatory support. Supplemental oxygen should be provided for documented hypoxia.
Routine administration of oxygen in the absence of hypoxia is not necessary.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
23
BACTERIAL PNEUMONIA
Treatment Of Pneumonia
•
Antibiotics
based on culture results
severely ill: broad-spectrum coverage
mild/moderately ill: base on gram stain results
community-acquired: erythromycin
hospital-acquired: aminoglycoside with cephalosporin or
penicillin
•
Correction of reversible patient abnormalities
drainage of purulent collections
chest physical therapy
mucolytics
reverse drug-related immunosuppression
correction of electrolytes
bronchodilators for patients who manifest bronchospasm
•
Supportive care
hydration
nutrition
oxygen as necessary
mask or nasal CPAP
intubation/ventilation if indicated
COMPLICATIONS
P
ulmonary complications of bacterial pneumonia primarily consist of hypoxia and dyspnea
in the acute phase. Fibrosis may develop in the area of infection following resolution.
Cavitation may be present, particularly with gram-negative pneumonias. Malnutrition and
dehydration also can occur in the acute phase. Long-lasting pneumonias result in a reversible
debilitation. Additional complications of empyema, bacteremia, and CNS problems are
discussed in further detail below.
Empyemas develop as a result of lymph node obstruction or extension of the pneumonia across
the visceral pleura. (Lymph node obstruction causes a back flow of infected lymph into the
pleural space). Viral and mycoplasma pneumonias usually do not cause empyemas. However,
mycoplasma infections in patients with sickle-cell anemia do commonly get lobar consolidation
and effusion. Group A streptococcus, bacteroides and staphylococcal infections give empyemas
early in the infection. (The latter is almost exclusively in children). Pneumococcus, escherichia
coli, pseudomonas, and klebsiella infections may develop empyema midway through the
pneumonia.
Bacteremia is obviously a very serious complication of bacterial pneumonia. Colony counts vary
from less than 10 to 3500 bacteria per ml of blood. Obviously, the greater the number of
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
24
BACTERIAL PNEUMONIA
bacteria, the worse the prognosis. Prognosis also worsens with age. Septic arthritis, pericarditis,
myocarditis, endocarditis, peritonitis, empyema of the gall bladder, and disseminated
intravascular coagulation (DIC) are other complications of bacteremia.
Bacteremia can “seed” the meninges or brain with bacteria. This can lead to meningitis or brain
abscess. Meningitis is common in pneumococcus bacteremia. Bacteroides infection is
associated with brain abscess. Aseptic meningitis or encephalitis is associated with enterovirus
pneumonia in children. Serious meningoencephalitis and Guillain-Barre syndrome are
occasional complications of mycoplasma pneumonia.
Additional Complications Of Bacterial Pneumonia
•
Local destruction of lung tissue from infection with scarring
•
Bronchiectasis
•
Pulmonary abscess
•
Respiratory failure
•
ARDS
•
Ventilator dependence
•
Superinfection
•
Death
TREATMENT AND CLINICAL MANIFESTATION OF STREPTOCOCCUS AND
STAPHYLOCOCCUS AUREUS PNEUMONIA
STREPTOCOCCUS PNEUMONIAE (PNEUMOCOCCUS) – (Typical Pneumonia)
P
neumococcus is the single most common cause of community-acquired pneumonia
requiring hospitalization. Pneumococcus infects a broad cross-section of the population
and produces a wide-spectrum of disease other than pneumonia. Pneumococcal
pneumonia develops in approximately 2 per 1000 people yearly. Its incidence is increased in
infants, the elderly, military recruits, renal and bone marrow transplants, and gold miners in
South Africa.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
25
BACTERIAL PNEUMONIA
Streptococcus Pneumoniae
Pneumococcus is gram-positive cocci that appear in pairs or short chains. It possesses a complex
polysaccharide capsule that aids identification. The pneumococcus organism is recovered from
sputum in less than half of the cases. Unfortunately, it is also recovered from many patients
without infection. Therefore, there are both false-positive as well as false-negative sputum
cultures. TTA improves the yield and specificity for pneumococcal specimens. A blood culture
is positive in 20-30% of patients.
Pneumococcus is carried in the upper respiratory tract in 5-60% of asymptomatic individuals.
The highest incidence is in infants and families with children. Transmission is from person to
person, possibly through aerosol droplets or physical contact. Infections predominate in winter
and early spring months. Men are affected twice as much as women. Up to 70% of patients
have a history of a preceding upper respiratory infection (URI). The seasonal activities of
respiratory viruses therefore coincide with pneumococcal pneumonia infections.
Clinical Manifestation
The first clinical manifestation of pneumococcal pneumonia is the abrupt onset of chills followed
by a sustained fever. Repetitive shaking chills are unusual without antipyretic therapy. Within
hours, cough, dyspnea and rusty mucoid sputum is produced. Most patients develop severe
pleuritic chest pain, tachypnea, and a splinted respiratory pattern.
Pneumococcal patients appear acutely ill, agitated, cyanotic, and in respiratory distress.
Tachypnea, tachycardia, and fever are invariably present. There are early, fine crackles and
decreased breath sounds in the involved lung segments. CXR abnormalities are unilateral on the
affected side. They consist of lobar consolidation or patchy bronchopneumonia. The latter is
more common in children. Cavitation and empyema are rare. Pleural effusion develops in 2550% of patients. The physical signs of consolidation gradually evolve.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
26
BACTERIAL PNEUMONIA
Leukocytosis is seen in most patients. The total WBC range is between 15,000-25,000 cells per
cubic mm. There is neutrophilia and a leftward shift on the differential count. An overwhelming
infection causes neutropenia with a count less than 3000 cells per cubic mm.
Appropriate antibiotic therapy provides a positive clinical response within 24-48 hours in
pneumococcal pneumonia. Tachypnea and tachycardia resolve gradually. Fever may persist up
to 5 days. The CXR may take 4-8 weeks to clear. Complications of pneumococcal pneumonia
are a result of spread into other areas. Empyema and purulent endocarditis are rare but require
drainage. Meningitis, endocarditis, arthritis and cellulitis also have been described. Asplenic
individuals may get fulminant septicemia and DIC. In hospitalized patients, the mortality rate is
15-20%. Mortality rate increases to greater than 50% for those more than 70 years old.
Treatment
The treatment of choice is procaine penicillin G, 600,000 units IM twice daily for 7-10 days (a
minimum of 5 afebrile days). For IV therapy, use aqueous penicillin G in a daily dosage of 2.44.8 million units. Larger doses or broader-spectrum agents should be avoided because of the
danger of superinfection and other unnecessary side-effects. Patients with significant
complications can be treated with 12-18 million units daily. If the patient has a delayed-type
penicillin allergy, cefazolin can be substituted. For significant allergy to penicillin, use
erythromycin. Chloramphenicol also can be used if meningitis is present in those with allergy.
Many strains have become resistant to various antibiotics. Resistance to penicillin now
approaches 40% for S. pneumoniae. If this is suspected, the drug of choice is vancomycin.
Sparfloxacin, a new-generation, broad-spectrum fluoroquinolone, is also useful. It has the added
advantage of being effective against other strains of penicillin-resistant pneumococci and
atypical organisms. Susceptibility testing must be performed on very sick individuals or those
not responding to therapy. The major preventive measure at the present time to pneumococcal
pneumonia is the pneumococcal vaccine. The vaccine is recommended for those who are in a
high-risk group (the elderly and those with underlying diseases).
STAPHYLOCOCCUS AUREUS - (Typical Pneumonia)
T
his organism accounts for less than 5% of community-acquired pneumonias but about
10% of hospital-acquired pneumonias. In the latter, it is usually contracted from the
bloodstream or from aspirated oral secretions. Approximately 15-30% of healthy adults
carry staph aureus in the nose. Health care workers may have a carriage rate greater than 50%.
Staphylococcus is easily transferred by hand contact.
Staphylococcus is a facultative gram-positive coccus. Gram stains are often contaminated with
oropharyngeal bacteria. Despite this, staph aureus is usually recovered in heavy growth from
sputum cultures. Less than 25% of aspiration cases are associated with a positive blood culture.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
27
BACTERIAL PNEUMONIA
Staphylococcus Aureus: Chest roentgenogram of an intravenous drug abuser showing bilateral
patchy densities and pleural involvement – multiple blood cultures positive for Staphylococcus
Aureus.
Staphylococcus Aureus: Detailed view of right lower lung field showing several lesions that
have excavated forming thin-wlled abscesses.
Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterial strain, which is resistant to
many antibiotics. MRSA is occurring with increased frequency, and can spread rapidly between
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
28
BACTERIAL PNEUMONIA
patients if proper infection-control procedures are not adhered to. As with many infections,
handwashing is the best way to prevent the spread of this bacterial strain. Vancomycin is used to
treat MRSA. Methicillin susceptible S. aureus is treated with semisynthetic penicillins such as
oxacillin or nafcillin.
Staphylococcus aureus is more likely to be found in patients with underlying pulmonary disease
and in those at risk of pneumonia. It commonly follows influenza infections and may complicate
measles infection in children. It can spread to the lungs from endocarditis or from other infected
vascular sites.
Clinical Manifestation
If the cause of staphylococcal pneumonia is from aspiration, the clinical manifestations of fever,
dyspnea, cough, and purulent sputum are present. If the cause is from the bloodstream, the
patient exhibits symptoms of endocarditis. Respiratory symptoms may be absent despite CXR
changes. The physical examination usually reveals fever, prostration, and respiratory distress.
Lobar consolidation is unusual. Crackles and decreased breath sounds are typical. Pleural
effusion, empyema, and abscess formation are common.
WBC’s greater than 15,000 cells per cubic mm, neutrophilia, and increases in band forms are
typical. If there is underlying endocarditis, there may be hematuria, anemia, abnormal renal
function, heart murmur, embolic skin lesions and heart failure. The CXR reveals multiple,
discrete, and often cavitary bilateral lesions, particularly in the lower lobes. In cases of airborne
acquisition, segmental or central consolidation is present. Abscess formation and pleural
effusion occur in 25% of cases.
Local complications of staphlyococcal pneumonia include abscess formation and empyema. In
children, staphylococcal infection is a common cause of pneumatoceles and pyopneumothorax.
Metastatic infections of the CNS, bones, joints, skin and kidneys are associated with positive
blood cultures. Sepsis and endocarditis are either a complication or an underlying cause of
staphylococcal pneumonia.
Treatment
Penicillinase-resistant penicillin (nafcillin, oxacillin) is recommended for uncomplicated cases in
doses of 8-12 grams IV per day for 10-14 days. For those with cavitation or empyema, continue
for 4-6 weeks (longer for underlying endocarditis). For those allergic to penicillin use a firstgeneration cephalosporin, and for those with an immediate-type allergy, use vancomycin.
A thoracentesis should be performed on pleural effusions that develop. Drain all empyema fluid.
If the strain is resistant to the usual penicillins use IV vancomycin, 2 grams per day. Place
hospitalized patients in total isolation to prevent its spread. Elderly and debilitated patients
should receive an influenza vaccine as a preventive measure.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
29
BACTERIAL PNEUMONIA
HEMOPHILUS INFLUENZAE – (Atypical Pneumonia)
H
emophilus influenzae is the major bacterial pathogen of childhood. It is recovered from
90% of children by age 5. It has been increasing in the adult population and now ranks
among the most common bacterial pneumonias requiring hospitalization. Hemophilus is
a frequent colonizer in COPD. Those with lung disease particularly asthma, young children, and
alcoholics are at the greatest risk from hemophilus.
Hemophilus Influenzae
Hemophilus is a small, thin, fastidious, gram-negative rod. It is difficult to detect by a sputum
gram stain. Cultures of expectorated sputum yield the organism in only 50% of documented
bacteremic cases. Recovery from blood specimens is more than 50%. It is occasionally
recovered from pleural fluid.
Clinical Manifestation
The clinical manifestations of hemophilus infection are indistinguishable from the other bacterial
pneumonias. A bronchopneumonia without bacteremia or intrathoracic complications is typical.
There may be a history of URI followed with fever, cough, dyspnea, and purulent secretions.
Patients can have subacute symptoms of cough and low-grade fever for weeks before the
diagnosis.
In about 75% of patients there is a WBC of 10-15,000 cells per cubic mm. Occasionally, there is
a leukopenia (which has proved fatal in children). The CXR is variable, but multilobar, patchy
bronchopneumonia appears in 75%. There is frank consolidation in 38% of patients. Small
parapneumonic effusions are common but rarely progress to empyema. Cavitation is rare.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
30
BACTERIAL PNEUMONIA
Treatment
Some strains of hemophilus are resistant to ampicillin. Initial treatment for a serious infection
consists of 750 mg to 1.5 gm of cefuroxime, cefotaxine, or ceftizoxine every 8 hours. Dosage
should be adjusted for those with renal disease. If susceptibility tests come back positive for
ampicillin, change to that medication. Trimethoprim-sulfamethoxazole is an acceptable
alternative for less severe cases and for oral therapy.
Death occurs in approximately 30%, primarily the elderly and those with underlying disease.
Young patients without bacteremia have the best prognosis. The fatality rate in children is about
5%. Most fatalities occur with metastatic infections.
KLEBSIELLA PNEUMONIAE – (Hospital Acquired)
K
lebsiella is the most common of the gram-negative bacterial pneumonias. Ninety percent
of the cases are in men. Those greater than age 40 are the most susceptible and 66% of
the cases are alcoholics. Klebsiella colonizes the pharynx in 30% of ambulatory
alcoholics. Diabetes mellitus and COPD also predispose to Klebsiella pneumonia. Aspiration is
the usual mechanism of infection.
Klebsiella Pneumoniae
Clinical Manifestation
Klebsiella invasion is manifested by the sudden onset of cough, pleuritic chest pain, dyspnea,
fever, chills, and production of thick, bloody, viscid sputum that has the appearance of currant
jelly. A large volume of sputum, fever greater than 39o C, tachypnea, and lung consolidation are
typical. Hemoptysis is also a possibility. Some patients present with profound toxicity,
prostration and hypotension.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
31
BACTERIAL PNEUMONIA
The WBC is normal in about 25% of cases. Neutropenia is a poor prognostic sign, as is
bacteremia and old age. Abnormal liver function and jaundice may be related to underlying
alcoholism. The CXR shows lobar consolidation, usually in the upper lobes. Approximately
50% have multilobar involvement. Abscess forms in 16-50% of patients.
Klebsiella is a facultative gram-negative rod. Sputum is typically purulent with an
overwhelming number of large gram-negative rods. Blood cultures are positive in
approximately 25%. There is a high mortality, particularly among alcoholics. Overall mortality
is 20-54%.
Metastatic complications are rare, but include pericarditis, arthritis, and meningitis. More typical
complications are localized and are a result of the severe necrotizing nature of klebsiella.
Alveolar septa are destroyed. This results in cavitation and, at its worst, lobar gangrene. Pleural
effusion may appear after the first week. After recovery, there is residual fibrosis, unclosed
cavities, and decreased lung volumes.
Treatment
Aminoglycosides and cephalosporins are the mainstays of treatment. These have in vivo
synergy. The combination enhances renal toxicity so renal function must be monitored. A
minimum of 14 days of treatment is recommended. Cavitation, empyema, or an abscess
warrants longer treatment. Aminoglycosides can be combined with trimethoprimsulfamethoxazole for the penicillin-allergic.
Other enterobacteriaceae associated with pneumonia are: Escherichia, Proteus, Morganella,
Serratia, and Salmonella, to name a few. These pneumonias also should be treated with a twodrug combination. Antipseudomonal penicillin and an aminoglycoside are preferred.
PSEUDOMONAS AERUGINOSA - (Hospital Acquired)
P
seudomonas is the most common cause of nosocomial pneumonia. Pseudomonas is an
aerobic gram-negative rod whose natural habitat includes water, vegetation, and moist soil.
It is a very hardy organism resistant to some disinfectants. To establish the diagnosis of
pseudomonas pneumonia requires being alert to the setting and type of patient in which it occurs.
It is difficult to diagnose pseudomonas from laboratory or X-ray testing. Suspect pseudomonas
pneumonia in the neutropenic patient who develops a clinical picture compatible with such a
diagnosis. Blood cultures are usually positive in these patients. Empyema is common and ideal
for recovering the organism for diagnosis. Consider TTA when the diagnosis is unclear. There
is a bacteremic and nonbacteremic syndrome of pseudomonas disease. The former is seen
primarily in those with blood or lymphatic malignancies. The latter is seen in debilitated patients
who aspirate oropharyngeal secretions.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
32
BACTERIAL PNEUMONIA
Pseudomonas Aeruginosa
Nonbacteremic disease is similar to enterobacteriaceae pneumonia in etiology, i.e., the elderly,
debilitated, COPD, and cardiac disease are common precursors. Bacteremic disease is usually
associated with conditions that alter a patient’s defenses. More than 50% of hospitalized patients
with malignancies carry the organism. Only 5% of the normal population has the organism.
Polymorphonuclear leukocytes are required for eradication of pseudomonas, so neutropenia is a
major risk factor for pseudomonal infection.
Clinical Manifestation (Nonbacterial vs Bacterial)
Nonbacteremic patients are usually toxic appearing, elderly, complaining of chills, fever, and
have a productive cough. Large amounts of purulent sputum are produced. Leukocytosis may
not be present at first, but generally evolves. CXR shows bilateral nodular infiltrates in the lower
lobes. Abscess formation and empyema are common.
Bacteremic types are generally patients with malignancy who are leukopenic (usually
neutropenic) from chemotherapy. There is an occasional history of immunosuppression from
steroid therapy or other illnesses. It is rare in previously healthy adults. Bacteremic
pseudomonas is manifested suddenly with a high fever, confusion, tachypnea, dyspnea, and a
productive cough of scanty and thin sputum. The volume of sputum increases as the disease
progresses and changes to thick, green sputum. The patient appears toxic and distressed. There
are scattered crackles and rhonchi.
Leukopenia is usually present as a result of previous immunosuppression. The CXR initially
shows little change but may reveal pulmonary vascular congestion (see Pseudomonas
Aeruginosa). A patchy bronchopneumonia usually develops with a tendency to multiple areas of
cavitation. Pseudomonas aeruginosa also invades vascular tissue where it produces a vasculitis
resembling pulmonary thromboemboli.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
33
BACTERIAL PNEUMONIA
The mortality rate for pseudomonas pneumonia varies from 36 to 81%. The highest rates are for
ICU patients and those with bacteremic disease. Major complications for nonbacteremic patients
are abscess and empyema. In bacteremic patients, metastatic infection can occur almost
anywhere.
Treatment
Pseudomonas should be treated with two potentially synergistic antimicrobial agents, like an
aminoglycoside and an antipseudomonal penicillin. If the strain is gentamicin and tobramycinresistant, use amikacin and a ureidopenicillin other than carbenicillin. Specific choices are
changed after therapy is instituted, based upon susceptibility tests. Treatment is for a minimum
of 3 weeks. If empyema, abscess, or persistent neutropenia are present, extend the therapy.
Anaerobic Bacteria - Anaerobic bacteria are a common cause of lower respiratory tract
infection in adults. They are often overlooked because of the failure to obtain an appropriate
specimen. Expectorated sputum is inadequate for anaerobic analysis so an invasive procedure
must be done. In most cases, the primary cause of an anaerobic pneumonia is aspiration.
Infections are associated with conditions that predispose to aspiration, such as, coma, seizures,
alcoholism, and general anesthesia. Aspiration is far more common than one might realize. It
has been detected in 2/3 of elderly patients suffering from coma or stupor and in 45% of normal
adults during sleep.
The development of infection from aspiration is related to the volume and character of the
material aspirated, virulence of the organism, and the state of the patient’s defenses. Normal
clearance mechanisms must be overwhelmed or depressed for infection to occur. A second
major risk factor is the presence of periodontal disease. Additional factors are underlying
pulmonary malignancy, bronchiectasis, infarction and other pulmonary conditions.
Clinical Manifestations
The clinical manifestations of anaerobic bacterial pneumonia depend upon the type of disease the
bacteria causes. There are four main categories of disease:
•
pneumonitis without cavitation
•
necrotizing pneumonia
•
lung abscess
•
empyema.
Note: (The latter almost always overlaps one of the other categories).
The first, pneumonitis without cavitation, is characterized much like the previous pneumonias
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
34
BACTERIAL PNEUMONIA
discussed. There is acute onset of fever and cough. The foul sputum and hemoptysis
characteristic of anaerobic lung abscess is often absent in uncomplicated cases. Physical
findings may include pharyngeal dysfunction, periodontal disease, or evidence of alcoholism.
There are crackles and decreased breath sounds in the involved area. The CXR shows a
bronchopneumonia infiltrate but usually no lobar consolidation. Dependent portions are
preferentially involved, particularly if the cause of the pneumonia is aspiration. Empyema may
be present.
The second category, necrotizing pneumonia, has an onset that produces severe illness, fever,
dyspnea, pleural pain, and a productive cough of purulent sputum in the patient. There is
tachypnea, tachycardia, and a temperature greater than 39o C. The WBC is greater than 20,000
cells per cubic mm as a general rule. The CXR reveals dense segmental infiltrates with multiple
small areas of necrosis (< 2 cm diameter). This picture rapidly progresses to multilobar
involvement in many patients. Empyema is present in about 30%.
Thirdly, a lung abscess develops from inappropriate treatment for an anaerobic pneumonia. A
normal fibrosing inflammatory response tends to limit the pneumonia and confine it to a single
segment. This causes the clinical manifestations to develop slowly and insidiously. Fatigue, a
low-grade fever, weight loss, and a productive cough for several weeks before seeking medical
attention are common. Fifty per cent of patients describe foul sputum and hemoptysis is also
sometimes reported. The patient appears chronically ill, has decreased breath sounds, and a
fever. Anemia may be present and indicates the duration of infection. A single abscess is
usually seen in a dependent segment, but additional abscesses may be present in other segments.
Again, empyema is present in about 30%.
The last category of anaerobic infections is empyema, but it is rarely seen by itself. Empyema is
generally a complication of one of the other categories. If present without a corresponding
parenchymal lung infection, suspect a subphrenic or intra-abdominal abscess. Diagnosis of
empyema is made via CXR.
Microbiological Diagnosis - Expectorated sputum is inadequate for anaerobic infections. In up
to 1/3 of the patients pleural fluid is present, so a diagnostic thoracentesis is indicated. If no
pleural fluid is available, TTA or TLA may be necessary. Rapid transport and processing of
anaerobic specimens is essential to identify the organism. The anaerobic environment must be
maintained for diagnosis.
Treatment - Uncomplicated anaerobic pneumonia usually responds promptly to treatment. With
appropriate antibiotics, 10 days of therapy is sufficient. The CXR returns to normal within 3
weeks. For complicated types of anaerobic pneumonia, it may take 1-3 weeks for fever to
disappear and longer for abscess cavities to close and empyema to resolve. The fatality rate for
anaerobic pneumonia is relatively low, but can be as high as 20% for the necrotizing
pneumonias. Complications are generally a result of delayed or inadequate therapy.
Penicillin G is the usual drug of choice, but seriously ill patients also require a second agent.
Possible choices are clindamycin, chloramphenicol, metronidazole, ticarcillin/potassium
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
35
BACTERIAL PNEUMONIA
clavulanate and cefoxitin alone or imipenem alone. Susceptibility testing should be performed
since some organisms may be resistant to any of the above. Coverage also should be provided
for aerobes and facultative organisms. Most are adequately treated with penicillin, clindamycin,
or chloramphenicol.
The dose and duration should be individualized. The acute phase requires penicillin G, IV in a
daily dose of 12-18 million units. Ten days are necessary for uncomplicated cases. Necrotizing
pneumonia, abscess, or empyema requires 4-8 weeks of IV therapy. Oral therapy longer than
this also may be necessary. Percutaneous drainage or surgical resection of an abscess is rarely
indicated; most can be cured with sufficient antibiotic therapy. It should be noted that therapy
may have to be continued for up to one year in stubborn cases. Empyema requires adequate
drainage by thoracentesis or closed chest tube drainage. Very rarely, open drainage with rib
resection is required.
Prevention - Since most cases of anaerobic pneumonia are related to aspiration, precautions
necessary to minimize aspiration in high-risk patients should be implemented. Unconscious
post-op patients, CNS disorders, and stroke victims are high-risk for aspiration so they should
have their airway protected. Cimetidine is useful to minimize a chemical pneumonitis from
gastric acid aspiration. Proper treatment of periodontal disease should be performed on those
who are high-risk for aspiration.
ATYPICAL PNEUMONIA SYNDROME
A
typical pneumonia syndrome consists of pneumonitis, fever, and a normal WBC without
a demonstrable bacterial pathogen. A number of organisms produce the syndrome, but it
is classically associated with Mycoplasma. Other organisms that produce an atypical
syndrome include Chlamydia psittaci and trachomatis, Coxiella burnetil, and numerous viruses.
Atypical pneumonia is a milder illness than bacterial pneumonia. It primarily affects young,
otherwise healthy individuals. Mycoplasma infection is the most common so it is described.
Mycoplasma is a facultative anaerobe that requires special hypertonically supplemented media
for its culture. It requires approximately 10 days for growth, but most patients are improving
long before this. It can be recovered from sputum and throat washings for specimens.
Epidemiology - Mycoplasma pneumonia is estimated at 1 case per year per thousand in the
United States. Approximately 15% of pneumonias in individuals older than 40 years old are
believed to be due to Mycoplasma. Transmission is through aerosol droplets produced by an
infected patient. Coughing is a critical factor in its spread. It spreads readily in families and
closed populations.
Clinical Manifestations - The incubation period following exposure is about 9-21 days. Fever,
chills, dry cough, and headache are typical early symptoms. Dyspnea, chest pain and hemoptysis
are uncommon. Associated symptoms of URI are present in 25-50% of patients at the onset.
Some patients note nausea, vomiting, diarrhea, and muscle pain.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
36
BACTERIAL PNEUMONIA
Within days, most of the early symptoms resolve and the patient is left with a persistent lowgrade fever and dry hacking cough. Temperature is rarely greater than 39o C. There are diffuse
crackles and rhonchi, particularly in the lower lobes. There are often few, if any, abnormal
physical findings. WBC is normal in approximately 75% and there is no evidence of lobar
consolidation. CXR findings are variable. There may be segmental, multilobar, interstitial, or
alveolar infiltrates. CXR findings are out of proportion to the physical findings.
Treatment And Prevention - Mycoplasma is generally a benign, self-limiting infection. It has
an excellent prognosis and death is rare. Exceptions are patients with sickle cell anemia,
multilobar involvement, and immunocompromised patients. Erythromycin or tetracycline, 2
grams daily, will shorten its course. (Tetracycline should be avoided in young children and
pregnant women due to its detrimental effect on developing teeth). A short course of therapy is
associated with relapse, so a minimum of 2 weeks is recommended.
VENTILATOR-ASSOCIATED PNEUMONIA
V
entilator-associated pneumonia (VAP) is defined as a pneumonia that develops 48 hours
or more after intubation in a patient that had no evidence of pneumonia at the time of
intubation. The incidence of VAP in ICU’s is 10-65%. Mortality rate ranges from 1355%. Aerobic gram-negative bacilli and staphylococcus aureus account for 50-70% of VAP
cases. Direct aspiration is the most common cause.
Risk factors for VAP are conditions that increase the risk of aspiration or that increase bacterial
colonization of the oropharynx or stomach. Conditions that increase risk of aspiration are a
recumbent supine position, endotracheal tube or ventilator circuit manipulation, and decreased
consciousness.
Conditions that increase bacterial colonization of the oropharynx and stomach are the use of
antacids, histamine type-2 receptor antagonists, and the prior use of antibiotics. Gastric
alkalinization with antacids and histamine type-2 receptor antagonists has been common
prophylactic therapy on ventilator patients in the past. This was done to prevent gastrointestinal
bleeding from stress ulcers. This is of no great concern for most patients. Few ICU patients
have bleeding stress ulcers so prophylactic therapy is unnecessary. Obvious exceptions are those
who are high-risk for GI bleeding (e.g., coagulopathy).
Diagnosis of VAP is difficult. A new or progressive infiltrate on the CXR is an indicator, along
with associated fever, leukocytosis, and purulent secretions. Other conditions cause the same
symptoms so these are not specific. Diagnosis of VAP based on clinical symptoms alone are
incorrect about 30% of the time. The CXR gives a false-positive diagnosis more than 50% of the
time. Culture results are correct around 62% of the time.
The most accurate way to diagnose VAP is via bronchoscopy specimens from the lower airways
using a protected brush or BAL. Catheter “mini-BAL” by RCP’s provides comparable results to
bronchoscopy techniques. Mini-BAL allows collection of specimens quickly before antibiotics
are started. It is also less costly and easier to perform than bronchoscopy.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
37
BACTERIAL PNEUMONIA
Current recommendations to prevent VAP emphasize decreasing colonization with pathogens
and avoidance of aspiration. Avoid gastric alkalinization and keep the head in a semi-erect
position. Give enteral feedings directly into the jejunum. Monitor the amount of residual
volume of intragastric feedings and avoid gastric overdistention.
Handwashing, gloves, and barrier precautions are of obvious importance. Ventilator circuits
should be changed every 48 hours or more instead of the traditional 24 hours. If tubing needs
draining take precautions there is no drainage into the airway. Avoid prophylactic antibiotic
therapy except in those with neutropenia. The benefits of prophylactic therapy outweigh the
risks in this patient subpopulation.
Diagnosis In The Mechanically Ventilated Patient - It is sometimes difficult to diagnose
pneumonia in those on mechanical ventilated. This is because the typical low-grade fever, chills,
and sweating of acute pneumonia are uncommon. Clinical, laboratory and CXR changes also are
often nonspecific and subtle for these patients. However, a new or progressive infiltrate on the
CXR is an obvious indicator of pneumonia. Lobar consolidation and air bronchograms are often
late findings. Cavitation from a necrotizing gram-negative organism takes more than four days
to become apparent on the CXR. A change in sputum characteristics may be the first clinical
sign of developing pneumonia in those being mechanically ventilated.
Sputum gram stains and cultures are helpful in 40-70% of cases, but most intubated patients
grow one or more organisms even without an infection. In 50-75% of mechanically ventilated
patients the lower respiratory tract is colonized with enteric gram-negative bacilli. Isolation of a
pathogen on a sputum culture does not differentiate colonization from infection so they are
nonspecific for pneumonia. Blood cultures are 100% specific, but less than 10% of the patients
have bacteremia. Specimens obtained from bronchoscopy using a protected brush and
bronchoalveolar lavage (BAL) are useful, but both have a high rate of false-negative results.
They should not be done routinely. Bronchoscopy or BAL specimens are reserved for those who
are severely immunocompromised or who fail to respond to aggressive broad-spectrum
antibiotics.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
38
BACTERIAL PNEUMONIA
CLINICAL PRACTICE EXERCISE
T
he following exercise is based upon the text material. It is discussed at the end of the
course. Individual experience may suggest alternative correct responses.
1. The patient is a 70 year old female receiving chemotherapy for lung cancer in an acute care
hospital. She is a previous smoker and has underlying COPD. She has developed respiratory
distress following emesis. Aspiration is suspected. Fever, dyspnea, and cough are present.
Crackles are heard in the lower lobes. Evaluate this information and make suggestions.
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
2. Gram stain of sputum reveals gram-positive cocci in large numbers. The WBC is 900 and
CXR shows multiple, discrete, bilateral lesions in the lower lobes. Sputum culture is pending.
Patient’s % saturation is 90% on 3 lpm O2 . Evaluate this information.
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
3. Sputum culture shows staphylococcus aureus as the predominant organism. The patient states
she is allergic to penicillin. What are your recommendations based upon this information?
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
SUMMARY
P
neumonia is an acute inflammation of the pulmonary parenchyma from bacteria, viruses,
mycoplasma, and other agents. The first phase of bacterial pneumonia is invasion of body
tissues. This results in production and secretion of antibodies (immunoglobulins) into the
respiratory tract. Chemotactic materials are released causing the attraction of fluid and white
blood cells into the area. The alveoli fill with exudative material. The WBC’s and macrophages
perform phagocytosis. Resolution occurs when the exudate begins to liquefy and be disposed.
Fibrosis and hyaline membranes often remain in the area.
Predisposing factors to pneumonia are related to the virulence of the organism and the patient’s
immunity. Common deficiencies in immunity include: smoking, alcoholism, malnutrition,
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
39
BACTERIAL PNEUMONIA
debilitation, chronic diseases, immunosuppression therapy, and antibody deficiencies.
Additional predisposing factors are: URI, intubation, diabetes, stroke, and malignancies.
Community-acquired pneumonias are usually pneumococcus and not very serious. Nosocomial
pneumonia is more dangerous, up to one third expire. Nosocomial pneumonias are likely to be
staphylococcus aureus or gram-negative bacilli. Typical pneumonia has a clinical picture of
abrupt onset of fever and chills. The patient is often dyspneic, has a productive cough, and
complains of pleuritic chest pain. Atypical pneumonia differs in that the onset is insidious and
complaints of headache, sore throat, muscle pain and fatigue are more common.
Diagnosis of pneumonia is made via epidemiological, clinical, laboratory, and X-ray data.
COPD predisposes to staphylococcus pneumoniae and hemophilus influenzae. A classic history
for bacterial pneumonia includes the sudden onset of chills, pleural chest pain, and dyspnea. The
WBC is usually elevated, but can be normal or low in COPD patients and those receiving
chemotherapy or immunosuppression therapy. Overwhelming infection also can lower the
WBC. The CXR determines the location, extent, and severity of the pneumonia. There may be
minimal changes early in the disease. It may take up to 3 months for the CXR to clear
completely.
Sputum specimens are obtained via expectoration, TTA, TLA, or bronchoscopy. Specimens
should be obtained before institution of antibiotics, if possible. TTA has the highest diagnostic
yield. Expectoration is the easiest and least invasive method. Problems associated with
expectoration are: inability to obtain an adequate specimen, oral flora contamination, and it is
inadequate for anaerobes.
Treatment of pneumonia consists of antibiotics, correction of reversible patient abnormalities,
and general supportive care. The initial choice of antibiotics is based upon which bacteria is
suspected. This is, in turn, based upon the clinical setting and results of preliminary tests, such
as, gram staining. Staphylococcus aureus, gram-negative bacilli, and pseudomonas are more
common in nosocomial infections.
Correctable patient problems include: hypoxia, malnutrition, excessive secretions, empyema,
and drug-related immunosuppression. Some may need oxygen, aerosols, CPT, thoracentesis,
nutritional support, and tapering or discontinuing the drug in question. Intubation and
ventilatory support are rarely needed. Intubation is necessary to protect the airway in some highrisk patients or to provide an avenue for suctioning.
Common causes of bacterial pneumonia are pneumococcus, staphylococcus aureus, neisseria
meningitidis, hemophilus influenzae, klebsiella pneumoniae and pseudomonas aeruginosa. In
adults, anaerobic bacteria are also common. Anaerobic bacteria cause 4 types of disease:
cavitation, necrosis, abscess, and empyema. Some complications of pneumonia are fibrosis,
empyema, bacteremia, and CNS infections.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
40
BACTERIAL PNEUMONIA
PRACTICE EXERCISE DISCUSSION
1. Patient’s age, chronic lung disease, smoking history, and chemotherapy make her high-risk
for pneumonia. Fever, cough, dyspnea, and crackles are compatible with pneumonia. Suggest
WBC to evaluate effect of chemotherapy on the leukocytes, sputum gram stain and culture, CXR,
low-flow O2 , oximetry or ABG’s to evaluate degree of dyspnea.
2. The most common gram-positive cocci are streptococcus and staphylococcus. The former is
more common in community-acquired pneumonia, the latter is more common in hospitalacquired pneumonia. Staphylococcus is also associated with those considered high-risk for
pneumonia, i.e., COPD and cancer in this patient. The WBC is very low, indicating a lack of
ability to respond to an infection. The CXR is compatible with early pneumonia. Oxygenation is
adequate but low on 3 lpm. One may want to consider obtaining a specimen for anaerobic
analysis if patient deteriorates.
3. The patient should be placed in total isolation to protect other patients. Due to the extremely
low WBC, reverse isolation to prevent further contamination of the patient is warranted.
Vancomycin is recommended due to the penicillin allergy.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
41
BACTERIAL PNEUMONIA
SUGGESTED READING AND REFERENCES
1. Braun, Phyllis, PhD, et al. (2001). Infection Control in the ICU. RT The Journal for
Respiratory Care Practitioners. On-line, available:
rtmagazine.com/articles.ASP?ArticleId=R0012A06.
2. WebMD & The Cleveland Clinic. (2002). Other Medical Concerns: Pneumonia. On-line,
available: my.webmd.com/content/article/46/1833_50746.htm.
3. Scanlan, L., et al. (1999). Egan's Fundamentals of Respiratory Care. 7th edition. St Louis,
Mosby-Year Book, Inc.
4. Murray, John F., et al. (2000). Textbook of Respiratory Medicine. 3rd Edition. Publisher:
WB Saunders Company.
5. Gold, Warren M., et al. (2002). Atlas of Procedures in Respiratory Medicine. Publisher:
WB Saunders Company.
6. Muller, Nestor L., et al. (2001). Radiologic Diagnosis of Diseases of the Chest. 1st Edition.
Publisher: WB Saunders Company.
7. Oakes, Dana F. (2000). Clinical Practitioners Pocket Guide to Respiratory Care. Health
Educator Publications, Inc.
8. Arky, Ronald MD, et al, Medical Economics Staff. (1999). Physicians' Desk Reference,
53rd Edition. Medical Economics Company, Inc.
9. Crofton J, Douglas A. RESPIRATORY DISEASES, 5th edition, 2000, Blackwell
Scientific Publications.
10. Fishman A. (editor) PULMONARY DISEASES AND DISORDERS, Vol. I, 3rd Edition,
2000, McGraw-Hill Co.
11. Kollef M, Silver P. “Ventilator-Associated Pneumonia: An Update for Clinicians”,
RESPIRATORY CARE, Nov 95, Vol. 40, #11, pp 1130-1137.
12. Seaton A, Seaton D, Leitch A. CROFTON AND DOUGLAS’S RESPIRATORY
DISEASES, 5th edition, 2000, Blackwell Scientific Publications.
13. Stephen, J. Pneumonia, Bacterial. Emedicine Medical Reference Textbook, June, 2000.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
42
BACTERIAL PNEUMONIA
POST TEST
DIRECTIONS: IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS ON THE ANSWER SHEET PROVIDED AND RETURN TO: RCECS, 16781
VAN BUREN BLVD, SUITE B, RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861.
IF YOU ELECTED ONLINE DELIVERY, COMPLETE THE TEST ONLINE – PLEASE
DO NOT MAIL OR FAX BACK.
1.
Specific predisposing factors to bacterial pneumonia include:
1.
2.
3.
4.
a.
b.
c.
d.
2.
the specimen is not contaminated with oral secretions
faster processing time.
less potential complications.
b & c.
The first stage in the pathology of pneumonia is:
a.
b.
c.
d.
4.
1, 2
2, 3
1, 2, 4
1, 2, 3, 4
Advantage(s) of transtracheal aspiration over expectorated sputum is:
a.
b.
c.
d.
3.
alcoholism
intubation
fat embolus
immunosuppressive therapy
contamination.
invasion.
colonization.
none of the above.
During the “red hepatization” stage of pneumonia:
a.
b.
c.
d.
e.
Alveoli are filled with RBC’s.
Alveolar capillaries are congested.
Alveolar exudate begins to break up.
Fluid is reabsorbed through the alveolar wall.
a & b.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
43
BACTERIAL PNEUMONIA
5.
What occurs after the initial invasion of body tissues in pneumonia?
1.
2.
3.
4.
a.
b.
c.
d.
e.
6.
Transtracheal aspiration
Transthoracic lung aspiration
Bronchoscopy
b&c
None of the above
Predisposition to pneumonia is related to:
a.
b.
c.
d.
e.
8.
4 only
1, 4
1, 2, 3
1, 2, 3, 4
2, 4
Which of the following techniques is the safest, easiest and has a high diagnostic yield?
a.
b.
c.
d.
e.
7.
Virulence of organism.
Presence of atopy.
Previous damage to respiratory epithelium.
Level of consciousness.
a & c.
Additional predisposing factors to pneumonia are:
1.
2.
3.
4.
a.
b.
c.
d.
e.
9.
IgG and IgA coat the invading organism.
Antibodies are released into bronchial secretions.
Leukocytes migrate into the lung.
PaO 2 begins to rise.
Debilitation.
Use of bronchodilators.
Malnutrition.
Chronic disease.
1, 2, 3
1, 3, 4
3, 4
1, 2, 3, 4
None of the above
The difference between typical and atypical pneumonia is:
a.
b.
c.
d.
typical pneumonia is gram negative organisms.
typical pneumonia is gram positive organisms.
atypical is usually life-threatening.
atypical is usually insidious rather than abrupt and headache is common.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
44
BACTERIAL PNEUMONIA
10.
What are the most common clinical manifestations of pneumonia?
a.
b.
c.
d.
e.
11.
What is the mainstay of treatment for bacterial pneumonia?
a.
b.
c.
d.
12.
An increase in leukocytes
A decrease in granulocytes
Corticosteroid therapy
b&c
a & b.
A problem associated with an expectorated sputum specimen is:
a.
b.
c.
d.
e.
15.
Patient history.
Patient physical.
Laboratory results.
Radiological results.
All of the above.
Which of the following is a high-risk situation concerning pneumonia?
a.
b.
c.
d.
e.
14.
oxygen
antibiotics
CPT
none of the above
Diagnosis of pneumonia is based on:
a.
b.
c.
d.
e.
13.
Fever
Chills
Atelectasis
Anxiety
a&b
Contamination with oral flora.
It is invasive.
It is costly.
Diagnostic yield is high.
All the above.
A classic history of pneumococcal pneumonia is:
1.
2.
3.
4.
a.
b.
c.
d.
e.
sudden onset of chills
pleuritic chest pain
coma
dyspnea
2, 3, 4
1, 3
3, 4
1, 2, 4
1, 2, 3, 4
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
45
BACTERIAL PNEUMONIA
16.
CXR infiltrates in aspiration pneumonia are most commonly found:
a.
b.
c.
d.
e.
17.
Initial WBC in patients with gram-negative bacterial pneumonia averages:
a.
b.
c.
d.
18.
3000 cells per cubic mm.
15,000 cells per cubic mm.
30,000 cells per cubic mm.
200 cells per cubic mm.
Often, the first clinical sign of developing pneumonia in the patient being ventilated is:
a.
b.
c.
d.
e.
19.
posterior segment of right upper lobe.
superior segments of the right and left lower lobes.
in the lingula.
all of the above.
a and b.
Decrease in VD/VT ratio.
Drop in PaO 2 .
A change in sputum characteristics.
Sweating.
All the above.
In the acute phase of pneumonia, what are the primary pulmonary complications?
1.
2.
3.
4.
a.
b.
c.
d.
e.
20.
Atelectasis
Dyspnea
Hypoxia
Air trapping
1, 2, 3, 4
2, 3
1, 3, 4
2, 3, 4
2, 4
What is the most common cause of atypical pneumonia?
a.
b.
c.
d.
Hemophilus
Mycoplasma
Klebsiella
Pseudomonas
KM: Test Version E
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
46
BACTERIAL PNEUMONIA
ANSWER SHEET
NAME____________________________________ STATE LIC #_______________________
ADDRESS_________________________________ AARC# (if applic.)___________________
DIRECTIONS: (REFER TO THE TEXT IF NECESSARY – PASSING SCORE FOR CE
CREDIT IS 70%). IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS AND RETURN TO: RCECS, 16781 VAN BUREN BLVD, SUITE B,
RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861. IF YOU ELECTED ONLINE
DELIVERY, COMPLETE THE TEST ONLINE – PLEASE DO NOT MAIL OR FAX BACK.
1. a b c d
16. a b c d e
2. a b c d
17. a b c d
3. a b c d
18. a b c d e
4. a b c d e
19. a b c d e
5. a b c d e
20. a b c d
6. a b c d e
7. a b c d e
8. a b c d e
9. a b c d
10. a b c d e
11. a b c d
12. a b c d e
13. a b c d e
14. a b c d e
15. a b c d e
KM: Test Version E
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
47
BACTERIAL PNEUMONIA
EVALUATION FORM
NAME:____________________________________________ DATE:______________
AARC # (if applic.)________________________ STATE LICENSE #:______________
RC Educational Consulting Services, Inc. wishes to provide our clients with the highest quality
CE materials possible. Your honest feedback helps us to continually improve our courses and
meet CE regulations in many states. Please complete this form and return/submit it with your
answer sheet. Thank you.
YES
NO
Were the objectives of the course met?
Was the material clear and understandable?
Was the material well-organized?
Was the material relevant to your job?
Did you learn something new?
Was the material interesting?
Were the illustrations, if any, helpful?
Would you recommend this course to a friend?
What was the most valuable portion of the material?
________________________________________________________________________
What was the least valuable portion of the material?
________________________________________________________________________
Suggestions for future courses: ______________________________________________
Comments: ______________________________________________________________
________________________________________________________________________
What is your specialty area?______________________________ Credentials?________
How did you hear about RCECS?____________________________________________
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
48