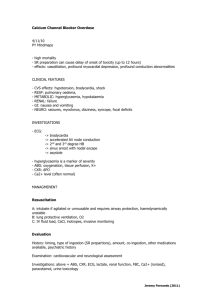
Calcium Homeostasis and Parathyroid Hormone
advertisement

University of Nebraska Medical Center Importance of Calcium Homeostasis Calcium Homeostasis and Parathyroid Hormone • Calcium is tightly regulated because calcium plays a very important role in physiologic processes CLS 413 Clinical Endocrinology and Toxicology Ricki Otten, MT(ASCP)SC uotten@unmc.edu 2 Roles of Calcium Forms of Calcium in Plasma • Muscle contraction – Muscles – Heart Ca2+ Ca2+ Ca2+ • Cellular processes C ll l Ca2+ Ca2+ – Release of neurotransmitters – Release of hormones – Activation of enzymes – Membrane structure – Metabolic switching and gene expression Ca2+ Ca2+ protein-bound FREE anion-bound filterable TOTAL 3 4 pH Dependent H+ displaces Ca2+ from protein Ca2+ free Ca2+ Ca2+ proteinbound Ca2+ H+ Ca2+ H+ Ca2+ Ca2+ H+ Ca2+ Ca2+ Ca2+ H+ Ca2+ protein-bound free anion-bound filterable pH total 5 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 6 1 Effects of Protein Ca2+ Effects of Excess Anions Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ Ca2+ protein-bound free anion-bound Ca2+ protein-bound Ca2+ FREE filterable anion-bound filterable total TOTAL 7 8 Indicate the expected changes (increased, decreased, no change) to the total and ionized calcium levels when the following ‘conditions’ are present Condition Total Calcium Level What we measure • Total calcium Ionized Calcium Level – Reflects all forms of calcium: protein‐bound, ‘free’ and anion‐bound Acid pH Alkaline pH • Free calcium – Physiologically active form – Commonly referred to as “Ionized calcium” Increased proteins Decreased proteins Excess anions 9 States of Calcium in Plasma (and phosphate and magnesium) Calcium or ionized Calcium? • Generally, healthy people who do not have a protein abnormality, the total calcium level reflects the ionized calcium level % of total • Ionized Ionized calcium measurements are needed in calcium measurements are needed in certain patient populations: – – – – – Liver disease Kidney disease Premature infant Hospitalized patients (especially in intensive care) Critically ill patients 11 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 10 calcium phosphate magnesium free (ionized) 50 55 55 protein-bound 40 10 30 complexed 10 35 15 Total (mg/dL) 8.6-10.3 2.5-4.5 1.7-2.4 Total (mmol/L) 2.2-2.6 0.7-1.0 0.8-1.5 12 2 States of Calcium in Plasma (and phosphate and magnesium) Bone is our ‘Calcium Bank’ • Body’s main reservoir of calcium (~98‐99%) – Very little calcium (~1‐2%) is in circulation Approximate % of total calcium • Need high store of calcium to maintain physiologic level in blood provides short term physiologic level in blood: provides short‐term exchange into plasma as needed phosphate magnesium free (ionized) 50 55 55 protein-bound 40 10 30 complexed 10 35 Total (mg/dL) 8.6-10.3 2.5-4.5 1.7-2.4 Total (mmol/L) 2.2-2.6 0.7-1.0 0.8-1.5 15 • Phosphate (PO42‐) also in bone • Very little phosphate (~0.1%) in circulation 13 Composition of Bone 14 Parathyroid Hormone (PTH) • Mineral organic crystalline salts • Produced by parathyroid glands – 75% of dry weight – Provides compressional strength – Calcium phosphate and calcium carbonate (majority) – 4 parathyroid glands embedded on ‘back side’ of thyroid gland • PTH is main regulator of ionized calcium (in plasma) • Organic matrix – 25% of dry weight – Collagen fibers (majority): provides tensile strength – Released when ionized calcium decreases – Low ionized calcium levels trigger PTH release • PTH has very short t1/2: 10‐15 minutes!! PTH vs Intra‐operative PTH levels 15 PTH: 3 Main Actions 16 PTH action: • Activates osteoclasts – Stimulates bone resorption (breaks down bone matrix) and releases calcium and phosphate into blood stream Decreased ionCalcium • Stimulates renal tubular calcium reabsorption – Kidney reabsorption of calcium into bloodstream (and excretion of phosphate into urine) • Stimulates enzymatic conversion of VitD2 to active VitD3 form by the kidney – VitD3 works on intestine to increase intestinal absorption of calcium (from gut) into bloodstream 17 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 18 3 PTH action: ‘Vitamin D’ PTH: Bone resorption Ca PO4 PTH: Kidney excretion of PO4 PTH: Kidney reabsorption Ca PTH: Kidney activation of VitD2 to VitD3 • Hormone (endogenously produced) • Considered a ‘fat soluble’ vitamin • Necessary for absorption of calcium by small intestine • Active form produced in kidney – 1,25‐(OH)2‐cholecalciferol = calcitriol = VitD3 • Vitamin D2 (precursor to VitD3) available in foods (cows milk is VitD fortified) VitD3: Intestinal absorption Ca PO4 19 20 ‘Vitamin D’ Pathway 7-dehydrocholesterol UV light (skin) cholicalciferol Need: Sunlight Healthy liver Healthy kidney Liver 25-(OH)-cholicalciferol Kidney active vitamin D3, calcitriol 1,25-(OH)2-cholicalciferol + 24,25-(OH)2-cholicalciferol (main target is the intestine) 21 22 Calcitonin (anti PTH?) main circulating form of VitD; what the lab usually measures (1000x higher than active form AND longer half life!) ACTIVE FORM needed for intestinal calcium absorption Produced by thyroid gland (C‐cells) Effects nearly opposite to those of PTH Of minor importance in humans Deficiency has no clinical effects Tumors producing calcitonin can cause hypocalcemia (then it is important!) • Procalcitonin produced by other tissues • • • • • • Rapid responder to stress of septicemia (bacterial infection): future marker of sepsis? 23 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 24 4 1,25-(OH)2-D3 Ca2+ Intestine Ca2+ Plasma Calcium and Phosphate PTH Bone Thyroid: calcitonin • Phosphate tends to move in opposite direction as calcium does Parathyroid hypocalcemia • Lots of phosphate released from bone • Lots of phosphate excreted into urine • Some phosphate absorbed by intestine in response to VitD3 Ca2+ 1,25-(OH)2-D3 P urine PTH Kidneys NET Effect: increased calcium, decreased phosphate 25-OH-D2 Liver – Low ionized calcium = PTH release that leads to: Overview of calcium homeostasis: • Disease can alter this relationship 25 26 Calcium and Phosphate in Disease Calcium and Magnesium • Magnesium tends to move in same direction as calcium does • This is because This is because – Magnesium’s ionic radius AND charge are very similar to calcium’s – Magnesium’s absorption and elimination pathways are identical to calcium’s 27 • Usual relationship between calcium and phosphate can be altered in some disorders – Some renal disorders – Bone metastases – Vitamin D abnormalities (increased or decreased levels) • When both calcium and phosphate are increased, – Results in calcium salt deposition in tissues, joints and kidneys – Metastatic calcification Calcium and Phosphate in Disease 28 Hypercalcemia • Primary Hyperparathryoidism (Incr PTH): – Incr Calcium • Symptoms: Decr Phosphorus – Fatigue <12 mg/dL – Malaise – Affects muscle function: muscle weakness (muscle atrophy if chronic) (the heart is a muscle) • Primary Hypoparathyroidism (Decr PTH): – Decr Calcium Incr Phosphorus • VitD Intoxication (Incr VitD); Bone Metasteses: – Incr Calcium – Depression – Apathy – Lack of concentration – Mild polyphagia, polydipsia, polyuria Incr Phosphorus • VitD Deficiency (Decr VitD); Renal Failure: – Decr Calcium Decr Phosphorus 29 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 30 5 Causes of Hypercalcemia “Expert Systems” • Primary hyperparathyroidism (most common) – Parathyroid adenoma (85%), hyperplasia (15%), carcinoma (<1%) • • • • • • Flow chart for diagnosing hypercalcemia PTH secreting tumors (some lung tumors) g ( g ) Bony metastases Vitamin D intoxication Malignancy Thiazide diuretics (increased renal retention) Many other factors Expert systems: removes judgment errors Expert systems: future of how lab will ‘serve’ medicine 31 32 Hypocalcemia Symptoms: – Neuromuscular excitability • Tetany (affects muscle function: heart is a muscle!) • Paresthesia (numbness, tingling, increased sensitivity) • Seizures – Respiratory arrest – Nervousness, irritability – Convulsions – Death 33 Causes of Hypocalcemia 34 “Expert Systems” • Vitamin D deficiency: most common, worldwide – Sunlight or dietary deprivation – Malabsorption Flowchart for diagnosing hypocalcemia • Abnormal vitamin D metabolism: – Renal failure (also decreased calcium reabsorption) Renal failure (also decreased calcium reabsorption) – Liver failure – Vitamin D dependent Rickets • Hypoparathyroidism (surgical removal thyroid gland) • Acute pancreatitis • Massive transfusion or plasma exchange 35 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 36 6 “Expert Systems” Flowchart for diagnosing Hypoparathyroidism 37 38 Laboratory Tests • Total calcium (plasma, serum) (CAP, 2004 survey) – Spectrophotometric (79%) • Need to acidify to convert all forms of calcium to ionCa • Metallochromic indicators or dyes change color when bound to calcium bound to calcium – O‐cresolphthalein complexone (CPC) – Arsenazo III • Easy to automate – Ion selective electrode (20%) • First must acidify to convert protein‐bound and complexed calcium into free calcium form – Atomic absorption (reference method) 39 • Most accurate and reproducible 40 Laboratory Tests Laboratory Tests • Total magnesium (plasma, serum) • Ionized calcium (heparinized whole blood) (CAP, 2004 survey) – Spectrophotometric – Ion selective electrode (ISE) – ISE uses a calcium selective membrane – Sample collection VERY IMPORTANT Sa p e co ect o O • Metallochromic indicators or dyes change color when bound to magnesium – – – – – – • Full tube (maintain heparin:blood ratio) • Tightly stoppered tube (loss of CO2 will change pH) • On ice (continued metabolic processes, ie glycolysis, will produce CO2 as metabolic byproduct and this will change pH) Calmagite (26%) Methylthymol blue (26%) Formazon dye (23%) Magon/xylidyl blue (13%) Chlorophosphonazo III (7%) Arsenazol (2%) These methods require calcium chelating agent such as EGTA – Atomic absorption (reference method) • Free magnesium: ISE 41 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 42 7 Laboratory Tests Laboratory Tests • Intact PTH • Phosphate (plasma, serum) – Sandwich immunoassay using 2 antibodies that can simultaneously bind with PTH – Spectrophotometric • All methods based on reaction of phosphate ions with ammonium molybdate • Phosphomolybdate complex can be measured 2 ways: 1. Directly measure how much UV light (340nm) the phosphomolybdate complex absorbs 2. Reduce the phosphomolybdate complex to molybdenum blue and measure the absorbance at 600‐700nm • Capture antibody is the solid phase antibody that binds to one epitope of PTH • Labeled antibody that binds to a second PTH epitope • Non Non‐competitive competitive immunoassay: increased sensitivity, immunoassay: increased sensitivity, specificity, reproducibility and convenience – Most likely will use Mass Spectrometry in future • Intra‐operative PTH – Half life is short – Patient on operating table while lab does assay – Atomic absorption (reference method) 43 Laboratory Tests 44 Laboratory Tests • Vitamin D2 and Vitamin D3 • Cyclic adenosine monophosphate (cAMP) – Usually reverse‐phase HPLC – Common steps: – Measured by HPLC or enzymatic methods – Urine sample • Extraction of VitD from serum/plasma • Purification P ifi ti • Quantitation – Usually done to determine if kidneys are responding to the PTH signal – Likely will be replaced by Mass Spectrometry • Increased sensitivity • Increased specificity • Thus liver and kidney function essential 45 46 Summary • Calcium regulation – PTH, vitamin D, bone, kidney, liver, small intestine • Vitamin D is a hormone – Final active form is 1,25‐(OH)2‐vitamin D3 (calcitriol) • PTH also affects phosphate and magnesium • Hypercalcemia and hypocalcemia require numerous tests – Expert systems reduce test utilization and associated costs 47 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 8 22 main circulating form of VitD; what the lab usually measures (1000x higher than active form AND longer half life!) ACTIVE FORM needed for intestinal calcium absorption 23 CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone 9 Hypercalcemia suspected Ionized calcium High Hyperproteinemia Normal VitD intoxication Intact PTH High High Neoplasia Sarcoid or TB Endocrinopathy Normal or low Normal or Low VitD2 & VitD3 HyperParathyroidism Calcium infusion Abnormal PTH Response Normal PTH Response *If ionized calcium unavailable, free calcium can be estimated by measuring total calcium, albumin and TSP *The calcium infusion test looks for a rapid fall in plasma PTH after IV administration of calcium gluconate CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone: Hypercalcemia Flow Chart 10 Hypocalcemia suspected Ionized calcium* Low Hypoalbuminemia Normal Plasma Phosphate Low Renal tubular disorder Normal or High BUN and Creatinine Normal HypoParathyroidism High Renal Failure Go to flowchart for Diagnosing HypoParathyroidism *Renal failure is a common cause of hypocalcemia due to inability to excrete phosphate and reabsorb calcium. Renal tubular disorders can cause hypocalcemia and hypophosphatemia due to excessive urinary loss of both CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone: Hypocalcemia Flow Chart 11 HypoParathyroidism VitD deficiency Intact PTH Low Normal VitD resistance Low High Urinary cAMP Primary HypoParathyroidism Low No PTH Response PTH infusion Renal PTH resistance (pseudohypoparathyroidism) Vit D3 High EDTA infusion No cAMP Response High Large cAMP Response Biologically inactive PTH *Cyclic AMP is the ‘second messenger’ formed after PTH binds to its receptor on renal tubule cells. If PTH is biologically active and the receptors are functioning, rises in PTH result in production of cAMP *EDTA infusion acts by binding ionized calcium. This normally will be a potent stimulus for release of PTH. Failure to respond to EDTA is diagnostic of primary hypoparathyroidism CLS 413 Clinical Endocrinology and Toxicology Calcium Homeostasis and Parathyroid Hormone: Hypoparathyroidism Flow Chart 12