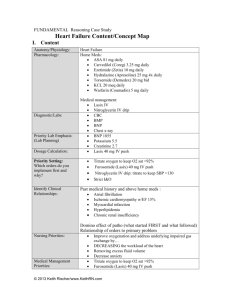
Heart Failure/Acute Renal Failure Content/Concept Map I. Content
advertisement
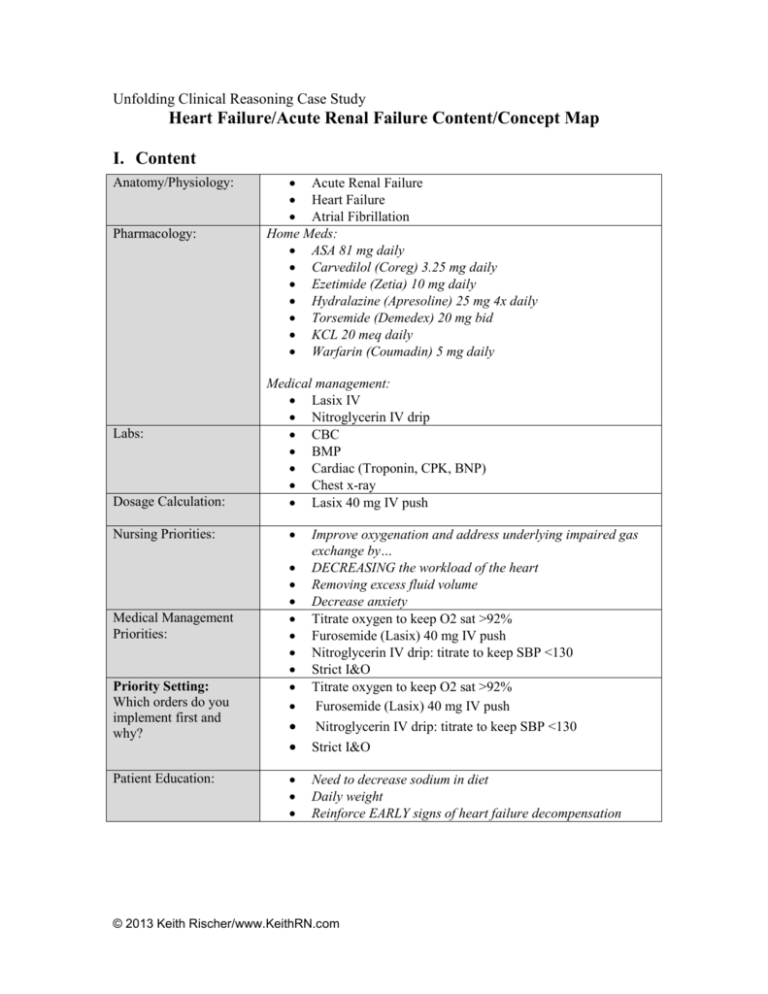
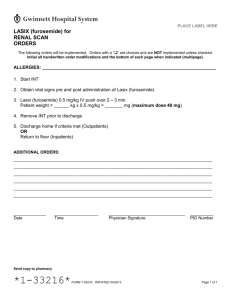
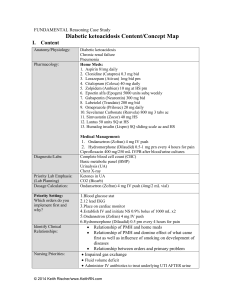
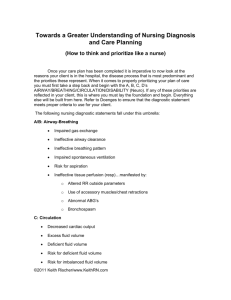
Unfolding Clinical Reasoning Case Study Heart Failure/Acute Renal Failure Content/Concept Map I. Content Anatomy/Physiology: Pharmacology: Labs: Dosage Calculation: Nursing Priorities: Medical Management Priorities: Priority Setting: Which orders do you implement first and why? Patient Education: Acute Renal Failure Heart Failure Atrial Fibrillation Home Meds: ASA 81 mg daily Carvedilol (Coreg) 3.25 mg daily Ezetimide (Zetia) 10 mg daily Hydralazine (Apresoline) 25 mg 4x daily Torsemide (Demedex) 20 mg bid KCL 20 meq daily Warfarin (Coumadin) 5 mg daily Medical management: Lasix IV Nitroglycerin IV drip CBC BMP Cardiac (Troponin, CPK, BNP) Chest x-ray Lasix 40 mg IV push Improve oxygenation and address underlying impaired gas exchange by… DECREASING the workload of the heart Removing excess fluid volume Decrease anxiety Titrate oxygen to keep O2 sat >92% Furosemide (Lasix) 40 mg IV push Nitroglycerin IV drip: titrate to keep SBP <130 Strict I&O Titrate oxygen to keep O2 sat >92% Furosemide (Lasix) 40 mg IV push Nitroglycerin IV drip: titrate to keep SBP <130 Strict I&O Need to decrease sodium in diet Daily weight Reinforce EARLY signs of heart failure decompensation © 2013 Keith Rischer/www.KeithRN.com II. Concepts (in order of emphasis) I. II. III. IV. V. VI. VII. III. I. Perfusion Gas Exchange Fluid and Electrolyte Balance Clinical Judgment Patient Education Communication Collaboration NCLEX Client Need Categories Safe and Effective Care Environment a. 20%–Management of Care i. Providing and directing nursing care that enhances the care delivery setting to protect clients, family/significant others, and healthcare personnel 1. Establish priorities 2. Collaboration w/treatment team 3. Advocacy II. III. Health Promotion & Maintenance: i. 9%–The nurse provides and directs nursing care of the client and family/significant others that incorporates knowledge of expected growth and development principles, prevention and/or early detection of health problems, and strategies to achieve optimal health. 1. Disease prevention 2. Physical assessment 3. Client education Physiologic Integrity a. 15%–Pharmacological & Parenteral Therapies: i. Providing care related to the administration of medications and parenteral therapies 1. Expected actions, adverse/side effects 2. Medication administration 3. IV therapies 4. Dosage calculation b. 12%–Reduction of Risk Potential: i. Reducing the likelihood that clients will develop complications or health problems related to existing conditions, treatments or procedures 1. Changes in VS 2. Diagnostic tests 3. Lab values 4. System specific assessments 5. Potential for alterations in body systems c. 13%–Physiological Adaptation: i. Managing and providing care for clients with acute, chronic, or life threatening health conditions. © 2013 Keith Rischer/www.KeithRN.com 1. Pathophysiology 2. F&E imbalances 3. Medical emergencies IV. QSEN Skills I. II. III. Patient-centered Care a. Implementation of care plan and evaluation of care b. Provide patient-centered care with sensitivity and respect for the diversity of human experience Evidence-based Practice a. Base individualized care plan on patient values, clinical expertise and evidence Teamwork and Collaboration a. Follow communication practices that minimize risks associated with handoffs among providers and across transitions in care (SBAR). Assert own position/perspective in discussions about patient care © 2013 Keith Rischer/www.KeithRN.com