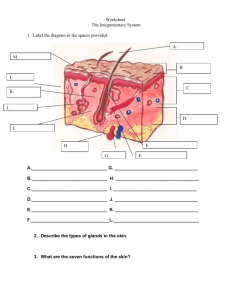
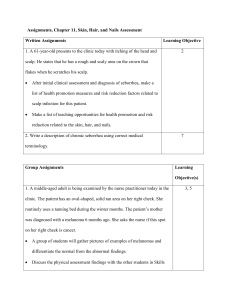
PHYSICAL EXAMINATION OF THE SKIN, HAIR AND NAILS
PHYSICAL EXAMINATION OF THE SKIN, HAIR AND NAILS (INTEGUMENT)
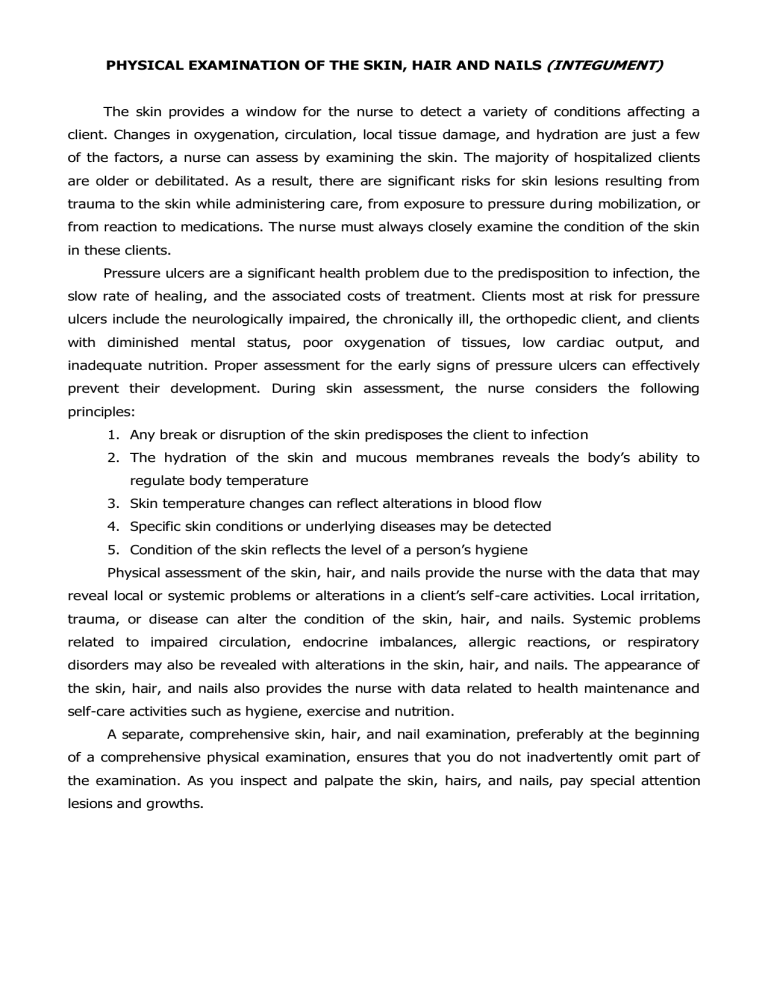
The skin provides a window for the nurse to detect a variety of conditions affecting a client. Changes in oxygenation, circulation, local tissue damage, and hydration are just a few of the factors, a nurse can assess by examining the skin. The majority of hospitalized clients are older or debilitated. As a result, there are significant risks for skin lesions resulting from trauma to the skin while administering care, from exposure to pressure during mobilization, or from reaction to medications. The nurse must always closely examine the condition of the skin in these clients.
Pressure ulcers are a significant health problem due to the predisposition to infection, the slow rate of healing, and the associated costs of treatment. Clients most at risk for pressure ulcers include the neurologically impaired, the chronically ill, the orthopedic client, and clients with diminished mental status, poor oxygenation of tissues, low cardiac output, and inadequate nutrition. Proper assessment for the early signs of pressure ulcers can effectively prevent their development. During skin assessment, the nurse considers the following principles:
1.
Any break or disruption of the skin predisposes the client to infection
2.
The hydration of the skin and mucous membranes reveals the body’s ability to regulate body temperature
3.
Skin temperature changes can reflect alterations in blood flow
4.
Specific skin conditions or underlying diseases may be detected
5.
Condition of the skin reflects the level of a person’s hygiene
Physical assessment of the skin, hair, and nails provide the nurse with the data that may reveal local or systemic problems or alterations in a client’s self-care activities. Local irritation, trauma, or disease can alter the condition of the skin, hair, and nails. Systemic problems related to impaired circulation, endocrine imbalances, allergic reactions, or respiratory disorders may also be revealed with alterations in the skin, hair, and nails. The appearance of the skin, hair, and nails also provides the nurse with data related to health maintenance and self-care activities such as hygiene, exercise and nutrition.
A separate, comprehensive skin, hair, and nail examination, preferably at the beginning of a comprehensive physical examination, ensures that you do not inadvertently omit part of the examination. As you inspect and palpate the skin, hairs, and nails, pay special attention lesions and growths.
PREPARING THE CLIENT:
To prepare for the examination, ask the client to remove all clothing and jewelry and put on an examination gown. In addition, ask the client to remove nail enamel, artificial nails, wigs, toupees, or hairpieces as appropriate.
Have the client sit comfortably on the examination table or bed for the beginning of the examination. The client may remain in a sitting position for most of the examination. However, to assess the skin on the buttocks and dorsal surfaces of the legs properly, the client may lie on her side or abdomen.
During the examination, ensure privacy by exposing only the body part being examined.
Make sure that the room is a comfortable temperature. If available, sunlight is best for inspecting the skin. However, a bright light that can be focused on the client works just as well. Keep the room door closed or the bed curtain drawn to provide privacy as necessary.
Explain what you are going to do, and answer any questions the client may have. Wear gloves when palpating any lesions because you may be exposed to drainage.
Clients from conservative religious groups (ex. Orthodox Jews or Muslims) may require that the nurse be the same sex as the client. Also, to respect the client’s modesty or desire for privacy, provide a long examination gown or robe.
EQUIPMENTS TO BE USED:
Examination light
Penlight
Mirror for client’s self-examination of skin
Magnifying glass
Centimeter ruler
Disposable gloves (for moist or draining lesions)
Wood’s light (if available)
Examination gown or drape
KEY POINTS TO REMEMBER IN THE EXAMINATION
Inspect skin color, temperature, moisture, texture
Check skin integrity
Be alert for skin lesions
Evaluate hair condition; loss or unusual growth
Note nail bed condition and capillary refill
SKIN ASSESSMENT
INSPECTION
ASSESSMENT PROCEDURE
Inspect general skin coloration.
Keep in mind that the amount of pigment in the skin accounts for the intensity of color as well as hue
While inspecting skin coloration, note any odors emanating from the skin
NORMAL FINDINGS
Inspection reveals evenly colored skin tones without unusual or discolorations. prominent
Small amounts of melanin are common in whiter skins, while large amounts of melanin are common in olive and darker skins. Carotene accounts for a yellow cast.
***The older client’s skin becomes pale due to decreased melanin production and decreased dermal vascularity
***Inspecting the palms is an opportunity to assess overall coloration
Client has slight or no odor of perspiration, depending on activity
ABNORMAL FINDINGS
Please refer to the table below for abnormal skin colors.
*** Acanthosis nigricans is the roughening and darkening of the skin in localized areas especially the posterior neck.
A strong odor of perspirations or foul odor may indicate disorder of sweat glands. Poor hygiene practices may indicate a need for client teaching or assistance with activities of daily living
ABNORMAL SKIN COLORS
Color
Cyanosis
(bluing)
Pallor
(decrease in color)
Condition
Increased amount of deoxygenated hemoglobin, associated with hypoxia
Reduced amount of oxyhemoglobin
Reduced visibility of oxyhemoglobin as a result of decreased blood flow
Congenital or autoimmune condition causing lack of pigment
Cause
Heart or lung disease; cold environment
Anemia
Shock
Vitiligo
Assessment Location
Nail beds (peripheral cyanosis) ; lips; mouth; skin (severe cases of central cyanosis)
Face; conjunctiva; nailbeds
Skin; nail beds; conjunctiva; lips
Patchy areas on the skin
Jaundice
(yellow-orange)
Erythema
(redness)
Tan-brown
Ecchymosis
(black and blue)
Increase deposition of bilirubin in the tissues
Increased visibility of oxyhemoglobin as a result of dilation or increased blood flow
Increased amount of melanin
Extravasation of blood into the subcutaneous tissue
Liver, gallbladder, or pancreatic disease; destruction of
RBC
Fever; direct trauma; blushing; alcohol intake
Suntan; pregnancy or
Addison’s disease
Trauma or fragile blood vessels
Sclera; mucous membranes; skin
Face; area of trauma
Areas exposed to sun; face; areola; nipples
Extremities, head, or trunk in areas easily exposed to injury
**Types of Cyanosis:
Central Cyanosis: results from a cardiopulmonary problem
Peripheral Cyanosis: may be a local problem resulting from vasoconstriction
ASSESSMENT PROCEDURE
Inspect for color variations.
Inspect localized parts of the body, noting any color variation
NORMAL FINDINGS
Keep in mind that some clients have suntanned areas, freckles, or white patches known as vitiligo. The variations are due to different amounts of melanin in certain areas. A generalized loss of pigmentation is seen in albinism. Dark-skinned clients have lighter color palms, soles, nailbeds, and lips. Freckle-like or dark steaks of pigmentation are also common in the sclera and nailbeds of dark-skinned clients
***White skinned clients have darker pigmentation around nipples, lips, and genitalia
ABNORMAL FINDINGS
Abnormal findings include rashes, such as the reddish (in lightskinned people) butterfly rash across the bridge of the nose and cheeks, characteristic of the disease, Discoid
Erythematosus (DLE)
Lupus
Albinism is generalized loss of pigmentation
Erythema (skin redness and warmth) is seen in inflammation, allergic reactions, or trauma
Erythema in the dark-skinned client may be difficult to see.
However, the affected skin feels swollen and warmer than the surrounding skin
Check skin integrity, especially carefully in pressure point areas (ex. sacrum, hips, elbows) . If any skin breakdown is noted, use a scale to document the degree of skin breakdown
Clinical tip: In the obese client, carefully inspect skin on the limbs, under breasts, and in the groin area where problems are frequent.
Skin is intact, and there are no reddened areas
Signs of Skin Breakdown (Ulcers)
Skin breakdown is initially noted as a reddened area on the skin that may progress to serious and painful pressure ulcers.
Depending on the color of the client’s skin, reddened areas may not be prominent, although the skin may feel warmer in the area of breakdown than elsewhere.
During any skin assessment, the nurse remains watchful for signs of skin breakdown, especially in cases of limited mobility or fragile skin (ex. in elderly or bedridden clients). Pressure ulcers, which lead to complications such as infection, are easier to prevent than to treat.
Notable pressure ulcer sites:
Occipital bone Heel Lateral Knee
Scapula
Spinous Process
Elbow
Iliac Crest
Sacrum
Ischium
Achilles Tendon
Sole
Ear
Shoulder
Anterior Iliac Spine
Trochanter
Thigh
Medial Knee
Lower Leg
Medial Malleolus
Lateral Malleolus
Lateral Edge of Foot
Posterior Knee
Some risk factors for skin breakdown leading to pressure ulcers include:
Poor circulation
Poor hygiene
Infrequent position changes
Dermatitis
Infection
Traumatic wounds
Stages of Pressure Ulcers:
Stage 1: Skin in unbroken but appears red; no blanching when pressed
Stage 2: Skin is broken, and there is superficial skin loss involving the epidermis alone or also the dermis. The lesion resembles a vesicle, erosion, or blister
Stage 3: Pressure area involves epidermis, dermis, and subcutaneous tissue.
The ulcer resembles a crater. Hidden areas of damage may extend
through the subcutaneous tissue beyond the borders of the external lesion but not through underlying fascia.
Stage 4: Pressure area involves epidermis, dermis, subcutaneous tissue, bone, and other support tissue. The ulcer resembles a massive crater with hidden areas of damage in adjacent tissue.
ASSESSMENT PROCEDURE
Inspect for lesions.
Observe the skin surface to detect abnormalities. Note color, shape, and size of lesion. For very small lesions, use a magnifying glass to note these characteristics
Clinical tip: When examining female or obese clients; lift the breasts (or ask the client to lift them) and skin folds to inspect all areas for lesions.
Perspirations and friction often cause skin problems in these areas in obese clients.
If you suspect a fungus, shine a
Wood’s light (an ultraviolet light filtered through a special glass) on the lesion
NORMAL FINDINGS
Smooth, without lesions.
Stretch marks (striae) , healed scars, freckles, moles, or birthmarks are common findings.
***Older clients may have skin lesions because of aging. Some examples are seborrheic or senile keratoses, senile lentigines, cherry angiomas, purpura, and cutaneous tags and horns
Common skin variations:
Freckles
Vitiligo
Striae
Seborrheic Keratosis
Scar
Mole
Cutaneous tags
Cutaneous horn
Cherry angioma
Lesion does not fluoresce
THE PRIMARY LESIONS
ABNORMAL FINDINGS
Lesions may indicate local or systemic problems.
Primary lesions arise from normal skin due to irritation or disease.
Secondary lesions arise from changes in the primary lesions.
Vascular lesions, reddish-bluish lesions, are seen with bleeding, venous pressure, aging, liver disease, or pregnancy.
Skin cancer lesions can be either primary or secondary lesions and are classified as squamous cell carcinoma, basal cell carcinoma, or malignant melanoma.
Blue-green fluorescence indicates fungal infections
TYPE AND DESCRIPTION
Macule, Patch
Flat, non-palpable skin color change (skin color may be brown, white, tan, purple, red)
Macule: <1cm, circumscribed border
Patch: >1cm, may have irregular border
Papule and Plaque
An elevated, palpable solid mass, with a circumscribed border
Papule: <0.5cm
Plaque: >0.5cm flat top)
(may be coalesced papules with a
EXAMPLES
Freckles
Flat moles
Petechiae
Rubella
Vitiligo
Port wine stains
Ecchymosis
Papules:
Elevated nevi
Warts
Lichen planus
Nodule and Tumor
Vesicle and Bulla
Circumscribed, elevated, palpable mass, containing serous fluid
Vesicle: <0.5cm
Bulla: >0.5cm
Wheal
Elevated mass with transient borders
Often irregular
Size and color vary
Caused by movement of serous fluid into the dermis
Does not contain free fluid in a cavity (e.g. vesicle)
Pustule
Pus-filled vesicle or bulla
Cyst
Elevated, solid, palpable mass
Extends deeper into dermis than a papule
Nodule: 0.5-2cm; circumscribed
Tumor: >1.2cm; doesn’t always have sharp borders
Encapsulated fluid-filled or semisolid mass
Located in the subcutaneous tissue or dermis
THE SECONDARY LESIONS
Plaques:
Psoriasis
Actinic keratosis
Nodules:
Lipoma
Squamous cell carcinoma
Poorly absorbed injection
Dermatofibroma
Tumors:
Larger lipoma
Carcinoma
Vesicles:
Herpes Simplex/Zoster
Varicella (Chickenpox)
Poison Ivy
Second-degree burn
Bulla:
Pemphigus
Contact dermatitis
Large burn blisters
Poison ivy
Bullous impetigo
Urticaria (hives)
Insect bites
Acne
Impetigo
Furuncles
Carbuncles
Sebaceous cyst
Epidermoid cyst
TYPE AND DESCRIPTION
Erosion
Loss of superficial epidermis
Does not extend to the dermis
Depressed, moist area
Ulcer
Skin loss extending past epidermis
Necrotic tissue loss
Bleeding and scarring possible
Scar (Cicatrix)
Skin mark left after healing of wound or lesion
Represents replacement by connective tissue of the injured tissue
Young scars: red or purple
Mature scars: white or glistening
EXAMPLES
Rupture vesicles
Scratch marks
Aphthous ulcer
Stasis ulcer of venous insufficiency
Pressure ulcer
Healed wound
Healed surgical incision
Fissure
Linear crack in the skin
May extend to the dermis
Scales
Flakes secondary to desquamated, dead epithelium
Flakes may adhere to skin surface
Color varies (silvery, white)
Texture varies (thick, fine)
Crust
Dried residue of serum, blood, or pus on skin surface
Large adherent crust is a scab
Keloid
Hypertrophied scar tissue
Secondary to excessive collagen formation during healing
Elevated, irregular, red
Greater incidence in African Americans
Atrophy
Thin, dry, transparent appearance of epidermis
Loss of surface markings
Secondary to loss of collagen and elastin
Underlying vessels may be visible
Lichenification
Thickening and roughening of the skin
Accentuated skin markings
May be secondary to repeated rubbing, irritation, scratching
THE VASCULAR LESIONS
A.
Petechia (Petechiae – plural)
Round red or purple macule
Small: 1-2 mm
Eczema
Keloid of ear piercing
Chapped lips or hands
Athlete’s foot
Dandruff
Psoriasis
Dry skin
Pityriasis rosea
Residue left after vesicle rupture
Impetigo
Herpes
Keloid of surgical incision
Aged skin
Arterial insufficiency
Contact dermatitis, often resulting from exposure to aero allergens, chemicals, foods, and emotional stress
Secondary to blood extravasation
Associated with bleeding tendencies or emboli to skin
B.
Ecchymosis (Ecchymoses – plural)
Round or irregular macular lesion
Larger than petechia
Color varies and changes: black, yellow, and green hues
Secondary to blood extravasation
Associated with trauma, bleeding tendencies
C.
Hematoma
A localized collection of blood creating an elevated ecchymosis
Associated with trauma
D.
Cherry Angioma
Papular and round
Red or purple
Noted on trunk, extremities
May blach with pressure
Normal age-related skin alteration
Usually not clinically significant
E.
Spider Angioma
Red, arteriole lesion
Central body with radiating branches
Noted on face, neck, arms, trunk
Rare below waist
May blanch with pressure
Associated with liver disease, pregnancy and vitamin B deficiency
F.
Telangiectasis (Venous Star)
Shape varies: spiderlike or linear
Color bluish or red
Does not blanch when pressure is applied
Noted on legs, anterior chest
Secondary to superficial dilation of venous vessels and capillaries
Associated with increased venous pressure states (varicosities)
SKIN CANCER
With the exception of malignant melanoma, most skin cancers are easily seen and easily cured, or at least controlled. Malignant melanoma can be deadly if not discovered and treated early, which is one reason why professional health assessment and skin-health assessment can be life-saving procedures.
Malignant melanoma is usually evaluated according to the mnemonic ABCDE:
A: Assymetrical
B: Borders that are irregular (uneven or notched)
C: Color variations
D: Diameter exceeding 1/8 to 1/4 of an inch
E: Elevated, not flat
Other warning signs include itching, tenderness, or pain, and a change in size or bleeding of a mole. New pigmentations are also warning signs
The most commonly detected skin cancers include basal cell carcinoma, squamous cell carcinoma, and Kaposi’s sarcoma.
ASSESSMENT PROCEDURE
If you observe a lesion, note its location, distribution, and configuration. Measure the lesion with a centimeter ruler
NORMAL FINDINGS
Normal lesions may be moles, freckles, birthmarks, and the like. They may be scattered over the skin in no particular pattern
CONFIGURATIONS OF LESIONS
ABNORMAL FINDINGS
Refer to the table below
CONFIGURATIONS
Discrete
Individual, separate and distinct
Grouped
Lesions are clustered
Confluent
Lesions merge and run together
Linear or Serpiginous
Lesions that form a line or snakelike shape
Annular
Lesions arranged in a circular pattern
Polycyclic or Targetoid
Lesions arranged in concentric circles resembling a bull’s eye
Generalized
Scattered over the body
Zosteriform
Linear arrangement along a nerve root
PALPATION
Insect bites
Herpes Simplex
EXAMPLES
Childhood exanthema
Poison ivy, dermatitis, hookworm
Ringworm
Eruptions from drug reactions such as urticaria, erythema multiforme
Measles
Herpes Zoster
ASSESSMENT PROCEDURE
Palpate skin to assess texture.
Use the palmar surface of your three middle fingers to palpate skin texture
Palpate to assess thickness. If lesions are noted when assessing skin thickness, put gloves on and palpate the lesion between the thumb and finger. Observe for drainage or other characteristics
Palpate to assess moisture.
Check under skin folds and in unexposed areas
Clinical tip: Some nurses believe that using the dorsal surfaces of the hands to assess moisture leads to a more accurate result
NORMAL FINDINGS
Skin is smooth and even
Skin is normally thin, but calluses (rough, thick secretions of epidermis) are common on areas of the body that are exposed to constant pressure
Skin surfaces vary from moist to dry depending on the area assessed. Recent activity or a warm environment may cause increased moisture
***The older client’s skin may feel dryer than a younger client’s skin because sebum production decreases with age
ABNORMAL FINDINGS
Rough, flaky, dry skin is seen in hypothyroidism. Obese clients often report dry, itchy skin
Very thin skin may be seen in clients with arterial insufficiency or in those on steroid therapy
Increased moisture or diaphoresis
(profuse sweating) may occur in conditions such as fever or hyperthyroidism. Occurrence of decreased moisture is associated with dehydration or hypothyroidism
Clammy skin is typical in shock or hypotension
Palpate to assess temperature
Use the dorsal surfaces of your hands to palpate the skin
Clinical tip: You may also want to palpate with the palmar surfaces of your hands because current research indicates that these surfaces of the hands and fingers may be more sensitive to temperature
Palpate to assess mobility and turgor. Ask the client to lie down. Using two fingers, gently pinch the skin on the sternum or under the clavicle.
Mobility refers to how easily the skin can be pinched.
Turgor refers to the skin’s elasticity and how quickly the skin returns to its original shape after being pinched.
Palpate to detect edema. Use your thumbs to press down on the skin of the feet or ankles to check for edema (swelling related to accumulation of fluid in the tissue)
Skin is normally a warm temperature
Skin pinches easily and immediately returns to its original position.
***The older client’s skin loses its turgor because of a decrease in elasticity and collagen fibers. Sagging or wrinkled skin appears in the facial, breast, and scrotal areas.
Skin rebounds and does not remain indented pressure is released when
Cold skin may accompany shock or hypotension. Cool skin may accompany arterial disease. Very warm skin may indicate a febrile state or hyperthyroidism
Decreased mobility is seen with edema. Decreased turgor seconds)
(a slow return of the skin to its normal state taking longer than 30
is seen in dehydration.
Indentations on the skin may vary from slight to great and may be one area or all over the body.
HAIR AND SCALP ASSESSMENT
INSPECTION AND PALPATION
ASSESSMENT PROCEDURE
Have the client remove any hair clips, hair pins, or wigs.
Then inspect the scalp and hair for general color and condition
At 1-inch intervals, separate the hair from the scalp and inspect and palpate the hair and scalp for cleanliness, dryness or oiliness, parasites, and lesions. Wear gloves if lesions are suspected or if hygiene is poor.
NORMAL FINDINGS
Natural hair color is opposed to chemically colored hair, varies among clients from pale blond to black to gray or white. The color is determined by the amount of melanin present.
Scalp is clean and dry. Sparse dandruff may be visible. Hair is smooth and firm, somewhat elastic. However, as people age, hair feels coarser, and drier.
ABNORMAL FINDINGS
Nutritional deficiencies may cause patchy gray hair in some clients. Severe malnutrition in
African-American children may cause copper-red hair color
Excessive scaliness may indicate dermatitis. Raised lesions may indicate infections or tumor growth. Dull, dry hair may be seen with hypothyroidism and malnutrition. Poor hygiene may indicate a need for client teaching or assistance with ADL
Inspect amount and distribution of scalp, body, axillae, and pubic hair. Look for unusual growth elsewhere on the body.
***Individuals of Black
American descent often have very dry scalps and dry, fragile hair, which the client may condition with oil or a petroleum jelly-like product.
(This kind of hair is of genetic origin and not related to thyroid disorders or nutrition.
Such hair needs to be handled very gently)
Varying amounts of terminal hair cover the scalp, axillary, body and pubic areas according to normal gender distribution. Fine vellus hair covers the entire body except for the soles, palms, lips, and nipples. Normal male pattern balding is symmetric.
***Older clients have thinner hair because of a decrease in hair follicles. Pubic, axillary, and body hair also decrease with aging. Alopecia is seen, especially in men. Hair loss occurs from the periphery of the scalp and moves to the center.
Elderly women may have terminal hair growth on the chin owing to hormonal changes
Excessive generalized hair loss may occur with infection, nutritional deficiencies, hormonal disorders, thyroid or liver disease, drug toxicity, hepatic or renal failure. It may also result from chemotherapy or radiation therapy.
Patchy hair loss may result from infections of the scalp, Discoid or
Systemic Lupus Erythematosus, and some types of chemotherapy
Hirsutism (facial hair on females) is a characteristic of Cushing’s disease and results from an imbalance of adrenal hormones or it may be a side effect of steroids.
NAIL ASSESSMENT
INSPECTION
ASSESSMENT PROCEDURE
Inspect nail grooming and cleanliness
Inspect markings nail color
Inspect shape of nails and
NORMAL FINDINGS
Nails are clean and manicured
Pink tones should be seen.
Some longitudinal ridging is normal
***Dark-skinned clients may have freckles or pigmented streaks in their nails
There is normally a 160-degree angle between the nail base and the skin
ABNORMAL FINDINGS
Dirty, broken, or jagged fingernails may be seen with poor hygiene. They may also result from the client’s hobby or occupation.
Pale or cyanotic nails may indicate hypoxia or anemia.
Splinter hemorrhages may be caused by trauma
Beau’s lines occur after acute illness and eventually grow out.
Yellow discoloration may be seen in fungal infections or psoriasis.
Nail pitting is common in psoriasis.
Nail pitting is common in psoriasis
Early clubbing (180-degree angle with spongy sensation) and late clubbing (greater than 180degree angle) can occur from hypoxia. Spoon nails (concave) may be present with iron deficiency anemia
COMMON NAIL DISORDERS
DISORDER
Beau’s Lines
Transverse depression in nails indicating temporary disturbance of nail growth
(nails grow over for several months)
Clubbing
Early clubbing (180 degrees)
Late clubbing (> 180 degrees)
Change in angle between nail and nail base; nail bed softening, with nail flattening often
Koilonychia / Spoon Nails
Concave curvature of the nails
Pitting
Pit formation on the nails
Splinter Hemorrhages
Red or brown linear streaks in nail bed
CAUSES
Acute illness
Systemic illness such as severe infection or nail injury
Chronic lack of oxygen due to heart or any pulmonary disease
Iron-deficiency anemia
Syphilis
Use of strong detergents
Psoriasis
Minor trauma
Subacute Bacterial Endocarditis
Trichinosis
Paronychia
Inflammation of skin at the base of the nail
PALPATION
Local infection
Trauma
ASSESSMENT PROCEDURE NORMAL FINDINGS
Palpate nail to assess texture Nails are hard and basically immobile
***Dark-skinned clients may
Palpate to assess texture and consistency, noting whether nailplate nailbed is attached to
Test capillary refill in nailbeds by pressing the nail tip briefly and watching for color change have thicker nails
***Older clients’ nails may appear thickened, yellow, and brittle because of decreased circulation in the extremities
Nails are smooth and firm; nailplate should be firmly attached to nailbed
Pink immediately to blanched nailbeds when pressure is released tone returns
ABNORMAL FINDINGS
Thickened nails (especially toenails may be caused by decreased circulation)
Paronychia indicates local infection. Detachment of nailplate from nailbed (onycholysis) is seen in infections or trauma
There is slow (greater than 2 seconds) capillary nailbed refill
(return of pink tone) with respiratory or cardiovascular disease that cause hypoxia
DOCUMENTATION OF FINDINGS
Sample Objective Data:
Skin is pink, warm, dry and elastic
(+) freckles across the nose and cheeks
(--) lesions or excoriations
(+) old appendectomy scar @ the RLQ, 4 in. long, thin, and white
With brown hair of shoulder length, clean and shiny
With evenly distributed hair along the scalp and perineum
Nails form 160-degree angle at base, hard, smooth, and immobile
Fingernails well manicured with clear enamel
Toenails clean and well-trimmed
(+) pink nailbeds without clubbing
(+) smooth cuticles
(--) nail plate detachment
With good capillary refill @ 2 secs.
APPROPRIATE NURSING DIAGNOSES
Wellness Diagnoses
Readiness for enhanced skin, hair, and nail integrity related to healthy hygiene and skin care practices, avoidance of overexposure to sun
Health-seeking behavior: Requests information on skin reactions and effects of using a sun-tanning lotion
Risk Diagnoses
Risk for impaired skin integrity related to excessive exposure to cleaning solutions and chemicals
Risk for impaired skin integrity related to prolonged sun exposure
Risk for imbalanced body temperature related to immobility, decreased production of natural oils, and thinning skin
Risk for impaired skin integrity of toes related to thickened, dried toenails
Risk for imbalanced body temperature related to severe diaphoresis
Risk for infection related to scratching of rash
Risk for impaired nail integrity related to prolonged used of nail polish
Risk for altered nutrition: Less than body requirements related to increased vitamine and protein requirements necessary for healing of wound.
Actual Diagnoses
Ineffective health maintenance to lack of hygienic care of the skin, hair and nails
Impaired skin integrity related to immobility and decreased circulation
Impaired skin integrity related to poor nutritional intake and bowel/bladder incontinence
Disturbed body image related to scarring, rash, or other skin condition that alters skin appearance
Disturbed sleep pattern related to persistent itching of the skin
Deficient fluid volume related to excessive diaphoresis secondary to excessive exercise and high environmental temperatures
PATIENT AND FAMILY EDUCATION WITH HOME HEALTH TEACHINGS
Skin:
1.
Instruct client how to reduce the risk of skin cancer by avoiding over exposure to the sun: wear wide-brimmed hats and long sleeves, use sunscreens with SPF greater than or equal to 15 approximately 15 minutes before going into the sun and after swimming or perspiring, avoid tanning at midday (11AM-2PM) and do not use indoor sunlamps, tanning parlors, or tanning pills.
2.
Teach the client to conduct a monthly self examination of the skin noting any moles, blemishes, or birthmarks. Tell client to inspect all skin surfaces. A family member can assist with hard to see areas of the skin
3.
Tell the client to report to a physician any changes in the size, shape, or color of lesions or a sore that does not heal. Older adults tend to have delayed wound healing. Instruct the client to report to a physician any lesions that bleed.
4.
Tell the client to apply alcohol-free lotion and moisturizer regularly to the skin to reduce itching and drying.
5.
Instruct adolescents on proper skin cleansing and the importance of balanced diet and adequate rest.
Hair and Scalp
1.
Clients may require instruction about basic hygiene measures, including shampooing and combing the hair
2.
Instruct clients who have head lice to shampoo thoroughly with a pediculicide, comb thoroughly with fine-tooth comb, and discard comb
3.
Instruct the client who has lice about ways to reduce transmission: a.
Do not share personal care items with others b.
Vacuum all rugs, furniture, and flooring thoroughly and discard vacuum bag c.
Use thorough hand washing d.
Launder all clothing, linen, and bedding in hot soap and water and dry in hot dryer.
Nails
1.
Instruct the client to cut nails only after soaking them at least 10 minutes in warm water.
2.
Caution client against the use of OTC preparations to treat corns, calluses, or ingrown toenails.
3.
Tell client to cut nails straight across and even with tops of fingers and toes. If client has
Diabetes Mellitus, tell client to file, not cut, nails.
4.
Instruct client to shape nails with a file or emery board.