Drug Allergy Update
advertisement

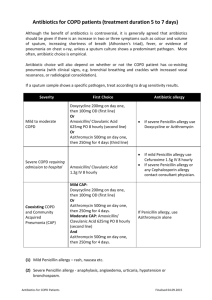
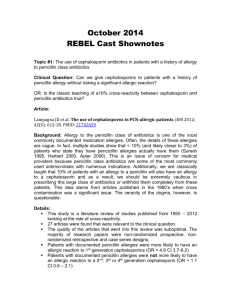
6/13/2014 Drug Allergy Update Disclosures Gap in Knowledge • None. • Fill a gap in knowledge regarding the evaluation and management of adverse drug reactions and drug allergies. • No discussion of off-label uses of medications. • No commercial support provided for this activity. Thanai Pongdee, MD, FAAAAI Division of Allergy and Pulmonary Medicine Mayo Clinic, Jacksonville ,FL SOWEGA-AHEC CURE Activity 06.17.14 ©2011 MFMER | slide-2 ©2011 MFMER | slide-3 ©2011 MFMER | slide-4 Adverse Drug Reactions (ADRs): Why is this important? Adverse Drug Reactions (ADRs): Definition Objectives • Most useful components of history in drug allergy evaluation • ADR- “Any noxious, unintended and undesirable effect of a drug, which occurs at standard doses when administer by proper route in humans for prevention, diagnosis, or treatment.” • How to manage beta-lactam allergies • For sulfa allergy, should all sulfa medications be avoided? • Adverse drug reactions are a major health problem in the United States1 • Over 2 MILLION serious ADRs yearly2 • 100,000 DEATHS yearly2 • Fourth-leading cause of death after heart disease, cancer, and stroke2 • Approximately 24% of hospitalized patients report reactions to antibiotics1 • Aspirin/NSAID allergy – do all NSAIDs have to be avoided? WHO. 1966. Technical Report Series No. 425 • What is drug desensitization and who is eligible? • Penicillin most frequently reported allergy1 • 1. Lee CE et al. Arch Inter Med 160:2819, 2000 • 2. Lazarou J, Pomeranz BH, Corey PN. JAMA. 1998;279:1200-1205. ©2011 MFMER | slide-5 Classification of adverse drug reactions Nomenclature Nomenclature Drug hypersensitivity • Immune mediated drug hypersensitivity (drug allergy) • Type A: predictable; strictly dose dependent • 80% of all side effects • Pharmacological side effects (e.g. gastrointestinal bleeding under treatment with NSAID) • Type B: not predictable; usually not dose dependent, and sometimes reactions to very small amounts • • • • 15-20% of all side effects Immunologic/allergic Non-immune mediated, “pseudoallergic” Idiosyncratic • Clinical symptoms due to different types of specific immune reactions (T-cell & B-cell/Ig mediated) Drug allergy Non-allergic hypersensitivity eg: Non-specific histamine release, Arachidonic acid pathway activation, Bradykinin pathway alteration, Complement activation • Non immune mediated drug hypersensitivity (non-allergic drug hypersensitivity) • Symptoms and signs similar to immune mediated hypersensitivity, but failure to demonstrate a specific immune process to the drug • Older term: “pseudoallergy” IgE-mediated Non IgE mediated drug allergy drug allergy • Idiosyncrasy • symptoms and signs due to some genetic alterations, e.g. an enzyme deficiency: e.g. hemolytic anaemia due to certain drugs in patients with G-6-P-deficiency Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature for allergy for global use: Report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol 2004;113:832-6 1 6/13/2014 Allergic Drug Reactions Patient’s history is an important component of the evaluation of drug allergies Gell and Coombs Classification • Type I - IgE Mediated • Example: Penicillin induced anaphylaxis • Type II – IgG or IgM cytotoxic mediated • Example: Penicillin-induced hemolytic anemia/ heparin induced thrombocytopenia • Type III - Immune Complex-Dependent • Example: Penicillin causing serum sickness • Type IV - Delayed Hypersensitivity • Example: Penicillin used topically causing contact dermatitis • What is the name of the medication and route? • How long ago did the reaction occur?* • Which systems were involved in the reaction?* • What were the characteristics of the reaction?* • When during the course did the reaction occur?* Patient’s history is an important component of the evaluation of drug allergies • Had the patient taken the same or a cross-reacting medication before the reaction? • Has the patient been exposed to the same or similar medication since the reaction?* • Has the patient experienced similar reactions in the absence of drug treatment?* • Why was the medication prescribed? • Does the patient have an underlying condition that favors reactions to certain medications? • What other medications was the patient taking concurrently at the time of the reaction?* • How long did it take for the reaction to resolve? • How was the reaction treated? • Review the medical record* Khan D et.al. J Allergy Clin Immunol. 2010;125:S126-137. Khan D et.al. J Allergy Clin Immunol. 2010;125:S126-137. Drug Allergy Testing • Is there a safe validated diagnostic test available? • If not, are there alternative medications available? • Drug challenge vs. desensitization Khan D et.al. J Allergy Clin Immunol. 2010;125:S126-137. Penicillin Allergy Penicillin Allergy • 63-year-old female • 85-year-old male • Adverse reaction to penicillin when she was a teenager • Adverse reaction to penicillin in the 1940s • Received oral penicillin and subsequently developed hives on her arms, facial swelling as well as the sensation of throat swelling and dyspnea • Recalls receiving an injection of penicillin into his finger and subsequently developing generalized hives and angioedema. He does not recall any respiratory distress or gastrointestinal distress. He was not hospitalized and did not seek emergency care. • Treated at ER • She was told she was allergic to penicillin and has avoided its use since that time. • Symptoms resolved after two to three days. • He was told he was allergic to penicillin and has avoided penicillin use since that time. Penicillin Allergy • 36-year-old female • States her mother told her she had an adverse reaction to penicillin when she was three years old. Recommendations for these patients? • Developed some type of rash after taking penicillin. No other specific details are known. A) Continue avoidance of penicillin and find an alternative antibiotic • She was told she was allergic to penicillin and has avoided its use since that time. B) Penicillin allergy skin testing What is the negative predictive value (NPV) and positive predictive value (PPV) of penicillin skin testing? A) NPV = ~80% PPV = ~80% B) NPV = ~50% PPV = almost 100% C) NPV = almost 98% PPV = ~50% C) These reactions happened so long ago, penicillin should be safe to give. 2 6/13/2014 Penicillin Allergy - Epidemiology Structures of Penicillin Allergenic Determinants Penicillin Allergenic Determinants • About 10% of the population self-reports “penicillin allergy” • ~90% are NOT allergic and able to tolerate penicillin Penicillin • Mayo Experience: ~97% of the patients who have a history of penicillin allergy are pcn skin test negative1,2,3,4,5 95% • Why the discrepancy between “claimed” and “real” penicillin allergy? • Previous reaction predictable, not truly allergic • Previous reaction due to underlying illness • Previous reaction due to interaction between illness/antibiotic • Penicillin allergy wanes and may resolve over time 1.Park MA et al. Ann Allergy Asthma Immunol 97 (2006): 681-87. 2.Frigas E. et al. Mayo Clinic Proceedings. 2008; 83(6): 651-657. 3.Park MA et al. Ann Allergy Asthma Immunol 99 (2007): 54-58. 4.Park MA, et al. International Archives of Allergy and Immunology 2010; 153(3):268-273. 5.Park MA, et al. International Archives of Allergy and Immunology 2011; 154:57-62. PrePen (penicilloyI-polylysine) 1. Sogn et al. demonstrated that among 167 patients with a positive PCN skin test, 140 (84%) of the patients were skin test positive to the PPL. Major determinant (Penicilloyl) 5% Penicilloyl Penicilloate Penilloate Minor determinants (Penicilloate, Penilloate) *Gadde J, Spence M, Wheeler B, Adkinson NF, Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. Jama 1993; 270:2456-63. Sogn DD, Evans R, 3rd, Shepherd GM, et al. Results of the National Institute of Allergy and Infectious Diseases Collaborative Clinical Trial to test the predictive value of skin testing with major and minor penicillin derivatives in hospitalized adults. Arch Intern Med 1992; 152:1025-32. Penicillin skin test • Penicillin skin test is designed to detect IgE antibodies to the components of penicillin 2. Gadde et al. reported that 115 (89.8%) of 128 patients with a positive PCN test were positive to the PPL. 3. However, several recent studies have shown a less robust detection of PCN allergy by PPL (64%-69%).* Penicillin • Penicillin skin test has been validated for IgE mediated reactions to PCN* Penicillin Skin Testing Predictive Value • Negative predictive value (using both major and minor determinants) approaches 100% • Gadde et al. studied a total of 5,063 outpatients with and without a history of PCN allergy. • 3% h/o PCN allergy/negative ST/challenged w/ PCN had an IgE mediated reaction to PCN • vs. 0.2% w/o h/o PCN allergy/negative ST/challenged w/ PCN • Sogn et al. *Blanca M, Romano A, Torres MJ, et al. Update on the evaluation of hypersensitivity reactions to betalactams. Allergy 2009; 64:183-93. Wong BB, Keith PK, Waserman S. Clinical history as a predictor of penicillin skin test outcome. Ann Allergy Asthma Immunol 2006; 97:169-74. Goldberg A, Confino-Cohen R. Skin testing and oral penicillin challenge in patients with a history of remote penicillin allergy. Ann Allergy Asthma Immunol 2008; 100:37-43. Jost BC, Wedner HJ, Bloomberg GR. Elective penicillin skin testing in a pediatric outpatient setting. Ann Allergy Asthma Immunol 2006; 97:807-12. *Gadde J, Spence M, Wheeler B, Adkinson NF, Jr. Clinical experience with penicillin skin testing in a large inner-city STD clinic. Jama 1993; 270:2456-63. Sogn DD, Evans R, 3rd, Shepherd GM, et al. Results of the National Institute of Allergy and Infectious Diseases Collaborative Clinical Trial to test the predictive value of skin testing with major and minor penicillin derivatives in hospitalized adults. Arch Intern Med 1992; 152:1025-32. • 1.2% (726 h/o pcn allergy/negative ST) • vs. 0% (568 negative h/o pcn allergy/negative ST) had an IgE mediated ADR to challenge with PCN Gadde et al. JAMA 1993; 270 (20); 2456-2463 Sogn et al. Arch Intern Med. 1992;152:1025-1032 Penicillin Skin Testing Predictive Value Penicillin Skin Testing Whom to Skin Test After the Skin Test • • Any patient with a history of a reaction to a penicillin class antibiotic that may have been IgE-mediated Skin test positive patients 1-3% of skin test-negative patients develop a mild reaction upon being challenged with penicillin • Rank MA, Park MA*. Anaphylaxis to piperacillin-tazobactam despite negative skin tests. Allergy. August 2007; 62(8): 964-5 • Patient’s reaction history is known to be a poor predictor of skin test reactivity • Many patients cannot recall specifics of their reaction • Penicillin skin testing is not predictive of non-IgE-mediated reactions (Stevens-Johnson syndrome, interstitial nephritis, hemolytic anemia, etc.) • Patients with convincing histories (i.e., anaphylaxis) lose penicillin-specific IgE antibodies over time Penicillin Skin Testing • Avoid all penicillins • Consider reevaluation in 3-5 years • If develop absolute need for penicillin – desensitize • Patients with vague histories could be allergic • Review of published studies revealed that among history-positive/skin test-positive patients, 1/3 had a vague reaction history* Solensky R et al: Ann Allergy Asthma Immunol 85:195, 2000 3 6/13/2014 Penicillin Skin Testing After the Skin Test Skin test negative patients What is the negative predictive value (NPV) and positive predictive value (PPV) of penicillin skin testing? • Low likelihood of an IgE mediated adverse reaction to PCN A) NPV = ~80% PPV = ~80% • In children and those with a history of anaphylaxis that is recent, consider oral challenge B) NPV = ~50% PPV = almost 100% C) NPV = almost 98% PPV = ~50% First principal of drug allergy • If an alternative medication that is equally efficacious, then give alternative medication • However, if no alternative medication is available, then testing or drug challenge or desensitization is warranted. Which penicillin skin test reagent do patients with a history of an IgE mediated reaction to penicillin react to most often? A) PrePen (penicilloyI-polylysine) B) Penicillin G C) Penicilloate D) Amoxicillin 60 year old female had hives 20 years ago after taking penicillin and has avoided penicillin since the original reaction. She has a proven Strep throat infection. What would be the next best step? • A) Give azithromycin • B) Give penicillin VK • C) Penicillin skin test: if negative give penicillin VK • D) Give cephalexin 60 year old female had hives 20 years ago after taking penicillin and has avoided penicillin since the original reaction. She has a proven Strep throat infection. What is the probability that she is still allergic to penicillin? A) About 20% B) About 30% C) About 50% D) About 90% Waning penicillin allergy • After one year: • 67 to 82% still will be positive to skin testing • After 5 years: • ~40% still will be positive to skin testing Penicillin skin testing is not predictive for which type of allergic drug reaction? Allergic cross-reactivity between beta-lactam antibiotics may be due to: A) Anaphylaxis A) beta-lactam portion of the molecule B) Urticaria B) R-group side chains C) Interstitial nephritis C) Either A or B D) Bronchospasm • After 10 years: • ~20% still will be positive to skin testing Blanca et al. JACI 1999; 103:918-24 Chandra et al. Arch Dis Child 1980; 55:857-860 4 6/13/2014 Beta-lactam Structures R-side chains Beta-lactam ring What is the cross-reactivity between penicillins and cephalosporins? Cephalosporin Challenges in Patients with History of Penicillin Allergy Reference (Year) A) Approximately 3% Dash CH (1975) B) Approximately 15% Petz LD (1978) C) Approximately 50% Goodman EJ (2001) Dalat SB (2004) Cephalosporin Reaction Rate + History Pcn ‐ History Pcn Allergy Allergy 7.7% (25/324) 0.8% (140/17,216) 8.1% (57/701) 1.9% (285/15,007) 0.33% (1/300) 0.04% (1/2,431) 0.17% (1/606) Fonacier L (2005) 8.4% (7/83) 0.06% (15/22,664) N/A MacPherson RD (2006) 0% (0/84) N/A Comments No reaction details No reaction details Reaction questionable Reaction = eczema Reactions convincing Khan et al. J Allergy Clin Immunol 2010;125:S126-37. Cephalosporin Challenges in Penicillin ST+ Patients Reference (Year) # of Patients # (%) of Reactions Girard (1968) Assem (1974) Warrington (1978) Solley (1982) Saxon (1987) Blanca (1989) Shepherd (1993) Audicana (1994) Pichichero (1998) Novalbos (2001) Macy (2002) Romano (2004) Greenberger (2005) Park (2010) Ahmed (2012) 23 3 3 27 62 16 9 12 39 23 42 75 6 85 21 2 (8.7) 3 (100) 0 0 1 (1.6) 2 (12.5) 0 0 2 (5.1) 0 1 (2.4) 0 0 5 (6%) 0 446 16 (3.6%) TOTAL Cephalosporin Challenges in Penicillin STPatients Reference (Year) # of patients # (%) reactions Sullivan (1981) 23 0 Solley (1982) 151 2 (1.3) Cephalosporin challenges0 in Penicillin Shepherd and 159 Burton (1993) ST + 3.6% vs Penicillin ST – 0.7% Audicana (1994) 18 0 patients 5 (0.7%) Park (2010) 726 Ahmed (2012) 152 1 (0.7%) Total 1229 0.7% What is the cross-reactivity between penicillins and cephalosporins? A) Approximately 3% B) Approximately 15% C) Approximately 50% Khan et al. J Allergy Clin Immunol 2010;125:S126-37. Cephalosporin Administration to Patients with History of Penicillin Allergy Penicillin Administration to Patients with History of Cephalosporin Allergy Penicillin Allergy/Cephalosporins • Early reports of relatively high reaction rates to cephalosporin's in penicillin-allergic patients were likely due to: • Trace contamination of cephalosporin's with penicillin • Similarity of R-group side chains between benzylpenicillin and early 1st generation cephalosporins (cephalothin, cephaloridine, cefamandole) Solensky R, et al. Ann Allergy Asthma Immunol 2010; 105:259. Solensky R, et al. Ann Allergy Asthma Immunol 2010; 105:259. 5 6/13/2014 35 yo with a history of anaphylaxis to amoxicillin and positive to the penicillin skin test needs a carbapenem. The carbapenem is the best antibiotic for the patient and no equivalent antibiotic is available for the type of infection. What is the best next step: Beta-lactam Structures Carbapenem Challenges in Patients with History of Penicillin Allergy Beta-lactam ring Reference (Year) A) Give full dose Beta-lactam ring B) Give as a graded challenge McConnell SA (2000) Prescott WA (2004) Carbapenem Reaction Rate + History Penicillin ‐ History Penicillin Allergy Allergy 6.3% (4/63) N/A P Value N/A 11% (11/100) 2.7% (3/111) 0.024 Sodhi M (2004) 9.2% (15/163) 3.9% (4/103) 0.164 Cunha BS (2008) 0% (0/110) N/A N/A Khan D et.al. J Allergy Clin Immunol. 2010;125:S126-137. Carbapenem Challenges in Penicillin ST+ Patients Carbapenem Administration to Patients with a History of Penicillin Allergy Reference (Year) Negative Romano A (2006) Romano A (2007) # of Patients 110 103 # of Reactions Carbapenem Given 0 Imipenem 0 Meropenem Atanaskovic (2008) 107 0 Meropenem Atanaskovic (2009) 123 0 Imipenem Comment Skin test to penicillin Positive One patient imipenem ST+ 35 yo with a history of anaphylaxis to amoxicillin and positive to the penicillin skin test needs a carbapenem. The carbapenem is the best antibiotic for the patient and no equivalent antibiotic is available for the type of infection. What is the best next step: One patient meropenem ST+ One patient meropenem ST+ One patient imipenem ST+ • All challenged patients also skin test‐negative to carbapenems Khan D et.al. J Allergy Clin Immunol. 2010;125:S126-137. May safely administer carbapenem 1. Give alternate drug 2. Give carbapenem via graded challenge 3. Desensitize to carbapenem A) Give full dose B) Give as a graded challenge Aztreonam (Monobactams) Aztreonam (a monobactam beta-lactam antibiotic) does not cross react with other betalactams with the exception of: • Share common beta-lactam ring with penicillin Aztreonam • There is NO in vitro immunologic cross-reactivity between aztreonam and penicillins/cephalosporins with the exception of ceftazidime (which has the identical R-group side chain as aztreonam) A) Ceftazidime B) Cefazolin • All penicillin skin test-positive patients challenged with aztreonam tolerated the medication C) Cefuroxime Ceftazidime • Case reports of patients allergic to aztreonam being able to tolerate all other beta-lactams except ceftazidime 6 6/13/2014 60 year old female with a history of anaphylaxis to a cephalexin 10 years ago needs ceftriaxone. What is the next best step assuming no better alternative medication is available? • A. Give ceftriaxone because cephalosporins do not cross-react • B. Desensitize to ceftriaxone • C. Give ceftriaxone as a graded challenge • D. Cephalosporin skin test because cephalosporin skin test has been standardized Not a lot of data! Beta-lactam Structures R-side chains Beta-lactam ring • Themes: • Speculation that side chains of cephalosporins play a bigger role • Similar side chains more likely to be “allergic” • Dissimilar side chains less likely to be “allergic” Romano et al. Allergy 2002 Cross-reactivity among cephalosporins by skin test and in vitro testing Cephalosporin Administration to Patients with History of Cephalosporin Allergy The most common class of antibiotic to cause allergic reactions aside from penicillin is: • Cross-reactivity with similar side chains: • ~68% (67-69%) • Cross-reactivity with dissimilar side chains: A) Macrolides • ~30% (28.6-38%) B) Sulfonamides • However, data is very limited and need caution. C) Quinolones Solensky R KD, Bernstein IL, Bloomberg GR, Castells MC, Mendelson LM, Weiss ME, et al. Drug Allergy: An Updated Parameter. Ann Allergy 2010; 105:273e1-e78. Antunez C, Blanca-Lopez N, Torres MJ, Mayorga C, Perez-Inestrosa E, Montanez MI, et al. Immediate allergic reactions to cephalosporins: evaluation of cross-reactivity with a panel of penicillins and cephalosporins. J Allergy Clin Immunol 2006; 117:404-10. Atanaskovic-Markovic M, Velickovic TC, Gavrovic-Jankulovic M, Vuckovic O, Nestorovic B. Immediate allergic reactions to cephalosporins and penicillins and their cross-reactivity in children. Pediatr Allergy Immunol 2005; 16:341-7. Somech R, Weber EA, Lavi S. Evaluation of immediate allergic reactions to cephalosporins in non-penicillinallergic patients. Int Arch Allergy Immunol 2009; 150:205-9. Solensky R, et al. Ann Allergy Asthma Immunol 2010; 105:259. Boston Collaborative Drug Surveillance Program – Skin reaction rates* due to antibiotics • Amoxicillin – 51.4 • TMP-SMX – 33.8 • Ampicillin – 33.2 • Cephalosporins – 21.1 • Erythromycin – 20.4 • Penicillin G – 18.5 The most common type of allergic reaction caused by sulfonamide antibiotics is: A) Anaphylaxis * Reaction rate per 1000 recipients B) Serum sickness-like reaction C) Maculopapular eruption D) Drug fever Patients with a history of allergy to trimethoprimsulfamethoxazole (Septra) should avoid the following non-antibiotic sulfonamides: A) Celecoxib (Celebrex) B) Sumatriptan (Imitrex) C) Furosemide (Lasix) D) All of these E) None of these Bigby M, et al. JAMA 1986; 256:3358‐63. 7 6/13/2014 Sulfonamides Definitions • Sulfonamides = drugs containing an SO2-NH2 moiety • Sulfonamide antibiotics • Aromatic amine (arylamine) at N4 position • Substituted ring at N1 position Sulfonamide Antibiotics Sulfamethoxazole N4 Aromatic Amine • Non-antibiotic sulfonamides • No aromatic amine at N4 position • No substituted ring at N1 position • Examples • Diuretics: Furosemide, thiazide • Oral hypoglycemics: Glyburide, chlorpropamide • Carbonic anhydrase inhibitors: Acetazolamide, dorzolamide • Other: Celecoxib, sumatriptan Glyburide N1 Substituted Ring Furosemide Acetazolamide Sulfonamide Moiety Celecoxib Sulfonamides Cross-Reactivity Aspirin and NSAIDS Adverse Reaction Types • N4 aromatic amine – essential for non-IgE mediated reactions to sulfonamide antibiotics • N1 substituted ring – appears important for IgE-mediated reactions to sulfonamide antibiotics • Growing body of evidence showing no increased risk of allergic reactions to non-antibiotic sulfonamides in patients with history of allergy to sulfonamide antibiotics Patterson R et al: Clin Ther 21:2065, 1999; Storm BL et al: N Eng J Med 349:1628, 2003; Shapiro LE et al: Drug Safety 26:187, 2003; Morgan M et al: J Allergy Clin Immunol 113:S180, 2004; Khan et al. J Allergy Clin Immunol 2010;125:S126-37. Which of the following NSAIDs will patients with AERD (aspirin exacerbated respiratory disease) not react to? A) ibuprofen B) naproxen C) celecoxib D) ketorolac Hydrochlorothiazide Reaction Type Underlying disease Crossreactions NSAID-induced rhinitis and asthma (AERD – aspirin exacerbated Respiratory disease) Asthma, nasal polyps, sinusitis Yes NSAID-induced urticaria/angioedema Chronic idiopathic urticaria Yes Single drug-induced urticaria/angioedema None No Multiple drug-induced urticaria/angioedema None Yes Single drug-induced anaphylaxis None No Skin testing for allergic reactions to aspirin/NSAIDs is highly valuable. A) True AERD (aspirin exacerbated respiratory disease) prevalence B) False AERD Natural History • Rare in children less than 10 years old • Questionnaires • 0.6% to 2.5% in general population • 3.8% to 11% in asthmatics • Oral challenges • all asthmatics, 10-20% • asthma, rhinosinusitis, polyps, 30-40% • hx of ASA/NSAID resp rxns, 60-100% • Acquired disorder with onset of symptoms beginning between teenage years and age 40 years • Average ages of onset were 29 and 34 years in two large studies 8 6/13/2014 AERD Natural History AERD Natural History • First clinical manifestation is usually nasal congestion • ASA/NSAID- induced respiratory reactions can occur at any time • URI may be an inciting event • Despite avoidance of aspirin and NSAIDs, mucosal inflammation of the upper and lower respiratory tracts persists and progresses • Chronic rhinitis progresses to chronic hyperplastic eosinophilic sinusitis with nasal polyposis Respiratory Reactions to Aspirin and NSAIDs • Asthma either previously present or begins de novo between 3 months to 5 years after onset of nasal congestion and polyposis Respiratory Reactions to Aspirin and NSAIDs • Reactions usually occur within 30 to 60 minutes after ingesting full therapeutic doses, but can occur up to 3 hours later • Cross-reactivity among NSAIDs that inhibit COX-1 is 100% • Most common eliciting agents • Aspirin (80%) • Ibuprofen (41%) COX-1-Inhibiting NSAIDs that Cross-react with ASA Generic name Generic name Brand name Mefenamic acid Ponstel Indomethacin Sulindac Indocin Clinoril Flurbiprofen Diflunisal Ansaid Dolbid Tolmetin Tolectin Ketoprofen Orudis, Oruval Ibuprofen Motrin, Advil, Rufen Diclofenac Voltaren, Cataflam Naproxen Naproxen sodium Naprosyn Anaprox, Aleve Ketoralac Etodolac Toradol Lodine Fenoprofen Nalfon Nabumetone Relafen Meclofenamate Meclomen Oxaprozin Daypro • Partial cross-reactivity with partially selective COX2 inhibitors • Salsalate tolerated up to 2000mg COX-1-Inhibiting NSAIDs that Cross-react with ASA (cont.) Feldene Respiratory Reactions to Aspirin and NSAIDs • 28% with mild rxns to 1000mg • 6% with rxns at doses of 1500mg • Reactions include rhinorrhea, nasal congestion, ocular itching/tearing, laryngeal spasm, and asthma exacerbations Piroxicam • Partial cross-reactivity with poor inhibitors of COX-1 • Most patients can safely tolerate up to 500mg acetaminophen • Reactions occur to ASA and all NSAIDs that preferentially inhibit cyclooygenase (COX)-1 Brand name Respiratory Reactions to Aspirin and NSAIDs • acetaminophen • salsalate • Only occurs in patients with AERD • meloxicam • nimesulide • Lack of cross-reactivity with selective COX-2 inhibitors • celecoxib Diagnosis of AERD • Diagnosis can be definitively established only through provocative aspirin challenges • No reliable in vitro test • 4 types of provocation challenges • • • • Oral Inhalation Nasal Intravenous 9 6/13/2014 Aspirin Desensitization AERD Treatment Aspirin Desensitization • Avoiding ASA/NSAIDs • Discovered in 1979 • ASA must be continued to maintain refractory state • Add-on treatment for underlying AERD • Indications: • Poorly controlled AERD • ASA/NSAID needed for CV disease, osteoarthritis, etc. • Does not prevent AERD from starting, continuing, and progressing • Eliminates acute respiratory reactions • Cross-desensitization with other NSAIDs • Treat underlying respiratory disease • Progressive administration of ASA leading to respiratory reac on → refractory state of tolerance • Treat underlying allergic inflammation Changes in clinical markers after aspirin desensitization Baseline ≥ 1 year after therapy Aspirin desensitization as add on therapy: • Clinical measures Median Range Median Range P values # sinus infections/yr 5.0 0-12 2.0 0-12 <0.0001 Olfactory scores 0.0 0-5 3.0 0-5 <0.0001 Nasal symptom scores 2.0 0-4 4.0 0-4 <0.0001 Asthma symptom scores 3.0 0-4 4.0 0-4 <0.0001 Sinus operations/yr Hospitalizations/yr ER visits/yr 0.22 0-3 0.0 0.0 0- 5 0.0 0-2 0-3 0.15 0-15 0.0 0-5 Effects of daily aspirin treatment <0.0001 <0.0001 <0.0001 Which of the following NSAIDs will patients with AERD (aspirin exacerbated respiratory disease) not react to? 1. 2. 3. 4. 5. 6. 7. 8. Decreases nasal congestion Decreases need for additional sinus/polyp surgery Decreases infectious sinusitis (from 5 to 2/year) Improves sense of smell Improves asthma control Reduces need for nasal corticosteroids Reduces need for bursts of systemic steroids Reduces daily systemic steroids (10.8 to 3.6 mg.) Most patients with a severe anaphylactic allergy to a specific NSAIDs are able to tolerate: A) ibuprofen A) Other NSAIDs B) naproxen B) No other NSAIDs C) celecoxib C) Only selective COX-2 inhibitors (like celecoxib) D) ketorolac Skin testing for allergic reactions to aspirins/NSAIDs is highly valuable. A) True B) False Drug tolerance induction (Desensitization) • Drug tolerance is defined as a state in which a patient with a drug allergy will tolerate a drug without an adverse reaction. • Drug tolerance does not indicate a permanent state of tolerance • Induction of drug tolerance procedures modify a patient’s response to a drug to temporarily allow treatment with it safely. Solensky R , et al. Drug Allergy: An Updated Parameter. Ann Allergy 2010; 105:273e1 - 273e78 . 10 6/13/2014 Drug tolerance induction (Desensitization) • They are indicated only in situations where an alternate non–cross-reacting medication cannot be used. • Induction of drug tolerance can involve IgE immune mechanisms, non-IgE immune mechanisms, pharmacologic mechanisms, and undefined mechanisms • All procedures to induce drug tolerance involve administration of incremental doses of the drug. 65 yo with a history of penicillin allergy (anaphylaxis) 20 years ago underwent penicillin skin testing. The penicillin skin test is positive and penicillin is the best medication. What percentage of patient’s will have a reaction to penicillin while undergoing penicillin desensitization? 1. 5% 2. 10% 3. 30% 4. 60% Solensky R , et al. Drug Allergy: An Updated Parameter. Ann Allergy 2010; 105:273e1 - 273e78 64 yo male underwent a successful “desensitization” to trimethoprim and sulfamethoxazole (Bactrim). After three weeks of consistently taking trimethoprim and sulfamethoxazole, the patient forgets to take it for three days. What is the best next step? A) Resume full dose trimethoprim and sulfamethoxazole since he is desensitized B) Proceed with a drug challenge to trimethoprim and sulfamethoxazole before being able to take the full dose C) Undergo a desensitization to trimethoprim and sulfamethoxazole Desensitization Take away points: Take away points: • Many medications can undergo successful desensitization • Penicillin skin test is only validated skin test for medications with high NPV • Drug desensitization may be considered if a medication is absolutely indicated. • Many have not been standardized Sulfonamide antibiotic desensitization is 80 to 90% successful in the short-term but decreases to 72% in the long-term1,2,3,4 • Growing body of evidence showing no increased risk of allergic reactions to non-antibiotic sulfonamides in patients with history of allergy to sulfonamide antibiotics • Patients with aspirin allergy and sulfonamide allergy can be desensitized as an outpatient in most cases • ASA desensitization for AERD can be done successfully as an outpatient • Aspirin desensitization should be considered for treatment of AERD • Contraindication: Severe non-IgE mediated ADR such as Stevens Johnson Syndrome, Toxic epidermal necrolysis, DRESS syndrome etc. • Not all patients with NSAID allergy need to avoid all NSAIDs • • Don’t challenge, test, or desensitize to patients with SJS, TEN, Serum Sickness, DRESS due to a medication 1.Bonfanti P, et al. Biomed Pharmacother. 2000 Feb;54(1):45‐9. 2.Kalanadhabhatta V, et al. Ann Allergy Asthma Immunol. 1996 Nov;77(5):394‐400. 3.Palusci VJ, et al. Pediatr Infect Dis J. 1996 May;15(5):456‐60. 4. Nguyen MT, Weiss PJ, Wallace MR. AIDS. 1995 Jun;9(6):573‐5. Thank you • Allergy Section • Thanai Pongdee, MD • Arveen Thethi, MD • Special thanks • Miguel Park, MD Evaluation Attended Live Activity on 06.17.14 • Allergy • • • • • • Allergic rhinitis Anaphylaxis Drugs Immunotherapy Foods Stinging insect http://www.surveymonkey.com/s/CURE53 Attended Archived Activity 06.18.14 or later http://www.surveymonkey.com/s/CURE53Archived • Asthma • Allergic and nonallergic • Exercise-induced • Refractory ©2011 MFMER | slide-98 11