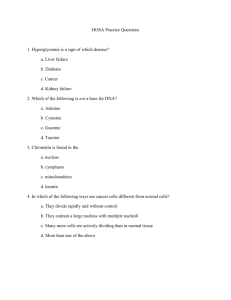
Developmental morphology of human fetal trachea
advertisement

Available online at www.scholarsresearchlibrary.com Scholars Research Library Archives of Applied Science Research, 2014, 6 (4):256-262 (http://scholarsresearchlibrary.com/archive.html) ISSN 0975-508X CODEN (USA) AASRC9 Developmental morphology of human fetal trachea Hemalatha Bangera, Anne D Souza, Mamatha Hosapatna, Antony sylvan D Souza and Vrinda Hari Ankolekar* Department of Anatomy, Kasturba Medical College, Manipal University, Manipal, Karnataka _____________________________________________________________________________________________ ABSTRACT Histologically the trachea is made up of mucosa, submucosa, hyaline cartilage and adventitia. Therefore the study of histogenesis of the fetal trachea provides not only the information on the functional morphology of the organ, but also gives a baseline in the investigations and management of pre and neonatal pathological conditions. The present study was carried out on 15 human fetuses of known gestational age of all trimesters in the department of Anatomy in KMC Manipal. The transverse section of trachea was taken. The sections were stained using Hematoxylin and Eosin and were observed under light microscope. The microscopic anatomy of the trachea was observed at different GA and the changes were observed. At first trimester the trachea was lined by pseudostratified columnar epithelium without any goblet cells. Incomplete rings of hyaline cartilage were also observed .The cellular components of the hyaline cartilage were predominant while the amount of ground substance was comparatively less. Smooth muscle was present at the posterior aspect of the trachea. Few cilia, goblet cells and seromucous glands appeared by 16th week. At third trimester the trachea was lined by pseudostratified ciliated columnar epithelium and goblet cells. Mature ‘C’ shaped hyaline cartilage with well differentiated territorial and interterritorial matrix was observed by 32 weeks. The present study is a preliminary attempt to highlight the histogenesis of trachea at various gestational periods. Keywords: pseudostratified columnar epithelium, trachea, trachialis, hyaline cartilage _____________________________________________________________________________________________ INTRODUCTION The trachea is formed by cartilage and fibromuscular membrane, lined internally by mucosa. The anterolateral portion is made up of incomplete rings of hyaline cartilage and posterolateral aspect by trachealis muscle [1]. Histologically it is made up of mucosa, submucosa, hyaline cartilage and adventitia. The epithelium of trachea is lined by pseudostratified predominantly ciliated with interspersed mucus secreting goblet cells. The lamina propria consists of fine connective tissue fibres and diffuse lymphatic tissue. Seromucous glands are present in the submucosa. Numerous blood vessels are seen in adventitia. The mucosa exhibits folds along the posterior wall of trachea where the cartilage is absent. [2, 3] The lower respiratory system begins its development during the 4th week as an outgrowth of the ventral wall of the foregut (respiratory diverticulum). The endodermal lining of the respiratory diverticulum gives rise to the epithelial lining of the trachea. The cartilaginous and muscular components of the trachea and lungs are derived from the surrounding splanchnic mesoderm. The diverticulum elongates in the caudal direction and soon becomes separated 256 Scholars Research Library Vrinda Hari Ankolekar et al Arch. Appl. Sci. Res., 2014, 6 (4):256-262 ______________________________________________________________________________ from the foregut by the esophagotracheal septum. The ventral portion forms the trachea and lung buds, while the dorsal portion forms the esophagus. [4] Very little information is available on the time of development of the tracheal cartilaginous rings. The morphological study of human fetal tracheal epithelium provides information about a potential respiratory epithelium which has not been exposed to environmental pollutants. [5]. Therefore the study of histogenesis of the fetal trachea provides not only the information on the functional morphology of the organ, but also gives a baseline in the investigations and management of pre and neonatal pathological conditions. MATERIALS AND METHODS The present study was carried out on 15 human fetuses (3 first trimester, 6 second trimester and 6 third trimester) of known gestational age (GA) in the department of Anatomy, Kasturba Medical College, Manipal. The spontaneously aborted and stillborn fetuses were procured from the department of Obstetrics and Gynecology, Kasturba Hospital Manipal for museum specimen preparation. The GA of first trimester fetuses ranged from 10 to 12 weeks whereas it ranged 16 to 24 weeks and 28 to 36 weeks for the second and third trimesters respectively. Fetuses with any external deformity were excluded from the study. The trachea was resected from the level of cricoid cartilage up to the bifurcation. The transverse section was taken at the midpoint between the cricoid and tracheal bifurcation and the tissues were processed for histological observation. The sections were stained using Hematoxylin and Eosin and were observed under light microscope. RESULTS The microscopic anatomy of the trachea was observed at different GA and the changes were observed. The sections were observed both under low and higher magnifications to explain the various functional components. First trimester: (10 to 12 weeks) When observed under 10X, the trachea was lined by pseudostratified columnar epithelium without any goblet cells by 12th week. In the lamina propria connective tissue was observed to have bundles of collagen fibers. There were no glands seen in the lamina propria. The blood vessels were not differentiated. Incomplete rings of hyaline cartilage were also observed. Smooth muscle was present at the posterior aspect of the trachea bridging the gap between the cartilage (Figure 1a). Figure 1: Section of trachea showing trachialis muscle at 16th (Figure 1a) and 32nd (Figure 1b) week of gestation (black arrows). Hematoxylin and Eosin, 40X 257 Scholars Research Library Vrinda Hari Ankolekar et al Arch. Appl. Sci. Res., 2014, 6 (4):256-262 ______________________________________________________________________________ 1- Pseudostratified columnar epithelium 2- Tracheal glands When the epithelium was observed under 40X, there were no cilia on the surface. The cellular components of the hyaline cartilage were predominant while the amount of ground substance was comparatively less. The lacunae and the cell nests were well differentiated (Figure 2). Figure 2: Fetal trachea at 12th week of gestation. Hematoxylin and Eosin, 40X 1- Pseudostratified columnar non ciliated epithelium 2- Lamina propria 3- Hyaline cartilage 4- Adventitia Black arrows show the cell nests in the cartilage. Second trimester: (16 to 24 weeks) When observed under 10X the trachea was lined by pseudostratified columnar epithelium with few cilia and goblet cells by 16th week. In the lamina propriaseromucus glands and blood vessels were observed by 16 weeks. The hyaline cartilage exhibited homogenous matrix and the cell nests were also observed (Figure 3). 258 Scholars Research Library Vrinda Hari Ankolekar et al Arch. Appl. Sci. Res., 2014, 6 (4):256-262 ______________________________________________________________________________ Figure 3: Fetal trachea at 16th week of gestation. Hematoxylin and Eosin, 40X 1- Pseudostratified columnar ciliated epithelium 2- Lamina propria 3- Tracheal glands 4- Hyaline cartilage Blue arrow showing the goblet cell and black arrow showing blood vessels in the lamina propria Third trimester: (28 to 36 weeks) When observed under 10X the trachea was lined by pseudostratified ciliated columnar epithelium and goblet cells. In the Lamina propria, numerous seromucus glands and blood vessels were well defined (Figure 4). 259 Scholars Research Library Vrinda Hari Ankolekar et al Arch. Appl. Sci. Res., 2014, 6 (4):256-262 ______________________________________________________________________________ Figure 4: Fetal trachea at 32 weeks of gestation. Hematoxylin and Eosin, 40X 1234- Pseudostratified columnar ciliated epithelium Lamina propria Tracheal glands Hyaline cartilage Mature ‘C’ shaped hyaline cartilage with well differentiated territorial and interterritorial matrix was observed by 32 weeks. The trachialis muscle was observed posteriorly (Figure 1b). 260 Scholars Research Library Vrinda Hari Ankolekar et al Arch. Appl. Sci. Res., 2014, 6 (4):256-262 ______________________________________________________________________________ The details regarding the appearance of basal membrane, connective tissue components were not able to study as specific stains were not used. As the fetuses were of known GA, the crown rump lengths were not considered. DISCUSSION Harjeet et al studied the development of the human trachea in serial sections of six embryos and fetuses of different crown rump lengths (CR). It was observed that at 11.5 mm CR stage the tracheal tube was lined by pseudostratified columnar epithelium with the basement membrane without any cartilage in the submucosa. At 12.5 mm CR stage the trachea showed a well-marked layer of pseudostratified ciliated columnar epithelium. At 22 mm CR stage tracheal tube was lined by a layer of pseudostratified columnar epithelium in which some cells beared cilia. At 30 mm CR stage the trachea showed incomplete rings in the cartilagenous stage in which chondrocytes are well defined [6]. According to Hamilton et al (1957) the cartilagenous rings in the trachea appear at about 20 mm CR stage and by 50 mm CR stage they are well defined. Tucker and O'Rahilly (1972) studied the development of the human larynx in closely graded emrbyos of one to 23 stages (developmental horizons of Streeter). He described the presence of cartilaginous tracheal rings in 30 mm stage embryos (stage 23) [7]. Grosser (1912) observed that the anlagan of the tracheal cartilagenous rings could be recognised as condensation of 'tissues" in embryos of 17 mm stage and the cartilage develops at 20 mm CR stage embryos [8]. Development of ciliated cells in the fetal human trachea was studied by light and electron microscopy in specimens obtained from 45 embryos or fetuses aged from 9 to 27 weeks of gestation by Gaillard et al. Four stages could be recognized during tracheal development. Up to 11 weeks (stage I), the trachea was covered with a columnar undifferentiated epithelium with abundant glycogen, apical microvilli, and primary cilia. From 12 to 18-19 weeks (stage II), centriologenesis and secondary ciliogenesis were very active, and the percentage of ciliated cells and secretory cells progressively increased. From 20 to 22-23 weeks, the density of ciliated cells was higher but, in parallel, the percentage of secretory cells decreased (stage III). After 24 weeks (stage IV), the ciliated border was apparently mature, the rootlets lengthened, and the cilia were correctly orientated [9]. According to Montgomery et al the tracheal pseudostratified columnar epithelium was found to be composed of four cell types: ciliated in various stages of development, non-ciliated, basal and degenerating cells [10]. In the present study it was observed that the cilia appeared by 16th week and the development of hyaline cartilage was similar to the observations by the previous authors. Merkel (1902) found the presence of muscle fibres in the dorsal wall of the trachea before the appearance of the cartilagenous rings. Tracheal glands are not seen even at 100 mm CR stage [11]. According to Stirling (1982-83) the trachialis muscle has been described in Quain's Anatomy as a muscle which lies between the ends of the cartilages and also in the intervals between them. His study revealed that there are two layers of the muscle: an inner circular and an outer longitudinal the fibres of the inner layer run transversely and get attached to the inner surface of the adjacent ends of a cartilage. He also found that the longitudinal muscle coat was represented by a few strands [12]. Fisher (1962) described three layers of the muscle; transverse, oblique and longitudinal [13]. In the present study the trachialis muscle was observed in the first trimester but the finer details such as the myofibrils and the direction of muscle fibers were not studied in detail. CONCLUSION The present study is a preliminary attempt to highlight the histogenesis of trachea at various gestational periods. REFERENCES [1] Standring S (2008) Gray’s anatomy: the anatomical basis of clinical practice, Pleura, lungs, trachea and bronchi 40th edn. Churchill Livingstone, London. pp 1004-1005 [2] Wheater’s functional histology Barbara Young, James S Lowe, Alans Stevens, John W Heath 5th edition UK pp238-239 [3] Victor P, Eroschenko, Di Fiores Atlas of histology with functional correlations 9th edition 1999 Susan Katz, pp242-243 261 Scholars Research Library Vrinda Hari Ankolekar et al Arch. Appl. Sci. Res., 2014, 6 (4):256-262 ______________________________________________________________________________ [4] TW Sadler TW, Langman’s Medical Embryology 10th edition, USA, pp- 196-197 [5] Mithal A and Emery JL. Thorax. 1976;31:167-171. [6] Harjeet, Sahni D, Jit I. Anat. Soc. India. 2004;53(1): 1-3. [7] Hamilton WJ, Boyd JD, Mossman HW. Human Embryology. Haffer. Cambridge; 1957, pp. 199. [8] Grosser O: Manual of Human Embryology. Vol. 2. Lippincott. Philadelphia; 1912, pp 475 [9] Gaillard DA, Lallement AV, Petit AF, Puchelle ES. Am J Anat. 1989, 185(4):415-28. [10] Montgomery PQ, Stafford ND, Stolinski C. J. Anat. 1990;173:43-59 [11] Merkel F, Atmungsorgane: Bardeleben'sHandbuch der Anatomie des Menschen. 6th Edn; 1902. [12] Stirling W. Journal of Anatomy 1982-83;17: 204-206. [13] Fisher AWF. Journal of Anatomy 1962: 92: 139-140. 262 Scholars Research Library