Application of Platelet-Rich Plasma to Enhance Tissue Repair
advertisement

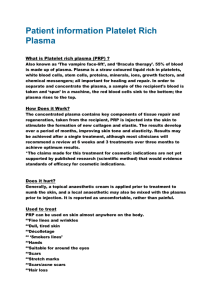
Application of Platelet-Rich Plasma to Enhance Tissue Repair Andrew P. Wroblewski, BS, Hector A. Mejia, MD, and Vonda J. Wright, MD For over 20 years, autologous blood products such as platelet-rich plasma (PRP) have been employed as a means to facilitate the healing process in fields such as orthopedics, dentistry, neurosurgery, cardiothoracic, and maxillofacial surgery. Proponents of this therapy advocate its effectiveness as a safe and natural way to expedite the healing process. Recent investigations of the specific growth factors present in PRP advocate its promise as an emerging therapy at the clinical level. However, there exist few controlled trials to objectively examine the proposed benefits of this therapy. Although some studies demonstrate promising results, the bulk of published data are largely anecdotal and the sample sizes are small. This article reviews the biological mechanisms by which PRP facilitates healing as well as the current clinical research that has investigated PRP therapy as a treatment for musculoskeletal injuries, such as tendonitis, tennis elbow, rotator cuff repair, Achilles tendon repair, muscle injuries, bone injuries, and anterior cruciate ligament repair. The increased prevalence of PRP therapy in treating musculoskeletal injuries warrants a more thorough investigation of its actual benefits if we are to endorse it as an effective therapy. Oper Tech Orthop 20:98-105 © 2010 Published by Elsevier Inc. KEYWORDS autologous blood, growth factors, musculoskeletal injuries, platelet-rich plasma D espite a recent explosion of clinical interest in plateletrich plasma (PRP), the concept of harnessing a patient’s own blood to facilitate healing has existed since the early 1980s.1 PRP contains bioactive elements vital for musculoskeletal tissue healing and has long piqued the interest of orthopedic surgeons as a source of autologous factors for augmenting tissue healing. The clinical use of PRP may enable patients to experience shorter recovery times, faster return to play, stronger tissue healing, and perhaps less pain during recovery. Because of this promise, the clinical use of PRP has outpaced the basic science research needed to document the mechanism of its healing potential. Simply put, “Why does PRP seem to make patients heal faster?” The current answer to this question is still incomplete. Much of the existing published data on PRP are anecdotal, with few laboratory studies documenting the content of the PRP, mechanism of action, or short- and long-term outcomes. Controlled, prospective studies of PRP use in musculoskeletal injuries are necessary to further our understanding Department of Orthopaedic Surgery, University of Pittsburgh, Pittsburgh, PA. Address reprint requests to Vonda J. Wright, MD, Department of Orthopaedic Surgery, University of Pittsburgh, Pittsburgh, PA. E-mail: wrigvj@ upmc.edu 98 1048-6666/10/$-see front matter © 2010 Published by Elsevier Inc. doi:10.1053/j.oto.2009.10.006 of this therapy and evaluate its efficacy. The purpose of this chapter is to describe the known characteristics of PRP, review its application in clinical settings, discuss the best procedures for PRP preparation, and to evaluate its use as an effective therapy in musculoskeletal injuries as a supplemental or stand-alone treatment. PRP Biochemistry Platelets are cytoplasmic fragments of megakaryocytes and play a central role in the complex process of hemostasis. Clot formation and platelet activation are considered the first steps of the healing process.2 Within 10 minutes of blood coagulation, platelets release a burst of proteins from their ␣, ␦, and granules. These organelles contribute the numerous biologically active molecules that provide platelets with their healing properties. The contents of the ␣-granule include many growth and differentiation factors that are released upon platelet activation during injury to the vessel wall.3 The combined effects of these growth factors create an elaborate autocrine and paracrine process, and therefore may result in tissue-specific responses. Within an hour of activation, 95% of the granule’s previously manufactured growth factors will be secreted. The platelets then sustain production of addi- Application of PRP for enhancing tissue repair tional growth factors over the next several days.4 For the platelets to release this cascade of molecules that contribute to tissue healing, they must first be activated. Conventionally, bovine thrombin and calcium have been used for platelet activation. Once activated, the resulting PRP mixture must be injected immediately, as the subsequent secretion of the granule contents occurs rapidly. However, the addition of thrombin and calcium to the platelet mixture produces a gel that cannot be injected even using a largegauge needle, thus limiting its use in certain surgical procedures. The application of soluble type-I collagen has been evaluated as an alternative to thrombin and calcium in platelet activation. Activation via type-I collagen produces a less rapid release of the granule contents, which enable a delayed administration of PRP. When compared with thrombin activation, the collagen-activated platelets produced equal concentrations of particular growth factors with less clot retraction. The collagen activation technique also permits in vivo activation that can be administered through a small-gauge needle. These results suggest that type-I collagen may be an effective method for platelet activation.5 Current Applications of PRP Each year, numerous recreational and competitive-level athletes sustain an array of musculoskeletal injuries, which sideline them for significant portions of their season. In the United States, these injuries account for over 100 million office visits each year. The ebullience of orthopedic surgeons over the emergence of PRP as a promising new therapy is due to its preliminary success in treating tendon, muscle, and bone injuries. Proponents of PRP believe that it will not only expedite the healing process but improve the quality of the damaged tissue as well. The high concentration of growth factors and cytokines in PRP hint at its promise as a standalone or supplemental treatment for these types of injuries.6 A few of the musculoskeletal injuries that have demonstrated positive responses to PRP therapy are discussed later in the text. Tendonitis Tendinopathy, or injuries to the tendon, range from acute or chronic tendonitis to a full-thickness tear. Tendon degeneration has many determinants. The combination of intrinsic elements, such as age-related decline, and extrinsic elements, such as acute physical trauma, demonstrate a role as a contributing factor in tendon injury.7 Exposure to fluoroquinolone antibiotics, genetic factors, matrix metalloproteases, and apoptosis all contribute to tendon injuries.8,9 Tendon healing is a dynamic process that occurs in 3 overlapping phases: inflammation, proliferation, and remodeling. These phases are mediated by many growth factors that are believed to act in a series of inter-related signaling pathways.10 In animal models, growth factor expression exhibits a substantial role in supraspinatus tendon-to-bone healing.11 The concentration of these cytokines is exaggerated in PRP. This increased concentration is a proposed explanation for 99 the effectiveness of PRP as a viable treatment option for tendon injuries. In vitro, PRP shows promotion of stromal and mesenchymal stem cell proliferation.12 Other studies demonstrate PRP to reduce macrophage proliferation and interleukin (IL) production within the first 72 hours after exposure.13,14 The ability of PRP to elicit diverse responses from cells indicates that it may halt excess inflammation while activating proliferation and maturation. This would inhibit the fibrous scar tissue healing that accompanies macrophageregulated tendon-to-bone healing.6,15 Tennis Elbow Chronic elbow epicondylar tendonitis, commonly referred to as tennis elbow, is often resolved with nonoperative treatment protocols. PRP therapy is currently under investigation as one of these protocols that would serve as an alternative to surgical intervention. In a recent study, patients whose symptoms had not resolved after nonoperative treatment protocol and were considering surgery were subjected to an injection of either buffered PRP or bupivacaine (the control). Patients who received the PRP treatment demonstrated a 60% improvement in their visual analog pain scores 8 weeks after the procedure, while the control group exhibited a 16% improvement. Continued evaluation showed that the PRP group exhibited an 81% improvement at 6 months post treatment and a 93% improvement at the final follow-up, 25.6 months post treatment. These results could not be compared with the control group because 60% of the control subjects either withdrew or sought other treatments after week 8.16 To endorse PRP injection as an effective alternative to surgical intervention in tennis elbow injuries, controlled, prospective studies with a large sample size are necessary to evaluate its long-term effectiveness. Rotator Cuff Repair The use of PRP as a supplemental therapy in the arthroscopic repair of a torn rotator cuff tendon may further increase the patient’s rate of recovery. A pilot study subjected 14 patients undergoing arthroscopic repair of rotator cuff tears to intraoperative application of autologous PRP with an autologous thrombin component. The subjects were followed for 24 months postsurgery and evaluated using a pain score (visual analog scale) and a functional score (UCLA and Constant scores). All patients recovered passive range of motion within 1 month of treatment. Patients demonstrated a significant decrease in their outcome measured pain scores at 6, 12, and 24 months. No significant differences between the preoperative and the 1-month postoperative pain scores were witnessed. The UCLA functional scoring increased from a preoperative level of 16.54-32.92 at the final follow-up. There were no reported complications related to the procedure.17 These results exhibit the application of autologous PRP to be a safe and stable procedure with no long-term adverse affects. Although the patients demonstrated marked improvement after surgery, the small sample size and lack of a control A.P. Wroblewski, H.A. Mejia, and V.J. Wright 100 group make it difficult to ascertain the benefits of this technique compared with surgery as the sole treatment. In another study, platelet-leukocyte–rich plasma was prepared from a whole unit of blood and used to produce platelet-leukocyte gel (PLG). The gel is similar to PRP in that it exhibits concentrations of platelets and leukocytes well above baseline levels. PLG was applied to patients undergoing open subacromial decompression to investigate its role in postoperative recovery. Compared with controls, the PLG group evidenced decreased pain scores, took less pain medication, and demonstrated an improved range of motion in the recovery process. The results of this study indicate that PLG is an effective agent in the return to full function after shoulder surgery.18 Achilles Tendon Repair In a retrospective study of Achilles tendon repairs, athletes treated with surgery and PRP therapy recovered range of motion earlier than the control groups, which received surgery alone. The PRP group also demonstrated no wound complications and returned to training activities faster than the controls. In addition, this study investigated the quality of the repaired tendon by measuring the cross-sectional area of the tendon using ultrasound. This is an aspect of the healing process that is often overlooked when investigating the effectiveness of PRP therapies. The ultrasounds of the PRP group showed tendons with a smaller cross-sectional area than those of the control group.19 In animal models, the use of PRP in Achilles tendon repairs displayed a greater maturation in tendon callus. Mechanical stimulation of the repaired tendons revealed an increased force to failure and ultimate stress in those treated with PRP. This increase is believed to be attributed to the benefits of PRP during the early phases of the healing process, which allows mechanical stimulation to proceed at an earlier time, driving the growth of new tendon at a faster rate than the control groups.20,21 Muscle Injuries Muscle injuries in sports may result from a blow, strain, or sometimes a laceration. They are most prevalent in sports that include physical contact, sprinting, or jumping. They usually occur after an eccentric contraction, resulting in an injury at the musculotendinous junction.22 Similar to tendon healing, muscle healing occurs in an arrangement of overlapping steps. The sequence of these steps is inflammation, proliferation, and remodeling, and they are regulated by growth factors and cell-to-cell interactions. Local vascularity and regeneration of intramuscular nerve branches are integral to the muscle healing process. PRP therapy has been shown to enhance both of these processes.23,24 Ultimately, the rate of recovery for any patient will be dependent on their own biology as well as the prescribed treatments. Standard procedure for treatment of these types of injuries follows the RICE acronym (Rest Ice Compression Elevation) and a gradual return to resistance exercise. Nonsteroidal anti-inflammatory drugs are typically used to alleviate pain as part of the recovery process. However, recent research suggests that they may obstruct the healing properties of the muscle tissue by inhibiting the fusion of the myogenic precursor cells.25 The importance of growth factors to the muscle healing process is evident through the large concentrations of cytokines found in healing tissue. Particular growth factors can enhance not only muscle regeneration after injury but muscle force as well.26 The inflammatory phase of muscle healing is governed by growth factors, macrophages, and products of the cyclooxygenase-2 pathway. Investigations of the interaction between transforming growth factor (TGF)  and prostaglandin E2 molecules suggest a negative feedback loop that controls the level of fibrosis formed during the healing process.27 A group of elite athletes subjected to a form of PRP therapy that uses ultrasound-guided injection displayed an expedited functional restoration by returning to full function in half of the expected time. They also lacked any evidence of excessive fibrosis. This treatment requires further investigation to validate its use in treating muscle injuries.6 Bone Overall, success of PRP as a clinical treatment after orthopedic trauma is debatable. Most studies evaluating its use in bone repair are in oral and craniofacial surgery. A clinical study exploring the application of autologous fibrin to cancellous bone during mandibular reconstruction evidenced radiographic consolidation in half the time of the control group. The accelerated consolidation witnessed was attributed to enhanced osteoconduction of the osteocomponent cells in the graft by the fibrin network, which formed from the concentration of platelets.28 As a result, dentists have developed a procedure where platelet-rich material is combined with autograft, allograft, demineralized bone matrix, and other materials to fill blemishes in the mandible and cranium.29 In cases where PRP has been used in spinal fusion it has exhibited positive results, with all patients obtaining union.30 In another study, callus formation was witnessed between 34 and 47 days in 3 patients during osteogenesis distraction when treated with a mixture of PRP and bone marrow cells. The role of PRP in the increased distraction and speedy bone formation is inconclusive, as it was used in combination with another osteoconductive substance.31 In a study that investigated the use of PRP in treating fractures of the foot and ankle, the concentration of plateletderived growth factor (PDGF) and TGF in the hematoma of 24 patients was measured. Seven of these fractures had failed to unite. They demonstrated no trace of PDGF and TGF proteins upon examination. Revision operations were performed and PRP was applied to the nonunions. Those subjected to this treatment exhibited radiographic union at an average of 8.5 weeks.32 Anterior Cruciate Ligament Although PRP is hypothesized to be an effective treatment for improving the biomechanics of anterior cruciate ligament (ACL) repair, recent studies of animal models have demonstrated conflicting results. Bilateral suture repair of ACL in pigs, with one side receiving suture repair, and the other side Application of PRP for enhancing tissue repair receiving suture repair and PRP application, yielded imperfect results. No significant differences in anteroposterior knee laxity at 30° and 60°, maximum tensile load, or linear stiffness were discovered at 14 weeks after suture repair.33 Studies of ACL grafts enhanced by collagen-platelet composite in goats exhibited similar findings. In the group that received ACL reconstruction alone, the average increase in anteroposterior knee laxity at 30° was 40% greater than the collagenplatelet-composite–treated group. At 60°, the average increase was 30%, favoring the control group. In regard to structural differences, no significant changes were witnessed.34 These findings emphasize the need for further research on the perceived benefits of PRP at the clinical level. Biological Properties of PRP Basic science research is essential to elucidate the proposed benefits of this therapy at the molecular level. Currently, much of its promise is attributed to the intrinsic properties of its growth factors. It is important to note that growth factors are not the only elements present in significant concentrations in PRP, as proteins of the cytokine and chemokine families are known to be present in varying concentrations as well. The elements identified in PRP include TGF, vascular endothelial growth factor (VEGF), platelet-derived endothelial growth factor, epidermal growth factor, insulin-like growth factor, platelet factor 4, IL-1, platelet-derived angiogenesis factor, epithelial cell growth factor, osteocalcin, osteonectin, thrombospondin-1, fibrinogen, fibronectin, and vitronectin. The concentrations of these various growth factors increase linearly as platelet concentration increases.3,35 The network of activated growth factors induces intracellular signaling pathways that lead to the production of proteins essential to the regenerative processes, such as cell proliferation, matrix formation, osteoid production, and collagen synthesis.36 Cell types that are involved in the healing process, such as osteoblasts, fibroblasts, epithelial cells, endothelial cells, and adult mesenchymal stem cells reveal the presence of membrane receptors that are specific for certain growth factors. Furthermore, when cytokines are released they bind to the transmembrane receptors on the surface of local or circulating cells. This supports the proposed role of growth factors as integral components in activating soft-tissue healing and bone regeneration.2,37 Simply put, at the time of injury, the platelets arrive via the capillaries and are activated, releasing their granule contents into the wound site. This influx of growth factors and proteins play an active role in synthesizing the necessary components for the regenerative process and may also play a paracrine role by recruiting other cells to the wound site. PDGF is a multiple mitogen that has been found in macrophages, endothelial cells, monocytes, fibroblasts, bone matrix, and ␣-granules of the platelets. The principal activities of PDGF include angiogenesis, macrophage activation, proliferative activity on fibroblasts, and chemotaxis for fibroblasts and collagen synthesis.38-40 It is recognized as a factor in bone metabolism by enhancing osteoblast replication and bone collagen degradation.41 PDGF is present in 3 isoforms: ␣␣, 101 , and ␣. Although the reason for these 3 isoforms is unclear, differential binding by various receptor cells is a proposed solution.42 This would imply that PDGF exhibits a dual nature, acting as both a stimulator and suppressor of osseous and soft-tissue repair.43 TGF is a bone morphogenetic protein.44 Studies of TGF reveal its role in simulating matrix production by bone cells and possibly its influence on the nature of the matrix.45 It is a key factor in the promotion of the proliferative activity of fibroblasts, as well as the synthesis of type-I collagen and fibronectin. TGF can promote differentiation or proliferation of osteoblast cell types while suppressing the development of osteoclast precursors. These findings suggest that while a player in both processes, TGF favors bone formation over bone resorption.39,46,47 Three isoforms of TGB are identified: 1, 2, and 3.48 Insulin-like growth factor-1 plays a role in the metabolism of numerous cell types. It is chemotactic for fibroblasts and enhances the synthesis of proteins.49 By stimulating the proliferation and differentiation of osteoblasts, it is able to promote bone formation.50,51 Platelet-derived endothelial growth factor enhances epidermal regeneration. It promotes the proliferation of keratinocytes and dermal fibroblasts to activate wound healing. Its presence augments the concentration and effects of other growth factors.52 Platelet factor 4 is released from the ␣-granules of platelets and is proposed to play a partial role in the influx of neutrophils into the wound site. It operates as a chemoattractant for fibroblasts and mediates the effects of heparin-like molecules to increase blood clotting.53,54 VEGF is a signaling protein that is a member of the cytosine-knot growth factor family. Its role in vasculogenesis and angiogenesis showcase its importance to the healing process.55 VEGF increases microvascular permeability and acts as a vasodilator, processes imperative to tissue healing. In vitro studies demonstrate the stimulation of cell migration and mitogenesis in endothelial cells by VEGF.53,55 Epidermal growth factor binds to a corresponding cell surface receptor with high affinity. This stimulates the expression of genes that induce DNA synthesis and cell proliferation.56 A summary of these growth factors, their role in the healing process, and their relative concentration in a sample of PRP are presented in Table 1. The Role of Dense Granules Although the ␣-granules are commonly recognized as the major contributors to the cascade of bioactive elements released from the platelets, it is important not to overlook the effects of the dense granules. The dense granules of platelets contain adenosine, serotonin, histamine, and calcium, the combination of which exhibit effects on the different stages of tissue repair. Adenosine is a nucleoside that is involved in many cellular processes. It acts as a primary cytoprotective agent that represses tissue damage. In the inflammatory process that accompanies A.P. Wroblewski, H.A. Mejia, and V.J. Wright 102 Table 1 Effect of the Growth Factors Produced by Platelets, and Their Average Concentrations in Platelet-Rich Plasma (PRP) Growth Factor PDGF TGF IGF-I PDEGF PDAF PF-4 EGF VEGF PRP Concentration (SD) Effect Macrophage activation and angiogenesis Fibroblast chemotaxis and proliferative activity Enhances collagen synthesis Enhances the proliferation of bone cells Enhances the proliferative activity of fibroblasts Stimulates biosynthesis of type I collagen and fibronectin Induces deposition of bone matrix Inhibits osteoclast formation and bone resorption Chemotactic for fibroblasts and stimulates protein synthesis Enhances bone formation by proliferation and differentiation of osteoblasts Promotes wound healing by stimulating the proliferation of keratinocytes and dermal fibroblasts Induces vascularization by stimulating vascular endothelial cells Stimulates the initial influx of neutrophils into wounds A chemoattractant for fibroblasts A potent antiheparin agent Cellular proliferation Differentiation of epithelial cells Angiogenesis Migration and mitosis of endothelial cells Creation of blood vessel lumen Creates fenestrations Chemotactic for macrophages and granulocytes Vasodilation (indirectly by release of nitrous oxide) ␣ 117.5 ng/mL (63.4)  9.9 ng/mL (7.5) 1: 169.9 ng/mL (84.5) 2: 0.4 ng/mL (0.3) 84.2 ng/mL (23.6) 470 pg/mL (320) 0.189 nmol/mL (0.07) 51 pmol/L (5) 76-854 pg/mL Abbreviations: PDGF, platelet-derived growth factor; TGF, transforming growth factor; IGF, insulin-like growth factor; PDEGF, plateletderived endothelial growth factor; PDAF, platelet-derived angiogenesis factor; PF-4, platelet factor 4; EGF, endothelial growth factor; VEGF, vascular endothelial growth factor. Reprinted with permission.57 diabetic nephropathy, the activation of the adenosine receptor demonstrates an anti-inflammatory response.58 Laboratory studies show the topical application of adenosine A2A receptor agonists to diabetic foot wounds to yield more rapid wound closure by amplifying the salutary functions of inflammatory cells, endothelial cells and fibroblasts.59 Adenosine can upregulate IL-10 production by immunostimulated macrophages.60 In addition, macrophage activation by adenosine yields proinflammatory cytokines, IL-1, and IL-18.61 Serotonin is a monoamine neurotransmitter and displays many observed effects relative to inflammation and healing.6 Its effect in augmenting capillary permeability is proposed to exceed those of histamine.62 It increases fibroblast proliferation, and macrophage cells have receptors sensitive to the hormone. Studies of the effects of this hormone on macrophage function advocate its position as a mediator at sites of inflammation by suppressing interferon-␥–induced 1a expression. Serotonin’s suppression of this expression is concentration-dependent and is much more potent than the related compounds dopamine, histamine, and tryptamine.63 Histamine is a biogenic amine that is used during the local immune response and is a strong activator of macrophages. It is released at the time of injury and acts as a vasodilator. In addition, it augments the permeability of the microvascular system of capillaries and venules through the contraction of the epithelial cells and the expulsion of the fenestrated diaphragms blocking gaps in the epithelial lining.64 This increase in permeability is imperative to the tissue healing pro- cess because it affords inflammatory and immune cells more access to the site of injury.53 Calcium functions as a key component in tissue repair through keratinocyte proliferation and differentiation. Calcium is necessary for skin fibroblasts, although keratinocytes are not as responsive to its effects. In the bone remodeling phase, calcium could be a necessary component for epidermal cell migration and regeneration. Overall, calcium plays a critical role in wound management, and is proposed to demonstrate a crucial role when delivered to the wound site by the dense granules.65 Methods of PRP Preparation PRP is defined as a volume of the plasma fraction of autologous blood with a platelet concentration above baseline.29 Plasma with a platelet concentration of approximately 1,407,640 L, or 5 times greater than the platelet count in normal blood, is the suggested working concentration for PRP therapy. The relative ease of PRP preparation has led to a variety of available commercial systems, each of which operate through different techniques and yield varying platelet concentrations. In implant dentistry, a field where PRP use is becoming increasingly common, 4 commercial systems are commonly used for the preparation of PRP in clinical settings. These include SMart-PReP autologous platelet-concentrate system (Harvest Technologies Corporation, Plymouth, MA), Platelet Concentrate Collection System (3i Implant In- Application of PRP for enhancing tissue repair novations, Palm Beach Gardens, FL), Curasan PRP Kit (Curasan, Pharma, GmbH AG, Lindigstrab, Germany), and Ace Platelet Concentration System (Ace Surgical Supply Company, Brockton, MA). Although these 4 systems are currently the most used systems, various other commercial systems are available for use.66 The Arthrex Autologous Conditioned Plasma Double Syringe System is specifically designed to extract PRP for a patient’s peripheral blood while eliminating the need for a second centrifugation step. The 3 techniques commonly used to prepare PRP through these systems are the gravitational platelet sequestration (GPS), the standard cell separator technique, and autologous selective filtration technology (plateletpheresis). Factors such as force and duration of centrifugation must be considered to ensure the reproducibility of a particular method, as they may lead to differences in the obtained platelet concentration. It is suggested that studies that display conflicting evidence of the proposed benefits of PRP may be the result of an insufficient platelet concentration.37 GPS is the most common and effective technique used in PRP preparation. It uses a centrifuge system to separate anticoagulated blood into distinct layers: the plasma, the buffy coat, and the red blood cells. The volume of PRP that results from the GPS technique is approximately 10% of the total volume of whole blood drawn. A 12-minute spin at a speed of 3200 rpm with a flat-bottomed, 60 mL plastic centrifuge tube produces a PRP volume of approximately 5 mL.53 In dentistry, the ACE Double-Centrifugation System has been compared to the Nahita single-centrifugation system to elucidate the differences in the obtained PRP. Analysis of the platelet concentration yields of the 2 methods revealed 336% for the double-centrifugation system and 227% for the single-centrifugation system. Although the double-centrifugation system produces higher platelet concentrations, the range of values achieved is much higher. Ultrastructural analysis of the 2 samples by transmission electron microscopy reveals changes in PRP structure for the double-centrifugation method. This method was also more susceptible to slight errors during the preparation process.67 Standard cell separators typically operate on a full unit of blood, usually through a continuous-flow centrifuge bowl or a continuous-flow disk separation technique and use both fast and slow spins.68 This will generally yield platelet concentrations 2-4 times higher than baseline levels.69 There exists a discontinuous technique that can produce a platelet count 5 times greater than baseline, while returning the red blood cells and some of the plasma to the patient to maintain the volume of the circulating blood.70,71 Compact office systems exist, which can yield approximately 6 mL of PRP from a starting blood volume of 45-60 mL. A blood sample this small would eliminate the need for reinfusion.72,73 However, a disadvantage of this technique is that it differs widely in the concentration of the available platelets accumulated, ranging from 30% to 85%, or 2 to 8 times baseline.68,73 Plateletpheresis uses a disposable proprietary filter to capture the platelets from whole blood. The captured platelets are collected to produce PRP. This method does not require a centrifuge. It produces a blood fraction with platelet and 103 growth factor concentrations similar to those of the centrifuge methods.74 Discussion Numerous athletes across all levels of competitiveness are sidelined by musculoskeletal injuries each year. Advancements in medicine demand less invasive therapies and faster recovery times for athletes suffering from these injuries. To continue to offer these patients the best treatments available, we must investigate all leads in search of promising new therapies. Currently, the major avenues being explored are stem cells, gene therapy, and autologous or bioengineered cytokines. However, these therapies are not yet ready for widespread clinical use. Because PRP is prepared from the patient’s own blood, the risk of experiencing complications is minimal. Preparation of PRP is quick, simple, and relatively inexpensive. In addition, it can work with a range of different cell types. All these factors exhibit PRP’s potential as an ideal biological therapy. More thorough clinical investigation of PRP is necessary in controlled, prospective, randomized studies to determine its effectiveness in treating musculoskeletal injuries. Types of injuries where PRP has shown the most promise are tears of the Achilles, patellar, quadriceps, or rotator cuff tendons. Another area requiring further investigation is the effect of PRP on different locations within a tissue. For example, tissues, such as tendon comprise 3 overlapping zones: the myotendinous junction, the midsubstance, and the osseotendinous junction.6 Each of these zones may exhibit different effects when exposed to PRP. Such differential effects can be studied individually using ultrasound-guided injections of PRP. The dosage and type of PRP may also contribute to the effectiveness of the treatment. It is suggested that studies that failed to demonstrate the benefits of PRP therapy may have used an insufficient dose or concentration of PRP. Rehabilitation procedures specific to PRP therapy should be designed to facilitate the patient’s recovery proceeding injection to maximize the effectiveness of this treatment. For example, the benefits of PRP may be augmented if the patient performs a series of gentle exercises to load the tendon before injection. This would contrast traditional rehabilitation methods after surgical treatments, but could display positive results. In summary, PRP may be a promising treatment option for musculoskeletal injuries. Preliminary research has expanded our knowledge of PRP at the molecular level, although its effectiveness as a clinical therapy is not yet proven. Prospective randomized trials are necessary to determine the efficacy of PRP therapy in all musculoskeletal injuries. The results of these studies will outline future use of this therapy as a viable treatment option. References 1. Knighton DR, Hunt TK, Thakral KK, et al: Role of platelets and fibrin in the healing sequence: An in vivo study of angiogenesis and collagen synthesis. Ann Surg 196:379-388, 1982 2. Anitua E, Andia I, Ardanza B, et al: Autologous platelets as a source of A.P. Wroblewski, H.A. Mejia, and V.J. Wright 104 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. proteins for healing and tissue regeneration. Thromb Haemost 91:4-15, 2004 Marx RE: Platelet-rich plasma (PRP): What is PRP and what is not PRP? Implant Dent 10:225-228, 2001 Marx RE: Platelet-rich plasma: Evidence to support its use. J Oral Maxillofac Surg 62:489-496, 2004 Fufa D, Shealy B, Jacobson M, et al: Activation of platelet-rich plasma using soluble type I collagen. J Oral Maxillofac Surg 66:684-690, 2008 Mishra A, Woodall J Jr, Vieira A: Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med 28:113-125, 2009 Nho SJ, Yadav H, Shindle MK, et al: Rotator cuff degeneration: Etiology and pathogenesis. Am J Sports Med 36:987-993, 2008 Khaliq Y, Zhanel GG: Fluoroquinolone-associated tendinopathy: A critical review of the literature. Clin Infect Dis 36:1404-1410, 2003 Xu Y, Murrell GA: The basic science of tendinopathy. Clin Orthop Relat Res 466:1528-1538, 2008 Sharma P, Maffulli N: Tendon injury and tendinopathy: Healing and repair. J Bone Joint Surg Am 87:187-202, 2005 Wurgler-Hauri CC, Dourte LM, Baradet TC, et al: Temporal expression of 8 growth factors in tendon-to-bone healing in a rat supraspinatus model. J Shoulder Elbow Surg 16:S198-S203, 2007 (suppl 5) Lucarelli E, Beccheroni A, Donati D, et al: Platelet-derived growth factors enhance proliferation of human stromal stem cells. Biomaterials 24:3095-3100, 2003 Woodall J Jr, Tucci M, Mishra A, et al: Cellular effects of platelet rich plasma: A study on HL-60 macrophage-like cells. Biomed Sci Instrum 43:266-271, 2007 Woodall J Jr, Tucci M, Mishra A, et al: Cellular effects of platelet rich plasmainterleukin1 release from prp treated macrophages. Biomed Sci Instrum 44:489-494, 2008 Kawamura S, Ying L, Kim HJ, et al: Macrophages accumulate in the early phase of tendon-bone healing. J Orthop Res 23:1425-1432, 2005 Mishra A, Pavelko T: Treatment of chronic elbow tendinosis with buffered platelet-rich plasma. Am J Sports Med 34:1774-1778, 2006 Randelli PS, Arrigoni P, Cabitza P, et al: Autologous platelet rich plasma for arthroscopic rotator cuff repair. A pilot study. Disabil Rehabil 30: 1584-1589, 2008 Everts PA, Devilee RJ, Brown Mahoney C, et al: Exogenous application of platelet-leukocyte gel during open subacromial decompression contributes to improved patient outcome. A prospective randomized double-blind study. Eur Surg Res 40:203-210, 2008 Anitua E, Sanchez M, Nurden AT, et al: Reciprocal actions of plateletsecreted TGF-beta1 on the production of VEGF and HGF by human tendon cells. Plast Reconstr Surg 119:950-959, 2007 Aspenberg P, Virchenko O: Platelet concentrate injection improves Achilles tendon repair in rats. Acta Orthop Scand 75:93-99, 2004 Virchenko, O, Aspenberg P: How can one platelet injection after tendon injury lead to a stronger tendon after 4 weeks? Interplay between early regeneration and mechanical stimulation. Acta Orthopade 77: 806-812, 2006 Jarvinen TA, Jarvinen TL, Kaariainen M, et al: Muscle injuries: Biology and treatment. Am J Sports Med 33:745-764, 2005 Yokota K, Ishida O, Sunagawa T, et al: Platelet-rich plasma accelerated surgical angio-genesis in vascular-implanted necrotic bone: An experimental study in rabbits. Acta Orthop 79:106-110, 2008 Sariguney Y, Yavuzer R, Elmas C, et al: Effect of platelet-rich plasma on peripheral nerve regeneration. J Reconstr Microsurg 24:159-167, 2008 Shen W, Prisk V, Li Y, et al: Inhibited skeletal muscle healing in cyclooxygenase-2 gene-deficient mice: The role of PGE2 and PGF2alpha. J Appl Physiol 101:1215-1221, 2006 Kasemkijwattana C, Menetrey J, Bosch P, et al: Use of growth factors to improve muscle healing after strain injury. Clin Orthop Relat Res 370: 272-285, 2000 Shen W, Li Y, Zhu J, et al: Interaction between macrophages, TGFbeta1, and the COX-2 pathway during the inflammatory phase of skeletal muscle healing after injury. J Cell Physiol 214:405-412, 2008 Tayapongsak P, O’Brien DA, Monteiro CB, et al: Autologous fibrin adhesive in mandibular reconstruction with particulate cancellous 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. bone and marrow. J Oral Maxillofac Surg 52:161-165, 1994; discussion 166 Marx RE, Carlson ER, Eichstaedt RM, et al: Platelet-rich plasma: Growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 85:638-646, 1998 Lowery GL, Kulkarni S, Pennisi AE: Use of autologous growth factors in lumbar spinal fusion. Bone 25:47S-50S, 1999 (suppl 2) Kitoh H, Kitakoji T, Tsuchiya H, et al: Distraction osteogenesis of the lower extremity in patients with achondroplasia/hypochondroplasia treated with transplantation of culture-expanded bone marrow cells and platelet-rich plasma. J Pediatr Orthop 27:629-634, 2007 Gandhi A, Bibbo C, Pinzur M, et al. : The role of platelet-rich plasma in foot and ankle surgery. Foot Ankle Clin 10:621-637:viii, 2005 Murray MM, Palmer M, Abreu E, et al: Platelet-rich plasma alone is not sufficient to enhance suture repair of the ACL in skeletally immature animals: An in vivo study. J Orthop Res 27:639-645, 2009 Spindler KP, Murray MM, Carey JL, et al: The use of platelets to affect functional healing of an anterior cruciate ligament (ACL) autograft in a caprine ACL reconstruction model. J Orthop Res 27:631-638, 2009 Eppley BL, Woodell JE, Higgins J: Platelet quantification and growth factor analysis from platelet-rich plasma: Implications for wound healing. Plast Reconstr Surg 114:1502-1508, 2004 Schilephake H: Bone growth factors in maxillofacial skeletal reconstruction. Int J Oral Maxillofac Surg 31:469-484, 2002 Whitman DH, Berry RL, Green DM: Platelet gel: An autologous alternative to fibrin glue with applications in oral and maxillofacial surgery. J Oral Maxillofac Surg 55:1294-1299, 1997 Raines EW, Ross R: Platelet-derived growth factor. I. High yield purification and evidence for multiple forms. J Biol Chem 257:5154-5160, 1982 Oates TW, Rouse CA, Cochran DL: Mitogenic effects of growth factors on human periodontal ligament cells in vitro. J Periodontol 64:142148, 1993 Matsuda N, Lin WL, Kumar NM, et al: Mitogenic, chemotactic, and synthetic responses of rat periodontal ligament fibroblastic cells to polypeptide growth factors in vitro. J Periodontol 63:515-525, 1992 Yang D, Chen J, Jing Z, et al: Platelet-derived growth factor (PDGF)-AA: A self-imposed cytokine in the proliferation of human fetal osteoblasts. Cytokines 12:1271-1274, 2000 Hauschka PV, Mavrakos AE, Iafrati MD, et al: Growth factors in bone matrix. Isolation of multiple types by affinity chromatography on heparin-Sepharose. J Biol Chem 261:12665-12674, 1986 Bucholz R, Einhorn TA, Marsh JL: Bone and joint healing, in Bucholz R, Heckman JD, Court-Brown C (eds): Bone Fractures in Adults. Lippincott Williams & Wilkins, 2006, pp 300-311 Celeste AJ, Iannazzi JA, Taylor RC, et al: Identification of transforming growth factor beta family members present in bone-inductive protein purified from bovine bone. Proc Natl Acad Sci USA 87:9843-9847, 1990 Wrana JL, Maeno M, Hawrylyshyn B, et al: Differential effects of transforming growth factor-beta on the synthesis of extracellular matrix proteins by normal fetal rat calvarial bone cell populations. J Cell Biol 106:915-924, 1988 Bonewald LF, Mundy GR: Role of transforming growth factor-beta in bone remodeling. Clin Orthop Relat Res 250:261-276, 1990 Mohan S, Baylink DJ: Bone growth factors. Clin Orthop Relat Res 263:30-48, 1991 Ten Dijke P, Hansen P, Iwata KK, et al: Identification of another member of the transforming growth factor type beta gene family. Proc Natl Acad Sci USA 85:4715-4719, 1988 Hock JM, Centrella M, Canalis E: Insulin-like growth factor I has independent effects on bone matrix formation and cell replication. Endocrinology 122:254-260, 1988 McCarthy TL, Centrella M, Canalis E: Further biochemical and molecular characterization of primary rat parietal bone cell cultures. J Bone Miner Res 3:401-408, 1988 Joseph BK, Savage NW, Daley TJ, et al: In situ hybridization evidence for a paracrine/autocrine role for insulin-like growth factor-I in tooth development. Growth Factors 13:11-17, 1996 Application of PRP for enhancing tissue repair 52. Einhorn TA: The science of fracture healing. J Orthop Trauma 19:S4S6, 2005 (suppl 10) 53. Alsousou J, Thompson M, Hulley P, et al: The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br 91:987-996, 2009 54. Maurer AM, Zhou B, Han ZC: Roles of platelet factor 4 in hematopoiesis and angiogenesis. Growth Factors 24:242-252, 2006 55. Ferrara N, Gerber HP: The role of vascular endothelial growth factor in angiogenesis. Acta Haematol 106:148-156, 2001 56. Herbst RS: Review of epidermal growth factor receptor biology. Int J Radiat Oncol Biol Phys 59:21-26, 2004 (suppl 2) 57. Alsousou J, Thompson M, Hulley P, et al: The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: A review of the literature. J Bone Joint Surg Br 91:987-996, 2009 58. Awad AS, Huang L, Ye H, et al: Adenosine A2A receptor activation attenuates inflammation and injury in diabetic nephropathy. Am J Physiol Renal Physiol 290:F828-F837, 2006 59. Cronstein BM: Adenosine receptors and wound healing, revised. ScientificWorldJournal 6:984-991, 2006 60. Nemeth ZH, Lutz CS, Csoka B, et al: Adenosine augments IL-10 production by macrophages through an A2B receptor-mediated posttranscriptional mechanism. J Immunol 175:8260-8270, 2005 61. Cruz CM, Rinna A, Forman HJ, et al: ATP activates a reactive oxygen species-dependent oxidative stress response and secretion of proinflammatory cytokines in macrophages. J Biol Chem 282:2871-2879, 2007 62. Parratt JR, West GB: Release of 5-hydroxytryptamine and histamine from tissues of the rat. J Physiol 137:179-192, 1957 63. Sternberg EM, Trial J, Parker CW: Effect of serotonin on murine macrophages: Suppression of Ia expression by serotonin and its reversal by 5-HT2 serotonergic receptor antagonists. J Immunol 137:276-282, 1986 105 64. Majno G, Gilmore V, Leventhal M: On the mechanism of vascular leakage caused by histaminetype mediators. A microscopic study in vivo. Circ Res 21:833-847, 1967 65. Lansdown AB: Calcium: A potential central regulator in wound healing in the skin. Wound Repair Regen 10:271-285, 2002 66. Rutkowski JL, Thomas JM, Bering CL, et al: Analysis of a rapid, simple, and inexpensive technique used to obtain platelet-rich plasma for use in clinical practice. J Oral Implantol 34:25-33, 2008 67. Tamimi FM, Montalvo S, Tresguerres I, et al: A comparative study of 2 methods for obtaining platelet-rich plasma. J Oral Maxillofac Surg 65: 1084-1093, 2007 68. Kevy SV, Jacobson MS: Comparison of methods for point of care preparation of autologous platelet gel. J Extra Corpor Technol 36:28-35, 2004 69. Choi BH, Zhu SJ, Kim BY, et al: Effect of platelet-rich plasma (PRP) concentration on the viability and proliferation of alveolar bone cells: An in vitro study. Int J Oral Maxillofac Surg 34:420-424, 2005 70. Weibrich G, Kleis WK: Curasan PRP kit vs. PCCS PRP system. Collection efficiency and platelet counts of two different methods for the preparation of platelet-rich plasma. Clin Oral Implants Res 13:437443, 2002 71. Weibrich G, Hansen T, Kleis W, et al: Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone 34:665671, 2004 72. Weibrich G, Kleis WK, Hafner G, et al: Growth factor levels in plateletrich plasma and correlations with donor age, sex, and platelet count. J Craniomaxillofac Surg 30:97-102, 2002 73. Marlovits S, Mousavi M, Gabler C, et al: A new simplified technique for producing platelet-rich plasma: A short technical note. Eur Spine J 13:S102-S106, 2004 (suppl 1) 74. Schoendorfer DW, Williamson LH, Sheckler VL, et al: Platelet collection with the Autopheresis-C apheresis system. Vox Sang 58:100-105, 1990